Back to Journals » Clinical Optometry » Volume 15
Ocular Protection Practice and Associated Factors Among Ethiopian Welders: Institution-Based Cross-Sectional Study
Authors Belete YA , Assefa NL , Tegegn MT
Received 6 June 2023
Accepted for publication 5 September 2023
Published 11 September 2023 Volume 2023:15 Pages 175—184
DOI https://doi.org/10.2147/OPTO.S424522
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Mr Simon Berry
Yared Ayelign Belete,1 Natnael Lakachew Assefa,2 Melkamu Temeselew Tegegn2
1Department of Ophthalmology and Optometry, School of Medicine, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia; 2Department of Optometry, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Melkamu Temeselew Tegegn, Department of Optometry, College of Medicine and Health Sciences, University of Gondar, P.O.BOX:196, Gondar, Ethiopia, Email [email protected]
Introduction: Work-related ocular injury is a global public health problem, particularly among welders and is reduced through proper ocular protection practice. No previous studies have explored ocular protection practice and associated factors among welders in Ethiopia or in the study area.
Objective: This study aimed to assess the proportion of ocular protection practice and associated factors among welders in Gondar city, Northwest Ethiopia.
Methods: An institution-based cross-sectional study was conducted among 403 welders in Gondar city, selected using systematic random sampling with an interval of 2, from July 6 to 23, 2021. Data were collected using a pre-tested structured questionnaire and an observational checklist. Binary logistic regression was used to identify factors associated with ocular protection practice and association was expressed using an adjusted odds ratio with a 95% confidence interval (CI). Variables with a P-value of less than 0.05 were considered statistically significant.
Results: Of 396 participated welders, 81.8% worked without job training, and 33.1% had faced ocular injury. Nearly 86% of welders had access to personal protective eyewear but their knowledge and attitude towards personal protective eyewear were 48.2% (95% CI: 44.8, 51.4) and 61.4% (95% CI: 57.6, 64.7), respectively. The proportion of a good-level of ocular protection practice was 56.8% (95% CI: 52.8, 61.9). Being gas welder (adjusted odds ratio [AOR]=0.26, 95% CI: 0.12, 0.53), work experience (AOR = 1.10, 95% CI: 1.01, 1.21), job training (AOR = 4.90, 95% CI: 2.32, 10.35), welders rated the cost of personal protective eyewear as fair (AOR = 2.30, 95% CI: 1.26, 4.20) and history ocular injury (AOR = 4.20, 95% CI: 2.40, 6.97) were positively associated with a good-level proportion of ocular protection practice.
Conclusion: This study found that the proportion of a good-level of ocular protection practice of welders was fair. Being gas welder, job training, work experience, history of ocular injury and welders rated the cost of personal protective eyewear as fair were significantly associated with a good-level of ocular protection practice.
Keywords: ocular protection practice, personal protective eyewear, welders, Gondar city
Introduction
Although protecting the eye from any form of ocular injury or harmful radiation exposure is one of the primary levels of disease prevention and health promotion;1 globally, approximately 1.6 million people are blind and 2.3 million people have bilateral visual impairment due to work-related ocular injuries,2 and more than half a million blind injuries happen in each year.3 In addition, according to the United States National Institute for Occupational Safety and Health report showed that approximately 2000 work-related eye injuries occurred in every day.4 Lack of job training, failure to use personal protective equipment, and lack of supervision by health and safety personnel were the main causes of work related ocular injury.5
Welding is a hazardous profession that involves cutting a single piece of metal into two and then fusing it back together using a flame or an electric arc, and other sources of heat.6 Arc and gas welding are the major types of welding.7 Arc (electric) welding uses a welding power supply to create an electric arc between an electrode and the base metal to melt the metals at the welding point whereas gas (oxyacetylene) welding uses the high temperature produced by burning a mixture of oxygen and acetylene to melt metals at the welding point.8
Welding-exposure-related ocular health hazards remain a critical occupational health and safety issue for welders in the world’s low- and middle-income countries.9 Studies conducted in sub-Saharan African countries have indicated that large-scale ocular injuries occur in small-scale industries including welding.10–13 Similarly, a study conducted in Addis Ababa, Ethiopia, showed that 99.6% of welders had a complained of visual problems during the welding process.14 Furthermore, welders are highly vulnerable to mid to severe perforating eye injuries, photo-keratitis, pterygium, cataract, and macular degeneration from their profession because welding is one of the highest artificial sources of flying particles or sharp object, thermal burn and harmful radiation (ultraviolet and infrared).10,15,16
The ocular protection practice is the practice of protecting an eye from the potential ocular health hazards of welding exposure by using personal protective eyewear.8 Evidence in African shows that the magnitude of ocular protection practice among welders’ ranges from 2.3% to 96.9%.17–20 Welding-related ocular injuries are largely preventable by adequate and proper use of eye protection devices.21,22 Welders must use eye protective devices such as safety glasses, helmets, face shields, and filter glasses to protect their eyes from harmful radiation and mechanical injuries.23 Despite welders having a good-level of awareness about work-related hazards and individual protective eyewear, most welders do not regularly use protective devices.8,24,25
Welder eyes exposed to ultraviolet and infrared radiation, metal fumes, particulate matter, and thermal burns can develop serious acute ocular conditions that leads to visual impairment. This cannot be prevented or reduced by the presence or availability of standard personal protective eyewear, which requires effective strategies to enhance welder knowledge, attitude, and utilization of personal protective eyewear during the welding process. In Ethiopia, the studies conducted in Addis Ababa14 and Tigray region,26 Ethiopia among welders did not assess the level of knowledge and attitude towards personal eye protective eyewear and ocular protection practice rather they assessed the awareness of occupational hazard. In addition, study done in Tigray region, Ethiopia26 reported that the overall use of personal protective equipments such as face mask, boots, ear plug, hand glove, apron and eye goggles rather ocular protection practice. So, this study filled the research gap by explored the level of knowledge and attitude towards personal eye protective eyewear, and magnitude of ocular protection practice and associated factors among welders in Ethiopia or in the study area. Moreover, this study provides the baseline data for policymakers to develop a standard on occupational eye health safety. Finally, the main objective of this study was to determine the proportion of ocular protection practice and associated factors among welders in Gondar city, Northwest Ethiopia.
Methods and Materials
Study Design, Setting, and Period
An institution-based cross-sectional study was conducted among 403 welders in Gondar City, Northwest Ethiopia, from July 6 to 23, 2021. Gondar City is located in the central Gondar zone 748 km from Addis Ababa, the capital city of Ethiopia. According to the Ethiopian census projection in 2017, approximately 234,951 people lived in Gondar City.27 Data from the Gondar City Administration Technical and Vocational Enterprises Development Department showed that there were 103 welding shops with 1130 welders. In Gondar City, the University of Gondar Tertiary Eye Care and Training Center and three private ophthalmic clinics provide comprehensive ophthalmic services including occupation-related ocular injuries.
Study Population and Eligibility Criteria
All welders who worked permanently in the respective welding shops in Gondar City and were available during the data collection period were included in this study.
Sample Size Determination and Sampling Procedure
Sample size was determined using a single population proportion formula with the consideration of the expected proportion of a good-level ocular protection practice was 50%, since there was no similar study conducted in Ethiopia, 95% confidence level, and margin of error of 5%. The calculated sample size was 384. And adding a non-response rate of 5%, the final required sample size was 403. To ensure representativeness, 90 welding shops were selected out of 103 welding shops using the lottery method. The selected welder shops (90 welding shops) comprised of 990 workers. Finally, the study participants from each welder shop were selected using a systematic random sampling technique with an interval of 2. A single number was taken from 1 to 2 using a lottery method to determine the first welder and continued with every K interval of 2 until the calculated sample size was attained. The interval was calculated by dividing the estimated number of welders present in the 90 welding shops (N = 990; n = 403; K = 990/403 = 2).
Operational Definitions
Ocular protection practice was assessed by using 11 questions. Participants who responded with the correct answer to the given question scored one point, whereas participants who responded incorrectly to the given question scored zero. The total score ranges from 0 to 11 points. Participants with scores equal to or exceeding the mean value were considered to have a good-level ocular protection practice whereas those with scores below the mean value were considered as having poor ocular protection practice.
Knowledge of personal protective eyewear was assessed using 4 knowledge questions, and the score points range from 0 to 4. Participants with scores equal to or exceeding the mean value were categorized as having a good-level knowledge about personal protective eyewear whereas those with scores below the mean value were categorized as having poor knowledge about personal protective eyewear.
Attitude towards personal protective eyewear was assessed using 6 attitude-related questions, and the score points range from 0 to 6. Participants with scores equal to or exceeding the mean value were categorized as having a good-level attitude towards personal protective eyewear whereas those with scores below the mean value were categorized as having poor attitude towards personal protective eyewear.
Ocular injury: any eye or ocular adnexa injury that occurred to the welders while working in welding within the past years.28
Data Collection Procedures (Instrument and Personnel)
An interviewer-administered Amharic (local language) pre-tested structured questionnaire and observational checklist were used to collect the data. The questionnaire was developed from the reviewed literature17,19,29,30 in the English, and translated into the Amharic version for data collection, and re-translated into the English by using language experts. The questionnaire included socio-demographic data, job-related data, and questions related to knowledge and attitude towards personal protective eyewear and ocular protection practice. In addition, the observational checklists where assessed welders who wear a personal protective eyewear are prescribed safety glasses or safety goggles over their prescription glasses or not, and handling, fitting and scratch of personal protective eyewear (see Supplementary Material). The data were collected by three well-trained BSc Optometrists.
Data Quality Maintenance and Analysis
Data quality was maintained by performing a pre-test on 5% of the sample size in Maksegnt town, Northwest of Ethiopia. In addition, data quality was assured by providing training for data collectors, checking the completeness of the data, and assigning supervisors during data collection.
After checking the completeness and consistency of the data, it was entered into Epi data version 4.6, and exported into Statistical Package for Social Science (SPSS) version 26 (SPSS Inc, Chicago, Illinois, USA) for analysis. Descriptive and analytical statistical analyses were performed. Binary logistic regression was fitted. All variables with a P value of less than equal to 0.2 in the bivariable analysis were entered into a multivariable binary logistic regression to identify possible predictors for ocular protection practice and association was expressed using an adjusted odds ratio with a 95% of a confidence interval.31 The fitness of the model was checked using Hosmer-Lemeshow’s goodness of fit. Variables with a two-sided P-value of less than 0.05 were considered statistically significant.
Ethical Approval
This study was conducted in accordance with the principles of the Declaration of Helsinki. Ethical approval was obtained from the University of Gondar, College of Medicine and Health Sciences School of Medicine Ethical Review Committee. A written letter of permission was obtained from the owner of each welding house. After providing a detailed explanation of the study purpose, verbal informed consent was obtained from each study participant. Verbal informed consent was accepted and approved by the ethical review committee of the University of Gondar, and the Ref. number was 688/06/2021. All study participants were informed of their right to refuse to participate and withdraw from the study at any time. Confidentiality was also maintained by avoiding any personal identifier from the data collection tool and using codes. Finally, the study participants who presented with ocular injuries were referred to the University of Gondar Tertiary Eye Care and Training Centre.
Results
Socio-Demographic Characteristics of the Study Participants
In total, 396 participants were included in the study, with a response rate of 98.3%. The median age of the study participants was 25 ± 9 years. Among 396 study participants, 300 (75.8%) were males and currently single (Table 1).
 |
Table 1 Socio-Demographic Characteristics of the Study Participants in Gondar City, Northwest Ethiopia, 2021 (n = 396) |
Job-Related Factors and Availability of Personal Protective Eyewear
Among a total of 396 participants, 164 (41.4%) worked on both arc and gas welding tasks. Nearly eighty-two percent (81.8%) of participants worked in welding without taking job training. Three hundred thirty-nine (85.6%) of participants had access to personal protective eyewear. Out of 396 study participants, 33.1% had a previous history of ocular injury (Table 2).
 |
Table 2 Job-Related Factors and Availability of Personal Protective Eyewear Among Welders in Gondar City, Northwest Ethiopia, 2021 (n = 396) |
Proportion of Ocular Protection Practice and Knowledge and Attitude Towards Personal Protective Eyewear
In the current study revealed that the proportion of a good level of ocular protection practice was 56.8% (95% CI: 52.8, 61.9).
Of 396 study participants, 191 (48.2% (95% CI: 44.8, 51.4)) and 243 (61.4% (95% CI: 57.6, 64.7)) had a good level of knowledge and attitude towards personal protective eyewear, respectively. The most utilized personal protective eye wear was sunglass (31.3%), followed by sunglass with face shield (24.0%) and Goggles (20.2%) (Table 3).
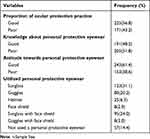 |
Table 3 Proportion of Ocular Protection Practice and Knowledge and Attitude Towards Personal Protective Eyewear Among Welders in Gondar City, Northwest Ethiopia, 2021 (n = 396) |
Factors Associated with a Good Level of Ocular Protection Practice
By applying bivariable analysis, educational status, job training, working experience, types of welding, access to personal protective eyewear, welders rated the cost of personal protective eyewear, and history of ocular injury was positively associated with a good level of ocular protection practice. However, multivariable binary logistic regression analysis revealed that types of welding, job training, working experience, welders rated the cost of personal protective eyewear, and history of ocular injury were significantly and independently associated with a good level of ocular protection practice.
The odds of having a good-level of ocular protection practice were 74% less likely in those participants who worked on gas welding than arc welding type (AOR = 0.26, 95% CI: 0.12, 0.53). Participants who underwent job training were 4.90 times more likely to have a good-level of ocular protection practice (AOR = 4.90, 95% CI: 2.32, 10.35) than their counterparts.
Regarding work experience, as the year of experience increased by a unit of the year, the odds of having a good-level of ocular protection practice of the welders was increased by a factor of 1.10 (AOR = 1.10, 95% CI: 1.01, 1.21). Welders rated the cost of the personal protective eyewear as fair were 2.30 times more likely to have a good level of ocular protection practice than those welders rated the cost of the personal protective eyewear as expensive (AOR = 2.30, 95% CI: 1.26, 4.20). Moreover, the odds of having a good-level of ocular protection practice were 4.09 times for those participants having a history of ocular injury as compared to participants who had not a history of ocular injury (AOR = 4.09, 95% CI: 2.40, 6.97) (Table 4).
 |
Table 4 Factors Associated with a Good-Level of Ocular Protection Practice Among Welders in Gondar City, Northwest Ethiopia, 2021 (n = 396) |
Discussion
In the current study, the proportion of a good level of ocular protection practice was 56.8% (95% CI: 52.8, 61.9) which was lower than the studies conducted in South Africa 89.0%,19 Nigeria 96.6%20 and Uganda 89.0%.32 This difference might be due to variations in accessing occupational health information, work experience in welding, duration of working time per day, measurement of outcome variable, and sample size. For instance, long working experienced participants and those with short working time per day could have a good-level utilization of eye protective devices. Evidence has shown that the occurrence of fogging is lower in short working hours per day, which is the main barrier to ocular protection practice.33 In addition, studies conducted in South Africa, Nigeria and Uganda were used only one question to assessed ocular protection practice while this study used eleven questions.
However, the proportion of a good-level of ocular protection practice in this study was higher than the studies conducted in south India 45.0%,34 Taiwan 41.9%,35 Benin 2.3%,17 different states of Nigeria 25.2–37.6%16,18,36 and Nepal 47.7%.37 This might be the variation in study design, data collection tools, and sample size. For example, studies in India and Benin were conducted with small sample size and a case–control study design was employed in Taiwan.
This study found that the odds of having a good level of ocular protection practice were 74% less likely for those gas welders’ participants than arc-type welders. This finding is consistent with those reported in India,34 Nigeria,8 and Ghana.12 As compared to gas welding, arc welding is used voltage and creates high temperature which leads to the development of photokeratitis, a condition where Ultraviolet light inflames the cornea or even burns the retina of the eyes12 that exposed the arc welders’ were utilized the personal protective eyewear. This finding indicated that stakeholder particularly occupational safety and health policy will design strategies to provide eye health education and training for welders to halt this discrepancy. Besides, this requires further similar research with large sample size by categorize the welders based on type of welding.
In the present study, job training was significantly associated with a good level of ocular protection practice. Participants who underwent job training were 4.90 times more likely to have a good level of ocular protection practice than those who did not job training. This result agreed with those studies conducted in India,34 Nigeria,38 and Ethiopia.26 Welders have baseline information about the nature of work and related ocular hazards and safety measures at a working time, which causes ocular protection practice to be higher in trained welders than untrained welders. This result implicates that participants having adequate information about their job are a precursor to establishing good ocular protection practice and requiring a multidisciplinary approach to create awareness on the impact of welding in the eye and utilization of personal protective eyewear.
Working experience was significantly associated with good level of ocular protection practice, as the year of experience increased by a unit of the year, the odds of having a good level of ocular protection practice of the welders was increased by a factor of 1.10, which was consistent with a study done in Nepal.39 Increasing the working experience of the welders might enhance their awareness of welding-related ocular hazards and adherence to the utilization of personal protective eye devices by exposing in different safety training sessions.
In the present study, welders who rated the cost of personal protective eyewear as fair were 2.30 times more likely to have a good level of ocular protection practice than those rated the cost the personal protective eyewear as expensive. Welders who rated the cost of personal protective eyewear as expensive may not afford it; therefore, the practice of ocular protection was poorer than that of participants who rated the cost of personal protective eyewear as fair. This requires provision of free or low-cost personal protective eyewear by the occupational safety and health policy organization in the country.
In this study, the odds of having a good level of ocular protection practice were 4.90 times more likely for those participants who had a history of ocular injury than those who had no history of ocular injury. This finding was in line with those studies conducted in Canada,40 Alabama, USA,28 Nepal,37 and Nigeria.18 Welders with previous injuries likely understood the impact of their work on the health of the eye and the preventative merits of protective eyewear and altered their protective eyewear utilization behavior after sustaining their ocular injuries.
The limitations of the study are that the data collection includes self-reports from the study participants, which may affect the precision of the result as a result of social desirability bias or recall bias.
Conclusion
This study found that the proportion of a good level of ocular protection practice of welders was fair. Being gas welders, job training, increased work experience, welders rating the cost of personal protective eyewear as fair and history of ocular injury were significantly associated with a good level of ocular protection practice. We recommend providing job training and affordable personal protective eyewear to enhance ocular protection practice and reduce ocular injury in welders.
In addition, large-scale observational and comparative cross-sectional studies between arc and gag welders were recommended for a better estimation of the level of ocular protection practice.
Data Sharing Statement
All the necessary data are included in the manuscript, and if needed, the supporting data are available from the corresponding author.
Funding
There is no funding provided for this research.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Disease prevention and healthy lifestyles; [cited May 22, 2021]. Available from: https://courses.lumenlearning.com/diseaseprevention/chapter/three-levels-of-health-promotion-disease-prevention/.
2. Caroline JM. Ocular injuries. J R Coll Surg Edinb. 1999;93(44):17–23.
3. Négrel A-D, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998;5(3):143–169. doi:10.1076/opep.5.3.143.8364
4. Eye safety |NIOSH |CDC; 2020 [cited Apr 9, 2021] Available from: https://www.cdc.gov/niosh/topics/eye/default.html.
5. Hunegnaw B, Molla M, Mulugeta Y, Meseret M. Assessment of occupational injury among industrial workers in the Bahir Dar city of northwest Ethiopia: institution-based cross-sectional study. J Environ Public Health. 2021;2021:1–8. doi:10.1155/2021/2793053
6. Khan MI. Welding Science and Technology. New Age International; 2007.
7. Antonini JM. Health effects of welding. Crit Rev Toxicol. 2003;33(1):61–103. doi:10.1080/713611032
8. Eze BI, Okoye O, Aguwa EN. Awareness and utilization of welders’ personal protective eye devices and associated factors: findings and lessons from a Nigerian population. Workplace Health Saf. 2015;63(4):170–178. doi:10.1177/2165079915578665
9. Omolase CO, Mahmoud AO. The welder’s protective goggle: an evaluation of its appreciation. Niger J Surg Sci. 2007;17:54–58.
10. Mulugeta D, Bejiga A. Work related ocular injuries in small scale industries. J Ophthalmol East Cent South Afr. 2018;21(2):5.
11. Ihekaire DE, Oji CS. Corneal injuries associated with ocular hazards in the welding industry: a case study of nekede mechanic village nekede, imo state, Nigeria. Int J Ophthalmol Vis Sci. 2017;2(2):37–54.
12. Tetteh KKK, Owusu R, Axame WK. Prevalence and factors influencing eye injuries among welders in Accra, Ghana. Adv Prev Med. 2020;2020:1–8.
13. Yego W, Ragot A. Awareness of ocular-related effects of welding among welders in Kakamega, Kenya. Eur J Public Health Stud. 2020;2(1). doi:10.5281/zenodo.3740238
14. Tadesse S, Bezabih K, Destaw B, Assefa Y. Awareness of occupational hazards and associated factors among welders in Lideta Sub-City, Addis Ababa, Ethiopia. J Occup Med Toxicol. 2016;11(1):1–6. doi:10.1186/s12995-016-0105-x
15. Kumah D, Cobbina F, Duodu D. Radiation-related eye diseases among welders of Suame ‘magazine’in the Kumasi metropolis. J Sci Technol Ghana. 2011;31(1). doi:10.4314/just.v31i1.64884
16. Okeigbemen V, Omoti A, Ovienria W. Pattern of ocular injuries and use of protective eye devices among welders. J Med Biomed Res. 2012;11(1):5–13.
17. Théodore S, Stanislas D, Soulé A, et al. Study of the practice of eye protection at work among Ahogbohoue welders (Cotonou, Benin Republic). Eur J Res Med Sci. 2020;8(2):8–13.
18. Ajayi IA, Adeoye AO, Bekibele CO, et al. Awareness and utilization of protective eye device among welders in a southwestern Nigeria community. Ann Afr Med. 2011;10(4):294–299. doi:10.4103/1596-3519.87047
19. Sithole H, Oduntan O, Oriowo M. Eye protection practices and symptoms among welders in the Limpopo Province of South Africa+. Afr Vis Eye Health. 2009;68(3):130–136. doi:10.4102/aveh.v68i3.163
20. Osagiede E, Ilokhor O, Ehimen F, et al. Assessment of awareness of occupational health problems, and the practices of safety measures among welders in a semi-urban town in South-South Nigeria. West J Med Biomed Sci. 2020;1(2):139–149.
21. Peate W. Work-related eye injuries and illnesses. Am Fam Physician. 2007;75(7):1017–1022.
22. Turbert D. Eye injury prevention. Am Acad Ophthalmol. 2019. Available from https://www.aao.org/eye-health/tips-prevention/preventing-injuries. Accessed September 5, 2023.
23. Goff T. Flexible welding protection. Occup Health Saf Waco Tex. 2006;75(9):32–34.
24. Fiebai B, Awoyesuku E. Ocular injuries among industrial welders in Port Harcourt, Nigeria. Clin Ophthalmol. 2011;5:1261–1263. doi:10.2147/OPTH.S20297
25. Nagaradagadde N, Mummidi SV, Khan Z, Misra M. Study on awareness of ocular occupational hazards among welders presenting to OPD of tertiary healthcare centre at Bhubaneshwar, Odisha. J Med Sci Clin Res. 2019;7(1):1014–1019. doi:10.18535/jmscr/v7i1.177
26. Gebrezgiabher BB, Tetemke D, Yetum T. Awareness of occupational hazards and utilization of safety measures among welders in Aksum and Adwa towns, Tigray region, Ethiopia, 2013. J Environ Public Health. 2019;2019. doi:10.1155/2019/4174085
27. Ethiopian Census - 2017 Projection - Amhara - North Gondar – Gondar; [cited May 24, 2021]. Available from: https://www.qotera.org/en-US/2017/amhara/north-gondar/gondar/.
28. Blackburn JL, Levitan EB, MacLennan PA, et al. Changes in eye protection behavior following an occupational eye injury. Workplace Health Saf. 2012;60(9):393–400. doi:10.3928/21650799-20120816-52
29. Anita OE, Monica OO, Uyinmwen OR. Eye safety practices among welders in Alimosho Local Government Area in Lagos, Nigeria. Savanna J Basic Appl Sci. 2019;1(1):121–125.
30. Oduntan AO. A survey of eye safety practices among welders in Nigeria. Clin Exp Optom. 1998;81(1):29–33. doi:10.1111/j.1444-0938.1998.tb06767.x
31. Lee SW. Regression analysis for continuous independent variables in medical research: statistical standard and guideline of Life Cycle Committee. Life Cycle. 2022;2. doi:10.54724/lc.2022.e3
32. Atukunda I, Lusobya RC, Ali SH, et al. Prevalence, pattern and factors associated with ocular disorders in small-scale welders in Katwe, Kampala. BMC Ophthalmol. 2019;19(1):1–8. doi:10.1186/s12886-019-1150-x
33. Lombardi DA, Verma SK, Brennan MJ, Perry MJ. Factors influencing worker use of personal protective eyewear. Accid Anal Prev. 2009;41(4):755–762. doi:10.1016/j.aap.2009.03.017
34. Prabhu M, Rokhade R, Chandra KP, Kakhandaki A. A study of awareness and use of personal protective eyewear among welders in a tier 2 city in South India. Indian J Clin Exp Ophthalmol. 2017;3(3):356–360.
35. C-K H, Yen Y-L, Chang C-H, et al. Case-control study on the prevention of occupational eye injuries. Kaohsiung J Med Sci. 2008;24(1):10–16. doi:10.1016/S1607-551X(08)70067-6
36. Mary CC, Anyalewechi NE, Chukwudi EE, et al. Knowledge, attitude and use of eye protectors by welders in a rural community of Imo State, Nigeria. Int J Health Sci Res. 2020;10:225–235.
37. Limbu B, Moore G, Marvasti AH, et al. Work related ocular injury: Nepal. Nepal J Ophthalmol. 2018;10(1):47–56. doi:10.3126/nepjoph.v10i1.21689
38. Sabitu K, Iliyasu Z, Dauda M. Awareness of occupational hazards and use of safety measures amongst welders in northern Nigeria. Ann Afr Med. 2009;8(1):46–51. doi:10.4103/1596-3519.55764
39. Budhathoki SS, Singh SB, Sagtani RA, et al. Awareness of occupational hazards and use of safety measures among welders: a cross-sectional study from eastern Nepal. BMJ Open. 2014;4(6):e004646. doi:10.1136/bmjopen-2013-004646
40. Zakrzewski H, Chung H, Sanders E, et al. Evaluation of occupational ocular trauma: are we doing enough to promote eye safety in the workplace? Can J Ophthalmol. 2017;52(4):338–342. doi:10.1016/j.jcjo.2016.11.034
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
