Back to Journals » International Journal of Nephrology and Renovascular Disease » Volume 16
Low-Intensity Extracorporeal Shockwave Therapy (LI-ESWT) in Renal Diseases: A Review of Animal and Human Studies
Authors Skov-Jeppesen SM, Petersen NA, Yderstraede KB, Jensen BL, Bistrup C , Lund L
Received 8 September 2022
Accepted for publication 25 January 2023
Published 6 February 2023 Volume 2023:16 Pages 31—42
DOI https://doi.org/10.2147/IJNRD.S389219
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Pravin Singhal
Sune Moeller Skov-Jeppesen,1,2 Nicky Anúel Petersen,1 Knud Bonnet Yderstraede,2,3 Boye L Jensen,4 Claus Bistrup,2,5 Lars Lund1,2
1Department of Urology, Odense University Hospital, Odense, Denmark; 2Clinical Institute, University of Southern Denmark, Odense, Denmark; 3Department of Endocrinology, Odense University Hospital, Odense, Denmark; 4Department of Cardiovascular and Renal Research, Institute of Molecular Medicine, University of Southern Denmark, Odense, Denmark; 5Department of Nephrology, Odense University Hospital, Odense, Denmark
Correspondence: Sune Moeller Skov-Jeppesen, Department of Urology, Odense University Hospital, Sdr. Boulevard 29, Odense, 5000, Denmark, Tel +45 51210911, Fax +45 65411726, Email [email protected]
Background: Low-intensity extracorporeal shockwave therapy (LI-ESWT) has been suggested as a treatment for vascular diseases such as ischemic heart disease, diabetic foot ulcers, and erectile dysfunction. Primarily, LI-ESWT is known for its ability to stimulate angiogenesis and activation of stem cells in target tissues. Application of LI-ESWT in chronic progressive renal diseases is a novel area. The aim of the present review was to summarize available data on the effects of LI-ESWT used in the setting of renal diseases.
Methods: We systematically searched PubMed, Medline, and Embase databases for relevant studies. Our review included the results from preclinical animal experiments and clinical research.
Results: Eleven animal studies and one clinical study were included in the review. In the animal studies, LI-ESWT was used for the treatment of hypertensive nephropathy (n=1), diabetic nephropathy (n=1), or various types of ischemic renal injury (ie, artery occlusion, reperfusion injury) (n=9). The clinical study was conducted in a single-arm cohort as a Phase 1 study with patients having diabetic nephropathy. In animal studies, the application of LI-ESWT was associated with several effects: LI-ESWT led to increased VEGF and endothelial cell proliferation and improved vascularity and perfusion of the kidney tissue. LI-ESWT reduced renal inflammation and fibrosis. LI-ESWT caused only mild side effects in the clinical study, and, similarly, there were no signs of kidney injury after LI-ESWT in the animal studies.
Conclusion: LI-ESWT, as a non-invasive treatment, reduces the pathological manifestations (inflammation, capillary rarefaction, fibrosis, decreased perfusion) associated with certain types of renal disease. The efficacy of renal LI-ESWT needs to be confirmed in randomized clinical trials.
Keywords: review, kidney disease, extracorporeal shockwave therapy, ESWT
Background
Low-intensity extracorporeal shockwave therapy (LI-ESWT) is a novel treatment method suggested to stimulate angiogenesis and tissue regeneration in target organs. LI-ESWT is defined as shockwave therapy applied with energy flux density up to 0.35 mJ/mm2, which is significantly lower than shockwave lithotripsy (ESWL, typically at energy >0.75 mJ/mm2). In coronary heart disease and peripheral artery disease, LI-ESWT has been applied to increase perfusion and reduce ischemic symptoms.1,2 Additionally, LI-ESWT promotes healing of chronic diabetic foot ulcers3 and may be an effective treatment for patients with vasculogenic type of erectile dysfunction.4
Shockwaves constitute a type of acoustic waves characterized by a high, short-lasting peak pressure followed by a mild, tensile phase. In biological tissues, the shockwaves induce shear stress upon cell membranes, cytoskeleton, and extracellular matrix. The effect is mediated through the process of mechanotransduction meaning that the physical pressure stimulus is converted into a biological response via sensory molecules on the cell surface.5 In the molecular scale, vascular endothelial growth factor (VEGF) and nitric oxide (NO) are released from endothelial cells in response to LI-ESWT which in turn increases endothelial cell growth, vascular relaxation, and angiogenesis.6–8
Chronic kidney disease (CKD) is characterized by irreversible pathological lesions of the kidney tissue including vascular rarefaction, interstitial fibrosis, and tubular atrophy. In particular, diabetic nephropathy and hypertensive nephropathy are major culprits leading to end-stage kidney disease that is associated with microvascular degeneration and glomerulosclerosis. Other causes that might promote CKD include acute transient renal ischemia, toxic insults/effects, and autoimmune disorders. LI-ESWT could prove as a feasible method to ameliorate the chronic manifestations of renal diseases and preserve kidney function.
The aim of the present systematic review was to assemble current data on LI-ESWT as a potential treatment option for renal diseases. Accordingly, our objective was to systematically collect and summarize existing literature on LI-ESWT treatment for renal diseases. We included both animal and human research data. We excluded studies where shockwave therapy was used in the setting of urological stone disease and cell culture/ex vivo studies.
Methods
We performed a systematic database search for studies on LI-ESWT in combination with renal disease. Both human and animal studies were included. We searched PubMed, Medline, and Embase databases. The following search string was used in PubMed: (shockwave or shockwaves or shock waves or shock wave or ESWT or SWT) and (kidney or kidneys or renal). We used the same terms for search build in the other databases. The databases were searched on August 29, 2022. No restrictions on publication year or language were applied. The search yielded a total of 14,894 articles which was reduced to 7043 different articles after removal of duplicates. Duplicates were identified in EndNote based on similarity between author, title, and year of publication. Finally, the 7043 articles were screened for eligibility by two researchers (S.M.S.J and N.A.P) based on title, abstract, and full-text reading (Flowchart, Figure 1). The two researchers worked independently screening the articles before meeting to decide which studies to include in the review. A third researcher (L.L) would take the decision on study eligibility in case of disagreement between the first two researchers. Furthermore, the literature lists of the eligible studies were screened for additional studies. Inclusion and exclusion criteria for the studies selected for this review are listed in Box 1. LI-ESWT was defined as shockwave therapy carried out with focal zone energy flux below 0.35 mJ/mm2 (low to medium energy level) in accordance with the guidelines provided by the International Society for Medical Shockwave Treatment (ISMST).9 Risk of bias was not assessed for the included studies since no randomized clinical studies were identified.
 |
Box 1 Eligibility Criteria |
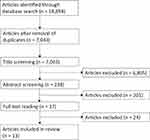 |
Figure 1 Flowchart. |
We screened the WHO International Clinical Trials Registry Platform, ClinicalTrials.gov, the EU Clinical Trials Register, and the Australian New Zealand Clinical Trials Registry for further studies. The registries were searched using the same terms as in our database search.
Results
We identified a total of 12 eligible studies. Of these, 11 were animal studies10–20 and one was a clinical study.21,22
We found two preclinical animal studies23,24 and two clinical studies25,26 that were non-eligible since they were only published in abstract format. Three unpublished clinical studies were located at ClinicalTrials.gov (Identifier: NCT03914157) and WHO International Clinical Trials Registry Platform (Main ID: JPRN-UMIN000030768 and JPRN-UMIN000030448). One unpublished clinical study was located at ClinicalTrials.gov (Identifier: NCT03445247), but the study had been suspended due to a lack of participants. The methods and results of the studies published in abstract format are not further described in the present review, but an overview is included in an Additional File (see Additional Tables 1 and 2).
Animal Studies
Six of the animal studies used rats10,12,15–17,20 and five studies used pigs.11,13,14,18,19 In the animal studies, different types of renal disease were induced by either Nω-nitro-
Clinical Studies
Skov-Jeppesen et al21,22 published a safety report from a clinical study that included measurement of renal functional outcomes after LI-ESWT in patients with diabetic nephropathy. Other studies have reported data only in abstract format. The study by Skov-Jeppesen et al21,22 was a single-arm cohort study with relatively small study population including 28 patients. In this study, LI-ESWT was applied with a Storz Modulith SLX-2 device and both kidneys were treated on upper, middle, and lower zone with 1000 shocks/zone and energy 0.265 mJ/mm2.21
The design and methods of the animal and clinical studies are summarized in Table 1.
 |
Table 1 Design and Methods |
Molecular Effects
The protein expression of VEGF was higher in the kidney tissue after LI-ESWT in the studies by Zhang et al,11 Sung et al,16 Hsiao et al,15 and Zhao et al18 However, there was no change in VEGF mRNA expression after LI-ESWT in the study by Caron et al10 Chen et al14 found that the protein expression of VEGF was unaffected by LI-ESWT. In the study by Yoshida et al,17 the expression of VEGF mRNA was upregulated in the contralateral, non-treatment kidney. In relation to nitric oxide synthase (NOS) expression, the studies by Zhang et al 2016,11 Sung et al,16 and Zhao et al18 found higher endothelial NOS (eNOS) expression after LI-ESWT. On the other hand, in the studies by Caron et al10 and Yoshida et al,17 there was no significant effect on eNOS expression. Xue et al12 found lower levels of inducible NOS (iNOS) after LI-ESWT. Chen et al19 found that there was no effect of LI-ESWT monotherapy on the expression of eNOS but combination therapy with mesenchymal stem cells caused an upregulation of eNOS. Skov-Jeppesen et al22 reported that nitric oxide metabolites in urine tended to be higher in patients with diabetic nephropathy after treatment with LI-ESWT, but the results were not statistically significant. Furthermore, there seemed to be a transient decrease in VEGF 1 month after LI-ESWT in the clinical study by Skov-Jeppesen et al but the evidence was not strong (p=0.056).22 Other findings included lower levels of inflammatory and apoptotic markers after LI-ESWT15,16,19 as well as less oxidative stress.12,15,16,19 A few studies also investigated the mechanotransduction signal of LI-ESWT suggesting that the shock wave pressure stimulus was mediated through membrane proteins such as focal adhesion kinase (FAK) and beta 1-integrin.11,14 Furthermore, LI-ESWT seemed to downregulate TGF-beta expression in the studies by Zhang et al 2016,11 Sung et al,16 and Hsiao et al15 This could indicate that LI-ESWT counteracts the initiation of fibrosis. Stromal cell-derived factor-1 (SDF-1), a chemoattractant for endothelial progenitor cells, was higher after LI-ESWT in the setting of renal ischemia,11,18,20 diabetic nephropathy,15 and proteinuric CKD16 but not in hypertensive renal disease.10 In summary, available data do not show consistent changes in VEGF and NO-synthase in kidney tissue subjected to LI-ESWT.
Cellular and Histological Effects
A common finding was lower interstitial fibrosis after LI-ESWT as demonstrated by trichrome staining at 4 weeks,11,13,18,19 7 weeks,14 and 60 days.16 Nonetheless, two studies found no effect of LI-ESWT on the degree of renal fibrosis at 4 days17 and 4 weeks10 after the treatment. LI-ESWT promoted endothelial cell proliferation16,20 and increased renal vascularity.11,14 On microCT scan, Zhang et al11 and Chen et al19 demonstrated that the density of small renal vessels recovered after LI-ESWT. Three studies14,18,19 found higher number of peritubular capillaries after LI-ESWT. Other studies reported ameliorated vascular and glomerular lesions after LI-ESWT15 as well as lymphangiogenesis.17 In diabetic rats, LI-ESWT promoted regeneration of glomerular podocyte cells.15 Intriguingly, the homing of circulating endothelial progenitor cells to kidney tissue was enhanced by LI-ESWT.16,18,20 Also, LI-ESWT improved inflammation as indicated by lower infiltration of macrophages.14,15 However, LI-ESWT did not affect the number of macrophages after ischemia-reperfusion injury in the study by Yoshida et al17 In summary, available data show stimulatory effects of LI-ESWT on kidney microvessel density and growth.
Renal Functional Effects
The effect of LI-ESWT on GFR was assessed directly in four of the animal studies11,14,18,19 and in the human study.21 Four studies11,14,18,19 demonstrated that single kidney GFR was significantly higher in pigs 4 weeks after LI-ESWT administration as evidenced by multidetector computed tomography (MDCT). In the clinical study,21 GFR was measured in patients by means of chrome-EDTA clearance. After six sessions of LI-ESWT, GFR was stable in patients with diabetic nephropathy up to 6 months.21,22 In five of the animal studies, LI-ESWT lowered the plasma concentration of creatinine, BUN, or cystatin C11,12,16,17,20 but there was no significant effect on these parameters in the studies by Caron et al10 and Chen et al14 In the animal studies, LI-ESWT improved tissue oxygenation as demonstrated by blood oxygen-level dependent magnetic resonance imaging (BOLD MRI)11,14,19 as well as renal arterial flow.16,18,19 Two studies, however, did not demonstrate a significant effect of LI-ESWT on renal arterial blood flow.11,14 Importantly, LI-ESWT ameliorated albuminuria and proteinuria in preclinical settings. In rats, proteinuria was lower 60 days after LI-ESWT in proteinuric CKD,16 and albuminuria was lower than 6 weeks after LI-ESWT in diabetic nephropathy.15 In pigs with renal ischemia, Zhao et al18 demonstrated that the urinary protein excretion was lowered at 4 weeks after LI-ESWT. However, the studies by Caron et al10 and Zhang et al11 did not corroborate this. In human diabetic nephropathy, there were no significant changes in median albuminuria 6 months after LI-ESWT.21,22 Other functional changes after LI-ESWT included improved arterial blood pressure11,13,15,18 which was, however, not confirmed in an animal model of hypertensive nephropathy10 and a model of renal ischemia.19 In the human study, ambulatory blood pressure was unchanged after LI-ESWT.21,22 In pigs treated with LI-ESWT, Zhao et al18 demonstrated that the renal blood flow was significantly higher in response to a systemic dose of acetylcholine which could indicate an improvement of the renal microvascular endothelial function. Nonetheless, LI-ESWT monotherapy did not enhance the vascular response to acetylcholine in pigs in the study by Chen et al18 In summary, LI-ESWT is neutral or slightly beneficial on GFR and albuminuria, but material is scarce and follow-up time is limited.
Safety
LI-ESWT was applied to a healthy control group in four of the animal studies allowing the study of side effects to the treatment. In rat studies, no histological changes were seen after application of LI-ESWT to healthy animals.10,12,20 LI-ESWT did not adversely affect urinary protein excretion, arterial blood pressure, or renal function.10,20 Furthermore, plasma levels of NGAL and KIM-1 remained unchanged at 24 hours and 1 week after LI-ESWT.12 In pigs, a single session of LI-ESWT caused no micro- or macroscopic haematuria and no signs of haemorrhage or tubular injury.11 Furthermore, urinary NGAL and protein levels and renal function were stable.11 There were no differences found between healthy pigs treated with six sessions of LI-ESWT and healthy pigs that received no intervention.11,18 In the remaining animal studies,13,14,16,17,19 LI-ESWT did not negatively affect any of the measured or observed variables. Xue et al12 found lower iNOS after LI-ESWT which can be interpreted as reduced oxidative stress/macrophage activation and therefore not a negative finding. In the published study with data from patients with diabetes, there was transient macroscopic haematuria in six out of 28 patients after LI-ESWT.22 Treatment with LI-ESWT caused short-lasting flank tenderness in the majority of the patients, and ultrasound scanning revealed no signs of renal hematoma.21,22 There were no correlations between the presence of haematuria and negative functional outcomes in the patients.21,22 During the intervention, the patients experienced LI-ESWT as a stinging sensation, but pain was only reported in 1/14 patients.21 Importantly, in patients with diabetic nephropathy, LI-ESWT had no negative impact on urinary kidney injury markers (KIM-1, calbindin, clusterin, osteoactivin, trefoil factor-3).22
The results of each study are listed in Table 2. Furthermore, Table 3 shows selected molecular, cellular and functional effects of renal LI-ESWT treatment.
 |
Table 2 Results |
 |
Table 3 Selected Effects of LI-ESWT |
Discussion
Shockwave therapy was invented originally for renal lithotripsy almost 40 years ago.27 The application of LI-ESWT as a treatment for kidney parenchymal diseases is a novel therapeutic approach, and data in this field are limited. The earliest study we identified was published in 2016, and, since then, nine additional preclinical animal studies and one human study have been published with renal outcome as primary effect parameter.
Taken together, data from animal studies vary from neutral to positive findings that range from improved GFR, attenuated proteinuria and inflammation, improved renal blood flow, and lower blood pressure. Variation between the results can be ascribed to different models of renal disease, different species, and different therapeutic protocols. In light of the non-invasive intervention, there is a need for functional and tissue data from human intervention trials.
Previous studies, focusing on other organs than kidneys, showed that the effect of LI-ESWT was mediated through different receptors and proteins associated with cell surfaces, including specific mechanosensory complexes, toll-like receptors, and ATP receptors that were activated by ATP released from cytoplasm in response to LI-ESWT.28–30 This way, LI-ESWT acts as a physical stimulus that potentially influences several types of cell surface receptors. The beneficial downstream signalling effects of LI-ESWT involve local angiogenesis as well as anti-inflammatory processes summarizing into reduced fibrosis. At the level of signalling pathways, LI-ESWT upregulates VEGF and NO which act as trophic factors for endothelium and stimulation of angiogenesis. VEGF and VEGF receptor activation were previously shown to be higher after LI-ESWT in heart, skeletal muscle, skin, and penile tissue.31–35 The activation of angiogenesis by LI-ESWT leads to improved tissue perfusion and oxygenation as shown clinically in ischemic myocardium and diabetic foot ulcers.36–38 Also, treatment with ESWL has previously been associated with increased levels of plasma nitrite and cyclic 3’, 5’-guanosine monophosphate (cGMP) suggesting that shockwaves stimulate the NO-cGMP signaling pathway.39–41
Histologically, LI-ESWT may promote tissue remodelling through activation of M2 reparative macrophages and inhibition of M1 inflammatory macrophages.42 In severe burn wounds and myocardial infarction, treatment with LI-ESWT suppressed pro-inflammatory cytokines and neutrophil and macrophage infiltration.43,44 LI-ESWT ameliorated TGF-beta expression and tissue collagen and fibrocyte content as demonstrated in ischemic heart diseases.44–46 Interestingly, a few studies indicated a synergistic effect between administration of endothelial progenitor cells and LI-ESWT to induce angiogenesis and improved tissue viability.47,48 It is likely that LI-ESWT upregulates the local production of SDF-1 which may attract circulating endothelial progenitor cells.47,49 This way, LI-ESWT treatment could provide a method to enhance cell-based therapies.
Only a few studies have tested the dose–response relationship of LI-ESWT. The treatment can be administered with lower or higher energy within the spectrum from 0.01 to 0.35 mJ/mm2. In the hind limb of rats, tissue oxygen tension was significantly higher after application with energy at 0.30 mJ/mm2 compared to energy at 0.10 mJ/mm2.50 On the other hand, an inappropriate high number of shockwaves might induce tissue necrosis.51 Furthermore, repetitive sessions of LI-ESWT have been found to negatively affect wound healing.52 With regard to the optimal timing of treatment, application of LI-ESWT to acutely injured skin showed there was no difference whether treatment was applied before or after ischemic injury.53 Hypothetically, another useful application of LI-ESWT could be a preconditioning treatment in relation to surgical procedures that induce renal ischemia, ie, partial nephrectomy or renal transplantation. Furthermore, LI-ESWT can be applied as either focused or radial therapy. Radial shockwaves differ from focused shockwaves in that they propagate in the body as spherical waves and do not focus the energy in a small, targeted area.5 In renal diseases, LI-ESWT was carried out as focused therapy in all of the studies and the potential of radial LI-ESWT is unknown.
In the present review of data from studies with primary renal outcome, LI-ESWT elicited beneficial effects as found in other organs, but some of the findings were not consistent between the studies with different renal disease models. In particular, Caron et al10 demonstrated no positive effects of LI-ESWT treatment. Of note, their study was based on rats with hypertensive renal disease induced by administration of L-NAME. The majority of the animal studies were based on renal artery stenosis/clamping and thus studied ischemia recovery and reperfusion injury. However, Hsiao et al15 based their renal disease model on streptozotocin injection to induce type 1 diabetic nephropathy and found positive effects of renal LI-ESWT. In relation to the method of LI-ESWT administration, we identified no simple differences that could explain the discrepancy between the outcomes. LI-ESWT was administered in the same way through all of the porcine studies, and the reported outcomes in these studies were overall positive and constitute the only data in large animals. However, only one type of renal disease model (ischemic renal disease) was used in the porcine studies. It remains unclear whether the protocol for LI-ESWT implemented in the porcine studies is also efficient in other types of renal diseases. In general, LI-ESWT was applied with energy densities in the lower end of the spectrum in the animal studies (0.09–0.13 mJ/mm2). Conversely, patients included in the clinical study were treated with relatively high energy levels at 0.265 mJ/mm2. There were no clear associations between the frequency or number of sessions of LI-ESWT and the outcomes. The most frequently used protocol for LI-ESWT was twice per week for 3 weeks for a total of six sessions but ranged from one session up to 12 sessions in total. A consistent finding across the preclinical studies was that there was no evidence of injury or damage to the kidneys.
The single human study was conducted as phase 1 study in order to first establish the clinical safety of LI-ESWT in renal parenchymal disease.21,22 In this study, transient macroscopic haematuria was observed in a minor part of the patients. Flank tenderness was more commonly reported after bilateral LI-ESWT. These side effects are well-known also from ESWL. The side effects did not require any intervention or treatment and were short-lasting after LI-ESWT. There were no reported signs of renal hematoma or negative functional outcomes (drop in GFR, hypertension, or albuminuria) related to LI-ESWT, and further clinical research is encouraged. In particular, future clinical studies should test the dose–response relationship of LI-ESWT considering the positive results demonstrated in animal studies at relatively low energy settings. Moreover, the optimal frequency of LI-ESWT and whether intervention can be repeated should be clarified.
Conclusions
LI-ESWT has shown several beneficial outcomes in ischemic cardiac disease, erectile dysfunction, and skin injury. Data on the effect in renal parenchymal diseases are scarce. In preclinical animal studies, LI-ESWT showed no adverse effects. In some cases, significant improvement was found in VEGF synthesis and renal vascularity with reduced renal fibrosis and improved renal function. There was a large heterogeneity between the studies with regard to the administration of Li-ESWT (intensity, frequency) and the type of renal disease. In a clinical setting, LI-ESWT has proven as a safe treatment in a small study population of patients with diabetic nephropathy. Future randomized controlled clinical trials are needed to determine the efficacy of LI-ESWT in renal diseases.
Abbreviations
LI-ESWT, low-intensity extracorporeal shockwave therapy; VEGF, vascular endothelial growth factor; NO, nitric oxide; eNOS, endothelial nitric oxide synthase; GFR, glomerular filtration rate; SDF-1, stromal cell-derived factor-1; BOLD MRI, blood oxygen-level-dependent magnetic resonance imaging.
Data Sharing Statement
All articles included in this systematic review are referenced in the manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas. All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Burneikaite G, Shkolnik E, Celutkiene J, et al. Cardiac shock-wave therapy in the treatment of coronary artery disease: systematic review and meta-analysis. Cardiovasc Ultrasound. 2017;15(1):11. doi:10.1186/s12947-017-0102-y
2. Cayton T, Harwood A, Smith GE, Chetter I. A systematic review of extracorporeal shockwave therapy as a novel treatment for intermittent claudication. Ann Vasc Surg. 2016;35:226–233. doi:10.1016/j.avsg.2016.02.017
3. Huang Q, Yan P, Xiong H, et al. Extracorporeal shock wave therapy for treating foot ulcers in adults with type 1 and type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Can J Diabetes. 2019;2019:1.
4. Sokolakis I, Hatzichristodoulou G. Clinical studies on low intensity extracorporeal shockwave therapy for erectile dysfunction: a systematic review and meta-analysis of randomised controlled trials. Int J Impot Res. 2019;31(3):177–194. doi:10.1038/s41443-019-0117-z
5. d’Agostino MC, Craig K, Tibalt E, Respizzi S. Shock wave as biological therapeutic tool: from mechanical stimulation to recovery and healing, through mechanotransduction. Int J Surg. 2015;24(PtB):147–153. doi:10.1016/j.ijsu.2015.11.030
6. Hatanaka K, Ito K, Shindo T, et al. Molecular mechanisms of the angiogenic effects of low-energy shock wave therapy: roles of mechanotransduction. Am J Physiol Cell Physiol. 2016;311(3):C378–85. doi:10.1152/ajpcell.00152.2016
7. Peng YZ, Zheng K, Yang P, et al. Shock wave treatment enhances endothelial proliferation via autocrine vascular endothelial growth factor. Genet Mol Res. 2015;14(4):19203–19210. doi:10.4238/2015.December.29.30
8. Yan X, Zeng B, Chai Y, Luo C, Li X. Improvement of blood flow, expression of nitric oxide, and vascular endothelial growth factor by low-energy shockwave therapy in random-pattern skin flap model. Ann Plast Surg. 2008;61(6):646–653. doi:10.1097/SAP.0b013e318172ba1f
9. DIGEST. Guidelines for extracorporeal shock wave therapy. The International Society for Medical Shockwave Treatment; 2019. Available from: https://www.shockwavetherapy.org/fileadmin/user_upload/ISMST_Guidelines.pdf:.
10. Caron J, Michel PA, Dussaule JC, Chatziantoniou C, Ronco P, Boffa JJ. Extracorporeal shock wave therapy does not improve hypertensive nephropathy. Physiol Rep. 2016;4:11. doi:10.14814/phy2.12699
11. Zhang X, Krier JD, Amador Carrascal C, et al. Low-energy shockwave therapy improves ischemic kidney microcirculation. J Am Soc Nephrol. 2016;27(12):3715–3724. doi:10.1681/ASN.2015060704
12. Xue Y, Xu Z, Chen H, Gan W, Chong T. Low-energy shock wave preconditioning reduces renal ischemic reperfusion injury caused by renal artery occlusion. Acta Cir Bras. 2017;32(7):550–558. doi:10.1590/s0102-865020170070000006
13. Zhang X, Zhu X, Ferguson CM, et al. Magnetic resonance elastography can monitor changes in medullary stiffness in response to treatment in the swine ischemic kidney. MAGMA. 2018;31(3):375–382. doi:10.1007/s10334-017-0671-7
14. Chen XJ, Zhang X, Jiang K, et al. Improved renal outcomes after revascularization of the stenotic renal artery in pigs by prior treatment with low-energy extracorporeal shockwave therapy. J Hypertens. 2019;37:2074–2082. doi:10.1097/HJH.0000000000002158
15. Hsiao CC, Huang WH, Cheng KH, Lee CT. Low-energy extracorporeal shock wave therapy ameliorates kidney function in diabetic nephropathy. Oxid Med Cell Longev. 2019;2019:8259645. doi:10.1155/2019/8259645
16. Sung PH, Chen KH, Li YC, Chiang JY, Lee MS, Yip HK. Sitagliptin and shock wave-supported peripheral blood derived endothelial progenitor cell therapy effectively preserves residual renal function in chronic kidney disease in rat-role of dipeptidyl peptidase 4 inhibition. Biomed Pharmacother. 2019;111:1088–1102. doi:10.1016/j.biopha.2019.01.025
17. Yoshida M, Nakamichi T, Mori T, Ito K, Shimokawa H, Ito S. Low-energy extracorporeal shock wave ameliorates ischemic acute kidney injury in rats. Clin Exp Nephrol. 2019;23(5):597–605. doi:10.1007/s10157-019-01689-7
18. Zhao Y, Santelli A, Zhu XY, et al. Low-energy shockwave treatment promotes endothelial progenitor cell homing to the stenotic pig kidney. Cell Transplant. 2020;29:963689720917342. doi:10.1177/0963689720917342
19. Chen XJ, Zhang X, Jiang K, et al. Adjunctive mesenchymal stem/stromal cells augment microvascular function in poststenotic kidneys treated with low-energy shockwave therapy. J Cell Physiol. 2020;235:9806–9818. doi:10.1002/jcp.29794
20. Liu J, Dou Q, Zhou C, et al. Low-energy shock wave pretreatment recruit circulating endothelial progenitor cells to attenuate renal ischaemia reperfusion injury. J Cell Mol Med. 2020;24(18):10589–10603. doi:10.1111/jcmm.15678
21. Skov-Jeppesen SM, Yderstraede KB, Bistrup C, et al. Low-intensity shockwave therapy in the treatment of diabetic nephropathy: a prospective Phase 1 study. Nephrol Dial Transplant. 2018;2018:1.
22. Skov-Jeppesen SM, Yderstraede KB, Jensen BL, Bistrup C, Hanna M, Lund L. Low-Intensity Shockwave Therapy (LI-ESWT) in diabetic kidney disease: results from an open-label interventional clinical trial. Int J Nephrol Renovasc Dis. 2021;14:255–266. doi:10.2147/IJNRD.S315143
23. Michel PA, Bonin P, Bige N, et al. Effects of shock wave therapy in chronic kidney diseases. Nephron Physiol. 2011;1:p12.
24. Hanna M, Pedersen D, Lund M, Marcussen N, Lund L. Low energy ESWT, a novel treatment for diabetic nephropathy (animal study). J Endourol. 2012;1:A6.
25. Lundrup RN, Skov-Jeppesen SM, Bistrup C, Jensen B, Yderstraede K, Lund L. Safety and effect of low-energy extracorporeal shockwave therapy (ESWT) on the renal allograft in transplant recipients-preliminary results. Scand J Urol. 2019;53(Supplement 221):4.
26. Aleksandre B, Andro D, Milad H, et al. Low intensity shock waves in the treatment of diabetic nephropathy: prospective, phase 1 study, Georgian arm. Eur Urol Suppl. 2019;18(12):e3635–e6. doi:10.1016/S1569-9056(19)35038-9
27. Chaussy C, Brendel W, Schmiedt E. Extracorporeally induced destruction of kidney stones by shock waves. Lancet. 1980;2(8207):1265–1268. doi:10.1016/S0140-6736(80)92335-1
28. Ha CH, Kim S, Chung J, An SH, Kwon K. Extracorporeal shock wave stimulates expression of the angiogenic genes via mechanosensory complex in endothelial cells: mimetic effect of fluid shear stress in endothelial cells. Int J Cardiol. 2013;168(4):4168–4177. doi:10.1016/j.ijcard.2013.07.112
29. Holfeld J, Tepekoylu C, Reissig C, et al. Toll-like receptor 3 signalling mediates angiogenic response upon shock wave treatment of ischaemic muscle. Cardiovasc Res. 2016;109(2):331–343. doi:10.1093/cvr/cvv272
30. Weihs AM, Fuchs C, Teuschl AH, et al. Shock wave treatment enhances cell proliferation and improves wound healing by ATP release-coupled extracellular signal-regulated kinase (ERK) activation. J Biol Chem. 2014;289(39):27090–27104. doi:10.1074/jbc.M114.580936
31. Holfeld J, Zimpfer D, Albrecht-Schgoer K, et al. Epicardial shock-wave therapy improves ventricular function in a porcine model of ischaemic heart disease. J Tissue Eng Regen Med. 2014;2014:1.
32. Cai HY, Li L, Guo T, et al. Cardiac shockwave therapy improves myocardial function in patients with refractory coronary artery disease by promoting VEGF and IL-8 secretion to mediate the proliferation of endothelial progenitor cells. Exp Ther Med. 2015;10(6):2410–2416. doi:10.3892/etm.2015.2820
33. Jeong HC, Jeon SH, Qun ZG, et al. Effects of next-generation low-energy extracorporeal shockwave therapy on erectile dysfunction in an animal model of diabetes. World J Mens Health. 2017;35(3):186–195. doi:10.5534/wjmh.17024
34. Wang CJ, Ko JY, Kuo YR, Yang YJ. Molecular changes in diabetic foot ulcers. Diabetes Res Clin Pract. 2011;94(1):105–110. doi:10.1016/j.diabres.2011.06.016
35. Holfeld J, Tepekoylu C, Blunder S, et al. Low energy shock wave therapy induces angiogenesis in acute hind-limb ischemia via VEGF receptor 2 phosphorylation. PLoS One. 2014;9(8):e103982. doi:10.1371/journal.pone.0103982
36. Kaller M, Faber L, Bogunovic N, Horstkotte D, Burchert W, Lindner O. Cardiac shock wave therapy and myocardial perfusion in severe coronary artery disease. Clin Res Cardiol. 2015;104(10):843–849. doi:10.1007/s00392-015-0853-0
37. Wang CJ, Wu RW, Yang YJ. Treatment of diabetic foot ulcers: a comparative study of extracorporeal shockwave therapy and hyperbaric oxygen therapy. Diabetes Res Clin Pract. 2011;92(2):187–193. doi:10.1016/j.diabres.2011.01.019
38. Jeppesen SM, Yderstraede KB, Rasmussen BS, Hanna M, Lund L. Extracorporeal shockwave therapy in the treatment of chronic diabetic foot ulcers: a prospective randomised trial. J Wound Care. 2016;25(11):641–649. doi:10.12968/jowc.2016.25.11.641
39. Park JK, Cui Y, Kim MK, et al. Effects of extracorporeal shock wave lithotripsy on plasma levels of nitric oxide and cyclic nucleotides in human subjects. J Urol. 2002;168(1):38–42. doi:10.1016/S0022-5347(05)64827-6
40. Sarica K, Balat A, Erbagci A, Cekmen M, Yurekli M, Yagci F. Effects of shock wave lithotripsy on plasma and urinary levels of nitrite and adrenomedullin. Urol Res. 2003;31(5):347–351. doi:10.1007/s00240-003-0351-0
41. Aksoy H, Aksoy Y, Turhan H, Keleş S, Ziypak T, Ozbey I. The effect of shock wave lithotripsy on nitric oxide and malondialdehyde levels in plasma and urine samples. Cell Biochem Funct. 2007;25(5):533–536. doi:10.1002/cbf.1349
42. Sukubo NG, Tibalt E, Respizzi S, Locati M, d’Agostino MC. Effect of shock waves on macrophages: a possible role in tissue regeneration and remodeling. Int J Surg. 2015;24:124–130. doi:10.1016/j.ijsu.2015.07.719
43. Davis TA, Stojadinovic A, Anam K, et al. Extracorporeal shock wave therapy suppresses the early proinflammatory immune response to a severe cutaneous burn injury. Int Wound J. 2009;6(1):11–21. doi:10.1111/j.1742-481X.2008.00540.x
44. Abe Y, Ito K, Hao K, et al. Extracorporeal low-energy shock-wave therapy exerts anti-inflammatory effects in a rat model of acute myocardial infarction. Circ J. 2014;2014:1.
45. Fu M, Sun CK, Lin YC, et al. Extracorporeal shock wave therapy reverses ischemia-related left ventricular dysfunction and remodeling: molecular-cellular and functional assessment. PLoS One. 2011;6(9):e24342. doi:10.1371/journal.pone.0024342
46. Lei PP, Tao SM, Shuai Q, et al. Extracorporeal cardiac shock wave therapy ameliorates myocardial fibrosis by decreasing the amount of fibrocytes after acute myocardial infarction in pigs. Coron Artery Dis. 2013;24(6):509–515. doi:10.1097/MCA.0b013e3283640ec7
47. Aicher A, Heeschen C, Sasaki K, Urbich C, Zeiher AM, Dimmeler S. Low-energy shock wave for enhancing recruitment of endothelial progenitor cells: a new modality to increase efficacy of cell therapy in chronic hind limb ischemia. Circulation. 2006;114(25):2823–2830. doi:10.1161/CIRCULATIONAHA.106.628623
48. Assmus B, Walter DH, Seeger FH, et al. Effect of shock wave-facilitated intracoronary cell therapy on LVEF in patients with chronic heart failure: the CELLWAVE randomized clinical trial. JAMA. 2013;309(15):1622–1631. doi:10.1001/jama.2013.3527
49. Gollmann-Tepekoylu C, Lobenwein D, Theurl M, et al. Shock wave therapy improves cardiac function in a model of chronic ischemic heart failure: evidence for a mechanism Involving VEGF signaling and the extracellular matrix. J Am Heart Assoc. 2018;7(20):e010025. doi:10.1161/JAHA.118.010025
50. Kraemer R, Sorg H, Forstmeier V, et al. Immediate dose-response effect of high-energy versus low-energy extracorporeal shock wave therapy on cutaneous microcirculation. Ultrasound Med Biol. 2016;42(12):2975–2982. doi:10.1016/j.ultrasmedbio.2016.08.010
51. Kamelger F, Oehlbauer M, Piza-Katzer H, Meirer R. Extracorporeal shock wave treatment in ischemic tissues: what is the appropriate number of shock wave impulses? J Reconstr Microsurg. 2010;26(2):117–121. doi:10.1055/s-0029-1243296
52. Zins SR, Amare MF, Tadaki DK, Elster EA, Davis TA. Comparative analysis of angiogenic gene expression in normal and impaired wound healing in diabetic mice: effects of extracorporeal shock wave therapy. Angiogenesis. 2010;13(4):293–304. doi:10.1007/s10456-010-9186-9
53. Mittermayr R, Hartinger J, Antonic V, et al. Extracorporeal shock wave therapy (ESWT) minimizes ischemic tissue necrosis irrespective of application time and promotes tissue revascularization by stimulating angiogenesis. Ann Surg. 2011;253(5):1024–1032. doi:10.1097/SLA.0b013e3182121d6e
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
