Back to Journals » Vascular Health and Risk Management » Volume 20
Cerebral Venous Sinus Thrombosis as an Initial Presentation of Nephrotic Syndrome: A Case Report
Authors Balla Y , Hashi AS , Osman AA , Hassan MS , Mutlu E
Received 15 February 2024
Accepted for publication 9 April 2024
Published 11 April 2024 Volume 2024:20 Pages 177—181
DOI https://doi.org/10.2147/VHRM.S458539
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Akash Batta
Yassir Balla,1 Abdullahi Said Hashi,2 Ahmed Adam Osman,3,4 Mohamed Sheikh Hassan,5 Eren Mutlu3
1Department of Internal Medicine, Somali-Sudanese Specialized hospital, Mogadishu, Somalia; 2Department of Anesthesiology and Reanimation, Mogadishu Somalia Turkish Training and Research Hospital, Mogadishu, Somalia; 3Department of Radiology, Mogadishu Somalia Turkish Training and Research Hospital, Mogadishu, Somalia; 4Faculty of Medicine and Surgery, University of Somalia, Mogadishu, Somalia; 5Department of Neurology, Mogadishu Somalia Turkish Training and Research Hospital, Mogadishu, Somalia
Correspondence: Ahmed Adam Osman, Department of Radiology, Mogadishu Somalia Turkish Training and Research Hospital, Mogadishu, Somalia, Email [email protected]
Abstract: Cerebral sinovenous thrombosis (CSVT) encompasses a spectrum of disorders involving thrombosis of the cerebral venous system. As shown by previous epidemiological studies, the prevalence of cerebral sinovenous thrombosis is 4– 7 cases per million people. Nephrotic syndrome was very rarely associated with thrombosis cerebral veins or sinuses. Hypercoagulability and thrombotic complications in nephrotic syndrome are most commonly seen in deep veins of the lower extremities and renal veins. Our case highlights a unique scenario in which cerebral sinovenous thrombosis was the initial presentation of nephrotic syndrome in a patient that was not an important past medical or surgical problem. The patient was brought to the emergency department with severe headache, vomiting, altered mental status, and generalized body swelling. Laboratory results showed proteinuria, hypoalbuminemia and hyperlipidemia. Non-contrast brain CT demonstrated hemorrhagic venous infarct associated with vasogenic edema. A subsequent brain MR venogram demonstrated occlusion of superior sagittal and right transverse sinuses. She was managed with low molecular weight heparin and intervenous corticosteroids then shifted to rivaroxaban and oral steroids, respectively, which resulted in massive clinical improvement and resolution of thrombus.
Keywords: nephrotic syndrome, cerebral venous sinus thrombosis, MR venography
Introductıon
Cerebral sinovenous thrombosis is a relatively uncommon medical condition that can lead to serious complications of nephrotic syndrome, with only a few isolated cases published in the literature. The most frequent sites reported for thrombus in patients are the superior sagittal, straight, and transverse sinuses, respectively.1 Glomerular damage as well as substantial loss of urine protein are hallmarks of nephrotic syndrome, a condition that results in severe acquired hypercoagulopathy and an increased risk of potentially fatal venous thromboembolic disorder. It is believed that thromboembolism is the most serious and potentially fatal complication of nephrotic syndrome after infection.2
Cerebral venous thrombosis presents as severe headache, altered mental status, convulsions and hemiplegia. Although brain CT or MRI may show intracerebral infarct or venous hemorrhage associated with vasogenic edema, MR or CT venogram is necessary of definitive diagnosis. CVST has relatively better outcome compared to other forms of stroke.3 Our case illustrates a unique scenario in which cerebral sinovenous thrombosis was the initial presentation of nephrotic syndrome in a patient who had no significant previous medical or surgical problem.
Case Presentation
A 28-year-old female patient was admitted to the emergency department of the hospital after 7 days of fever, severe headache, vomiting, altered mental status, and generalized body swelling. She was on oral contraceptive pills. At the emergency room, a preliminary physical examination revealed that the patient’s heart rate was 86 beats per minute, blood pressure of 137/65 mm Hg, a respiratory rate of 20 breaths per minute, a temperature of 37.2°C, and oxygen saturation of 99%. Neurologic examination revealed an uncooperative, decreased level of consciousness with a Glasgow Coma Scale of 12/15. She had left side weakness with muscle power of 2/5. There were no meningeal irritation signs. Cranial nerve examination including pupillary reflex and eye movements were normal. Fundus examination demonstrated bilateral papilledema. The rest of the physical examination was unremarkable.
Laboratory results showed proteinuria 5g/24h (Normal < 150mg/24), PCR (Protein creatinine ratio) 60 g/day (Normal at <30 mg/dl), hypoalbuminemia 1.5 g/dl (Normal 3.4 to 5.4 g/dL), total cholesterol 275mg/dl (Normal less than 200 mg/dL), Triglyceride 230 mg/dl (Normal less than 130 mg/dl).
A non-contrast brain CT showed right front-parietal venous hemorrhagic infarct associated with vasogenic edema (see Figure 1). MR venography was done which demonstrated a large filling defect area in the anterior aspect of the superior sagittal sinus and the right transverse indicating thrombosis (see Figure 2).
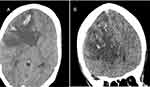 |
Figure 1 (A and B) Non-contrast cranial CT showed multiple hyperdense venous hemorrhages in the right frontal lobe with surrounding extensive hypodense vasogenic edema. |
The patient was diagnosed with nephrotic syndrome with concomitant cerebral venous sinus thrombosis. The patient was admitted to High Dependency Unit (HDU). Low molecular weight heparin and intravenous corticosteroids were started. The oral contraceptive pills were stopped. On day 7, she was switched to rivaroxaban, and prednisone 1 mg/kg/day was used to treat her nephrotic syndrome. On discharging day, she was fully conscious with a significant reduction in her body weight.
The patient was successfully treated with high-dose prednisone after two weeks of discharge, and a successful tapering attempt was made. She used rivaroxaban for six months before stopping it when her nephrotic condition improved. On outpatient follow-up, the albumin level returned to the normal range. She did not experience worsening of neurological symptoms. Likewise, she had no recurrence of the neurological symptoms.
Discussion
Thrombosis of the cerebral veins or sinuses is a rare type of stroke that typically strikes young people.4 Cerebral sinovenous thrombosis accounts for approximately 0.5% to 1% of all forms of strokes. The risk of CVST is three times higher in women of reproductive age than in males of the same age group, most likely as a result of pregnancy, postpartum illness, and oral contraceptive use.5 Magnetic resonance imaging with magnetic resonance venography is the standard diagnosis of choice for cerebral sinovenous thrombosis. CVST still remains unreported complication of nephrotic syndrome.1,6
Nephrotic syndrome is defined by proteinuria of ≥3.5 g/24 hours, albuminemia <3.0 g, peripheral edema, hyperlipidemia, lipiduria, and elevated risk of thrombotic disorders.7 There are multiple possible reasons for the hypercoagulable state observed in nephrotic syndrome, including enhanced procoagulatory activity, thrombocytosis, and urinary loss of anticoagulant proteins, particularly antithrombin III.8
Delays in diagnosis can result from the diverse, vague, and non-specific clinical presentation of cerebral venous thrombosis. But the majority of patients have headaches, nausea, vertigo, low consciousness, seizures, and papilledema, which causes CVST to be misdiagnosed.9 Our case report presents a unique scenario in which cerebral sinovenous thrombosis is an initial presentation of nephrotic syndrome, a rare condition that causes delays in diagnosis and treatment. Such cases are often missed due to the rarity and lack of awareness about the association between these two conditions, making it important for clinicians to consider such an association when evaluating patients with severe headaches, seizures, focal neurological deficits, and altered mental status.10
There is no current guideline over the prophylactic use of anticoagulation and in daily practice, it is not routinely used unless the patient has a thrombosis history.11,12 Our case emphasizes the diagnostic challenge of developing a patient-specific treatment plan to address both conditions and highlights the importance of monitoring prothrombotic risk factors. To reduce the risk of further embolic events and to avoid a recurrence, the patient was managed with anticoagulation therapy. In comparison to the general population, individuals with nephrotic syndrome and those taking OCPs had a higher prevalence of cerebral sinovenous thrombosis, which can appear in the early stages of the disease.
Conclusion
Our case highlights the significance of clinical suspicion in patients presenting with severe headaches, dizziness, and focal neurological symptoms. With diligent physical examination, appropriate imaging, and early anticoagulation of the CVST could reduce morbidity and prevent life-threatening complications.
Ethics Approval and Consent
No institutional approval was required to publish the case details. The patient provided informed written consent to participate in the study.
Consent for Publication
The patient provided informed written consent for this case to be published in a peer-reviewed journal.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Alvis-Miranda HR, Milena Castellar-Leones S, Alcala-Cerra G, Rafael Moscote-Salazar L. Cerebral sinus venous thrombosis. J Neurosci Rural Pract. 2013;4(4):427–438. doi:10.4103/0976-3147.120236
2. Waller AP, Agrawal S, Wolfgang KJ, et al.; the Pediatric Nephrology Research Consortium (PNRC). Nephrotic syndrome‐associated hypercoagulopathy is alleviated by both pioglitazone and glucocorticoid which target two different nuclear receptors. Physiol Re. 2020;8(15):e14515.
3. Goyal G, Charan A, Singh R. Clinical presentation, neuroimaging findings, and predictors of brain parenchymal lesions in cerebral vein and dural sinus thrombosis: a retrospective study. Ann Indian Acad Neurol. 2018;21(3):203. doi:10.4103/aian.AIAN_470_17
4. Grunt S, Wingeier K, Wehrli E, et al. Cerebral sinus venous thrombosis in Swiss children. Dev Med Child Neurol. 2010;52(12):1145–1150. doi:10.1111/j.1469-8749.2010.03722.x
5. Devasagayam S, Wyatt B, Leyden J, Kleinig T. Cerebral venous sinus thrombosis incidence is higher than previously thought: a retrospective population-based study. Stroke. 2016;47(9):2180–2182. doi:10.1161/STROKEAHA.116.013617
6. Urch C, Pusey CD. Sagittal sinus thrombosis in adult minimal change nephrotic syndrome. Clin Nephrol. 1996;45(2):131–132.
7. Al-Azzawi HF, Obi OC, Safi J, Song M. Nephrotic syndrome-induced thromboembolism in adults. Int J Crit Illness Injury Sci. 2016;6(2):85–88. doi:10.4103/2229-5151.183019
8. Kerlin BA, Ayoob R, Smoyer WE. Epidemiology and pathophysiology of nephrotic syndrome-associated thromboembolic disease. Clin J Am Soc Nephrol. 2012;7(3):513–520. doi:10.2215/CJN.10131011
9. Kodner C. Nephrotic syndrome in adults: diagnosis and management. Am Family Phys. 2009;80(10):1129.
10. Moeindarbari S, Beheshtian N, Hashemi S. Cerebral vein thrombosis in a woman using oral contraceptive pills for a short period of time: a case report. J Med Case Rep. 2022;16(1):260. doi:10.1186/s13256-022-03473-w
11. Mirrakhimov AE, Ali AM, Barbaryan A, Prueksaritanond S, Hussain N. Primary nephrotic syndrome in adults as a risk factor for pulmonary embolism: an up-to-date review of the literature. Int J Nephrol. 2014;2014:1–9. doi:10.1155/2014/916760
12. de Freitas GR, Bogousslavsky J. Risk factors of cerebral vein and sinus thrombosis. In: Handbook on Cerebral Venous Thrombosis. Vol. 23. Karger Publishers; 2008:23–54.
13. Khomand P, Hassanzadeh K. A case-series study of cerebral venous thrombosis in women using short course oral contraceptive. Iran J Neurol. 2016;15(2):92.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

