Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 7
Possible impact of the CYP2D6*10 polymorphism on the nonlinear pharmacokinetic parameter estimates of paroxetine in Japanese patients with major depressive disorders
Authors Saruwatari J , Nakashima H, Tsuchimine S, Nishimura M, Ogusu N, Yasui-Furukori N, Noai M, Kamihashi R
Received 15 January 2014
Accepted for publication 4 March 2014
Published 28 April 2014 Volume 2014:7 Pages 121—127
DOI https://doi.org/10.2147/PGPM.S60747
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Junji Saruwatari,1 Hiroo Nakashima,1 Shoko Tsuchimine,2 Miki Nishimura,1 Naoki Ogusu,1 Norio Yasui-Furukori2
1Division of Pharmacology and Therapeutics, Graduate School of Pharmaceutical Sciences, Kumamoto University, Kumamoto, Japan; 2Department of Neuropsychiatry, Graduate School of Medicine, Hirosaki University, Hirosaki, Japan
Abstract: It has been suggested that the reduced function allele with reduced cytochrome P450 (CYP) 2D6 activity, CYP2D6*10, is associated with the interindividual differences in the plasma paroxetine concentrations, but there is no data presently available regarding the influence of the CYP2D6*10 polymorphism on the pharmacokinetic parameters, eg, Michaelis–Menten constant (Km) and maximum velocity (Vmax), in Asian populations. The present study investigated the effects of the CYP2D6 polymorphisms, including CYP2D6*10, on the pharmacokinetic parameters of paroxetine in Japanese patients with major depressive disorders. This retrospective study included 15 Japanese patients with major depressive disorders (four males and eleven females) who were treated with paroxetine. The CYP2D6*2, CYP2D6*4, CYP2D6*5, CYP2D6*10, CYP2D6*18, CYP2D6*39, and CYP2D6*41 polymorphisms were evaluated. A total of 56 blood samples were collected from the patients. The Km and Vmax values of paroxetine were estimated for each patient. The allele frequencies of CYP2D6*2, CYP2D6*4, CYP2D6*5, CYP2D6*10, CYP2D6*18, CYP2D6*39, and CYP2D6*41 were 6.7%, 0%, 10.0%, 56.7%, 0%, 26.7%, and 0%, respectively. The mean values of Km and Vmax were 50.5±68.4 ng/mL and 50.6±18.8 mg/day, respectively. Both the Km and Vmax values were significantly smaller in CYP2D6*10 allele carriers than in the noncarriers (24.2±18.3 ng/mL versus 122.5±106.3 ng/mL, P=0.008; 44.2±16.1 mg/day versus 68.3±15.0 mg/day, P=0.022, respectively). This is the first study to demonstrate that the CYP2D6*10 polymorphism could affect the nonlinear pharmacokinetic parameter estimates of paroxetine in Asian populations. The findings of this study suggest that the CYP2D6*10 polymorphism may be associated with the smaller values of both the Km and Vmax in Japanese patients with major depressive disorders, and these results need to be confirmed in further investigations with a larger number of patients.
Keywords: pharmacokinetics, dose requirement, Michaelis–Menten constant, maximum velocity
Introduction
Paroxetine is a selective serotonin reuptake inhibitor that is widely used in the treatment of mental disorders, including depression, panic disorders, and obsessive compulsive disorder.1 Two previous studies suggested that the plasma drug concentration is associated with the therapeutic response to paroxetine.2,3 Gilles et al suggested an upper threshold of paroxetine serum concentrations (39.1 ng/mL) for the preferable response.2 Another recent study suggested that the plasma paroxetine concentrations of 64.2 ng/mL may distinguish responders from nonresponders and remitters from nonremitters, and low drug concentrations may be associated with preferable treatment.3
Paroxetine is extensively metabolized in humans and exhibits nonlinear kinetics.4,5 It is metabolized by oxidation and methylation in the liver to unstable metabolites that are further conjugated with glucuronic or sulfuric acid.4,6 Cytochrome P450 (CYP) 2D6 is most likely to be the major contributor to paroxetine metabolism in humans.6
CYP2D6 is one of the most widely investigated CYPs in relation to its genetic polymorphisms.7,8 To date, more than 100 allelic variants have been reported for CYP2D6.9 A combination of polymorphisms, including single nucleotide polymorphisms, duplications, insertions/deletions, and/or gene conversions has been reported to cause either increased or reduced activity levels.7,8 Despite the low frequency of nonfunctional CYP2D6 alleles (eg, CYP2D6*4, *5, *18) in Asian populations, the CYP2D6*10 allele that causes intermediate enzyme activity is present at a high frequency of about 50% in Asian populations.7–11 Additionally, the CYP2D6*39 allele is also common in Asian populations, and it may reduce the expression level of CYP2D6 protein, but it does not alter the CYP2D6 activity.11 Among these alleles, it has been suggested that the CYP2D6*10 allele has a significant impact on the plasma paroxetine concentrations in Asians.11–14 Therefore, the therapeutic drug monitoring of paroxetine can substantially contribute to preventing an overdose, especially in the Asian patients with the CYP2D6*10 allele. Because knowing the pharmacokinetic parameters is necessary to optimize the dose administered to each patient, several previous studies have been performed in Caucasian and African-American subjects.15–17 These studies demonstrated that the pharmacokinetic parameters of paroxetine were associated with the CYP2D6 polymorphisms.15–17 Although there are large interethnic differences in the frequencies of the CYP2D6 genotypes, as described above, there is presently no data available regarding the influence of the CYP2D6 polymorphisms on the nonlinear pharmacokinetic parameters, eg, the Michaelis–Menten constant (Km) and maximum velocity (Vmax), in Asian populations.
The aim of the present study was thus to investigate the effects of the CYP2D6 polymorphisms, including CYP2D6*10, on the nonlinear pharmacokinetic parameter estimates of paroxetine in Japanese patients with major depressive disorders using the Michaelis–Menten method.
Material and methods
Subjects and protocol
This retrospective study was conducted at Hirosaki University Hospital (Hirosaki, Japan). The patients with major depressive disorders were recruited from the participants of previous studies.3,18 A dose of 20 mg/day of paroxetine (Paxil®; GlaxoSmithKline, Brentford, UK) was administered at around 8 pm for the first week; thereafter, the dose of paroxetine was increased to 40 mg/day from the 2nd to the 6th weeks. When mild side effects were observed, the dose was maintained. The dose of paroxetine was decreased when moderate side effects were observed. During the paroxetine treatment period, blood samples (10 mL) were collected. The patients were included if they fulfilled all of the following conditions: having received paroxetine for 2 weeks or longer and not taking any drugs that may alter the pharmacokinetics of paroxetine; having normal renal and hepatic functions; and having data available from at least three therapeutic drug monitoring time points at different paroxetine doses. A total of 15 patients were included in the study (four males, eleven females). The mean ± standard deviation age, body weight, the daily paroxetine dose, the time after the last paroxetine dose, and the number of blood samples collected for the pharmacokinetic analysis are shown in Table 1. The mean time after the last paroxetine dose was 13.5±3.4 hours (range: 10–20 hours). A total of 56 blood samples were collected for the pharmacokinetic analyses of paroxetine, and the mean number of blood samples collected per patient was 3.7±0.7 samples (range: 3–5 samples). The range of the daily dose was 10–40 mg/day. The study protocol was approved by the Ethics Committee of the Hirosaki University School of Medicine, and written informed consent was obtained from the patients or their families before the study.
Assays of paroxetine
The plasma paroxetine concentrations were measured using a high-performance liquid chromatography method, as reported previously.3,18
Cytochrome P450 2D6 genotype determination
Genomic DNA was extracted from 5 mL of whole blood via manual extraction using the QIAamp DNA Blood Maxi Kit (QIAGEN, Venlo, the Netherlands). The CYP2D6*5 (deleted) allele was identified using a long polymerase chain reaction (PCR) analysis.19 Genotyping for CYP2D6*2 (rs16947), CYP2D6*4 (rs3892097), CYP2D6*10 (rs1065852), CYP2D6*18 (GTGCCCACT insertion), CYP2D6*39 (rs1135840), and CYP2D6*41 (rs28371725) was performed using real-time PCR with 5′-nuclease allele discrimination assays (ABI PRISM® 7000 Sequence Detection System; Life Technologies, Carlsbad, CA, USA) according to the manufacturer’s protocol (assay identification numbers: C_27102425_10, C_27102431_D0, C_11484460_40, C_32407220_60, C_27102414_10, and C_34816116_20, respectively).
Data analyses and statistics
The Km and the Vmax values of the paroxetine concentrations were estimated by nonlinear regression using the Michaelis–Menten kinetic equation,

where the Dose and Conc are the daily dose and the plasma paroxetine concentration, respectively, in each patient. The comparisons of the patients’ characteristics and the pharmacokinetic parameters associated with the CYP2D6 genotypes were made using the Mann–Whitney U-test or by Fisher’s exact test. Additionally, we determined the associations of the CYP2D6 genotypes with the concentration to dose ratios or pharmacokinetic parameters of paroxetine using a multiple linear regression model with an adjusted regression coefficient (β). The model was developed using the time after the last paroxetine dose or the number of blood samples collected as a random effect. Correlations between the patients’ characteristics and the pharmacokinetic parameters were also assessed using Spearman’s rank correlation coefficient (r). A P-value <0.05 was considered to be statistically significant. The relationships between the daily doses and the plasma concentration of paroxetine were plotted based on the mean values of the observed pharmacokinetic parameters. All statistical analyses were performed with the R software program (version 3.0.0; R Foundation for Statistical Computing, Vienna, Austria).
Results
Six genotypes were identified in the 15 subjects studied: CYP2D6*2/*10 (n=2), CYP2D6*10/*39 (n=2), CYP2D6*39/*39 (n=2), CYP2D6*10/*10 (n=6), CYP2D6*5/*39 (n=2), and CYP2D6*5/*10 (n=1). None of the subjects was identified as a homozygote for the defective CYP2D6 alleles (ie, CYP2D6*4, CYP2D6*5, and CYP2D6*18). The allele frequencies of CYP2D6*2, CYP2D6*4, CYP2D6*5, CYP2D6*10, CYP2D6*18, CYP2D6*39, and CYP2D6*41 were 6.7%, 0%, 10.0%, 56.7%, 0%, 26.7%, and 0%, respectively. The subjects were grouped into two groups according to the combination of these alleles: extensive metabolizers (CYP2D6*2/*10, *10/*39, and *39/*39) and intermediate metabolizers (*10/*10 and *5/*10); the CYP2D6*10/*10 genotype and the other genotypes; or CYP2D6*10 allele carriers and noncarriers.
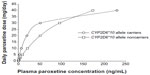
The mean plasma concentrations, the concentrations corrected for dose, and the Km and the Vmax values of paroxetine among all patients enrolled are shown in Table 1. The mean values of Km and Vmax were 50.5±68.4 ng/mL and 50.6±18.8 mg/day, respectively (Table 1). The individual and mean values of the Km and Vmax in CYP2D6*10 allele carriers and noncarriers, respectively, are shown in Figure 1. Both the Km and Vmax values were significantly smaller in CYP2D6*10 allele carriers than in the noncarriers (Table 1 and Figure 1). Figure 2 shows the simulated relationships between the plasma concentration and the daily dose based on the observed mean values of the Km and Vmax in the CYP2D6*10 allele carriers and the noncarriers.
  | Figure 3 Individual and mean values of the plasma concentration in each daily dose of paroxetine among the CYP2D6*10 allele carriers (solid circles) and the noncarriers (open circles). |
Carrying a CYP2D6*10 allele was associated with a lower concentration to dose ratio (β= −1.80, P=0.015) compared with that observed in the CYP2D6*10 allele noncarriers using a multiple linear regression model, which was adjusted for the time after the last paroxetine dose. In CYP2D6*10 allele carriers, the Km value was significantly smaller (β= −84.2, P=0.041), and the Vmax value tended to be smaller (β= −17.1, P=0.075) than that in noncarriers as determined using a multiple linear regression model that was adjusted for the number of blood samples collected.
Figure 3 shows the plots of the daily dose versus plasma concentration of paroxetine in CYP2D6*10 allele carriers and the noncarriers. When we compared the plasma paroxetine concentrations between the CYP2D6 genotypes using the Mann–Whitney U-test, the plasma concentrations did not differ significantly between the CYP2D6*10 allele carriers and the noncarriers among the patients treated with 20 mg/day, 30 mg/day, or 40 mg/day of paroxetine (P=0.673, P=1.000, and P=0.400, respectively) while no CYP2D6*10 allele noncarrier was treated with 10 mg/day of paroxetine (Figure 3).
On the other hand, the Km and Vmax values did not differ between the CYP2D6 intermediate and extensive metabolizers (25.7±16.7 ng/mL versus 72.1±89.3 ng/mL, P=0.189 and 46.8±12.1 mg/day versus 54.0±23.5 mg/day, P=0.336, respectively) and between the CYP2D6*10/*10 genotype and the other genotypes (27.5±17.5 ng/mL versus 65.8±85.7 ng/mL, P=0.388 and 49.3±11.2 mg/day versus 51.5±23.2 mg/day, P=0.607, respectively).
Since the mean age was significantly lower in CYP2D6*10 allele carriers than in the noncarriers (Table 1), we analyzed the association of the pharmacokinetic parameters with subjects’ age separately in the CYP2D6*10 allele carriers and noncarriers. The Km values did not correlate with the age in CYP2D6*10 allele carriers (r= −0.119, P=0.728) and noncarriers (r=0.400, P=0.750), and the Vmax values also did not correlate with age in the CYP2D6*10 allele carriers (r=0.005, P=0.989) and noncarriers (r= −0.600, P=0.417).
Discussion
In this study, we found that the CYP2D6*10 polymorphisms were associated with smaller values of Km and Vmax in Japanese patients with major depressive disorder. Two previous studies reported that the CYP2D6 genotypes could influence the pharmacokinetic parameters of paroxetine in patients with major depressive disorder or obsessive-compulsive disorder, but these studies included mainly Caucasian patients.16,17 Findling et al reported that the oral clearance and volume of distribution were highly associated with the CYP2D6 polymorphisms.16 In the study by Findling et al the decreased oral clearance associated with an increase in the paroxetine dose, ie, the saturation of the clearance, was more pronounced in the CYP2D6 extensive metabolizers than in the intermediate and poor metabolizers.16 Another population pharmacokinetic study revealed that the Vmax values were significantly smaller in the CYP2D6 intermediate and poor metabolizers than those in the extensive metabolizers.17 Since the frequency of the CYP2D6 genotypes exhibits a large interethnic variability, and because the CYP2D6*10 allele is the most common in Asian populations,7–11 we focused on the influence of the CYP2D6*10 polymorphism on the pharmacokinetic parameters of paroxetine in the present study. To the best of our knowledge, this is the first study to demonstrate that the CYP2D6*10 polymorphism could have an impact on the nonlinear pharmacokinetic parameter estimates of paroxetine in Japanese patients with major depressive disorders.
The CYP2D6.10 enzyme has a P34S substitution that results in an unstable enzyme with reduced affinity for CYP2D6 substrates.7,8 In vitro studies demonstrated that paroxetine showed an approximately 13-fold greater inhibition constant, ie, Ki, value in CYP2D6.10 than in CYP2D6.1.20 In this study, we observed smaller Vmax values in the CYP2D6*10 allele carriers (Table 1 and Figure 1). The results of this study are in line with the findings of the previous Korean and Japanese studies showing that the plasma paroxetine concentrations at doses of 30~40 mg/day were higher in the carriers of the defective or reduced function alleles, including CYP2D6*10, than the homozygotes for the wild type allele.12,14 The results of this study also suggest that the paroxetine metabolism could become saturated at a lower dose in the CYP2D6*10 allele carriers compared to the noncarriers (Figure 2).
A recent study of Japanese patients indicated that the plasma paroxetine concentrations at doses of 10~20 mg/day were not associated with the defective or reduced function alleles, mainly CYP2D6*10,14 although the results were not confirmed in another previous study.13 Paroxetine is extensively metabolized via high affinity CYP2D6 to unstable intermediate metabolites,6 and mechanism-based inhibition of CYP2D6 by these metabolites has been observed.14,21 The present study demonstrated that the values of Km, which is the paroxetine concentration at the dose of Vmax/2, were significantly smaller in the CYP2D6*10 allele carriers compared to the noncarriers (Table 1, Figures 1 and 2), suggesting that the rate of the paroxetine metabolism at a low dose could be greater in the CYP2D6*10 allele carriers. We speculate that the lower formation of the unstable metabolite in the CYP2D6*10 allele carriers might be associated with the decreased inhibitory effect on CYP2D6, thus resulting in smaller Km values in the CYP2D6*10 allele carriers.
In this study, there were no significant differences in the Km and Vmax values between the CYP2D6 intermediate (ie, CYP2D6*10/*10 or *5/*10 genotypes) and extensive metabolizers or between the CYP2D6*10/*10 genotype and the other genotypes. These results may be in line with another recent study showing that the average area under the concentration-time curves of paroxetine in the homozygous CYP2D6*10/*10 carriers was not different from that in the subjects heterozygous for CYP2D6*10.12 Therefore, the effects of the CYP2D6*10/*10 genotype or the intermediate metabolizers on the paroxetine pharmacokinetics might be comparable to those of the heterozygotes for the CYP2D6*10 allele. The findings of this study may suggest that the effects of the CYP2D6*10/*10 or *5/*10 genotype might not be associated with the interindividual differences in the Km and Vmax values in Japanese patients with major depressive disorders. Nevertheless, further studies of a larger number of subjects are required to elucidate whether the CYP2D6*10/*10 or *5/*10 genotype can affect the nonlinear pharmacokinetic parameters of paroxetine.
CYP2D6 activity has been reported to be lower in elderly subjects than in young subjects. For example, Schulz et al reported a reduction in amitriptyline metabolism (young versus elderly half-life: mean 16.2 versus 21.7 hours; clearance: mean 10.8 versus 12.5 mL/min/kg, respectively) in a group of elderly healthy males (mean age: 71 years) compared with younger healthy males (mean age: 22 years).22 In this study, the mean age was significantly lower in CYP2D6*10 allele carriers than in the noncarriers (Table 1). However, the mean ages in CYP2D6*10 allele carriers and the noncarriers represent younger and older adults, respectively (Table 1), but not elderly subjects, and we did not observe any correlation between the patient’s age and the Km or Vmax in the CYP2D6*10 allele carriers and noncarriers in the present study. These results suggest that age might not have affected the associations between the CYP2D6*10 polymorphism and pharmacokinetic parameters of paroxetine in this study. However, the findings were obtained from a small sample of patients, and therefore the effects of age (younger versus older adults) on the nonlinear pharmacokinetic parameters of paroxetine remain unknown.
A major limitation of this study was that the number of subjects was small. Since we assessed the impact of different CYP2D6 genotypes on the pharmacokinetic parameters of paroxetine, the sample sizes were small when the patients were stratified by the genotypes. Additionally, the observed pharmacokinetic parameters showed large interindividual variations (Table 1 and Figure 1), and we could not observe any significant effect of the CYP2D6*10 polymorphism on the relationship between the plasma concentrations and the daily dose of paroxetine (Figure 3). Therefore, the associations between the pharmacokinetic parameters and the CYP2D6*10 polymorphism might be overestimated, and the possibility of a Type 1 error cannot be excluded. Moreover, although two previous studies suggested that the plasma drug concentration is associated with the therapeutic response to paroxetine,2,3 other previous studies have failed to find any correlation of the plasma paroxetine concentration with the efficacy or adverse events.23,24 Therefore, the findings of the present study should be replicated with a larger number of subjects, and future studies are needed to elucidate the impact of the CYP2D6*10 polymorphism on the pharmacokinetic parameters as well as the dose requirement of paroxetine, after incorporating the clinical efficacy and adverse effects.
Conclusion
We herein provide findings showing that the CYP2D6*10 polymorphism may be associated with smaller values of both the Km and Vmax in Japanese patients with major depressive disorders, suggesting that our results may be helpful for obtaining appropriate blood paroxetine concentrations based on the CYP2D6*10 genotypes. Since the findings of this study were based on a small sample size, these results need to be confirmed in further investigations with a larger number of patients.
Acknowledgments
The authors wish to thank all of the study participants. This work was supported by KAKENHI (No 25860117 and No 24590652), a research fund from Hirosaki University School of Medicine, and a grant from the Hirosaki Research Institute for Neurosciences.
Disclosure
The authors report no conflicts of interest in this work.
References
Gibiino S, Serretti A. Paroxetine for the treatment of depression: a critical update. Expert Opin Pharmacother. 2012;13(3):421–431. | |
Gilles M, Deuschle M, Kellner S, et al. Paroxetine serum concentrations in depressed patients and response to treatment. Pharmacopsychiatry. 2005;38(3):118–121. | |
Yasui-Furukori N, Nakagami T, Kaneda A, et al. Inverse correlation between clinical response to paroxetine and plasma drug concentration in patients with major depressive disorders. Hum Psychopharmacol. 2011;26(8):602–608. | |
Kaye CM, Haddock RE, Langley PF, et al. A review of the metabolism and pharmacokinetics of paroxetine in man. Acta Psychiatr Scand Suppl. 1989;350:60–75. | |
Sindrup SH, Brøsen K, Gram LF. Pharmacokinetics of the selective serotonin reuptake inhibitor paroxetine: nonlinearity and relation to the sparteine oxidation polymorphism. Clin Pharmacol Ther. 1992;51(3):288–295. | |
Jornil J, Jensen KG, Larsen F, Linnet K. Identification of cytochrome P450 isoforms involved in the metabolism of paroxetine and estimation of their importance for human paroxetine metabolism using a population-based simulator. Drug Metab Dispos. 2010;38(3):376–385. | |
Zhou SF. Polymorphism of human cytochrome P450 2D6 and its clinical significance: Part I. Clin Pharmacokinet. 2009;48(11):689–723. | |
Teh LK, Bertilsson L. Pharmacogenomics of CYP2D6: molecular genetics, interethnic differences and clinical importance. Drug Metab Pharmacokinet. 2012;27(1):55–67. | |
CYP2D6 allele nomenclature [webpage on the Internet]. The Human Cytochrome P450 (CYP) Allele Nomenclature Database [updated Jun 21, 2006]. Available from: http://www.imm.ki.se/cypalleles/cyp2d6.htm. Accessed December 14, 2013. | |
Suzuki Y, Fukui N, Tsuneyama N, et al. Effect of the cytochrome P450 2D6*10 allele on risperidone metabolism in Japanese psychiatric patients. Hum Psychopharmacol. 2012;27(1):43–46. | |
Sakuyama K, Sasaki T, Ujiie S, et al. Functional characterization of 17 CYP2D6 allelic variants (CYP2D6.2, 10, 14A-B, 18, 27, 36, 39, 47–51, 53–55, and 57). Drug Metab Dispos. 2008;36(12):2460–2467. | |
Yoon YR, Cha IJ, Shon JH, et al. Relationship of paroxetine disposition to metoprolol metabolic ratio and CYP2D6*10 genotype of Korean subjects. Clin Pharmacol Ther. 2000;67(5):567–576. | |
Sawamura K, Suzuki Y, Someya T. Effects of dosage and CYP2D6-mutated allele on plasma concentration of paroxetine. Eur J Clin Pharmacol. 2004;60(8):553–557. | |
Ueda M, Hirokane G, Morita S, et al. The impact of CYP2D6 genotypes on the plasma concentration of paroxetine in Japanese psychiatric patients. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30(3):486–491. | |
Sindrup SH, Brøsen K, Gram LF, et al. The relationship between paroxetine and the sparteine oxidation polymorphism. Clin Pharmacol Ther. 1992;51(3):278–287. | |
Findling RL, Nucci G, Piergies AA, et al. Multiple dose pharmacokinetics of paroxetine in children and adolescents with major depressive disorder or obsessive-compulsive disorder. Neuropsychopharmacology. 2006;31(6):1274–1285. | |
Feng Y, Pollock BG, Ferrell RE, Kimak MA, Reynolds CF, Bies RR. Paroxetine: population pharmacokinetic analysis in late-life depression using sparse concentration sampling. Br J Clin Pharmacol. 2006;61(5):558–569. | |
Yasui-Furukori N, Tsuchimine S, Nakagami T, et al. Association between plasma paroxetine concentration and changes in plasma brain-derived neurotrophic factor levels in patients with major depressive disorder. Hum Psychopharmacol. 2011;26(3):194–200. | |
Steen VM, Andreassen OA, Daly AK, et al. Detection of the poor metabolizer-associated CYP2D6(D) gene deletion allele by long-PCR technology. Pharmacogenetics. 1995;5(4):215–223. | |
Ramamoorthy Y, Tyndale RF, Sellers EM. Cytochrome P450 2D6.1 and cytochrome P450 2D6.10 differ in catalytic activity for multiple substrates. Pharmacogenetics. 2001;11(6):477–487. | |
Bertelsen KM, Venkatakrishnan K, Von Moltke LL, Obach RS, Greenblatt DJ. Apparent mechanism-based inhibition of human CYP2D6 in vitro by paroxetine: comparison with fluoxetine and quinidine. Drug Metab Dispos. 2003;31(3):289–293. | |
Schulz P, Turner-Tamiyasu K, Smith G, Giacomini KM, Blaschke TF. Amitriptyline disposition in young and elderly normal men. Clin Pharmacol Ther. 1983;33(3):360–366. | |
Tasker TC, Kaye CM, Zussman BD, Link CG. Paroxetine plasma levels: lack of correlation with efficacy or adverse events. Acta Psychiatr Scand Suppl. 1989;350:152–155. | |
Normann C, Hörn M, Hummel B, Grunze H, Walden J. Paroxetine in major depression: correlating plasma concentrations and clinical response. Pharmacopsychiatry. 2004;37(3):123–126. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.