Back to Journals » Clinical Ophthalmology » Volume 16
Factors Associated with Ophthalmology Referral and Adherence in a Teleretinal Screening Program: Insights from a Federally Qualified Health Center
Authors Song A , Johnson NA, Mirzania D, Ayala AM , Muir KW , Thompson AC
Received 1 July 2022
Accepted for publication 29 August 2022
Published 12 September 2022 Volume 2022:16 Pages 3019—3031
DOI https://doi.org/10.2147/OPTH.S380629
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ailin Song,1 Nicholas A Johnson,1 Delaram Mirzania,1,2 Alexandria M Ayala,1 Kelly W Muir,3,4 Atalie C Thompson3,5
1Duke University School of Medicine, Durham, NC, USA; 2Department of Ophthalmology and Visual Sciences, Kellogg Eye Center, University of Michigan Health, Ann Arbor, MI, USA; 3Department of Ophthalmology, Duke University, Durham, NC, USA; 4Durham Center of Innovation to Accelerate Discovery and Practice Transformation, Durham Veterans Affairs Health Care System, Durham, NC, USA; 5Wake Forest Baptist Health, Winston Salem, NC, USA
Correspondence: Atalie C Thompson, Wake Forest Baptist Health, Janeway Tower, 6 th Floor, 1 Medical Center Blvd, Winston Salem, NC, 27103, USA, Tel +1 650-868-8050, Email [email protected]
Background: Early detection of ophthalmic conditions such as diabetic retinopathy (DR) and glaucoma is crucial to preventing vision loss. Previous studies have evaluated teleretinal screening programs for DR in well-insured populations. The purpose of this retrospective study was to evaluate a teleretinal screening program in a population of uninsured and underinsured patients seen in a Federally Qualified Health Center (FQHC).
Methods: We conducted a retrospective chart review of patients (age ≥ 18) who underwent teleretinal imaging (TRI) at a FQHC between January 2015 and September 2019. TRI gradings and patient demographic and clinical information were abstracted. Factors associated with referral for a dilated eye exam by an ophthalmologist, adherence to recommended follow-up dilated eye exam, and ophthalmology visit attendance were examined.
Results: 3130 TRIs were graded in 2216 eyes (1107 patients). 65.2% (N = 722) self-identified as Hispanic and 56.3% (N = 623) required interpreter services. Follow-up dilated fundus examination (DFE) was recommended for 388 TRIs, 49% (N = 190) of which were completed within 1 year. Adherence to the recommended ophthalmology exam was not associated with any baseline clinical or demographic characteristics (p > 0.05). Older age, male sex, hypertension, proteinuria, and higher A1c were significantly associated with greater odds of ophthalmology referral based on TRI (all p < 0.05), after adjusting for covariates. Less severe diabetic retinopathy, no insurance coverage, and Hispanic ethnicity were associated with lower odds of attending an ophthalmology visit, regardless of follow-up recommendations based on TRI (all p < 0.05).
Conclusion: In an FQHC serving predominantly uninsured and underinsured patients, only 49% of recommended DFE were completed within one year. Less severe diabetic retinopathy, lack of insurance coverage, and Hispanic ethnicity were associated with a lower likelihood of having a DFE regardless of recommendation. These results suggest that greater system-level efforts are needed to increase adherence to follow-up eye exams after TRI to ensure sight-saving care for underserved populations.
Keywords: teleretinal screening, teleophthalmology, uninsured, underinsured, adherence, ophthalmology referral
Introduction
Diabetic retinopathy (DR) and glaucoma are leading causes of blindness worldwide.1 Early detection and timely referral to an ophthalmologist are imperative to the prevention of vision loss. However, only about 60% of patients with diabetes in the United States receive dilated eye examinations annually.2 Likewise, it has been estimated that 78% of individuals with glaucoma remain undiagnosed and untreated.3
Telemedicine approaches combining retinal imaging and remote image interpretation, also known as teleretinal imaging (TRI), have been proposed as a strategy to improve screening.4 Countries such as Singapore and the United Kingdom have demonstrated successful nationwide DR screening programs using telemedicine.5,6 In the United States, teleretinal screening programs have been implemented in selected populations, including patients in the Veterans Affairs system, rural areas, and urban safety-net clinics.7–13 If clinically important pathology is identified on TRI, referral to an ophthalmologist for dilated eye examination and management is crucial. While factors for ophthalmology referral have been explored in a regional telemedicine program serving primarily rural patients,9 it is not clear whether these factors generalize to other settings.
Federally Qualified Health Centers (FQHC) are funded by the United States federal government under Section 330 of the US Public Health Service Act to provide medical care in medically underserved areas and to medically underserved populations.14 Nearly 23 million patients and one out of seven Medicaid enrollees receive primary care services at FQHCs; nearly 75% of the FQHC patient population are uninsured or insured with Medicaid.15,16 In 2014, more than 1 in 4 people living in poverty were seen by FQHCs.17 FQHCs form the backbone of the medical safety net in the United States and are important providers of preventive health care to underserved populations. Nevertheless, teleretinal screening programs in FQHCs are underexplored in the literature.
The purpose of this study was to evaluate a teleretinal screening program implemented in a FQHC located in North Carolina. By collecting patient demographic and clinical characteristics, we examined factors associated with referral to an ophthalmologist for dilated fundus examination (DFE) based on findings from teleretinal imaging, patient adherence to recommended DFE within one year, and completion of DFE regardless of referral recommendation.
Patients and Methods
The Institutional Review Board at Duke University approved this study with a waiver of written informed consent due to the retrospective nature of the study. Patient data were anonymized to ensure patient privacy. This study was conducted in accordance with the Declaration of Helsinki.
All patients age 18 and older with diabetes mellitus who presented to Lincoln Community Health Center between January 1, 2015, and September 4, 2019, as part of an ongoing teleretinal screening program were included in this retrospective study. Lincoln Community Health Center is an FQHC located in Durham, North Carolina, that provides primary and preventive health care to the medically underserved. TRIs were obtained using a nonmydriatic fundus camera (Canon CR-2 AF; Tokyo, Japan). Multiple TRIs were acquired for some patients given the longitudinal nature of the screening program. Images were manually graded for suspicion of diabetic retinopathy, glaucoma, age-related macular degeneration, retinal vein occlusions, and other retinal pathology by a glaucoma specialist. Based on the grading, patients were recommended to repeat TRI in one year or referred to an ophthalmologist for DFE. A sample TRI grading and recommendation form is provided in Supplementary Materials. TRI gradings, patient demographics, relevant medical history, laboratory data, and information from subsequent ophthalmology visits were abstracted from electronic health records (EHR). Medical history was determined from ICD-9/10 codes. Regarding insurance coverage, the primary coverage information in the EHR was collected, including coverage by Project Access, a community support program that connects Durham residents without health insurance to specialty healthcare resources.
Statistical Analysis
Baseline descriptive statistics were performed on clinical and demographic data. Bivariate analyses with generalized estimating equations were performed to evaluate the association of demographic and clinical characteristics with three different outcomes 1) recommendation of a follow-up DFE by ophthalmology within one year vs repeat teleretinal imaging; 2) actual follow-up DFE by ophthalmology vs no DFE within one year; 3) adherence to follow-up recommendation for DFE within one year. The non-adherent group was comprised of patients who did not attend a recommended DFE within one year, and the adherent group was comprised of patients who completed a DFE within one year if recommended. Variables with a p-value of <0.05 were entered into separate multivariable models to determine which factors were independently associated with each outcome. A p-value <0.05 was set as the a priori alpha level.
In addition, the agreement between TRI gradings and DFE findings was determined for glaucoma and diabetic retinopathy if DFE was completed, and Kappa statistics were estimated.
Results
This study included 3130 TRIs that were captured and graded for 2214 eyes of 1107 patients. Among the graded TRIs, 3118 were provided a follow-up recommendation, and the recommendation was missing from 12 grading forms. Interpreter services were required for 56.3% (N = 623) of patients; 65.2% (N = 722) self-identified as Hispanic ethnicity. Patient baseline characteristics are shown in Table 1.
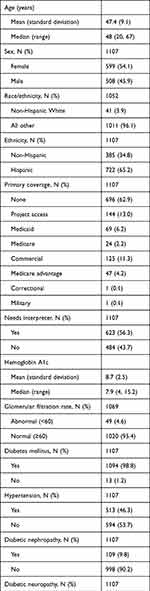 |
Table 1 Baseline Study Patient Characteristics (N = 1107 Patients) |
A recommended follow-up for dilated fundus examination was made in 388 of the TRIs (12.4% of TRIs). In bivariate analyses, older age and medical comorbidities, including diabetic nephropathy, diabetic neuropathy, hypertension, proteinuria, GFR <60, and higher HbA1c, were associated with higher odds of referral to ophthalmology for DFE based on TRI (all p < 0.05; Table 2). On the other hand, female sex (OR, 0.75; p = 0.001), Hispanic ethnicity (OR, 0.79; p = 0.009), and need for interpreter services (OR, 0.81; p = 0.017) were factors associated with a lower likelihood of receiving a recommendation for DFE with ophthalmology. In the multivariable model, older age, male sex, hypertension, proteinuria, and higher HbA1c levels remained significantly associated with higher odds of ophthalmology referral (all p < 0.05), after adjusting for ethnicity, need for interpreter services, diabetic nephropathy, diabetic neuropathy, and GFR (Table 3).
 |
Table 2 Bivariate Analysis of Factors Associated with Ophthalmology Referral Following Teleretinal Imaging (N = 3118) |
 |
Table 3 Multivariable Analysis of Factors Associated with Ophthalmology Referral Following Teleretinal Imaging |
A total of 396 follow-up visits with ophthalmology occurred during the study period, regardless of follow-up recommendations after TRI. In bivariate analyses, diagnosis of moderate-to-severe non-proliferative diabetic retinopathy (NPDR) or proliferative diabetic retinopathy (PDR) based on TRI, history of diabetic nephropathy, diabetic neuropathy, or hypertension, and older age were associated with greater odds of attending an ophthalmology visit (all p < 0.05, Table 4). Hispanic ethnicity, lack of insurance coverage, and need for interpreter services were associated with lower odds of attending an ophthalmology visit (all p < 0.05, Table 4). In the multivariable model, diagnosis of moderate-to-severe NPDR or PDR based on TRI was associated with greater odds of attending an ophthalmology visit (aOR, 3.69; p < 0.0001, compared with no diagnosis of DR/diagnosis of mild NPDR), no insurance coverage (aOR, 0.74; p = 0.016, compared with insurance coverage), and Hispanic ethnicity (aOR, 0.75; p = 0.015, compared with non-Hispanic ethnicity) were associated with lower odds of attending an ophthalmology visit, after adjusting for need for interpreter services, age, and history of diabetic nephropathy, diabetic neuropathy, hypertension, or proteinuria (Table 5).
 |
Table 4 Bivariate Analysis of Factors Associated with Dilated Fundus Examination by Ophthalmology Within 1 Year of Teleretinal Imaging |
 |
Table 5 Multivariable Analysis of Factors Associated with Ophthalmology Visit Attendance, Regardless of Follow-Up Recommendation Based on Teleretinal Imaging |
Recommendation for a DFE based on TRI was associated with a significantly higher likelihood of completing a follow-up DFE within 1 year of TRI (OR 3.77; 95% CI 2.99, 4.75, p < 0.0001). Follow-up DFE was recommended for 388 TRI visits, 49% (N = 190) of which were completed within 1 year. Twelve percent (N = 46) were completed after 1 year, 9% (N = 36) were not completed but returned for TRI, 28% (N = 108) were lost to follow-up completely, and 2% (N = 8) of patients did not return because they were deceased. Also, a minority of TRIs that were recommended for a repeat TRI underwent a DFE with ophthalmology within 1 year (N=202/2730, 7.40%). All TRI encounters where patients were diagnosed with moderate-to-severe non-proliferative diabetic retinopathy or proliferative diabetic retinopathy were referred for follow-up DFE with ophthalmology (N = 83), but only 59% of those referrals resulted in a follow-up DFE (N = 49). Adherence to a recommended follow-up with ophthalmology for DFE was not significantly associated with any of the baseline patient clinical or demographic characteristics (all p > 0.05). Approximately half of the follow-up ophthalmology exams were completed at the FQHC (N=196/396), and the remaining were completed at one of the three local ophthalmology referral centers.
There was excellent agreement between the TRI gradings and DFE diagnoses among patients who underwent subsequent ophthalmology DFE: 92.2% agreement (Kappa 0.82, p < 0.0001) for presence or absence of diabetic retinopathy and 88.4% agreement (Kappa 0.24, p < 0.0001) for glaucoma gradings (ie, glaucoma vs glaucoma suspect vs no glaucoma). Supplemental Tables 1 and 2 show the comparison between TRI gradings and DFE diagnoses for diabetic retinopathy and glaucoma, respectively.
Discussion
This study evaluated a teleretinal screening program implemented in an FQHC, a unique clinical setting that plays a central role in the preventive health care of medically underserved patients. Existing literature demonstrates that teleretinal screening is effective in narrowing disparities in preventive eye care.9,11,18,19 The majority of patients in our study had no insurance or payer for medical visits (62.9%) and a small percentage (13.0%) was enrolled in Project Access, a local non-profit organization that provides access to subspecialty care for a defined period of time at no cost to uninsured patients. Furthermore, 96.1% of patients in the study population were from minority racial/ethnic groups, with the majority being Hispanic and Spanish-speaking. It is well established that insurance status affects health care utilization, and ethnic/racial disparities exist in eye examination rates.20–23 Despite the high risk of these underserved populations for developing vision-threatening conditions, teleretinal screening programs dedicated to these populations have been underexplored. To our knowledge, our study is the first to examine demographic and clinical factors associated with ophthalmology referral from a teleretinal screening program in an FQHC.
In our study population, higher burden of systemic disease, including higher HbA1c levels, hypertension, and proteinuria, as well as older age were associated with a greater likelihood of receiving a recommendation for ophthalmology DFE based on TRI. Moreover, all TRIs graded as moderate-to-severe NPDR or PDR were referred for a DFE within 1 year. These findings are consistent with other studies documenting higher prevalence of DR and need for referral in patients with systemic comorbidities,9 highlighting the importance of screening in these at-risk populations. Interestingly, our study population was relatively young, with a mean age of 47.4 years, which suggests that TRI screening may benefit younger and middle-aged adults with diabetes mellitus. While the association between male sex and higher odds of ophthalmology referral identified in this study appears less intuitive, there is in fact emerging literature suggesting that the male sex is associated with greater prevalence of DR as well as higher severity of DR.24,25 Overall, the factors identified in this study have the potential to inform future screening strategies for patients at increased risk for vision-threatening eye disease.
We additionally explored factors associated with attending an ophthalmology visit following TRI, regardless of follow-up recommendations based on TRI. In the multivariable model, moderate-to-severe NPDR or PDR was significantly associated with higher odds of attending an ophthalmology visit after adjusting for need for interpreter services, age, and history of diabetic nephropathy, diabetic neuropathy, hypertension, or proteinuria. This association is reassuring as it suggests that patients with more severe diabetic retinopathy were following up with an ophthalmologist. We hypothesize that these patients may have been prioritized in the care coordination process. On the other hand, having no insurance coverage and Hispanic ethnicity remained significantly associated with lower odds of attending an ophthalmology visit, regardless of follow-up recommendation. This finding should be interpreted in context as neither factor was significantly associated with the need to follow up with ophthalmology (ie, ophthalmology referral) in our study when accounting for covariates. While our finding reveals disparities in completion of DFE by an ophthalmologist following TRI, it provides evidence that TRI serves to provide needed eye screening services to populations that otherwise may not be able to access ophthalmic care.
Furthermore, we found that the need for interpreter services was associated with lower odds of attending an ophthalmology visit in bivariate analysis. Although the association did not persist after adjustment for covariates including Hispanic ethnicity, most interpreter services were required for the Spanish language; we suspect that the association between need for interpreter services and odds of attending an ophthalmology visit was largely obscured by the strong relationship between Hispanic ethnicity and odds of attending an ophthalmology visit. A prior study showed that Spanish-speaking patients experienced difficulty communicating with eye care professionals in diabetic retinopathy evaluations.26 These challenges and other unmeasured variables, such as level of education, literacy, or perceptions of implicit bias, may create additional barriers for Spanish-speaking patients receiving a recommendation to schedule an in-person DFE with an ophthalmologist.27–29 For example, low disease knowledge has been identified as an important barrier to follow-up in patients with chronic eye diseases,30 and may contribute to low adherence to follow-up appointments after teleretinal screening as well.
Moreover, given that our cohort consisted primarily of younger and middle-aged adults of working age, it is possible that such patients may experience difficulty getting time off of work for subspecialty care visits.30 Future studies should incorporate patient interview to determine possible barriers to attending follow-up recommendations in non-English-speaking populations and should aim to improve health equity in receipt of eye care services.
In our cohort, fewer than half of the TRIs recommended for a follow-up DFE were completed as recommended within 1 year, and at least 28% were lost to follow-up. These findings and the fact that none of the evaluated factors were associated with adherence to recommended ophthalmology follow-up visits suggest that adherence to DFE following teleretinal screening remains a pervasive public health challenge. By comparison, the rates of adherence to follow-up DFE in prior studies ranged from 5% in primary care clinics of a large county hospital to 87% in a Veterans Affairs Healthcare System.31–35 Though teleretinal screening programs have been shown to improve screening rates,34 further evaluation and management with an ophthalmologist are ultimately needed to treat patients with signs of disease on TRI. Failing to attend the recommended evaluation may result in delays in care and worse outcomes.
System-level approaches to improve coordination of care may help improve adherence to recommended ophthalmology visits following teleretinal screening and are therefore needed to ensure sight-saving care in underserved populations. For example, Bresnick et al examined patients’ adherence to post-screening recommendations and found low rates of adherence, suggesting the need for a more robust tracking and recall system for non-adherence.31 Similarly, Keenum et al assessed the adherence patterns in a DR screening program in a publicly funded county clinic and found that fewer than 30% of patients obtained follow-up eye care within the recommended time frame.35 Their study additionally identified younger age, lack of knowledge about glycated hemoglobin levels, and needing assistance in making appointments as risk factors for non-adherence,35 suggesting the role of patient self-efficacy and eye health education in improving follow-up rates.35,36 Innovative strategies such as personalized interventions and immediate feedback on referral status based on artificial intelligence-supported screening have shown promise in recent randomized controlled trials for improving adherence to recommended follow-up primary eye care exams.37,38 Similar strategies could be extended to a teleretinal screening setting since TRI is often captured in primary care settings as in our study.
Future directions based on findings from this study include patient-centered research focused on understanding barriers to adherence, quality improvement initiatives to improve adherence, and randomized controlled trials to identify optimal strategies for eye care following teleretinal screening.
Strength and Limitations
The findings of this study should be interpreted in the context of the following limitations. This study abstracted retrospective data from the electronic health record, which may not contain comprehensive information. It is possible that the number of patients who followed up with ophthalmology as recommended was underreported, as visits outside of the EHR system used in this study may not be captured. However, with the increasing integration of EHRs across regional health systems, the ability to electronically capture follow-up for ophthalmic care continues to improve. The retrospective study design also limits our ability to draw causal conclusions; associations identified in this study may be confounded by unmeasured variables. Additionally, while the agreement between TRI grading and DFE diagnoses was nearly perfect for diabetic retinopathy (Kappa 0.82), the agreement was lower for glaucoma (Kappa 0.24). These results are consistent with previous studies reporting human experts’ limited accuracy in detecting glaucoma using fundus photographs.39,40 Recent advances in artificial intelligence have demonstrated improved performance compared with human experts and may aid in future glaucoma screening efforts.41 Finally, the study population was derived from a single FQHC, potentially limiting the generalizability of our findings. Future studies with multi-center and prospective designs can help to address these limitations.
This study has several strengths. First, our study considered teleretinal imaging in the context of an important and previously underexplored patient setting with a predominantly Spanish-speaking patient base. The findings of this study provide new insights into teleretinal screening for medically underserved patients, including uninsured, underinsured, and ethnic/racial minority patients, especially in an FQHC. Second, having a single ophthalmologist evaluate all retinal images provided consistency in diagnosis; the high agreement between TRI gradings and final diagnoses based on subsequent dilated fundus examinations further demonstrates the grading accuracy. Third, while previous studies on teleretinal screening tend to focus on DR, the study program also screened for other ocular conditions, such as glaucoma and macular degeneration, maximizing the utility of tele-retinal screening in preventing vision loss. Finally, our study included a large sample size and explored a range of clinical and demographic variables.
Conclusions
In a Federally Qualified Health Center serving predominantly uninsured and underinsured patients, those referred to ophthalmology based on teleretinal screening were more likely to have higher burdens of systemic disease. Adherence to the recommended follow-up DFE following TRI was less than 50%. Hispanic patients and patients requiring interpreter services may be less likely to attend a DFE following TRI. These data underscore the importance of increased efforts to better understand barriers to ophthalmic care for underserved patients, as well as to develop interventions to improve adherence to follow-up evaluation following teleretinal screening.
Abbreviations
DR, diabetic retinopathy; FQHC, Federally Qualified Health Center; TRI, teleretinal imaging; DFE, dilated fundus examination; EHR, electronic health records; NPDR, non-proliferative diabetic retinopathy; PDR, proliferative diabetic retinopathy; GFR, glomerular filtration rate; SD, standard deviation; CI, confidence interval; OR, odds ratio; aOR, adjusted odds ratio.
Acknowledgments
Interim findings from this study were presented at the 2021 Association for Research in Vision and Ophthalmology (ARVO) Annual Meeting as a poster presentation. The abstract of the poster was published in Investigative Ophthalmology & Visual Science. 2021; 62(8): 1146. https://iovs.arvojournals.org/article.aspx?articleid=2774222.
Funding
Dr. Thompson receives support from the NIH/NEI K23EU030897 and the American Glaucoma Society.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Steinmetz JD, Bourne RRA, Briant PS, et al. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9(2):e144–e160. doi:10.1016/S2214-109X(20)30489-7
2. Flaxel CJ, Adelman RA, Bailey ST, et al. Diabetic retinopathy preferred practice pattern®. Ophthalmology. 2020;127(1):P66–P145. doi:10.1016/j.ophtha.2019.09.025
3. Shaikh Y, Yu F, Coleman AL. Burden of undetected and untreated glaucoma in the United States. Am J Ophthalmol. 2014;158(6):1121–1129.e1. doi:10.1016/j.ajo.2014.08.023
4. Song A, Lusk JB, Roh KM, et al. Practice patterns of fundoscopic examination for diabetic retinopathy screening in primary care. JAMA Netw Open. 2022;5(6):e2218753. doi:10.1001/jamanetworkopen.2022.18753
5. Scanlon PH. The English National Screening Programme for diabetic retinopathy 2003–2016. Acta Diabetol. 2017;54(6):515–525. doi:10.1007/s00592-017-0974-1
6. Nguyen HV, Tan GSW, Tapp RJ, et al. Cost-effectiveness of a national telemedicine diabetic retinopathy screening program in Singapore. Ophthalmology. 2016;123(12):2571–2580. doi:10.1016/j.ophtha.2016.08.021
7. Wilson C, Horton M, Cavallerano J, Aiello LM. Addition of primary care-based retinal imaging technology to an existing eye care professional referral program increased the rate of surveillance and treatment of diabetic retinopathy. Diabetes Care. 2005;28(2):318–322. doi:10.2337/diacare.28.2.318
8. Cavallerano AA, Conlin PR. Teleretinal imaging to screen for diabetic retinopathy in the Veterans Health Administration. J Diabetes Sci Technol. 2008;2(1):33–39. doi:10.1177/193229680800200106
9. Jani PD, Forbes L, Choudhury A, Preisser JS, Viera AJ, Garg S. Evaluation of diabetic retinal screening and factors for ophthalmology referral in a telemedicine network. JAMA Ophthalmol. 2017;135(7):706. doi:10.1001/jamaophthalmol.2017.1150
10. Cuadros J, Bresnick G. EyePACS: an adaptable telemedicine system for diabetic retinopathy screening. J Diabetes Sci Technol. 2009;3(3):509–516. doi:10.1177/193229680900300315
11. Carvalho de AB, Ware SL, Lei F, Bush HM, Sprang R, Higgins EB. Implementation and sustainment of a statewide telemedicine diabetic retinopathy screening network for federally designated safety-net clinics. PLoS One. 2020;15(11):e0241767. doi:10.1371/journal.pone.0241767
12. Daskivich LP, Vasquez C, Martinez C, Tseng CH, Mangione CM. Implementation and evaluation of a large-scale teleretinal diabetic retinopathy screening program in the Los Angeles County Department of Health Services. JAMA Intern Med. 2017;177(5):642–649. doi:10.1001/jamainternmed.2017.0204
13. Chasan JE, Delaune B, Maa AY, Lynch MG. Effect of a teleretinal screening program on eye care use and resources. JAMA Ophthalmol. 2014;132(9):1045–1051. doi:10.1001/jamaophthalmol.2014.1051
14. Health Resources and Services Administration. Federally Qualified Health Centers. Official web site of the U.S. Health Resources & Services Administration; April 21, 2017. Available from: https://www.hrsa.gov/opa/eligibility-and-registration/health-centers/fqhc/index.html.
15. Health Resources and Services Administration. National Health Center data. Available from: https://data.hrsa.gov/tools/data-reporting/program-data/national.
16. National Association of Community Health Centers. Health Centers and Medicaid. Available from: http://nachc.org/wp-content/uploads/2015/11/Medicaid_FS_2014.pdf.
17. Nath JB, Costigan S, Hsia RY. Changes in demographics of patients seen at federally qualified health centers, 2005–2014. JAMA Intern Med. 2016;176(5):712. doi:10.1001/jamainternmed.2016.0705
18. Owsley C, McGwin G, Lee DJ, et al. Diabetes eye screening in urban settings serving minority populations: detection of diabetic retinopathy and other ocular findings using telemedicine. JAMA Ophthalmol. 2015;133(2):174–181. doi:10.1001/jamaophthalmol.2014.4652
19. Chin EK, Ventura BV, See KY, Seibles J, Park SS. Nonmydriatic fundus photography for teleophthalmology diabetic retinopathy screening in rural and urban clinics. Telemed J E Health. 2014;20(2):102–108. doi:10.1089/tmj.2013.0042
20. Shi Q, Zhao Y, Fonseca V, Krousel-Wood M, Shi L. Racial disparity of eye examinations among the U.S. working-age population with diabetes: 2002–2009. Diabetes Care. 2014;37(5):1321–1328. doi:10.2337/dc13-1038
21. Kushel MB. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200. doi:10.1001/jama.285.2.200
22. Baker RS, Watkins NL, Wilson MR, Bazargan M, Flowers CW. Demographic and clinical characteristics of patients with diabetes presenting to an urban public hospital ophthalmology clinic. Ophthalmology. 1998;105(8):1373–1379. doi:10.1016/S0161-6420(98)98015-0
23. Gregg EW, Geiss LS, Saaddine J, et al. Use of diabetes preventive care and complications risk in two African-American communities. Am J Prev Med. 2001;21(3):197–202. doi:10.1016/s0749-3797(01)00351-8
24. Ozawa GY, Bearse MA, Adams AJ. Male-female differences in diabetic retinopathy? Curr Eye Res. 2015;40(2):234–246. doi:10.3109/02713683.2014.958500
25. Cherchi S, Gigante A, Contini P, et al. Male type 2 diabetic patients have higher diabetic retinopathy prevalence. Diabetes. 2018;67(Supplement1):599–P. doi:10.2337/db18-599-P
26. Hudson SM, Modjtahedi BS, Altman D, Jimenez JJ, Luong TQ, Fong DS. Factors affecting compliance with diabetic retinopathy screening: a qualitative study comparing English and Spanish speakers. Clin Ophthalmol. 2022;16:1009–1018. doi:10.2147/OPTH.S342965
27. DuBard CA, Gizlice Z. Language spoken and differences in health status, access to care, and receipt of preventive services among US Hispanics. Am J Public Health. 2008;98(11):2021–2028. doi:10.2105/AJPH.2007.119008
28. Jacobson HE, Hund L, Soto Mas F. Predictors of English health literacy among U.S. Hispanic Immigrants: the importance of language, bilingualism and sociolinguistic environment. Lit Numeracy Stud. 2016;24(1):43–64. doi:10.5130/lns.v24i1.4900
29. Gonzalez CM, Deno ML, Kintzer E, Marantz PR, Lypson ML, McKee MD. Patient perspectives on racial and ethnic implicit bias in clinical encounters: implications for curriculum development. Patient Educ Couns. 2018;101(9):1669–1675. doi:10.1016/j.pec.2018.05.016
30. Thompson AC, Thompson MO, Young DL, et al. Barriers to follow-up and strategies to improve adherence to appointments for care of chronic eye diseases. Invest Ophthalmol Vis Sci. 2015;56(8):4324–4331. doi:10.1167/iovs.15-16444
31. Bresnick G, Cuadros JA, Khan M, et al. Adherence to ophthalmology referral, treatment and follow-up after diabetic retinopathy screening in the primary care setting. BMJ Open Diabetes Res Care. 2020;8(1):e001154. doi:10.1136/bmjdrc-2019-001154
32. Conlin PR, Fisch BM, Cavallerano AA, Cavallerano JD, Bursell SE, Aiello LM. Nonmydriatic teleretinal imaging improves adherence to annual eye examinations in patients with diabetes. J Rehabil Res Dev. 2006;43(6):733–740. doi:10.1682/jrrd.2005.07.0117
33. Stebbins K, Kieltyka S, Chaum E. Follow-up compliance for patients diagnosed with diabetic retinopathy after teleretinal imaging in primary care. Telemed J E-Health. 2021;27(3):303–307. doi:10.1089/tmj.2019.0264
34. Hatef E, Alexander M, Vanderver BG, Fagan P, Albert M. Assessment of annual diabetic eye examination using telemedicine technology among underserved patients in primary care setting. Middle East Afr J Ophthalmol. 2017;24(4):207. doi:10.4103/meajo.MEAJO_19_16
35. Keenum Z, McGwin G, Witherspoon CD, Haller JA, Clark ME, Owsley C. Patients’ adherence to recommended follow-up eye care after diabetic retinopathy screening in a publicly funded county clinic and factors associated with follow-up eye care use. JAMA Ophthalmol. 2016;134(11):1221–1228. doi:10.1001/jamaophthalmol.2016.3081
36. Basch CE, Walker EA, Howard CJ, Shamoon H, Zybert P. The effect of health education on the rate of ophthalmic examinations among African Americans with diabetes mellitus. Am J Public Health. 1999;89(12):1878–1882. doi:10.2105/ajph.89.12.1878
37. Callinan CE, Kenney B, Hark LA, et al. Improving follow-up adherence in a primary eye care setting. Am J Med Qual. 2017;32(1):73–79. doi:10.1177/1062860615616860
38. Mathenge W, Whitestone N, Nkurikiye J, et al. Impact of artificial intelligence assessment of diabetic retinopathy on referral service uptake in a low resource setting: the RAIDERS randomized trial. Ophthalmol Sci. 2022:100168. doi:10.1016/j.xops.2022.100168.
39. Medeiros FA, Alencar LM, Zangwill LM, Bowd C, Sample PA, Weinreb RN. Prediction of functional loss in glaucoma from progressive optic disc damage. Arch Ophthalmol. 2009;127(10):1250–1256. doi:10.1001/archophthalmol.2009.276
40. Chan HHL, Ong DN, Kong YXG, et al. Glaucomatous optic neuropathy evaluation (GONE) project: the effect of monoscopic versus stereoscopic viewing conditions on optic nerve evaluation. Am J Ophthalmol. 2014;157(5):936–944. doi:10.1016/j.ajo.2014.01.024
41. Jammal AA, Thompson AC, Mariottoni EB, et al. Human versus machine: comparing a deep learning algorithm to human gradings for detecting glaucoma on fundus photographs. Am J Ophthalmol. 2020;211:123–131. doi:10.1016/j.ajo.2019.11.006
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
