Back to Journals » Nature and Science of Sleep » Volume 16
Depression, Sleep Health & Sociodemographic Correlates in a Nationwide Survey: Implications for Depression Treatment During the COVID-19
Authors Chery MJ , Baral A , Rolle LD , Abdshah A, Bernard MJ, Poudel L, Francois L, Jones DL, Jean-Louis G , Blanc J
Received 6 September 2023
Accepted for publication 4 December 2023
Published 13 January 2024 Volume 2024:16 Pages 17—31
DOI https://doi.org/10.2147/NSS.S434148
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sarah L Appleton
Maurice Junior Chery,1 Amrit Baral,1 LaShae D Rolle,1 Alireza Abdshah,1 Maritza J Bernard,2 Laxmi Poudel,3 Laura Francois,1 Deborah L Jones,4 Girardin Jean-Louis,4 Judite Blanc4
1Department of Public Health Sciences, the University of Miami Miller School of Medicine, Miami, Florida, USA; 2Anne Bates Leach Eye Hospital at Bascom Palmer Eye Institute, the University of Miami Miller School of Medicine, Miami, FL, USA; 3South Florida Integrative Medicine, Miami, FL, USA; 4Department of Psychiatry and Behavioral Sciences, University of Miami Miller School of Medicine, Miami, FL, USA
Correspondence: Judite Blanc, Department of Public Health Sciences, the University of Miami Miller School of Medicine, 1120 NW 14th St, Room 1448, Miami, FL, 33136, USA, Tel +1 954 471 0739, Email [email protected] Maurice Junior Chery, Department of Public Health Sciences, the University of Miami Miller School of Medicine, 1120 NW 14th St, Room 1448, Miami, FL, 33136, USA, Tel +1 343 204 7128, Email [email protected]
Purpose: The COVID-19 pandemic has had a profound impact on mental health worldwide, with depression and sleep problems among the most common issues experienced by many individuals. Depression can lead to sleep problems, which can increase the risk of developing depressive symptoms. However, it is unclear which United States (US) sub-population was most affected by depression and sleep problems during the pandemic.
Methods: We conducted a secondary analysis using self-reported data from the 2021 National Health Interview Survey (NHIS), focusing on adults aged 18 years and above (n=29,763). We utilized self-reported responses to questions about prescription medication and frequency of depressive feelings to determine participants’ depression status. Appropriate weights were applied to account for the sampling design of the surveys. Our analysis involved descriptive statistics and chi-squared tests to compare sociodemographic, clinical, behavioral, and sleep-related characteristics between US adults with and without depression. Additionally, logistic regression was used to examine the associations between sleep duration, sleep quality and depression.
Results: The overall prevalence of depression in our sample was 44.4%. It were higher in certain demographic groups, including younger adults (18– 39 years, 47.7%), non-Hispanic whites (47.9%), females (50.1%), those at the lower income bracket (52.2%), those with no college or degree (48.7%) uninsured individuals (45.2%), and those reporting poor general health (71.9%). Individuals with depression had a 12% increased odds of experiencing short sleep (aOR: 1.12, 95% CI:1.04– 1.20, p< 0.001), 34% increased odds of experiencing long sleep (aOR: 1.34, 95% CI: 1.20– 1.50, p < 0.001) and more than 2.5 fold increased odds of reporting poor sleep quality (aOR:2.57, 95% CI: 2.40– 2.78; p< 0.0001). In the multivariate analysis, all variables (sex, race/ethnicity, education, health insurance coverage, marital status, general health status and use of sleep medications, smoking and alcohol use status) were significantly predictors of poor sleep quality, with the exceptions of age and family income.
Conclusion: The findings emphasize the need to address sleep health in treating depression, especially during times of public health crises.
Keywords: depression, sleep health, sleep hygiene, sleep disparities, sleep quality, COVID-19
Introduction
The COVID-19 pandemic, declared by the World Health Organization in March 2020, has profoundly impacted global health, extending beyond the direct effects of the SARS-CoV-2 virus.1 In the US, the scenario during the NHIS 2020 was marked by escalating case numbers, stretching healthcare systems and leading to implementation of varying degrees of restrictions and lockdowns across different states to curb the virus spread.2,3 According to the Centers for Disease Control and Prevention (CDC), by the end of 2020, the US had reported over 20 million cases and more than 350,000 deaths attributed to COVID-19.4 To adapt to the evolving conditions and ensure the safety of both respondents and interviewers, the NHIS adjusted its data collection strategy, transitioning from in-person interviews to an online format, an adaptation that was pivotal in the continuity of the survey amidst the pandemic conditions.5 While the immediate physical health impacts have been widely studied, the pandemic’s mental health consequences, specifically depression and sleep outcomes, are becoming increasingly apparent.6 Depression is a pervasive global health issue, affecting over 5% of adults and experiencing a marked increase in incidence over the past decade.7 According to the National Institute of Mental Health (NIMH), an estimated 19.4 million adults in the United States had at least one major depressive episode in 2019, and the prevalence continue to rise to nearly one in ten Americans by the end of the year.8,9 These trends were exacerbated by the COVID-19 pandemic, culminating to a more than three-fold increase in the prevalence of depression among adults, as compared to pre-pandemic levels.10
Within the US, various studies have specifically focused on distinct demographics such as adolescents and university students. Collectively, these investigations have found depression prevalence rates averaging 36%, with specific studies reporting figures ranging from 10% to 48%.11–15 Studies conducted in China during the lockdown reflect a surge in mental health issues among university students, with the prevalence of anxiety and depression rising sharply.16,17 The lockdown, social isolation, and abrupt shift to online learning have heightened interpersonal sensitivity, exacerbating anxiety and depression levels.16 In addition, another research underlines the grave mental health implications of the pandemic and lockdown measures.18 These findings echoed in other international contexts, emphasizing the universal nature of these mental health challenges. Along with depression, sleep, which is also essential for overall well-being and physical and mental health, has been notably disrupted during the pandemic.10,19 A trend of decreasing sleep duration has been reported, with almost 70% of adults in the US reporting insufficient sleep for at least one night per month and more than a third experiencing sleep disturbances, which disproportionately affect non-Hispanic Blacks.20,21 Moreover, specific to the interaction between depression and sleep quality, another study among postgraduate students in China during the COVID-19 campus lockdown reveals a significant correlation between interpersonal sensitivity and depression, mediated and moderated by sleep quality.22 This highlights the intricate interplay between these factors, accentuating the need for a comprehensive examination of these dynamics in varied geographical and cultural contexts.
There is also a consequential association between depression and sleep health, where approximately 75% of individuals diagnosed with depression report sleep difficulties.23 This is a noteworthy association with significant consequences. However, the extent of this association during the unique circumstances of the COVID-19 pandemic has not been thoroughly examined on a large scale. Therefore, we used a population-based, nationally representative dataset, the National Health Interview Survey (NHIS), to examine the relationship between depression and sleep health during the COVID-19 outbreak.
Our study seeks to extend these insights, exploring the nuanced relationships between depression and sleep health in the context of the COVID-19 pandemic in the US, drawing parallels and distinctions with international findings. The outcomes of this study are aimed to contribute significantly to the global discourse on mental health, offering cross-cultural insights and evidence-based interventions to mitigate the ongoing and post-pandemic mental health crisis.
Materials and Methods
Data Source and Study Sample
We utilized data from the 2021 National Health Interview Survey (NHIS) collected by the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention (CDC). The NHIS is a cross-sectional survey conducted annually to collect data through in-person interviews with non-institutionalized civilians in the US using validated instruments.24,25 We used a sample of adults aged 18 years and older with depression (N=29,763 unweighted). All data for this study were sourced from the National Health Interview Survey (NHIS), with strict adherence to the privacy and data protection protocols as mandated by the National Center for Health Statistics (NCHS), ensuring confidentiality and security of participant information through encryption and secure server storage, in compliance with relevant privacy legislation and NCHS guidelines.26 In accordance with the definition of a “human subject” outlined in 45 CFR 46.102(e), our research was determined to not involve human subjects.27 As a result, the study was exempt from the need for IRB review, approval, or oversight.
Variables Definition
In our study, the major dependent variables were nightly sleep duration and sleep quality. Sleep duration, measured through the National Health Interview Survey (NHIS) question “On average, how many hours of sleep do you get in 24 hours?”, was categorized into three levels: short sleep (less than 7 hours), normal sleep (7–8 hours), and long sleep (9 hours or more), based on existing literature.28
According to a recently published study29 that utilized NHIS data, sleep quality was assessed using a binary variable based on responses to four NHIS questions: (a) Did you have trouble falling asleep in the past 30 days? (b) Did you have trouble staying asleep in the past 30 days? (c) Did you wake up feeling not well-rested in the past 30 days? And (d) Did you take any medication to help you fall asleep or stay asleep in the past 30 days? The responses were in the form of Yes/No. If any of the indicators were reported as “Yes”, the overall sleep quality was categorized as poor.
The independent variable in our study is self-reported diagnosis of depression. To assess the current depression status, we constructed a depression status variable based on the responses to two self-questions. Participants were asked the following questions: 1. “Do you take prescription medication for depression?” with response options (yes/no). 2. “How often do you feel depressed?” with response choices including daily, weekly, monthly, a few times a year, or never. It’s important to note that if participants responded with daily, weekly, monthly, or a few times a year, it was interpreted as a “Yes” answer. Individuals who answered affirmatively to either of these two questions were classified as having depression. In the context of this paper, we will use the term “Depression” for brevity. However, it should be noted that when we refer to “Depression”, we are specifically referencing the “Self-reported diagnosis of depression”.
Other potential confounders and covariates, such as demographic characteristics (age group in years, sex, race/ethnicity, education, family income, health insurance, and marital status), clinical characteristics (general health status and use of sleep medications), and behavioral variables of interest (smoking and alcohol use status) were included in our analysis.
Statistical Analysis
First, we used descriptive statistics and chi-squared tests to examine the differences in the distribution of sociodemographic, clinical, behavioral, and sleep-associated characteristics among US adults by depression status (Table 1).
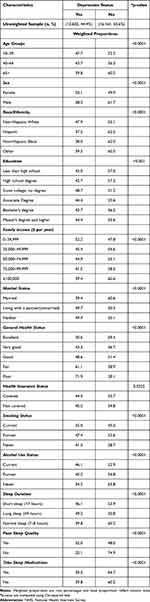 |
Table 1 Prevalence (Weighted Percentage) of Self-Reported Depression Among US Adults by Sociodemographic, Behavioral, Clinical, and Sleep Characteristics, 2021 NHIS |
Second, we used multivariable multinomial logistic regression to assess the odds of reporting short or long sleep compared to normal sleep among those with depression, as summarized in (Table 2).
 |
Table 2 Weighted and Adjusted Odds Ratios for Nightly Sleep Duration Associated with Self-Reported Diagnosis of Depression Using Multivariate Multinomial Logistic Regression Analysis, 2021 NHIS |
Next, we used univariable binary logistic regression to examine the association between depression and three variables related to the quality of sleep (Table 3).
 |
Table 3 Univariable and Multivariable Binary Logistic Regression Analysis Assessing the Predictors of Poor Sleep Quality, 2021 NHIS |
In our analytic approach, we incorporated variables that were identified as statistically significant predictors from the univariable analyses. Additionally, variables that were biologically and theoretically plausible were considered for inclusion in the multivariable regression models, ensuring a comprehensive and robust analysis.
Appropriate survey sampling weights provided by the NHIS were used as the basis for all analyses. All statistical tests were two-tailed, with an alpha less than 0.05 considered statistically significant, and SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA)30 was used for statistical analysis. All participants provided informed consent at registration, and the available data were de-identified.
Results
The analysis was based on a sample of 29,763 (unweighted) adults, with a mean age of 43 years (SD=10). The weighted total sample revealed that 44.4% of participants with depression (Table 1).
Sociodemographic Characteristics
The prevalence of depression decreases with age. Individuals aged 65 years and above had the lowest proportion (39.8%), whereas those aged 18–39 had the highest proportion (47.7%). Females (50.1%) reported a higher prevalence of depression than males (38.3%). Non-Hispanic Whites (47.9%) had a higher depression prevalence, followed by Blacks (38.0%), and Hispanics (37.5%). Individuals with high school degree reported the lowest proportion of depression (42.7%), while participants with some college, no degree reported having the highest proportion of depression (48.7%). When examining income, we observed a higher prevalence of depression (52.2%) among individuals in the lowest-income bracket ($0–34,999). In general, the reported depression proportion decreased as income increased. Those earning more than $100,000 reported the lowest prevalence of depression (39.4%). Furthermore, those without health insurance reported a higher depression proportion (45.2%) than those with health insurance coverage (44.3%). Participants living with a partner (49.7%) and single individuals (49.9%) reported higher depression than did married participants (39.4%). There was a dose-response relationship between general health status and the prevalence of depression, where those with poor general health status reported 71.9% prevalence of depression.
Behavioral and Clinical Characteristics
Current smokers (55.0%) reported a higher prevalence of depression than former smokers (47.4%) and nonsmokers (41.3%). Similarly, the prevalence of depression was highest among current alcohol users (46.1%), followed by former (45.2%) and non-drinkers (34.2%).
Sleep Characteristics
The prevalence of depression was highest (49.2%) among those who were long sleepers (≥9 hours), followed by short sleepers (<7 hours) (46.1%), compared to normal sleepers (7–9 hours) (39.8%). Individuals with poor sleep quality reported having higher prevalence of depression (52.0%) as compared to those without poor sleep quality (25.1%).
Regression Analyses: Association Between Depression and Sleep Health
Nightly Sleep Duration
We conducted a multivariable multinomial logistic regression analysis to assess the relationship between night sleep duration and depression. The weighted and adjusted odds ratios (aORs) derived from this analysis are presented in Table 2. Individuals with depression had higher odds of experiencing short sleep (aOR: 1.12, 95% CI:1.04–1.20, p <0.01) and even greater odds of having long sleep (aOR: 1.34; 95% CI:1.20–1.50; p < 0.001) in reference to normal sleep, than individuals without depression. Compared to people aged 65 years and older, those age range–18–39 and 40–64 were less likely to experience long sleep, with odds ratios (aOR:0.69, 95% CI:0.60–0.81, p < 0.0001) and (aOR: 0.50, 95% CI:0.50–0.63, p < 0.0001), respectively. Regarding gender differences, females had lower odds of being short sleepers (aOR: 0.84, 95% CI:0.78–0.90, p < 0.0001) compared to males. Non-Hispanic Blacks had a markedly greater likelihood of experiencing short sleep (aOR:1.40, 95% CI: 1.23–1.55, p < 0.0001) compared to their non-Hispanic White counterparts.
Current smokers had a higher likelihood of short sleep (aOR:1.16; 95% CI:1.04–1.30, p < 0.01) than non-smokers. Alcohol users, both current (aOR: 1.40, 95% CI: 1.24–1.58, p<0.0001) and former (aOR: 1.42, 95% CI: 1.24–1.63, p<0.0001) had 40% and 42% greater odds of having short sleep as compared to non-drinkers respectively. Those with poor sleep quality had 67% greater odds of having short sleep (aOR: 1.67, 95% CI: 1.55–1.80, p<0.0001) and 13% lower odds of experiencing long sleep (aOR: 0.87, 95% CI: 0.76–0.99, p=0.0363) as compared to those without poor sleep quality.
Sleep Quality Outcomes
The results from both univariable and multivariable binary logistic regression models, which assess the association between depression and poor sleep quality as well as evaluate other predictors of poor sleep quality, are presented in Table 3. In the univariable analysis, factors such as age, sex, race/ethnicity, education, family income, marital status, general health status, health insurance, smoking, alcohol use, and sleep duration all demonstrated a statistically significant association with poor sleep quality. Consequently, we incorporated these variables into the multivariable logistic regression analysis. In the multivariable model, individuals who reported depression were over twice as likely to experience poor sleep quality (aOR: 2.57, 95% CI: 2.40–2.78, p < 0.0001). When comparing short sleep duration to normal sleep duration, there was a 67% increase in the odds of having poor sleep quality (aOR: 1.67, 95% CI: 1.55–1.81, p<0.0001). In the univariable analysis, the 18–39 age group had slightly lower odds (OR: 0.89, 95% CI: 0.82–0.97, p<0.01) of short sleep than those aged 65 and older. However, this association was not statistically significant in the adjusted analysis. Females had almost 50% greater odds (aOR: 1.49, 95% CI: 1.39–1.60, p<0.0001) of experiencing poor sleep quality as compared to males The results also showed significant differences among ethnicities: Non-Hispanic Blacks had notably lower odds (aOR: 0.66, 95% CI: 0.58–0.74, P<0.0001) of poor sleep quality, followed by Hispanics (aOR: 0.69, 95% CI: 0.62–0.77, p<0.0001) when compared to non-Hispanic Whites.
Current smokers were 20% more likely (aOR: 1.20, 95% CI: 1.06–1.36, p<0.01) to have poor sleep quality than non-smokers. Both current and former alcohol users reported greater odds of poor sleep quality. Specifically, current alcohol users had a 56% increased chance (aOR: 1.56, 95% CI: 1.38–1.75, p < 0.0001), while former drinkers had 40% higher odds (aOR: 1.40, 95% CI: 1.21–1.60, p < 0.0001) than non-drinkers. Lastly, those who were married had a slightly better sleep quality (aOR: 0.90, 95% CI: 0.83–0.98; p=0.0139) compared to those who were single or not living with a partner.
Discussion
This study aimed to investigate the relationship between depression and sleep outcomes during the COVID-19 pandemic. We found a strong association between depression and sleep health in a nationally representative sample of adults during the COVID-19 pandemic period. The prevalence of depression in our sample was 44.4%, and was significantly affected by sleep duration and quality. In our sample, individuals with depression had a 12% higher likelihood of experiencing short sleep, 34% higher odds of experiencing long sleep durations and were more than 2.5 more likely to experience poor sleep quality. Our findings align with data from a nationally represented survey indicates that the prevalence of depression in the US surged to over three times its previous rate during the COVID-19 pandemic compared to the period before its onset.31,32 Our results are also consistent with a nationwide study from Brazil, which reported a 28% rise in sleep duration issues and a significant 32% upswing in sleep quality problems during the COVID-19 pandemic.33 A 2020 study from a Kentucky University and data from Texas A&M University both reported a depression prevalence rate of around 36%.11,12 Similarly, during China’s lockdown, 46.8% noted depression symptoms, highlighting the significant increase in depression during such conditions.16 In the context of broader research, our findings align seamlessly with prior studies that have underscored the disruption of sleep patterns in individuals with depression.34–36 Such disturbances in sleep are characteristic features of depression and are often associated with diminished activity in the serotoninergic neurotransmission system.34–36
Sleep influences an array of physiological functions, impacting everything from transient metabolic responses to sustained neurocognitive adaptations.37 One crucial aspect of sleep research is the delineation of normal sleep durations. Contemporary research posits that a sleep duration of 7–8 hours is generally conducive to positive health outcomes.38 Our study corroborates this finding, demonstrating that sleep durations at either extreme, too short, or excessively long, were associated with depression. Furthermore, it is critical to note that sleep quality is as important as sleep quantity, with evidence suggesting that interventions specifically targeting sleep quality might benefit patients more than those focusing solely on sleep duration.39
Depression is a multifaceted condition that profoundly influences individuals’ overall health and functional capacity of individuals.40 It has a complex bidirectional relationship with numerous physical and psychological disorders, serving as both a contributor and consequence.40 Depression and sleep disturbances share many pathophysiological mechanisms, and ameliorating depression often mitigates sleep disturbances, reinforcing this interconnectedness.35 Despite the historical view of sleep disturbances as merely symptomatic manifestations of depression, the current understanding identifies this relationship as bidirectional.41 While depression is a known risk factor for insomnia, recent research suggests that insomnia can also act as a precursor to the subsequent development of depression.41,42 This interplay presents a promising focal point for targeted intervention.
Older age is often linked to shorter sleep outcomes in the existing literature as it is associated with physiological changes, higher rates of chronic illnesses, and lifestyle factors leading to disrupted sleep patterns.43 However, our study found that younger individuals (18–39 years) accounted for a higher proportion of depression than their older counterparts did. Studies like that of Xu offer parallels, illuminating mental health struggles among younger Chinese college students during the COVID-19 lockdown.17 These findings diverge from conventional patterns in mental health research, implying that older adults may encounter more disruptions in their mental health.44 The COVID-19 pandemic has brought about significant disruptions to daily life, and has profoundly affected mental health and, by extension, sleep health.45 Younger individuals, particularly those between the ages of 18–39, have been confronted with many unique stressors.32 Many have faced job insecurity owing to layoffs, furloughs, or the transition to remote work and education.46,47 In addition, social isolation resulting from lockdowns and physical distancing measures could exacerbate feelings of loneliness and psychological distress, leading to increased rates of depression.48
Furthermore, young adults are notably active on social media and other digital platforms that are rife with COVID-19-related content.49,50 Overconsumption of pandemic-related news, often referred to as “doomscrolling”, could have led to increased stress, anxiety, and depressive symptoms.51 These findings underscore the need for targeted mental health interventions for younger adults, especially in the context of a public health crisis such as the COVID-19 pandemic.
Our study is in line with the gender disparity in depression rates, with females reporting a higher prevalence of depression than males. This aligns with the existing literature, which has consistently indicated that females experience depression at a higher rate than males.52 An interesting difference was observed in the present study in terms of sleep health outcomes. Females had 16% lower odds of experiencing short sleep duration; they had a 49% higher likelihood of having poor sleep compared to their male counterparts. This distinction suggests that while females may achieve the recommended hours of sleep, the quality of sleep may be compromised, potentially due to difficulties in initiating and maintaining sleep. This is consistent with prior research that found that women report poorer sleep despite similar or longer sleep durations than men.53 Biological factors, such as hormonal changes during the menstrual cycle, pregnancy, and menopause, can affect mood and sleep patterns in women.54 Psychologically, women are more likely to ruminate during stressful events that can lead to depression and sleep disturbances.55 Socially, the added stressors and demands that women face, such as caregiving and work-life balance issues, can also contribute to higher rates of depression and disrupted sleep.56 Nevertheless, it is crucial to emphasize the need for further studies to confirm these findings. A better understanding can inform the development of gender-tailored interventions to address depression and sleep health problems, particularly in stressful situations, such as the COVID-19 pandemic.
Our results found that Non-Hispanic Whites, comprising approximately 2/3 of our sample size, had the highest prevalence of depression (47.9%) and reported 31% higher odds of poor sleep quality than Non-Hispanic Blacks and Hispanics. This deviates significantly from prior research that often emphasizes higher sleep disturbances among racial/ethnic minorities, particularly non-Hispanic Blacks.57 It’s essential to underscore that “taking medication for depression symptoms” was a key metric in our assessment of depression prevalence. This raises a pertinent point: the increased prevalence among Non-Hispanic Whites could be indicative of their comparatively greater access to healthcare systems and thus, to prescribed medications for depression.58 One of the pronounced elements was the intensified sense of social isolation that seemed to disproportionately affect Non-Hispanic Whites. Given the cultural and societal structures they predominantly inhabit, such as living alone or in smaller nuclear families, the brunt of social distancing and lockdown measures may have been felt more acutely by this group.59 On the other hand, racial and ethnic minorities often benefit from intrinsic cultural and community support systems.59 These networks, characterized by strong familial ties and close-knit communities, have historically played a role in resilience against external stressors. In the context of the pandemic, such protective communal bonds could have been instrumental in cushioning the adverse impacts of isolation and providing a supportive framework to navigate the challenges, thereby potentially offsetting the rates of depression and sleep disturbances seen in other groups.
We observed a higher prevalence of depression among individuals with some college level education (48.7%). These results mirror the existing literature that identifies lower educational attainment as a risk factor for poor mental health outcomes, likely exacerbated during the pandemic by factors such as job instability and exposure risk associated with lower-skilled jobs.60,61 Participants with a (associate, bachelor, master or higher) degree reported the lower rate of depression, which might be attributed to a range of protective factors such as larger social networks, greater financial stability, and increased access to resources, including the ability to work remotely.62 Remote work accessibility has been predominantly available to higher-educated individuals, potentially shielding them from the economic and psychological impacts of the pandemic.62 Participants in the lowest-income bracket ($0–34,999 / year) exhibited a higher rate of depression (52.2%). The COVID-19 pandemic has been especially straining for low-income individuals, intensifying mental health problems.63 Finally, those without health insurance coverage reported a slightly higher rate of depression (45.2%) than those who were insured (44.3%). This could be a result of underreporting because those without coverage might be less likely to seek help and be diagnosed.64
Limitations and Strengths
We acknowledge several limitations in our study that are essential to consider when interpreting the results. Our study’s conclusions are primarily reliant on self-reported data from participants rather than direct medical evaluations, necessitating caution during their interpretation and application in a clinical context. In addition to the reliance on self-reported data, the cross-sectional design of our study is another limitation. This design inherently limits our ability to establish causal relationships between depression and sleep disturbances.
Despite these limitations, our study offers significant value using a nationally representative sample of the US population, which enables a thorough examination of self-reported depression status, sleep disturbances and sociodemographic factors. Robust and diverse sample sizes enhance the applicability and relevance of our findings.
Conclusion
This study emphasizes the well-documented association between depression and sleep health outcomes during the COVID-19 pandemic. Findings show that younger individuals, women, people of different racial and ethnic backgrounds, and socioeconomic statuses face unique challenges. Our results challenge various traditional views in mental and sleep health research, revealing a complex interplay between demographic and socioeconomic factors and mental health during the pandemic. Recognizing these patterns is crucial for clinicians and policymakers. It suggests a need for specialized interventions tailored to the needs of these specific populations. Furthermore, our results accentuate the importance of continuous research in this domain to ensure effective strategies are in place to support mental and sleep health, especially in times of crises.
Funding
The National Institutes of Health (NIH) National Heart, Lung, and Blood Institute (NHLBI) Determinants of Insufficient Sleep among Blacks and Effects on Disparities in Health Outcomes (ESSENTIALS; R01HL142066-06) and Mechanisms of sleep deficiency and effects on brain injury and neurocognitive functions among older blacks (MOSAIC; R01AG067523-05).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio Medica Atenei Parm. 2020;91(1):157–160. doi:10.23750/abm.v91i1.9397
2. Gabriel JM. National Coronavirus lockdowns: the interplay of tightening and easing. SSRN Electr J. 2020. doi:10.2139/ssrn.3732059
3. ptpmcrender.pdf. Available from: https://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC7286282&blobtype=pdf.
4. Shumskaya M, Benjamin S, Niepielko MG, Lorusso N. Statistics with Epidemiology of COVID-19; 2021. doi:10.25334/H1HE-5Z05
5. Blumberg SJ, Parker JD, Moyer BC. National Health Interview Survey, COVID-19, and online data collection platforms: adaptations, tradeoffs, and new directions. Am J Public Health. 2021;111(12):2167–2175. doi:10.2105/AJPH.2021.306516
6. Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi:10.1016/j.jad.2020.08.001
7. Santomauro DF, Mantilla Herrera AM, Shadid J. COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet Lond Engl. 2021;398(10312):1700–1712. doi:10.1016/S0140-6736(21)02143-7
8. Santo L, Peters ZJ, DeFrances CJ. Emergency department visits among adults with mental health disorders: United States, 2017–2019. NCHS Data Brief. 2021;426:1–8.
9. Goodwin RD, Dierker LC, Wu M, Galea S, Hoven CW, Weinberger AH. Trends in US depression prevalence from 2015 to 2020: the Widening Treatment Gap. Am J Prev Med. 2022;63(5):726–733. doi:10.1016/j.amepre.2022.05.014
10. Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials. Sleep Med Rev. 2021;60:101556. doi:10.1016/j.smrv.2021.101556
11. Wang X, Hegde S, Son C, Keller B, Smith A, Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. 2020;22(9):e22817. doi:10.2196/22817
12. Lee J, Jeong HJ, Kim S. Stress, Anxiety, and Depression Among Undergraduate Students during the COVID-19 Pandemic and their Use of Mental Health Services. Innov High Educ. 2021;46(5):519–538. doi:10.1007/s10755-021-09552-y
13. Rudenstine S, McNeal K, Schulder T, et al. Depression and anxiety during the COVID‐19 pandemic in an urban, low‐income public university sample. J Trauma Stress. 2021;34(1):12–22. doi:10.1002/jts.22600
14. Liu CH, Zhang E, Wong GTF, Hyun S, Hahm H. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for US young adult mental health. Psychiatry Res. 2020;290:113172. doi:10.1016/j.psychres.2020.113172
15. Hawes MT, Szenczy AK, Klein DN, Hajcak G, Nelson BD. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol Med. 2022;52(14):3222–3230. doi:10.1017/S0033291720005358
16. Xu H, Wang Z, Peng L, Mi Y, Zeng P, Liu X. The study of psychological traits among Chinese college students during the COVID-19 campus lockdown. Front Psychol. 2022;13. doi:10.3389/fpsyg.2022.1051770
17. Xu H, Pei Y, Yong Z, Liu X, Wang W. Pathway from interpersonal sensitivity to depression among Chinese college students during the COVID-19 campus lockdown. Environ Health Prev Med. 2023;28:34. doi:10.1265/ehpm.22-00249
18. Zhang X, Liu X, Mi Y, Wang W, Xu H. Resilience and depressive symptoms mediated pathways from social support to suicidal ideation among undergraduates during the COVID-19 Campus Lockdown in China. Psychol Res Behav Manag. 2022;15:2291–2301. doi:10.2147/PRBM.S377158
19. Lippman S, Gardener H, Rundek T, et al. Short sleep is associated with more depressive symptoms in a multi-ethnic cohort of older adults. Sleep Med. 2017;40:58–62. doi:10.1016/j.sleep.2017.09.019
20. Sheehan CM, Frochen SE, Walsemann KM, Ailshire JA. Are U.S. adults reporting less sleep?: findings from sleep duration trends in the National Health Interview Survey, 2004–2017. Sleep. 2018;42(2):zsy221. doi:10.1093/sleep/zsy221
21. Jean-Louis G, Turner AD, Seixas A, et al. Epidemiologic methods to estimate insufficient sleep in the US population. Int J Environ Res Public Health. 2020;17(24):9337. doi:10.3390/ijerph17249337
22. Liu X, Peng L, Wang Z, Zeng P, Mi Y, Xu H. Effects of interpersonal sensitivity on depressive symptoms in postgraduate students during the COVID-19 pandemic: psychological capital and sleep quality as mediators. Front Psychiatry. 2023;14. doi:10.3389/fpsyt.2023.1100355
23. Nutt D, Wilson S, Paterson L. Sleep disorders as core symptoms of depression. Dialogues Clin Neurosci. 2008;10(3):329–336. doi:10.31887/DCNS.2008.10.3/dnutt
24. Zablotsky B, Lessem SE, Gindi RM, Maitland AK, Dahlhamer JM, Blumberg SJ. Overview of the 2019 national health interview survey questionnaire redesign. Am J Public Health. 2023;113(4):408–415. doi:10.2105/AJPH.2022.307197
25. NHIS. 2020 NHIS; 2022. Available from: https://www.cdc.gov/nchs/nhis/2020nhis.htm.
26. NHIS. About the National Health Interview Survey; 2020. Available from: https://www.cdc.gov/nchs/nhis/participants/yourprivacy.htm.
27. 45 CFR 46.102 -- Definitions for purposes of this policy. Available from: https://www.ecfr.gov/current/title-45/part-46/section-46.102.
28. Heslop P, Smith GD, Metcalfe C, Macleod J, Hart C. Sleep duration and mortality: the effect of short or long sleep duration on cardiovascular and all-cause mortality in working men and women. Sleep Med. 2002;3(4):305–314. doi:10.1016/S1389-9457(02)00016-3
29. Inam M, Kianoush S, Sheikh S, et al. The association between race, ethnicity and sleep quality and duration: a National Health Interview Survey Study. Curr Probl Cardiol. 2023;48(12):102004. doi:10.1016/j.cpcardiol.2023.102004
30. Rodriguez RN. Sas. WIREs Comput Stat. 2011;3(1):1–11. doi:10.1002/wics.131
31. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open. 2020;3(9):e2019686. doi:10.1001/jamanetworkopen.2020.19686
32. Jahrami H, BaHammam AS, Bragazzi NL, Saif Z, Faris M, Vitiello MV. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2021;17(2):299–313. doi:10.5664/jcsm.8930
33. Moreno CR, Conway SG, Assis M, et al. COVID-19 pandemic is associated with increased sleep disturbances and mental health symptoms but not help-seeking: a cross-sectional nation-wide study. Sleep Sci. 2022;15(1):1–7. doi:10.5935/1984-0063.20220027
34. Adrien J. Neurobiological bases for the relation between sleep and depression. Sleep Med Rev. 2002;6(5):341–351. doi:10.1053/smrv.2001.0200
35. Thase ME. Depression and sleep: pathophysiology and treatment. Dialogues Clin Neurosci. 2006;8(2):217–226. doi:10.31887/DCNS.2006.8.2/mthase
36. Mayers AG, Baldwin DS. The relationship between sleep disturbance and depression. Int J Psychiatry Clin Pract. 2006;10(1):2–16. doi:10.1080/13651500500328087
37. Worley SL. The extraordinary importance of sleep. Pharm Ther. 2018;43(12):758–763.
38. Wyckoff S, Ford N, Waits K, Goulet H, Sherlin L. Sleep better, live better; 2021. Available from: https://getversus.com/s/Sleep-Better-Live-Better.pdf.
39. Bin YS. Is sleep quality more important than sleep duration for public health? Sleep. 2016;39(9):1629–1630. doi:10.5665/sleep.6078
40. Gaynes BN, Burns BJ, Tweed DL, Erickson P. DEPRESSION AND HEALTH-RELATED QUALITY OF LIFE. J Nerv Ment Dis. 2002;190(12):799. doi:10.1097/00005053-200212000-00001
41. Fang H, Tu S, Sheng J, Shao A. Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med. 2019;23(4):2324–2332. doi:10.1111/jcmm.14170
42. Steiger A, Pawlowski M. Depression and sleep. Int J Mol Sci. 2019;20(3):607. doi:10.3390/ijms20030607
43. Scullin MK, Bliwise DL. Sleep, cognition, and normal aging: integrating a half century of multidisciplinary research. Perspect Psychol Sci. 2015;10(1):97–137. doi:10.1177/1745691614556680
44. Lippe B, Hall B. Mental health disorders in older adult populations. In: Gatchel RJ, Schultz IZ, Ray CT editors. Handbook of Rehabilitation in Older Adults. Handbooks in Health, Work, and Disability. Springer International Publishing; 2018:243–261. doi:10.1007/978-3-030-03916-5_12
45. Clemente-Suárez VJ, Martínez-González MB, Benitez-Agudelo JC, et al. The impact of the COVID-19 pandemic on mental disorders. a critical review. Int J Environ Res Public Health. 2021;18(19):10041. doi:10.3390/ijerph181910041
46. Allmang S, Plummer JA, Copeland V, Riascos MC. Untangling the effects of COVID-19 on youth employment: directions for social work research. J Soc Soc Work Res. 2022;13(3):433–439. doi:10.1086/720981
47. Ganson KT, Tsai AC, Weiser SD, Benabou SE, Nagata JM. Job insecurity and symptoms of anxiety and depression among US young adults during COVID-19. J Adolesc Health. 2021;68(1):53–56. doi:10.1016/j.jadohealth.2020.10.008
48. Ellis WE, Dumas TM, Forbes LM. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can J Behav Sci Rev Can Sci Comport. 2020;52(3):177–187. doi:10.1037/cbs0000215
49. Neavel C, Watkins SC, Chavez M. Youth, social media, and telehealth: how COVID-19 changed our interactions. Pediatr Ann. 2022;51(4):e161–e166. doi:10.3928/19382359-20220321-03
50. Tiffany Field P. Social media and mental health in youth during COVID-19: a narrative review. Int J Psychol Res Rev. 2021;4:54. doi:10.28933/ijprr-2021-08-2905
51. Gao J, Zheng P, Jia Y, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15(4):e0231924.
52. Seedat S, Scott KM, Angermeyer MC, et al. Cross-national associations between gender and mental disorders in the World Health Association world mental health survey. Arch Gen Psychiatry. 2009;66(7):785–795. doi:10.1001/archgenpsychiatry.2009.36
53. Mallampalli MP, Carter CL. Exploring sex and gender differences in sleep health: a Society for Women’s Health Research Report. J Womens Health. 2014;23(7):553–562. doi:10.1089/jwh.2014.4816
54. Williams NJ, Jean-Louis G, Ravenell J, et al. A community-oriented framework to increase screening and treatment of obstructive sleep apnea among blacks. Sleep Med. 2016;18:82–87. doi:10.1016/j.sleep.2015.07.019
55. Nolen-Hoeksema S. Emotion regulation and psychopathology: the role of gender. Annu Rev Clin Psychol. 2012;8(1):161–187. doi:10.1146/annurev-clinpsy-032511-143109
56. Maume DJ, Sebastian RA, Bardo AR. Gender, work-family responsibilities, and sleep. Gend Soc. 2010;24(6):746–768. doi:10.1177/0891243210386949
57. Rodriquez EJ, Livaudais-Toman J, Gregorich SE, Jackson JS, Nápoles AM, Pérez-Stable EJ. Relationships between allostatic load, unhealthy behaviors, and depressive disorder in U.S. adults, 2005–2012 NHANES. Prev Med. 2018;110:9–15. doi:10.1016/j.ypmed.2018.02.002
58. Caraballo C, Massey D, Mahajan S, et al. Racial and ethnic disparities in access to health care among adults in the United States: a 20-year National Health Interview Survey Analysis, 1999–2018. medRxiv. 2020;2020. doi:10.1101/2020.10.30.20223420
59. Taylor RJ, Chatters LM, Taylor HO, Carr D. Race and objective social isolation: older African Americans, Black Caribbeans, and Non-Hispanic Whites. J Gerontol B Psychol Sci Soc Sci. 2019;74(8):1429–1440. doi:10.1093/geronb/gby114
60. Belo P, Navarro-Pardo E, Pocinho R, Carrana P, Margarido C. Relationship between mental health and the education level in elderly people: mediation of leisure attitude. Front Psychol. 2020;11:11. doi:10.3389/fpsyg.2020.00573
61. Niemeyer H, Bieda A, Michalak J, Schneider S, Margraf J. Education and mental health: do psychosocial resources matter? SSM Popul Health. 2019;7:100392. doi:10.1016/j.ssmph.2019.100392
62. Orr AE, Savage T. Expanding access to and ensuring equity in the benefits of remote work following the COVID-19 pandemic. J Sci Policy Governance. 2021;18(4):1–8. doi:10.38126/JSPG180413
63. Li M, Zhou B, Hu B. Relationship between income and mental health during the COVID-19 pandemic in China. Int J Environ Res Public Health. 2022;19(15):8944. doi:10.3390/ijerph19158944
64. Walker ER, Cummings JR, Hockenberry JM, Druss BG. Insurance status, use of mental health services, and unmet need for mental health care in the United States. Psychiatr Serv Wash DC. 2015;66(6):578–584. doi:10.1176/appi.ps.201400248
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
