Back to Journals » Clinical Optometry » Volume 16
Comprehensive Primary Eye Care: A Comparison Between an In-Person Eye Exam and a Tele-Eye Care Exam
Authors Blais N , Tousignant B , Hanssens JM
Received 27 September 2023
Accepted for publication 16 December 2023
Published 5 January 2024 Volume 2024:16 Pages 17—30
DOI https://doi.org/10.2147/OPTO.S436659
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Mr Simon Berry
Nicolas Blais,1,* Benoit Tousignant,1,2,* Jean-Marie Hanssens1,*
1School of Optometry, Université de Montréal, Montréal, Québec, Canada; 2Department of Social and Preventive Medicine School of Public Health, Université de Montréal, Montréal, Québec, Canada
*These authors contributed equally to this work
Correspondence: Nicolas Blais, School of Optometry, Université de Montréal, Montréal, Québec, Canada, Tel +1-418-215-2741, Email [email protected]
Introduction: Proper access to primary eye care is essential in addressing vision impairment, and tele-eye care examinations are a promising solution that could facilitate this access in many rural or remote areas. Even though remote eye exams are becoming increasingly frequent, comprehensive tele-eye care exams are still limited by the lack of published data. The aim of this study is to compare a comprehensive tele-eye care exam with a gold standard in-person primary eye care exam with an emphasis on refractive measurements, ocular health assessment, confidence level of the eye care providers and patient satisfaction.
Methods: Sixty-six participants underwent two comprehensive eye exams performed by two eye care providers. One was a gold standard in-person exam, while the other was a remote exam performed by an eye care provider through videoconference. An overall patient satisfaction survey and a questionnaire for visual comfort with a trial frame from each modality were completed and the eye care providers scored their confidence level for each test. Exam results and diagnoses were compared between both modalities.
Results: Tele-refraction has a good to excellent agreement with in-person subjective refraction in terms of sphero-cylindrical power and best corrected visual acuity. There was no statistically significant difference for visual comfort between both modalities. The agreement between in-person and remote exams for ocular health assessment ranged from fair to almost perfect, but there was a low prevalence of ocular pathologies within the study sample. The confidence level of the eye care providers and patient satisfaction were statistically higher in-person.
Conclusion: Tele-eye care appears to be statistically and clinically non-inferior to in-person eye exams, especially for refraction, but the low prevalence of ocular pathologies somewhat limits the comparison of its efficacy for ocular health assessment. More studies on comprehensive tele-eye care exams are needed.
Keywords: primary eye care, tele-eye care, tele-ophthalmology, tele-optometry, tele-refraction
Introduction
Primary eye care is described by the American Academy of Ophthalmology as “the provision of appropriate, accessible, and affordable care that meets patients’ eye care needs in a comprehensive and competent manner”.1 Proper access to primary eye care is essential in addressing vision impairment, which represents a significant global financial burden estimated at $411 billion annually due to productivity losses.2,3 Fortunately, 90% of vision loss is preventable or treatable, with uncorrected refractive errors and cataracts being the leading causes of vision impairment and blindness, respectively.4 Unfortunately, even in high-income countries like Canada, access to primary eye care is suboptimal, or even non-existent, in many rural, remote or northern areas.5 Telemedicine is defined as the use of information and communication technologies to provide remote health care to patients and is a promising solution to improve access to primary eye care, especially in underserved regions of the world.6 For years now, it has been used as a complement or an alternative to in-person encounters between patients and eye care providers (ECPs) to screen for specific ocular diseases like diabetic retinopathy, glaucoma and age-related macular degeneration.7–9 However, traditional tele-eye care screening programs often exclude refraction and vision function assessment. Self-performed online vision tests are another type of service that cannot be considered comprehensive primary eye care, since they are unassisted and almost exclusively tested for visual acuity and sometimes subjective online self-refraction to deliver a spectacle prescription that will allow patients to buy glasses or contact lenses online afterward.10 The American Optometric Association states that
Direct-to-patient eye and vision-related applications may provide data related to elements of a comprehensive eye exam but do not constitute patient care and fragmentation of a comprehensive eye exam into components delivered independently is deleterious and deceptive to patients.10
The components of an eyecare evaluation have a complex interaction that may trigger different prioritizations of the components of this evaluation. Hence, it is vital to break each component down in order to discuss the core tenets of each portion of an eye exam.
Comprehensive eye exams are traditionally performed by ECPs in-person, but technological advances in tele-eye care in the last few years have enabled remote ones. This modality of eye exams implies that patients must go to a clinic where an in-clinic technician will assist the remote ECP to perform a hybrid comprehensive exam, which includes both asynchronous and synchronous telemedicine components.11 Although tele-eye care has rapidly gained popularity during the COVID-19 pandemic, the scientific literature on remote comprehensive eye exams does not reflect the extent of their new availability.12–14 Just like in practice, most published studies in tele-eye care focus on remote disease-specific screening, which means that only a few articles describe protocols that include all three elements of a comprehensive eye exam: refraction, visual function, and ocular health assessment.15,16 To date, articles on subjective tele-refraction have reported a statistically significant agreement between in-person and remote measurements, showing that remote manifest refraction appears to be equivalent to the in-person one.17–19 Lutz de Araujo et al did not compare both exam modalities, but they studied a tele-eye care strategy implemented in the public health system of southern Brazil and concluded that refractive errors were the conditions for which subjective tele-refraction had the best ability to fully managed remotely.20 There are even fewer studies on the remote assessment of visual function, but one study by Randhawa et al described in 2023 how tele-eye care had “fair agreement on near heterophoria but poor agreement on the break and recovery values of negative and positive fusional vergences” by Risley prism.21 They also concluded that the fused cross-cylinder for accommodative testing was not equivalent between the two exam modalities. In terms of remote ocular health assessment, studies often focus on the ability of tele-eye care to diagnose a specific eye disease rather than on its ability to identify ocular abnormalities during a comprehensive eye exam.22–24
Consequently, even though there are remote eye exams performed every day throughout the world, practice guidelines on comprehensive tele-eye care exams are limited by the lack of published data. Most of these guidelines mainly state that the ECP should respect the same standards of practice regardless of the eye care modality they are using to deliver care, which often ends up being subject to interpretation for the ECP using telemedicine.10,25,26
In order to contribute to practice guidelines for tele-eye care, the aim of this study is to compare a comprehensive tele-eye care exam with a gold standard in-person primary eye care exam with an emphasis on refractive measurements (refractive error, best corrected visual acuity (BCVA), visual comfort), ocular health assessment (agreement between test results and diagnoses), confidence level of the ECP and patient satisfaction.
Methods
The present study uses repeated-measure design to compare tele-eye care and in-person eye exams. Eye care-naive participants were recruited through social media for students of the University of Montreal, and they provided informed consent. Exclusion criteria were previous knowledge of primary eye care, acute ocular conditions or diseases and visual deficiency as defined by the Health Insurance Act (chapter A-29) of Quebec.27 Chronic diseases like diabetic retinopathy and glaucoma were not exclusion criteria. This study complies with the Declaration of Helsinki, and approval was obtained from the ethics committee of the Université de Montréal for health research (certificate CERC-21-030-D).
Each participant underwent two successive comprehensive eye exams, in a random order. One was an in-person gold standard eye exam performed by an EPC at the optometry clinic of the School of Optometry of the Université de Montréal. The other was a tele-eye care exam performed by a remote ECP (located in a different room at the same clinic) with the assistance of an in-clinic technician who was a final-year optometry student. Two investigator optometrists performed these exams and were randomly assigned to an exam modality for each participant to minimize the effect of inter-examiner variability.
Both exams were performed according to the clinical guidelines of the Ordre des Optometrists du Québec and the American Optometric Association and according to Clinical Procedures for Ocular Examination.16,28,29 The participants first underwent pre-testing with automated instruments performed by an optometric assistant: lensometry, auto-refraction, keratometry, non-contact tonometry, pachymetry, perimetry, fundus photography and optical coherence tomography of macula and optic nerve. The pre-testing results were sent to the electronic medical record used by both ECPs and were therefore a common starting point for both exams. The ECP performed every test of the in-person exam, while the remote ECP relied on the help of the in-clinic technician to execute testing, except for tests involving the digital phoropter. Some tests like case history, visual acuity and color vision were delegated completely to the technician since little clinical knowledge is needed to properly execute them, compared to cover test, extraocular motility (EOM) and pupillary reflexes that require clinical judgment and interpretation from the ECP. Thereby, the technician recorded videos of these tests and uploaded them on the tele-eye care platform of DigitalOptometrics™. All test results were added to the electronic medical record for the remote ECP to review along with the recorded videos before joining the exam using videoconferencing. The remote ECP then performed subjective refraction using a digital phoropter (see Figure 1) and observed the slit lamp live video of the anterior segments recorded by the in-clinic technician (see Figure 2), which allowed the ECP to instruct the technician during real-time video transmission when necessary. People in Figures 1 and 2 provided written informed consent for the images to be published. Tests for both comprehensive eye exams are listed in Table 1, with non-dilated fundoscopy being the only test that was only performed in-person.
 |
Table 1 Comprehensive Eye Exam Workflows |
 |
Figure 1 Remote ECP Set-Up During Tele-Refraction. |
 |
Figure 2 Desktop View of the Remote ECP During Slit Lamp Live Video Transmission. |
Upon completion of both exams, the participants completed a 5-Point Likert scale questionnaire including four questions on patient satisfaction between both exam modalities (see Supplementary Figure 1). Participants were also asked to choose their favorite eye care modality. Finally, the in-person ECP puts the subjective refraction BCVA results into trial frames. Using a randomized and double-blind design, meaning that neither the patient nor the in-clinic technician assisting the patient during the trials knew which trial frame contained the BCVA results from which exam, monocular distance LogMAR visual acuity was measured with both trial frames. Participants were then asked to walk and look at a distance of 6 m and visual comfort was then compared between both spectacle prescriptions using another 5-Point Likert scale questionnaire adapted from previous studies measuring patient satisfaction from spectacle correction (see Supplementary Figure 2).30–32 Participants were also asked to subjectively rank their overall subjective appreciation of both trial frame prescriptions. When needed, a spectacle prescription was issued to participants who completed both eye exams. Comparisons of binocular vision assessments (objective and subjective ocular alignment, sensory fusion, stereoscopic acuity, and accommodative testing) will be reported in a subsequent publication.
Data Analysis and Statistical Approach
Statistical analyses were performed using SPSS version 28.0.1.0.33 For refractive measurements (sphere, cylinder and axis), only right eyes were considered (n = 66 eyes).34,35 Sphere, cylinder and axis values were converted to power vectors spherical equivalent (Seq), J0 and J45 for statistical analyzes, as described by Miller.36 A Bland-Altman Plot was used to analyze the spherical equivalent between both modalities. Agreement for refraction and BCVA were compared using Intraclass Correlation Coefficients (ICC) since statistically equivalent results were expected between exam modalities.34,37 Wilcoxon signed-rank test was used to compare visual comfort questionnaires. For ocular health assessment, the results of the following tests were analyzed: entering distance visual acuity, color vision, EOM, pupillary reflexes, anterior segment, and posterior segment. Since the outcomes of these tests are qualitative and quantitative and have different units of measure, every normal test result, according to clinical norms, was categorized as “within normal limits” and was given a value of “0”, while abnormal results were categorized as “outside normal limits” and was given a value of “1”.29 Having every test result represented by a binomial variable of “0” or “1” to represent respect of clinical norms allowed the use of Krippendorff’s Alpha Coefficient.38 This analysis was used to compare, between both exam modalities, the ability to identify abnormal test results (“red flags”) using the same tests on the same participants, except for non-dilated fundoscopy. To compare the agreement for ocular health diagnoses, the authors developed an index of morbidity adapted to primary eye care, since no published study offered a way to grade the severity of a diagnosed or misdiagnosed ocular condition. The index of morbidity was used to classify diagnoses according to the follow-up or referral timeline planned by the ECP who made the diagnosis (see Table 2). The confidence levels of the ECP and patient satisfaction were analyzed using the Wilcoxon signed-rank test since statistically different results were expected between exam modalities.
 |
Table 2 Index of Morbidity of Ocular Health Diagnoses |
Results
Refractive Measurements
Sixty-six participants (aged 18–61 years, mean (SD) = 29.7 (10.6) y.o.) were included in the study. The dioptric range of spherical equivalent measured in-person was −8.75 to +2.63 D. Tele-refraction resulted in a median hyperopic overcorrection of +0.07 D. Figure 3 is a Bland–Altman plot showing the variability of spherical equivalent results differences between tele-refraction and in-person subjective refraction. The 95% limits of agreement are reported, as calculated using ±1.96 SD (0.26 D) from the mean difference of +0.07 D. 98.49% of all spherical equivalent differences are within the limits of agreement and a clinical tolerance interval ±0.50 D centered on the ideal mean difference of zero between methods is shown.19 The ICC indicates an excellent (>0.90) agreement between both exam modalities for right eye BCVA, spherical equivalent and for the power associated with a vertically oriented Jackson Cross-Cylinder (J0) and a good agreement (0.75–0.90) for the power associated with an obliquely held Jackson Cross-Cylinder (J45) (see Table 3). The visual comfort questionnaire included statements on quality of vision, presence of distortion, dizziness when walking and acceptability to wear prescription daily. The Wilcoxon signed-rank test showed no statistically significant difference between both trial frames for all four items (see Table 4). 8% of all participants strongly preferred the prescription obtained in-person against another 8% who strongly preferred the one obtained remotely. 30% slightly preferred the one obtained in-person, while 32% slightly preferred the one obtained remotely. 23% were neutral about which trial frame they preferred.
 |
Table 3 Power Vectors of Refractive Errors and BCVA Between in-Person and Tele-Eye Care Modalities |
 |
Table 4 Visual Comfort with Trial Frame Between in-Person and Tele-Eye Care Modalities |
 |
Figure 3 Bland-Altman Plot for the Agreement of Spherical Equivalent Measurements Between Tele-Refraction and In-Person Refraction. |
Ocular Health Assessment
According to the Krippendorff’s Alpha Coefficient, the agreement between “within normal limits” and “outside normal limits” was almost perfect for distance visual acuity (a = 0.857) and color vision (a = 1.000), substantial for anterior (a = 0.660) and posterior (a = 0.624) segments, and fair for EOM (a = 0.267).39 No statistical analysis of pupillary reflexes results was conducted since there were no “outside normal limits” result noted for this test throughout all examinations, regardless of the eye care modality (see Figure 4). Among all 30 ocular conditions diagnosed by the in-person ECP, two were classified as morbidity index 1, 20 as index 2, six as index 3 and two as index 4 (see Table 5) None of the participants presented with a condition that necessitated an immediate referral (morbidity index 5) to secondary or tertiary eye care. Since index 1 and 2 regroup conditions with very little risk of harming patients even if gone unnoticed by the ECP, the agreement for these conditions was compared to higher morbidity index conditions. An agreement of 86.4% was found for index 1 and 2 conditions and an agreement of 87.5% for indexes 3 and 4. Overall, only four out of 30 conditions were not diagnosed by the remote ECP, including three index 2 conditions (mostly mild dry eye disease) and one index 3 condition (inactive corneal pannus). However, the remote ECP also identified four conditions that were not diagnosed in-person, including mild dry eye, mild blepharitis, and suspicion of papilledema. Upon completion of both examinations, four patients would have been referred by the remote ECP for further investigation in secondary eye care for one case of narrow iridocorneal angles and three cases of papilledema suspects, for a total of four patients who could not be entirely managed through remote primary eye care. The in-person ECP ruled out one of these cases of suspicious papilledema when performing non-dilated fundoscopy and therefore referred the same three other patients for the same reasons, along with the case of inactive corneal pannus that was sent to the university dry eye clinic, for a total of four patients that could not be managed by in-person primary eye care alone.
 |
Table 5 Index of Morbidity of Ocular Health Diagnoses Agreement for Tele-Eye Care Compared to in-Person Eye Care |
 |
Figure 4 Percentage of Ocular Health Tests Results Outside of Clinical Norms. Abbreviations: VA, visual acuity; EOM, extraocular motility. |
Confidence Levels of the ECP and Patient Satisfaction
The in-person ECP had a mean (SD) confidence level of 5.00 (0.01) compared to 4.30 (0.05) for the remote ECP (see Table 6). The mean (SD) patient satisfaction for all four items, which included a level of trust in the accuracy of exam results, ease to communicate, ease to establish a trust relationship with the ECP and general satisfaction, was 4.95 (0.03) compared to 4.52 (0.08) for tele-eye care (see Table 7). The Wilcoxon signed-rank test revealed a statistically significant difference between the confidence levels of the in-person ECP and those of the remote ECP for each eye test (p < 0.001). It also showed that patient satisfaction was significant statistically different between both eye exams with a p-value lower than 0.001 for every satisfaction criterion. Both the confidence levels of the ECP and patient satisfaction were higher for the in-person eye care modality.
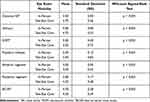 |
Table 6 Confidence Levels of ECPs for Ocular Health Tests Results |
 |
Table 7 Patient Satisfaction Levels |
Discussion
This study used a repeated-measure design to compare a remote eye exam with an in-person one. For refractive measurements, the results obtained with tele-refraction were statistically equivalent to in-person refraction. Tele-refraction induces a slight hyperopic overcorrection of +0.07 D in terms of spherical equivalence. Blais et al also found a slight hyperopic overcorrection of +0.08 D using a similar protocol, which is a good indicator of effective accommodation control during subjective refraction.17 Interestingly, a previous study by Randhawa et al that also used the DigitalOptometrics™ platform obtained a slight myopic overcorrection for tele-refraction, but in their study, tele-refraction was performed by a remote refractionist technician instead of a remote eye doctor, which could explain the myopic overcorrection.19 Overall, both refractive techniques were quite similar once the participant was placed behind the digital phoropter since they were both performed by an ECP using the same standardized procedure. Apart from the fact that the voice of the ECP was coming either from the room or from the videoconferencing system, there was very little difference between the technique of gold standard in-person subjective refraction and tele-refraction. The excellent agreement for BCVA correlates with the agreement of refractive measurements between both exam modalities, given that similar spectacle prescriptions should result in similar BCVA.
The only spherical equivalent difference laying outside the 95% limits of agreement can be explained by the fact that the participant had right-eye esotropia and amblyopia, which may have caused bi-ocular balance to fluctuate from one refraction to the other. It is also possible that patients with binocular vision disorders have wider fluctuations in their subjective refraction over small periods of time due to the stability of their accommodation. The chosen clinical tolerance interval is stricter in other studies comparing two types of subjective refraction, like one by Tousignant et al, but the “repeatability of refractive error measurements in clinical settings has a certain degree of variability”.32,40 Three studies investigating the inter-examiner reproducibility of non-cycloplegic subjective refractions showed 95% reproducibility limits for stigmatic data of ±0.74D in a study that included 99 cataractous, pseudophakic or healthy eyes, ±0.78D in a study with 40 optometrists who performed refraction on an asymptomatic low myope, and up to ±1.71D in a case of severe ametropia measured by 50 different optometrists.40–42 These findings on reproducibility of refractive measurements justify the choice of the ±0.50 D limits of non-inferiority for the Bland-Altman analysis.
Considering that a digital phoropter can be controlled as easily by an in-person ECP as by a remote one, tele-refraction really is not that different from in-person subjective refraction. Compared to cover test, EOM, pupillary reflexes and even slit lamp that have to be executed by a technician, tele-refraction allows the remote ECP to perform this test without assistance, using the same instrument and technique. Now that technology in primary eye care allows ECPs to provide subjective tele-refraction, it might be simply considered as another tool that facilitates the delivery of the same gold standard subjective refraction. Another promising alternative to in-person subjective refraction is a Conformité Européenne (CE) marked Web-based test that measures visual acuity and both spherical and cylindrical refractive errors. In their study, Wisse et al found that it was “valid and safe method for measuring the visual acuity and refractive error in healthy eyes, particularly for mild myopia”.43 Notwithstanding the fact that self-performed online refraction tests are unassisted and isolated from the rest of the comprehensive primary eye care eye exam, there might be more than one appropriate way to manage refractive errors remotely if such tools get properly incorporated into a comprehensive primary eye care model.
To the knowledge of the authors, there have previously been no study on the efficiency of delegating the technical part of collecting ocular health assessment results to technicians under the supervision of an ECP compared to an ECP performing the assessment alone. However, a study by Marmamula et al compared the efficacy of trained community eye‐health workers and teachers with reference to vision technicians for visual acuity screening and reported no significant difference in their agreement and diagnostic accuracy compared to those of the vision technician.44 The outcomes of their study indicate that, depending on the level of training of the technician, some exam results like visual acuity can remain accurate even when delegated to less experienced personnel. Another study by Paudel et al assessed the “clinical competency of 1-year trained vision technicians in detecting and referring causes of visual impairment in India” compared to an optometrist and found that these technicians competently detect and manage refractive errors and cataracts, but their referral decisions were incorrect in 21.6% of cases.45 Therefore, delegating interpretation of clinical results may lead to improper patient management, which is why an ECP must always supervise clinical encounters and make clinical decisions.
Entering distance visual acuity (a = 0.857) and color vision (a = 1.000) had an almost perfect agreement, which can be explained by the fact that these tests require little clinical judgment and are performed in the same way in-person and remotely, with the only difference being that they are delegated to the in-clinic technician in tele-eye care. The fact that the agreement was almost perfect between how many “outside normal limits” results were found in-person versus remotely indicates that these two tests may be safe enough for delegation when the in-clinic technician is trained properly.
For pupillary reflexes, the sample of participants did not include any pupil abnormality and therefore no statistical analysis was made. Even though tele-eye care did not identify any false-positive for pupillary reflexes, a larger sample including more pupil abnormalities would be necessary to better evaluate the efficacy of recorded videos for pupillary reflexes remote assessment. With the agreement for statistical equivalence between “within normal limits” and “outside normal limits” results being fair for EOM (a = 0.267), a McNemar analysis testing for statistical difference was performed and showed that there was no statistically significant difference for EOM (p = 0.063), even though statistical equivalence was not perfect. EOM was the test with the weakest agreement between exam modalities. Just like pupillary reflexes, the evaluation of EOM is subjective and subtle abnormalities can easily go unnoticed. Both these tests were filmed by in-clinic technician, but some technical issues made the asynchronous review by the ECP more challenging, which probably affected their confidence levels for these tests. Indeed, the angulation of the webcam was unstable from one participant to another since it was set up on a telescopic arm on the slit-lamp table to facilitate its placement in front of the participant sitting in the exam chair. The automatic focus feature of the webcam made it hard to maintain proper focus on the eye of the participants when the transilluminator or the ruler entered the field of view of the camera. Dark-pigmented irises were also easily saturated by the transilluminator during pupillary reflexes, which lowered the contrast between the iris and the pupil. Due to these filming issues, live videorecording might be more appropriate to try and address technical issues as they arise. The ECP could tell the technician when the point of view of the webcam is suboptimal for him to correct right away when possible. Even though an infrared webcam could address the image saturation issue for pupillary reflexes, a more objective way to evaluate EOM and pupils would probably be more reliable than recorded videos. In fact, since these two tests can be tricky to perform even by an in-person ECP, the automatization of these tests using objective measurements with instruments would be even more useful in tele-eye care where the data acquisition is complex and technician-dependent. It would simplify delegation and technician training as well as data review by possibly allowing automated comparison with a normative database. An eye-tracker system capable of detecting subtle motility restriction could possibly increase the efficacy of tele-eye care examinations, although none has been commercialized for this exact purpose so far. Binocular pupillometry would also be an objective and reliable addition to remote comprehensive eye exams. A study by Cohen et al found that a binocular pupillometer “detected clinically significant RAPDs with high sensitivity and specificity”.46
The anterior (a = 0.660) and posterior (a = 0.624) segments results had substantial agreement between exam modalities. Statistical equivalence represents the ability of slit-lamp evaluation and fundus photo analysis to identify “red flags” in terms of ocular health, which is crucial in order to identify as many ocular conditions as possible and to diagnose them properly. Even though the agreement is not perfect for these two tests, most conditions were properly diagnosed by the remote ECP. Just like for EOM, the McNemar analysis showed no statistically significant difference for both anterior (p > 0.999) and posterior (p > 0.999) segments. The agreement between both exam modalities is similar for lower and higher morbidity index conditions, but lower index conditions were much more prevalent in the study sample, especially for morbidity index 2 conditions. In terms of conditions that could not be managed remotely, just as many got referred for further investigation, either for an in-person follow-up or for referrals to secondary eye care. However, in addition to misdiagnosing three cases of mild ocular surface issues like mild dry eye, tele-eye care did not report an inactive corneal pannus that was reported by the in-person ECP and could not rule out a papilledema based only on the slightly blurred fundus photo. Once again, slit-lamp videos were reviewed asynchronously, but live videoconferencing might be more appropriate to optimize the ocular health assessment by allowing the remote ECP to guide the in-clinic technician through the slit-lamp routine when abnormalities are identified. The main limiting factor of this study in determining the efficacy of tele-eye care in ocular health assessment is the small prevalence of eye disease in our sample, especially for higher morbidity index diagnoses.
Regarding the perception of tele-eye care among ECPs and participants, it is interesting that both patients and doctors preferred the in-person examination even though exam outcomes were very similar, especially in terms of refractive measurements. A possible reason for the confidence level of the ECP to be higher in-person is the fact that both investigators were new to remote eye exams. Their level of confidence may have been influenced by their limited experience with tele-eye care. Also, patient satisfaction results should be interpreted considering that every participant lived in areas an urban area with easy access to primary eye care. It is unclear what level of appreciation patients from underserved areas would have towards tele-eye care. Some of these communities could show a high degree of interest in tele-eye care, but it could also be perceived as culturally inappropriate by some others like indigenous ones for instance.
Due to the exclusion criteria, this study offers no data on the efficacy of tele-eye care for pediatric patients, children, and low vision patients. The study sample size was also too small to include pupillary abnormalities. Another limitation is the fact that there are various tele-eye care platforms available and therefore many other ways to execute remote eye exams. The generalization of the results of this study is therefore limited to remote eye exams performed using a similar hybrid workflow to the one described, especially for video transmission that can be either synchronous or asynchronous. The training of the in-clinic technician also limited this study since it was probably not representative of the level of training of an in-clinic technician in a regular tele-optometry clinic in Canada. The final-year optometry student in this study may have been overqualified since opticians or optometric assistants without specific training in tele-optometry can work as in-clinic technicians in Canada. This might have increased the efficacy of the tele-eye care eye exam compared to a remote eye exam workflow that would involve an in-clinic technician with less training and knowledge on tele-optometry.
Although comprehensive tele-eye care exams have the potential to improve access to eye care, there are also limitations to this type of remote service. Its structure relies greatly on proper internet connection, making these exams technology-dependent since the stability and speed of the connection can alter the efficiency of the exam. In some remote areas with unstable connections, this may present as a barrier. This exam modality also requires the remote ECP to delegate many techniques to an on-site technician, even though technical knowledge and clinical judgment are necessary to perform some of the tests. Therefore, the level of training and experience of the technician might influence the quality of the data collection. Tests that require clinical judgement should be observed synchronously by the remote ECP to assure he or she can intervene during the tests to instruct the technician when necessary. This would allow the remote ECP to have more control over the quality of the data provided by the on-site technician. Another issue with tele-eye care is that some tests like dilated fundus examination or retinoscopy cannot be delegated or even recorded with videos as easily as other tests like cover test or slit lamp, which means that in-person encounters are inevitable in many cases, especially for young children.
Conclusion
This study aims to compare a comprehensive tele-eye care exam with a gold standard in-person primary eye care exam in terms of refractive measurements, visual comfort, ocular health assessment, confidence level of the ECP and patient satisfaction. It confirmed that tele-refraction is statistically and clinically non-inferior to in-person refraction and allows to remotely screen and manage vision impairment secondary to uncorrected refractive error, even though the study sample was limited due to the number of participants and the low prevalence of ocular pathologies. It also showed that tele-eye care allows remote ECPs to properly identify most of the clinical ocular health abnormalities encountered in the study as accurately as in-person eye exams, which led to similar diagnoses between both eye care modalities. However, ECPs were less confident when assessing patients remotely, just as patient satisfaction levels were higher for in-person exams. Even though tele-eye care is very technician-dependent, remote eye care providers should have the ability to guide the in-clinic technician when necessary and observe tests in real time, especially for the assessments that require more advanced training to perform properly or more clinical judgement to analyze. This study brought forward new data for stakeholders to consider regarding access to primary eye care. Additional studies on tele-eye care would increase the knowledge base on the potential of remote primary eye care exams, especially for binocular vision assessment, pediatrics and low vision patients and cost-effectiveness analysis. Future studies should aim towards recruiting larger samples of participants and do so within populations that are more likely to present ocular pathologies like in actual remote settings lacking access to primary eye care.
Acknowledgments
The authors would like to thank Fannie Brisson, OD, Anne-Marie Fontaine, OD, Claudelle Jolicoeur, OD, Emma Lamontagne, OD, Jolaine Primeau, OD, and Julien Leduc, final-year optometry student, for their precious help throughout this research project.
An abstract of this paper was presented at the 2022 ARVO Annual Meeting, held in Denver, CO, May 1–4, 2022, and virtually. This poster’s abstract was published in “Poster Abstracts” in Investigative Ophthalmology & Visual Science June 2022, Vol.63, 1387 – A0083:
https://iovs.arvojournals.org/article.aspx?articleid=2782352
Another abstract of this paper was presented at the 2022 AAO Annual Meeting, held in San Diego, CA, October 25–31, 2022, in-person. The poster’s abstract was not published in a Journal but can be found online in the Past Meeting Abstract Archives:
Funding
This study was supported by Mitacs and IRIS The Visual Group through the Mitacs Accelerate program. These sponsors were not involved in the stages from study design to submission of the paper.
Disclosure
Dr Nicolas Blais reports grants from Mitacs, Canadian Institutes of Health Research and IRIS The Visual Group, during the conduct of the study. The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
References
1. American Academy of Ophthalmology. Definition of primary eye care; 2014. Available from: https://www.aao.org/education/clinical-statement/definition-of-primary-eye-care--policy-statement#:~:text=Primary%20eye%20care%20is%20the,a%20lifetime%20of%20continuing%20care.
2. World Health Organization. Blindness and vision impairment; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment.
3. World Health Organization. World Report on Vision. Geneva: World Health Organization; 2019.
4. The international agency for the prevention of blindness. Causes of Vision Loss; 2023. Available from: https://www.iapb.org/learn/vision-atlas/causes-of-vision-loss/.
5. van Staden D. The universal eye health imperative for Canada: an inescapable reality of unmet need. Can J Public Health. 2020;111(4):627–630. doi:10.17269/s41997-020-00307-4
6. World Health Organization. Global Observatory for eHealth. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth. Geneva: World Health Organization; 2010.
7. Kapoor R, Yuksel-Elgin C, Patel V, et al. Detecting common eye diseases using the first teleophthalmology GlobeChek Kiosk in the United States: a pilot study. Asia-Pac J Ophthalmol. 2020;9(4):315–325. doi:10.1097/APO.0000000000000295
8. Selvin G, Joseph A. Chapter 2 - Comprehensive Eye Telehealth. In: Maa A, editor. Ocular Telehealth. Elsevier; 2023:7–15.
9. Yogesan K, Goldschmidt L, Cuadros J, Ricur G. Digital Eye Care and Teleophthalmology. Springer Cham; 2023.
10. American Optometric Association. Position statement regarding telemedicine in optometry; 2020. Available from: https://www.aoa.org/AOA/Documents/Advocacy/position%20statements/AOA_Policy_Telehealth.pdf.
11. Tan IJ, Dobson LP, Bartnik S, Muir J, Turner AW. Real-time teleophthalmology versus face-to-face consultation: a systematic review. J Telemed Telecare. 2016;23(7):629–638. doi:10.1177/1357633X16660640
12. Chong JC, Tan C-HN, Chen DZ. Teleophthalmology and its evolving role in a COVID-19 pandemic: a scoping. Ann Acad Med Singap. 2021;50(1):61–76. doi:10.47102/annals-acadmedsg.2020459
13. New Zealand Association of Optometrists. Practical Guidance for COVID-19 Level Three. New Zealand: New Zealand Association of Optometrists; 2020.
14. Hayhurst C. A turning point for telehealth: COVID-19 spurs rapid uptake of connected care. Biomed Instrum Technol. 2020;54(4):242–250. doi:10.2345/0899-8205-54.4.242
15. Blais N, Tousignant B, Hanssens J-M. Tele-refraction in tele-eye care settings. Clin Exp Optometry. 2022;2022:1–9.
16. American Optometric Association. Evidence-Based Clinical Practice Guideline. In: Comprehensive Adult Eye and Vision Examination. St. Louis, MO; 2015.
17. Blais N, Le Borgne M, Hanssens JM. Tele-refraction: comparison of a remotely performed refraction with a Gold Standard in-person refraction. Boston: American Academy of Optometry; 2021.
18. Curtis R, Hazari H, Eden K, Hopman WM, Irrcher I, Bona MD. Validation of a portable, remotely delivered refraction approach compared to standard in-clinic refraction in a low-vision population. J Telemed Tel. 2020;1(1):1357633X20960628.
19. Randhawa H, Morettin C, McLeod H, et al. The validity of spectacle prescriptions via tele-optometric comprehensive eye examinations; a pilot study. Invest Ophthalmol Vis Sci. 2020;61(7):1604.
20. Lutz de Araujo A, Moreira T, Varvaki Rados DR, et al. The use of telemedicine to support Brazilian primary care physicians in managing eye conditions: the TeleOftalmo Project. PLoS One. 2020;15(4):e0231034. doi:10.1371/journal.pone.0231034
21. Randhawa HK, McLeod HM, Kattouf VM, Pang Y, Sanghera N, Performance V. Binocular vision and accommodative testing in the teleoptometric comprehensive eye examination in a student population. Optometry Visual Perform. 2023;11:1.
22. Chandrasekaran S, Kass W, Thangamathesvaran L, et al. Tele-glaucoma vs clinical evaluation: the new jersey health foundation prospective clinical study. J Telemed Telecare. 2019;2019:1.
23. Maa AY, Evans C, DeLaune WR, Patel PS, Lynch MG. A novel tele-eye protocol for ocular disease detection and access to eye care services. Telemed J e-Health. 2014;20(4):318–323. doi:10.1089/tmj.2013.0185
24. Maa AY, Wojciechowski B, Hunt KJ, et al. Early experience with technology-based eye care services (TECS): a novel ophthalmologic telemedicine initiative. Ophthalmology. 2017;124(4):539–546. doi:10.1016/j.ophtha.2016.11.037
25. Fédération des autorités réglementaires optométriques du Canada [Federation of Optometric Regulatory Authorities of Canada]. FORAC-FAROC Policy on Teleoptometry. [En ligne]; 2020. Available from: https://www.forac-faroc.ca/wp-content/uploads/2020/03/FORAC-FAROC-POLICY-ON-TELEOPTOMETRY-JULY-2019-A.pdf.
26. Canadian Association of Optometrists. Position statement: the use of teleoptometry in post-COVID practice; 2021. Available from: https://opto.ca/document/use-teleoptometry-post-covid-practice.
27. Association québécoise des parents d’enfants handicapés visuels. Définitions et normes légales [Definitions and Legal Standards]. ; 2023. Available from: https://www.aqpehv.qc.ca/deficience-visuelle.
28. Ordre des optométristes du Québec. Lignes directrices - Guide d’exercice clinique [Guidelines - Clinical Practice Guide]; 2023. Available from: https://www.ooq.org/sites/default/files/2023-04/Guide%20exercice%20clinique_20230220.pdf.
29. Carlson NB, Daniel K. Clinical Procedures for Ocular Examination. New York: McGraw-Hill; 2016.
30. Alderson AJ, Green A, Whitaker D, Scally AJ, Elliott D. A comparison of spectacles purchased online and in UK optometry practice. Optometry Vision Sci. 2016;93(10):1196. doi:10.1097/OPX.0000000000000955
31. Pesudovs K, Garamendi E, Elliott D. The quality of life impact of refractive correction (QIRC) questionnaire. Invest Ophthalmol Visual Sci. 2003;44(13):163.
32. Tousignant B, Garceau M-C, Bouffard-Saint-Pierre N, Bellemare -M-M, Hanssens J-M. Comparing the Netra smartphone refractor to subjective refraction. Clin Exp Optometry. 2020;103(4):501–506. doi:10.1111/cxo.13003
33. IBM Corp. IBM SPSS Statistics for Macintosh, Version 28.0. Armonk, NY: IBM Corp; 2021.
34. McAlinden C, Khadka J, Pesudovs K. Statistical methods for conducting agreement (comparison of clinical tests) and precision (repeatability or reproducibility) studies in optometry and ophthalmology. Ophthalmic Physiol Opt. 2011;31(4):330–338. doi:10.1111/j.1475-1313.2011.00851.x
35. Zhang HG, Ying GS. Statistical approaches in published ophthalmic clinical science papers: a comparison to statistical practice two decades ago. Br J Ophthalmol. 2018;102(9):1188–1191. doi:10.1136/bjophthalmol-2017-311529
36. Miller JM. Clinical applications of power vectors. Optom Vis Sci. 2009;86(6):599–602. doi:10.1097/OPX.0b013e3181a6a211
37. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. doi:10.1016/j.jcm.2016.02.012
38. Hughes J. krippendorffsalpha: an R package for measuring agreement using Krippendorff’s alpha coefficient. R J. 2021;13:413–425. doi:10.32614/RJ-2021-046
39. Landis JR, Koch G. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi:10.2307/2529310
40. Leinonen J, Laakkonen E, Laatikainen L. Repeatability (test‐retest variability) of refractive error measurement in clinical settings. Acta Ophthalmol Scandin. 2006;84(4):532–536. doi:10.1111/j.1600-0420.2006.00695.x
41. MacKenzie GE. Reproducibility of sphero-cylindrical prescriptions. Ophthalmic Physiol Opt. 2008;28(2):143–150. doi:10.1111/j.1475-1313.2008.00549.x
42. Mathebula SD, Rubin A. Interexaminer reproducibility for subjective refractions for an ametropic participant. BMJ Open Ophthalmol. 2022;7(1):e000954. doi:10.1136/bmjophth-2021-000954
43. Wisse RPL, Muijzer MB, Cassano F, Godefrooij DA, Prevoo Y, Soeters N. Validation of an independent web-based tool for measuring visual acuity and refractive error (the manifest versus online refractive evaluation trial): prospective open-label noninferiority clinical trial. J Med Internet Res. 2019;21(11):e14808. doi:10.2196/14808
44. Marmamula S, Khanna RC, Mettla AL, et al. Agreement and diagnostic accuracy of vision screening in children by teachers, community eye‐health workers and vision technicians. Clin Exp Optometry. 2018;101(4):553–559. doi:10.1111/cxo.12559
45. Paudel P, Cronjé S, O’Connor PM, Rao GN, Holden BA. Clinical competency of 1-year trained vision technicians in andhra pradesh, India. Ophthalmic Epidemiol. 2015;22(6):409–416. doi:10.3109/09286586.2015.1082605
46. Cohen LM, Rosenberg MA, Tanna AP, Volpe N. A novel computerized portable pupillometer detects and quantifies relative afferent pupillary defects. Curr Eye Res. 2015;40(11):1120–1127. doi:10.3109/02713683.2014.980007
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
