Back to Journals » Substance Abuse and Rehabilitation » Volume 15
Female Patients Show a Larger Reduction in Suicidal Ideation in Inpatient Addiction Treatment Than Male Patients: Results of a Single-Center Observational Study
Authors Grote V , Wagner T, Riedl D, Kautzky-Willer A, Fischer MJ, Scheibenbogen O, Musalek M
Received 9 January 2024
Accepted for publication 16 March 2024
Published 29 March 2024 Volume 2024:15 Pages 31—42
DOI https://doi.org/10.2147/SAR.S454436
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Rajendra D. Badgaiyan
Vincent Grote,1,* Tim Wagner,1,2,* David Riedl,1,3 Alexandra Kautzky-Willer,4 Michael J Fischer,1,5,6 Oliver Scheibenbogen,2 Michael Musalek7– 9
1Ludwig Boltzmann Institute for Rehabilitation Research, Ludwig Boltzmann Gesellschaft, Vienna, Austria; 2Anton Proksch Institute, Vienna, Austria; 3University Hospital of Psychiatry II, Medical University of Innsbruck, Innsbruck, Austria; 4Division of Endocrinology and Metabolism, Medical University of Vienna, Vienna, Austria; 5Vamed Rehabilitation Center Kitzbühel, Kitzbühel, Austria; 6Clinic for Rehabilitation Medicine, Hannover Medical School MHH, Hannover, Germany; 7Department of General Psychiatry, Sigmund Freud University, Vienna, Austria; 8Institute for Social Aesthetics and Mental Health, Sigmund Freud University, Vienna, Austria; 9Institute for Social Aesthetics and Mental Health, Sigmund Freud University, Berlin, Germany
*These authors contributed equally to this work
Correspondence: Vincent Grote; Oliver Scheibenbogen, Email [email protected]; [email protected]
Background: Substance use disorders (SUD) are prevalent disorders worldwide. Among other associated health problems, patients with SUD are at an increased risk of dying of suicide, with females displaying an even higher risk than males. Therefore, the aim of this study was to conduct a gender-sensitive evaluation of changes in suicidal ideation during multimodal inpatient treatment at a hospital facility specialized in treating addiction.
Methods: A total of 694 patients (68.2% male) completed routine assessment including suicidal ideation, abstinence confidence, impulsivity, emotion regulation, self-efficacy and autonomy and joy both before (T1) and at the end (T2) of treatment. Mean changes were evaluated with repeated measures MANOVAs.
Results: Before treatment, a total of n=127 (18.3%) of the respondents reported suicidal ideation, which was reduced to n=72 (10.4%) by the end of treatment. Among female patients, the change in reported suicidal ideation compared from T1 to T2 (21.7% vs 7.7%) was significantly higher than among male patients (T1: 16.7%%, T2: 11.6%; p=0.040). Generally, females reported worse symptoms scores and slightly higher numbers of suicidal thoughts at baseline (effect sizes ranging from η²=.008 – 0.044). While both genders significantly profited from the treatment, female patients generally showed larger improvements than male.
Discussion: Our study underscores the beneficial effect of addiction-specialized inpatient treatment on suicidal ideation. Additionally, we found a substantial gender effect: while female patients generally were more distressed before treatment, they also reported higher symptom reduction during the treatment. This result highlights the need to perform more gender-sensitive research and develop more gender-sensitive treatment programs.
Keywords: addiction, inpatient therapy, alcohol, drugs, gender medicine
Introduction
With an estimated 3.8% of all global deaths and 4.6% of global DALYs (disability-adjusted life-years), the health impact of harmful alcohol use is substantial.1 In Austria, 5% of the population over the age of 15 is addicted to alcohol, and a further 12% consume alcohol to the extent that is harmful to health.2 However, substance use disorders (SUD) are usually only the tip of the iceberg. Beneath the surface, numerous comorbid disorders such as anxiety disorders,3 personality disorders,4,5 trauma sequelae,6 externalizing disorders7,8 and affective disorders9,10 can be found. The prevalence rates of comorbid disorders in dependence disorders vary considerably, with affective disorders being the most common.9,11–13
Problematic drinking as well as drug use are considered to be significant predictors of suicidal ideation14 and suicidal behavior, based on the results of many studies.15–17 Wilcox, Conner and Caine18 showed that the suicide rate of individuals struggling with alcohol addiction could be ten times higher (and, for other drugs, even up to fourteen times higher) than the rate seen for the general population. Psychoactive substances such as alcohol strongly reduce inhibitions when taken in high doses by dampening inhibitory pathways.19 At the same time, risky behavior increases when taking such substances, which also increases the probability of suicidal acts,20 which is partially explained by neurobiological links between suicide and substance use disorders (SUD).17
In addition, researchers have also identified psychological factors that facilitate the risk of suicidal behavior, including impulsiveness and aggression alone or in addition to the presence of psychiatric comorbid disorders.21–23 These factors are strongly expressed in addiction patients with personality disorders, and especially alcoholics with B-cluster disorders show an increased vulnerability to suicidal behavior24 (for an overview:25). As (abstinence) self-efficacy and (abstinence) confidence are considered to be important influencing factors with regard to staying sober after treatment,26,27 one study indicated that low self-efficacy is related to suicidal ideation in a sample of patients with addictive disorders.28 Additionally, researchers have observed connections between (mal)adaptive emotion regulation and suicidal ideation, suggesting that low abilities to regulate emotions are linked to suicidal behavior in patients with SUDs.29 As individuals seeking addiction treatment often experience a variety of predisposing and precipitating risk factors, such as relationship problems, financial and career concerns, and advanced health problems, certain sociodemographic factors are associated with suicidal ideation. Risk factors in patients with SUD include being female, having a low socioeconomic status, being single and being unemployed.21,30–32 Females with an alcohol use disorder have been found to have a two-fold risk for death by suicide as compared to males.33
Thus, in primary psychiatric care, special attention is given to the treatment of substance-dependent individuals for suicide prevention. On average, it takes individuals with SUD ten years from the first manifestation of alcohol-associated problems until they seek professional help in Austria.34,35 Many patients already have a long history of suffering, and the accompanying physical and psychological problems are often already chronic. Accordingly, subjective feelings of existential threat, as well as feelings of hopelessness and helplessness, are common. These findings indicate that the increased risk of suicidal behavior among persons with substance use disorders requires a better understanding and assessment of the associated factors.
The aim of the present study was (a) to investigate the prevalence of suicidal ideation in a sample of patients with SUD, (b) to detect changes in suicidal ideation occurring during the inpatient treatment, (c) to identify factors associated with a reduction in the number of suicidal thoughts, and (d) to highlight gender differences associated with suicidal ideation in patients with SUD.
Materials and Methods
Patients and Procedure
Data from patients with various addictive disorders were collected as part of a routine assessment during an inpatient therapeutic stay in hospital facility specialized in the treatment of addiction patients (Anton Proksch Institute, Kalksburg/Vienna) between July 2019 and February 2022. In order to partake in the treatment, patients must exhibit an absence of acute psychotic occurrences, lack notable cognitive impairments, and possess adequate proficiency in the German language to actively participate in therapy. Depending on their specific needs, all patients received a set of multidisciplinary therapies that included medical and nursing treatment, psychological therapies, nutritional counseling and physiotherapy. The inpatient treatment was based on a resource-oriented approach of addictive disorders to reduce the suicide rate. In addition to medical and psychotherapeutic basic modules, addiction-specific intervention modules such as relapse prevention as well as modules for sports, movement, relaxation, and social and vocational (re)integration are available to patients. An additional treatment- pillar consists of the Orpheus modules36 to support patients in (re)claiming a meaningful and joyful life. In analogy to Orpheus the eponymous hero of Greek mythology individuals struggling with addiction are intended to perceive abstinence not as deprivation but as a foundation for transformation and an opportunity for life redesign. In Austria, the costs for the rehabilitation treatment are covered by the social insurance institutions. Patients typically continue outpatient treatment following their inpatient stay to stabilize the treatment outcome.
In addition to meeting the treatment inclusion criteria, study participants were required to (a) be aged 18 or older, (b) provide written informed consent, (c) submit complete assessment data, and (d) identify as either male or female. Exclusion criteria comprised individuals with (a) court-ordered therapy or (b) a non-binary gender identity. The data recorded for the patients were gathered by means of a systematic, standardized survey procedure at the beginning (T1; after the first week, within day 7–10 of treatment) and end (T2; within the last week) of their therapeutic stay. Data were collected electronically using a multifunctional web-based application called the Life App, which is based on the Computer-based Health Evaluation Software (CHES).37 Participation in the survey was voluntary, so reasons for non-participation could be multifaceted (eg, motivation, cognitive impairment, early discharge, discomfort, privacy concerns, early termination of treatment). Patients signed a written informed consent before baseline assessment. The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Sigmund Freud University (UBWCF2VXAVBDSV88362, vote on 16 December 2020).
Assessment Instruments
The ICD-10 Symptom Rating (ISR)38 was used to evaluate the severity of various psychopathological symptoms. The ISR is based on the listed symptoms of ICD-10 Chapter F and comprises a total of 29 questions to assess six subscales. In this study, five subscales were used, namely, depression, compulsion, somatization and eating disorders. Higher scores indicate worse levels of psychological well-being. Suicidal ideation was assessed by means of a single item from the ISR supplementary scale (‘I am thinking about killing myself’). Responses could be given on a five-point scale ranging from 0 (strongly disagree) to 4 (strongly agree). Higher scores indicate more severe suicidal ideation and patients with scores higher than 0 were classified as having suicidal ideation. The Heidelberg Scales for Abstinence Confidence (HEISA)39 was used to assess the degree of patients’ confidence in whether they can abstain from substance use in different situations. The questionnaire comprises a total of 17 items, four of which represent the four subscales of unpleasant feelings, temptations and cravings, reckless thinking and pleasant feelings. Higher scores indicate higher levels of confidence in abstaining. The assessment of the psychological trait impulsivity was conducted using the I-8 impulsiveness scale.40 The scale measures four facets of impulsive behavior by using two items each: Urgency, intention, perseverance and risk behavior. High scores on the intention and perseverance scale indicate low levels of impulsiveness, while high scores on the urgency and risk behavior scale indicate high levels of impulsiveness. Emotion regulation abilities of the patients was assessed with the Emotion Regulation Questionnaire (ERQ).41 The ERQ consists of ten items to assess the habitual use of two emotion regulation strategies: Cognitive Reappraisal refers to the reinterpretation of a situation that evokes emotion to alter its meaning and change the emotional impact. Expressive Suppression refers to the attempt to hide and/or reduce ongoing emotions. The measurement of the outcome self-efficacy was tested using the German General Self-Efficacy Scale (in German: Selbstwirksamkeitserwartung or SWE).42 The SWE consists of 10 items which are summed up to a total score with higher scores indicating higher self-efficacy beliefs. And finally, the patients feelings of autonomy and joy were measured by using the AUFF (in German: Autonomie und Freude;43). The AUFF consists of 12 items which are summed up to a total score with higher scores indicating higher levels of autonomy and joy.
Statistical Analysis
Demographics for the sample are presented with means and standard deviations (SD). Since it was only possible to complete the survey if all questions had been answered, no values were missing from the data set. The participation in the observational study was on a voluntary basis. The number of cases was derived from the number of all patients treated at the study center (clinical trial center: Anton Proksch Institute, Kalksburg/Vienna, Austria). Therefore, we did not estimate the sample size before carrying out this cohort study. According to Cohen,44 in the given 2x2x2 design [men vs women as factor A and patients with (Sui+) vs without (Sui-) suicidal ideation at T1 as factor B with two time points (factor C: pre vs post) per AxB combination], four samples of 82 participants each (N=328) would be required to ensure small to medium effects at the level of α = 0.01 with a power (1 - β) of 0.8. With the given sample size of n = 694, a post-hoc calculation indicates a satisfactory power (1 - β > 0.80) to detect gender differences in suicidal ideation in patients with SUD. Differences in sociodemographic aspects of the sample as well as checks for biases were tested for significance with chi-squared tests and independent sample t-tests. If the Levene’s test indicated homogeneity of variances, we performed Welch’s tests. General linear models (GLM) were used to perform a per protocol analysis of pre-post therapy improvements via repeated measures analysis of variances (ANOVA) and multivariate ANOVAs. In addition to the p-values, partial eta-squared (ηp2), Cohen’s d (d), and phi (ϕ) were calculated as measures of effect sizes. Effect size values of d = 0.3, η2 = 0.01 and ϕ = 0.1 were considered small; d = 0.5, η2 = 0.06 and ϕ = 0.3 were medium; and d = 0.8, η2 = 0.14 and ϕ = 0.5 were large.45 P-values < 0.05 (two-sided) were considered to be statistically significant and all calculation were performed with IBM SPSS 26.0.
Results
Sociodemographic and Clinical Data
Initially, data from n = 1295 patients were collected. Of these, n = 540 patients were excluded because they only completed one assessment timepoint. Further reasons for exclusion were self-reported poor German language skills (n = 3), a therapeutic stay due to a court order (n = 42), and a prematurely canceled stay (< 17 days, n = 7; shortest time interval for the survey recommended by hospital officials) or extended therapeutic stay (> 122 days, n = 9; two-times longer than recommended by hospital guidelines). The excluded patients were significantly younger than included patients (46.4 vs 49.2 years; p < 0.001, d = 0.21), reported slightly higher scores for suicidal ideations (0.37 vs 0.28; p = 0.020, d = 0.12) and more frequently reported suicidal ideation (p(χ2) = 0.026, φ = 0.076) than the included sample. However, all differences had a small effect size.
The remaining n = 694 (53.6%) patients were included in the analyses. The mean age was 49.2 (SD = 11.8) years, and 68.2% were male. Most frequent reason for therapy was problematic alcohol use (82.4%), followed by misuse of medication (6.3%), behavioral addictions (3.3%) and other forms of addictions (eg, cannabinoids, opioids; 3.3%). Approximately half of the patients had finished basic education or an apprenticeship (55.9%), and most were not living in a relationship (76.7%). The mean interval between admission to and discharge from the rehabilitation center was 57.4 (SD = 18.7) days. For details, see Table 1.
 |
Table 1 Sociodemographic Characteristics (n = 694) |
Prevalence and Extent of Suicidal Ideation in Inpatient Addiction Treatment
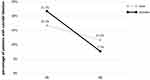
At T1, a total of n = 127 (18.3%) of the respondents reported suicidal ideation. At T2, the prevalence of suicidal ideation was reduced to n = 72 (10.4%) (ie, the number of persons with suicidal ideation was almost reduced by half). While at T1, a higher proportion of female patients, as compared to male patients, reported experiencing suicidal ideation (21.7% vs 16.7%; χ2= 2.54, p=0.11). However, at T2, the proportion decreased among female patients in contrast to male patients (7.7% vs 11.6%; χ2= 2.51, p=0.11). Although there was no significant difference in the proportion of suicidal thoughts between genders at either T1 or T2, the overall reduction in prevalence was significantly more pronounced among female patients than male patients (χ2= 4.20, p=0.040; see also Figure 1).
Overall, n = 154 (22.2%) different patients reported suicidal ideation at either T1 or T2. Of these, n = 101 (65.6%) reported weaker, n = 25 (16.2%) reported consistent, and n = 28 (18.2%) reported stronger suicidal ideation when comparing T1 and T2. A Sankey diagram in Figure 2 illustrates the changes in the expressions of suicidal ideation.
Pre-Post Improvements of Patients During Hospital Treatment
Before treatment, statistically significant differences in the baseline scores of all variables except risk behavior (I8) were found when comparing patients with and without suicidal ideation (effect sizes ranging from ηp² = 0.017 to ηp² = 0.116, see Supplementary Material Table S1). The multivariate ANOVA revealed a statistically significant decrease in symptoms for suicidal (p < 0.001; ηp² = 0.719) as well as non-suicidal patients (p < 0.001; ηp² = 0.495) with large effect sizes. Based on the self-reported ratings, statistically significant improvements in patients with suicidal ideation were observed across all variables, except for risk behavior (I8 questionnaire). In patients without suicidal ideation, all scores significantly improved. Most of the scales showed higher effects for patients with than without suicidal ideation at T1, and a higher number of large effect sizes (ηp² > 0.14) was also detected in this group. In both groups, the largest improvements were observed for depression (sui+: ηp² = 0.580, sui-: ηp² = 0.435), autonomy and joy (sui+: ηp² = 0.560, sui-: ηp² = 0.314), and anxiety (sui+: ηp² = 0.473, sui-: ηp² = 0.208). Table 2 provides an overview of the main results. By the means of a repeated measures ANOVA, we also determined an overall significant interaction effect between time and suicidal ideation (p < 0.001, ηp² = 0.080). More precisely, ten out of the seventeen investigated scales indicated significant interactions. The highest, but still small, effect sizes were found for depression (ηp² = 0.035), anxiety (ηp² = 0.035), and autonomy and joy (ηp² = 0.032). For a detailed illustration of all interactions, see Supplementary Material Table S1.
 |
Table 2 Pre-Post Treatment Effects of Patients with and without Suicidal Ideation (n = 694), Sorted by Effect Size |
Gender-Dependent Pre-Post Improvements
Before treatment, statistically significant differences in the baseline scores of all variables except somatization (ISR) and reappraisal (ERQ) were found when comparing male and female patients (effect sizes ranging from ηp² = 0.008 to ηp² = 0.044, see Supplementary Material Table S2). On the one hand, male patients reported higher confidence in abstaining, better emotion regulation, more feelings of autonomy and joy, higher self-efficacy, lower depression, anxiety and compulsion, as well as less urgent feelings of impulsiveness and greater intentions to persevere. Females, on the other hand, reported less risky behaviors in terms of impulsiveness.
No significant difference was observed in the ratings of the suicidal ideation when comparing male and female patients prior to the treatment (p = 0.288). Multivariate ANOVA revealed a statistically significant main effect of time for male (p < 0.001; ηp² = 0.485) as well as female (p < 0.001; ηp² = 0.624) patients between the two measurements. Based on the self-reported ratings, significant improvements for all variables, except for suppression (ERQ), were observed for female patients. Males reported significant changes for all variables. Generally, female patients indicated higher improvements and reported large effect sizes (ηp² > 0.14) more often than male patients. The highest effects for both groups were found in terms of depression (ISR; female: ηp² = 0.539, male: ηp² = 0.423), autonomy and joy (AUFF; female: ηp² = 0.493, male: ηp² = 0.296), and anxiety (ISR; female: ηp² = 0.352, male: ηp² = 0.212) ratings (see Table 3). As for suicidal ideation, female patients showed improvements with moderate (ηp² = 0.074) and male patients with small effect sizes (ηp² = 0.035). Due to the high number of patients without suicidal ideation at T1, gender-specific analyses were repeated in patients with suicidal ideation at T1. While we found large significant improvements with high effect sizes for both genders, female patients (ηp² = 0.287) reported higher improvements than male patients (ηp² = 0.171).
 |
Table 3 Pre-Post Treatment Effects for Female and Male Patients (n = 694), Sorted by Effect Size |
Again, by conducting a repeated measures ANOVA, a significant overall interaction effect for time and gender was observed (p < 0.001; ηp² = 0.062). In ten out of seventeen scales, significant time*gender interactions were observed. The largest effect of gender on improvement during the treatment was found for autonomy and joy (AUFF; ηp² = 0.031), temptations and cravings (HEISA; ηp² = 0.023), and unpleasant feelings (HEISA; ηp² = 0.021). For a detailed overview, see Supplementary Material Table S2.
Discussion
The aim of this study was to investigate the prevalence of suicidal ideation in a sample of patients with SUD as well as to detect changes in suicidal ideation occurring during the inpatient treatment, identifying factors associated with a reduction in the number of suicidal thoughts, and highlighting gender differences associated with suicidal ideation in patients with SUD. The results of the study underline the necessity of performing a detailed anamnesis of current suicidal ideation in inpatients undergoing SUD treatment and provides initial findings on the effectiveness of a resource-oriented treatment of the addictive disorder using the example of the “Orpheus Model”36 to reduce the suicide rate.
In our sample, a substantial proportion of patients (~18%) reported suicidal ideation. This prevalence agrees with other results reported for inpatients,46 but is higher than those reported for outpatient samples with SUD.47 Before treatment, female patients reported a higher prevalence of suicidal ideation than male patients (22% vs 17%), although this difference was not statistically significant. Studies of the general population have shown that female participants tend to report suicidal ideation more often than male.48 Some studies found no significant gender difference in this regard in patient samples treated for SUD,47,49,50 while others supported the hypothesis that females show higher rates of suicidal ideation or behavior.30,32 However, most of these studies investigated suicidal ideation differently (eg, in terms of lifetime suicidal ideation) and, given the increased risk of dying from suicide among females patients with alcohol use disorders as compared to among male patients,33 it seems fair to assume that a heightened risk for suicidal ideation exists among females with SUDs. Some researchers have hypothesized that, in females with an alcohol use disorder, the risk of dying from suicide may be increased by a heightened susceptibility to the effects of alcohol,51,52 an accelerated progression toward dependence (ie, “telescoping effect”)53, and earlier onset health issues and psychosocial complications caused by alcohol.54 Female patients in our sample, however, not only reported having more suicidal thoughts before treatment, but also fewer suicidal thoughts at the end of treatment (8% vs 12%). This indicates that females may benefit more from inpatient treatment in terms of a reduction in suicidal ideation than men. This finding agrees with those from previous studies, which found that psychosocial interventions for suicidal ideation and behavior are more effective in females than males.55 However, the latter authors also critically noted that only 18% of RCTs reported gender differences for psychosocial interventions to reduce the risk of suicide, thus highlighting the fact that this is still a relatively neglected area of research and clinical practice.
At baseline, a clear pattern of gender differences could be observed: While female patients reported higher levels of anxiety, depression and compulsion, male patients reported higher levels of confidence in abstaining, more feelings of autonomy and joy, and higher self-efficacy. In the past, other authors have clearly pointed out that females are more at risk for depressive56 and anxiety disorders than males.57 In line with previous research,41,58 male patients in our study tended to suppress emotion more actively than female patients as a strategy for regulating their emotions. While emotion suppression is often associated with dysfunctional coping and negative long-term outcomes,59 some studies indicated a potential male advantage associated with the short-term regulation of negative emotions by expressive suppression.60
Overall, patients largely benefitted from the inpatient treatment in terms of a reduction in overall symptoms. The largest improvements were found for depressive symptoms, anxiety, as well as a substantial increase in subjective autonomy and joy. While both males and females profited from the therapy, female patients generally showed larger effect sizes than male patients. This finding agrees with those of previous studies, which reported better treatment success61 as well as greater reductions in post-treatment substance use in female participants.62
However, several limitations of the study have to be considered. First, a floor effect for suicidal ideation was observed, which indicated that suicidal ideation might not have been assessed perfectly. Given the substantial gender effects we observed in our study, we conclude that gender-specific assessment tools are needed. Another limitation is the high dropout rate seen in our sample. In addition, it is not clear whether some patients reported higher levels of suicidal ideation at baseline due to the withdrawal symptoms they experienced in the first week of treatment. In our sample, no exact data on the use of agonist treatment is available. However, the data for patients at T1 are collected 7–10 days after admission and thus for most patients with an alcohol use disorder – which constitutes the majority of our sample – alcohol withdrawal and its drug treatment is completed by this time. Additionally, since some patients are admitted early or do not require withdrawal (eg, in case of behavioral addictions), it can be assumed that the majority of individuals were not under the influence of withdrawal medications. Also, participation in the study was voluntary; therefore, individuals experiencing severe withdrawal symptoms and having limited cognitive resources would likely face challenges in completing the questionnaire and would therefore not have participated. It has to be assumed that the change of environment partially causes the observed improvements during treatment and thus may be an important mechanism of change in itself. As treatment motivation is already a part of therapeutic work in patients with substance use disorders, the willingness for inpatient admission can be considered as part of treatment success. In the case of substance use disorders, inpatient treatment is even more stigmatized and laden with shame compared to other psychiatric conditions, which is why the change in setting, according to the bio-psycho-social treatment concept, represents a crucial step in the treatment process.
The presence of the psychologist during the assessment procedures may have increased the social desirability bias. To reduce this bias, the psychologists have been instructed to stay in the background and only interact with the patient if there are problems during the assessment. One notable limitation of this study is the presence of self-selection bias. Participants were not randomly assigned to groups; rather, they voluntarily chose to participate. This self-selection introduces the possibility that individuals with specific characteristics or motivations may be overrepresented in the study sample and thus the findings may not be fully generalizable to the broader population. Future research with randomized controlled designs or additional statistical controls could help mitigate the impact of self-selection bias on the interpretation of study outcomes. In addition, long-term follow-up is necessary to evaluate the sustainability of the improvements observed in this study.
Conclusion
Our study underscores the beneficial effect of addiction-specialized inpatient treatment on suicidal ideation, as well as psychopathologies and protective factors such as self-efficacy and positive feelings of autonomy and joy. The findings show that addiction treatment has the potential to lower the suicidal risk and reduce the risk of other comorbidities, supporting protective factors such as emotion regulation, impulsiveness and self-efficacy. Targeting and encouraging positive aspects and focusing on healthy aspects of the patients psyche during inpatient therapy should be considered as important to reduce psychopathologies such as depression or anxiety.
In addition, we found substantial gender differences both in terms of psychological distress at baseline as well as the therapeutic outcome: While female patients generally were more distressed at the beginning of the inpatient therapy they also reported a larger improvement of distress during the therapy program. This result highlights the need to perform more gender-sensitive research and develop more gender-sensitive treatment programs.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Sigmund Freud University, Vienna (UBWCF2VXAVBDSV88362, vote on 16 December 2020).
Data Sharing Statement
The data sets analyzed in this manuscript are not publicly available due to ethical and legal restrictions (data contain potentially identifying and sensitive patient information). If not already reported within this work, the authors may provide descriptive data on individual medical indicators for admission and discharge or the expected change due to inpatient health care for various groups and diagnoses. Requests for access to anonymized data sets should be directed to the corresponding author Vincent Grote ([email protected]).
Informed Consent Statement
Written informed consent was obtained from all subjects involved in the study.
Acknowledgments
The authors sincerely thank Sara Crockett for proofreading support. We also want to thank Silvia Lechner for the organizational support of this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223–33. doi:10.1016/s0140-6736(09)60746-7
2. Bachmayer S, Strizek J, Uhl A. Handbuch Alkohol–Österreich, Band 1: Statistiken und Berechnungsgrundlagen 2020: Gesundheit Österreich GmbH; 2021.
3. Pasche S. Exploring the comorbidity of anxiety and substance use disorders. Curr Psychiatry Rep. 2012;14(3):176–181. doi:10.1007/s11920-012-0264-0
4. Hasin D, Kilcoyne B. Comorbidity of psychiatric and substance use disorders in the United States: current issues and findings from the NESARC. Curr Opin Psychiatry. 2012;25(3):165–171. doi:10.1097/YCO.0b013e3283523dcc
5. Kienast T, Stoffers J, Bermpohl F, Lieb K. Borderline personality disorder and comorbid addiction: epidemiology and treatment. Dtsch Arztebl int. 2014;111(16):280–286. doi:10.3238/arztebl.2014.0280
6. Tripp JC, Jones JL, Back SE, Norman SB. Dealing with complexity and comorbidity: comorbid PTSD and substance use disorders. Curr Treat Options Psychiatry. 2019;6(3):188–197. doi:10.1007/s40501-019-00176-w
7. Chan YF, Dennis ML, Funk RR. Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. J Subst Abuse Treat. 2008;34(1):14–24. doi:10.1016/j.jsat.2006.12.031
8. van Emmerik-van Oortmerssen K, van de Glind G, van den Brink W, et al. Prevalence of attention-deficit hyperactivity disorder in substance use disorder patients: a meta-analysis and meta-regression analysis. Drug Alcohol Depend. 2012;122(1–2):11–19. doi:10.1016/j.drugalcdep.2011.12.007
9. Lai HM, Cleary M, Sitharthan T, Hunt GE. Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: a systematic review and meta-analysis. Drug Alcohol Depend. 2015;154:1–13. doi:10.1016/j.drugalcdep.2015.05.031
10. Hunt GE, Malhi GS, Cleary M, Lai HM, Sitharthan T. Prevalence of comorbid bipolar and substance use disorders in clinical settings, 1990–2015: systematic review and meta-analysis. J Affect Disord. 2016;206:331–349. doi:10.1016/j.jad.2016.07.011
11. Grant BF, Saha TD, Ruan WJ, et al. Epidemiology of DSM-5 drug use disorder: results from the national epidemiologic survey on alcohol and related conditions-III. JAMA psychiatry. 2016;73(1):39–47. doi:10.1001/jamapsychiatry.2015.2132
12. Scheibenbogen O, Feselmayer S. Über die Bedeutung der Epidemiologie komorbider Strörungen in der Suchtbehandlung. Spektrum Psychiatrie. 2008;1:48–50.
13. Wu LT, Blazer DG. Substance use disorders and psychiatric comorbidity in mid and later life: a review. Int J Epidemiol Apr. 2014;43(2):304–317. doi:10.1093/ije/dyt173
14. Harmer B, Lee S, Duong TVH, Saadabadi A. Suicidal Ideation. In: StatPearls. StatPearls Publishing LLC.; 2022.
15. Darvishi N, Farhadi M, Haghtalab T, Poorolajal J, Voracek M. Alcohol-related risk of suicidal ideation, suicide attempt, and completed suicide: a meta-analysis. PLoS One. 2015;10(5):e0126870. doi:10.1371/journal.pone.0126870
16. Poorolajal J, Haghtalab T, Farhadi M, Darvishi N. Substance use disorder and risk of suicidal ideation, suicide attempt and suicide death: a meta-analysis. J Public Health. 2016;38(3):e282–e291. doi:10.1093/pubmed/fdv148
17. Rizk MM, Herzog S, Dugad S, Stanley B. Suicide risk and addiction: the impact of alcohol and opioid use disorders. Curr Addict Rep. 2021;8(2):194–207. doi:10.1007/s40429-021-00361-z
18. Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend. 2004;76:S11–9. doi:10.1016/j.drugalcdep.2004.08.003
19. Smith JL, Mattick RP, Jamadar SD, Iredale JM. Deficits in behavioural inhibition in substance abuse and addiction: a meta-analysis. Drug Alcohol Depend. 2014;145:1–33. doi:10.1016/j.drugalcdep.2014.08.009
20. Conner KR, Bagge CL. Suicidal behavior: links between alcohol use disorder and acute use of alcohol. Alcohol Res. 2019;40(1). doi:10.35946/arcr.v40.1.02
21. Andersson HW, Lilleeng SE, Ruud T, Ose SO. Suicidal ideation in patients with mental illness and concurrent substance use: analyses of national census data in Norway. BMC Psychiatry. 2022;22(1):1. doi:10.1186/s12888-021-03663-8
22. Rodriguez-Cintas L, Daigre C, Braquehais MD, et al. Factors associated with lifetime suicidal ideation and suicide attempts in outpatients with substance use disorders. Psychiatry Res Apr. 2018;262:440–445. doi:10.1016/j.psychres.2017.09.021
23. Pompili M, Serafini G, Innamorati M, et al. Suicidal behavior and alcohol abuse. Int J Environ Res Public Health. 2010;7(4):1392–1431. doi:10.3390/ijerph7041392
24. Preuss UW, Koller G, Barnow S, Eikmeier M, Soyka M. Suicidal behavior in alcohol-dependent subjects: the role of personality disorders. Alcohol Clin Exp Res. 2006;30(5):866–877. doi:10.1111/j.1530-0277.2006.00073.x
25. Yuodelis-Flores C, Ries RK. Addiction and suicide: a review. Am J Addict. 2015;24(2):98–104. doi:10.1111/ajad.12185
26. Zingg C, Schmidt P, Kufner H, Kolb W, Zemlin U, Soyka M. [The relationship between self-efficacy and abstinence from alcohol after outpatient and inpatient treatment--A two year follow-up]. Der Zusammenhang zwischen Selbstwirksamkeit und Alkoholabstinenz bei ambulant und stationar behandelten Patienten: Ergebnisse einer 2-Jahres-Katamnese. Psychother Psychosom Med Psychol. 2009;59(8):307–313. German. doi:10.1055/s-2008-1067530
27. Kadden RM, Litt MD. The role of self-efficacy in the treatment of substance use disorders. Addict Behav. 2011;36(12):1120–1126. doi:10.1016/j.addbeh.2011.07.032
28. Czyz EK, Bohnert AS, King CA, Price AM, Kleinberg F, Ilgen MA. Self-efficacy to avoid suicidal action: factor structure and convergent validity among adults in substance use disorder treatment. Suicide Life Threat Behav. 2014;44(6):698–709. doi:10.1111/sltb.12101
29. Ghorbani F, Khosravani V, Sharifi Bastan F, Jamaati Ardakani R. The alexithymia, emotion regulation, emotion regulation difficulties, positive and negative affects, and suicidal risk in alcohol-dependent outpatients. Psychiatry Res. 2017;252:223–230. doi:10.1016/j.psychres.2017.03.005
30. Armoon B, SoleimanvandiAzar N, Fleury MJ, et al. Prevalence, sociodemographic variables, mental health condition, and type of drug use associated with suicide behaviors among people with substance use disorders: a systematic review and meta-analysis. J Addict Dis. 2021;39(4):550–569. doi:10.1080/10550887.2021.1912572
31. Masferrer L, Garre-Olmo J, Caparros B. Risk of suicide: its occurrence and related variables among bereaved substance users. J Subst Use. 2016;21(2):1–7. doi:10.3109/14659891.2014.998733
32. Andersson HW, Mosti MP, Nordfjærn T. Suicidal ideation among inpatients with substance use disorders: prevalence, correlates and gender differences. Psychiatry Res. 2022;317:114848. doi:10.1016/j.psychres.2022.114848
33. Roerecke M, Rehm J. Cause-specific mortality risk in alcohol use disorder treatment patients: a systematic review and meta-analysis. Int J Epidemiol. 2014;43(3):906–919. doi:10.1093/ije/dyu018
34. Bachmayer S, Strizek J, Uhl A. Handbuch Alkohol – Österreich. Band 1: Statistiken und Berechnungsgrundlagen; 2021.
35. Uhl A, Bachmayer S, Kobrna U, et al. Handbuch: alkohol - Österreich: zahlen, Daten, Fakten, Trends 2009; 2009.
36. Mader R, Scheibenbogen O, Musalek M. Alkoholkrankheit - bewährte und neue Behandlungsmöglichkeiten. J Für Neurologie, Neurochirurgie Und Psychiatrie. 2016;3:102–108.
37. Holzner B, Giesinger JM, Pinggera J, et al. The computer-based health evaluation software (CHES): a software for electronic patient-reported outcome monitoring. BMC Med Inf Decis Making. 2012;12:126. doi:10.1186/1472-6947-12-126
38. Tritt K, von Heymann F, Zaudig M, Zacharias I, Söllner W, Loew T. Entwicklung des Fragebogens »ICD-10-Symptom-Rating« (ISR) [Development of the “ICD-10-symptom-rating” (ISR) questionnaire]. Z Psychosom Med Psychother. 2008;54(4):409–418. German. doi:10.13109/zptm.2008.54.4.409
39. Körkel J, Schindler C, Hannig J. Die Heidelberger Skalen zur Abstinenzzuversicht (HEISA-16 und HEISA-38). In: Elektronisches Handbuch zu Erhebungsinstrumenten im Suchtbereich (EHES; Version 20). Institut für Umfragen, Methoden und Analysen (ZUMA) e. V; 1998.
40. Kovaleva A, Beierlein C, Kemper C, Rammstedt B. Eine Kurzskala zur Messung von Impulsivität nach dem UPPS-Ansatz: Die Skala Impulsives-Verhalten-8(I-8). GESIS; 2012.
41. Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85(2):348–362. doi:10.1037/0022-3514.85.2.348
42. Schwarzer R, Jerusalem M. Generalized self-efficacy scale. In: Weinman J, Wright S, Johnston M, editors. Measures in Health Psychology: A User’s Portfolio Causal and Control Beliefs. NFER-NELSON; 1995:35–37.
43. Scheibenbogen O, Kuderer M, Musalek M Autonomie und Freude Fragebogen (AUFF); 2019.
44. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Lawrence Erlbaum Associates, Inc; 1977.
45. Ellis PD. The Essential Guide to Effect Sizes: Statistical Power, Meta-Analysis, and the Interpretation of Research Results. Cambridge University Press; 2010.
46. Haynes CJ, Deane FP, Kelly PJ. Suicidal ideation predicted by changes experienced from pre-treatment to 3-month postdischarge from residential substance use disorder treatment. J Subst Abuse Treat. 2021;131:108542. doi:10.1016/j.jsat.2021.108542
47. Lopez-Goni JJ, Fernandez-Montalvo J, Arteaga A, Haro B. Suicidal ideation and attempts in patients who seek treatment for substance use disorder. Psychiatry Res. 2018;269:542–548. doi:10.1016/j.jad.2016.07.011
48. Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008;30(1):133–154. doi:10.1093/epirev/mxn002
49. Kelly LM, Rash CJ, Alessi SM, Zajac K. Correlates and predictors of suicidal ideation and substance use among adults seeking substance use treatment with varying levels of suicidality. J Subst Abuse Treat. 2020;119:108145. doi:10.1016/j.jsat.2020.108145
50. Wines JD Jr, Saitz R, Horton NJ, Lloyd-Travaglini C, Samet JH. Suicidal behavior, drug use and depressive symptoms after detoxification: a 2-year prospective study. Drug Alcohol Depend. 2004;76:S21–9. doi:10.1016/j.drugalcdep.2004.08.004
51. Hommer D, Momenan R, Kaiser E, Rawlings R. Evidence for a gender-related effect of alcoholism on brain volumes. Am J Psychiatry. 2001;158(2):198–204. doi:10.1176/appi.ajp.158.2.198
52. Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clinic Psychol Rev. 2004;24(8):981–1010. doi:10.1016/j.cpr.2004.08.003
53. Piazza NJ, Vrbka JL, Yeager RD. Telescoping of alcoholism in women alcoholics. Int J Addict. 1989;24(1):19–28. doi:10.3109/10826088909047272
54. Zilberman M, Tavares H, el-Guebaly N. Gender similarities and differences: the prevalence and course of alcohol- and other substance-related disorders. J Addict Dis. 2004;22(4):61–74. doi:10.1300/j069v22n04_06
55. Krysinska K, Batterham PJ, Christensen H. Differences in the Effectiveness of psychosocial interventions for suicidal ideation and behaviour in women and men: a systematic review of randomised controlled trials. Arch Suicide Res. 2017;21(1):12–32. doi:10.1080/13811118.2016.1162246
56. Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol Bull. 2017;143(8):783–822. doi:10.1037/bul0000102
57. McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. 2011;45(8):1027–1035. doi:10.1016/j.jpsychires.2011.03.006
58. Haga SM, Kraft P, Corby E-K. Emotion regulation: antecedents and well-being outcomes of cognitive reappraisal and expressive suppression in cross-cultural samples. J Happiness Stud. 2009;10(3):271–291. doi:10.1007/s10902-007-9080-3
59. Chapman BP, Fiscella K, Kawachi I, Duberstein P, Muennig P. Emotion suppression and mortality risk over a 12-year follow-up. J Psychosom Res. 2013;75(4):381–385. doi:10.1016/j.jpsychores.2013.07.014
60. Cai A, Yang J, Xu S, Yuan J. The male advantage in regulating negative emotion by expressive suppression: an event-related potential study. Acta Psychologica Sinica. 2016;48(5):482–494. doi:10.3724/sp.J.1041.2016.00482
61. Green CA. Gender and use of substance abuse treatment services. Alcohol Res Health. 2006;29(1):55–62.
62. Marsh JC, Cao D, D’Aunno T. Gender differences in the impact of comprehensive services in substance abuse treatment. J Subst Abuse Treat. 2004;27(4):289–300. doi:10.1016/j.jsat.2004.08.004
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.