Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 15
Vitamin D Levels Among Rheumatoid Arthritis Sudanese Patients: Prevalence and Correlation to Disease Activity – A Bicentric Study
Authors Mustafa Mohamed ME , Imad Taha Z, Hamza SB , Abdalla YA , Noor SK, William J
Received 10 July 2023
Accepted for publication 16 September 2023
Published 20 September 2023 Volume 2023:15 Pages 181—187
DOI https://doi.org/10.2147/OARRR.S425397
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Chuan-Ju Liu
Mohamed Elfaith Mustafa Mohamed,1,2 Ziryab Imad Taha,1,3– 5 Salih Boushra Hamza,2,5 Yassin A Abdalla,2,5 Sufian K Noor,6 Jimmy William5,7
1Rheumatology Speciality Department, Sudan Medical Specialization Board, Khartoum, Sudan; 2Department of Internal Medicine, Faculty of Medicine and Health Sciences, Omdurman Islamic University, Khartoum, Sudan; 3Department of Clinical Medicine, Medical and Cancer Research Institute (MCRI), Nyala, Sudan; 4Department of Internal Medicine, University of Bahri, Faculty of Medicine, Khartoum, Sudan; 5Rheumatology Department, Ziryab Research Group, Khartoum, Sudan; 6Department of Internal Medicine, Nile Valley University, Faculty of Medicine, Atbara, Sudan; 7General Internal Medicine Department, Sligo University Hospital, Sligo, Ireland
Correspondence: Jimmy William, Sligo University Hospital, The Mall, Rathquarter, Sligo, F91 H684, Ireland, Tel +353 851173213, Email [email protected]
Purpose: To evaluate vitamin D levels among adult Sudanese RA patients and identify its correlation with RA disease activity.
Patients and Methods: A bicentric cross-sectional analytical hospital-based study was performed in two Khartoum State Hospitals between October 2019 and January 2020, enrolling 90 Sudanese patients with RA. Serum vitamin D levels were measured with a standard reference level of 30ng/mL– 100ng/mL. A detailed interview-based questionnaire was used to collect the patient’s information, clinical data and lab results—disease activity was assessed via the DAS-28 score. The data was then analyzed using SPSS v-24.
Results: Vitamin D levels were low in 79 candidates (87.8%), 53 of which (67.1%) showed moderate insufficiency (10– 30ng/mL), and 26 candidates (32.9%) had severe deficiency (less than 10 ng/mL). Regarding the disease activity, 57 participants (63.3%) had moderate disease activity (DAS-28=3.2– 5.1), and 22 participants (24.4%) had high disease activity (DAS-28 > 5.1). A significant negative correlation was reported between high DAS-28 scores and low vitamin D levels with p-value = < 0.001 (95% CI: − 0.8591 to 0.0015) and r = − 0.44.
Conclusion: Most adult Sudanese rheumatoid arthritis patients showed low vitamin D levels (87.8%), which was also significantly correlated with increased disease activity (P-value < 0.05). Moreover, the prevalence of low vitamin D levels was significantly higher than in numerous countries worldwide.
Keywords: vitamin D, rheumatoid arthritis, DAS-28 score, Sudan
Introduction
Rheumatoid arthritis (RA) is a long-lasting autoimmune inflammatory disorder that affects the joints and can have widespread systemic effects. While RA’s exact causes remain unclear, genetic and non-genetic factors, such as environmental, infectious, and hormonal elements, are believed to contribute to its prevalence.1 Vitamin D has been implicated in RA, and there is a higher incidence of osteoporosis among RA patients (~2-fold higher than the general population), leading clinicians to prescribe vitamin D and calcium often.2,3 Recent evidence suggests that vitamin D may be inversely correlated with RA occurrence, progression, disease activity, and flare-ups, indicating its potential anti-inflammatory and immune-regulating roles. Vitamin D serves as a precursor to a steroid hormone and undergoes chemical conversions in the liver and kidney, resulting in the production of 25OHD, which serves as an objective indicator of vitamin D status, and 1,25-dihydroxy vitamin D (1,25(OH)2D), the primary bioactive form.4
Vitamin D exerts its anti-inflammatory effects by influencing innate and adaptive immune systems. Immune cells such as dendritic cells and monocytes/macrophages, which belong to the innate immune system, express an enzyme called 1-alpha-hydroxylase that converts vitamin D into its active form, 1,25(OH)2D, which they utilize for autocrine and paracrine responses. In the adaptive immune system, vitamin D suppresses the expression of proteins involved in autoimmunity driven by T helper type 1 (Th1) cells and also inhibits antigen presentation, antibody production, lymphocyte proliferation, dendritic cell differentiation, and the release of cytokines like interleukin-2 (IL-2), IL-6, interferon-gamma (IFN-gamma), and tumour necrosis factor-alpha (TNF-alpha). Additionally, vitamin D promotes the development of monocytes into macrophages and influences their chemotaxis (movement towards chemical signals) and cytokine expression.4,5
Many autoimmune diseases, including inflammatory bowel disease, type 1 diabetes, multiple sclerosis, and rheumatoid arthritis, are characterized by Th1 cytokine-mediated immune responses. By suppressing Th1 responses, vitamin D helps shift the T cell response towards an immunosuppressive state.5 Thus, in this study, we aim to assess the prevalence of low vitamin D levels among Sudanese RA patients and its correlation to disease activity.
Materials and Methods
Participants
This is a descriptive, cross-sectional, bicentric, analytical hospital-based study that included RA patients who fulfilled the 2010 ACR/EULAR criteria to assess the correlation between RA activity and Vitamin D levels.6 It included patients from Two Teaching Hospitals (Haj El-Safi Teaching Hospital and Khartoum North Teaching Hospital) in Khartoum North State – Outpatient Rheumatology Clinics between October 2019 and January 2020, with a wide catchment area of approximately a million residents.
Inclusion Criteria
- Known adult Sudanese RA patients (over 18 years old).
- Patients on regular follow-up (at least one year of follow-up post diagnosis of RA or ≥80% of the appointments ~ ≥4 Visits since diagnosis).
- Patients with complete hospital record charts (Including Date of Diagnosis, Lab results document, follow-up outcomes clearly documented).
Exclusion Criteria
- Patients with overlapping connective tissue diseases.
- Patients with malnutrition, hepatic, renal or thyroid diseases.
- Patients on vitamin D supplements in the past six months.
- Patients on medications affecting Vitamin D absorption or excretion.
- Pregnant women.
To date, there is no official documentation regarding the prevalence of Rheumatoid Arthritis (RA) in Sudan. However, an estimate derived from a study published in Nature Scientific Reports indicates that Sudan has a relatively low age-standardized prevalence of RA compared to other Middle Eastern and North African regions, with an estimated rate of 83.0 cases per 100,000 population (95% uncertainty interval: 71.6–97.1).7 Based on this estimation, it is suggested that a sample size of at least 50 participants or more could be appropriate for a research study using Cochran’s equation as a guideline.8
Ethical Consideration
Ethical approval was attained from the Sudan Medical Specialisation Board (SMSB). The study complied with the tenets of the Declaration of Helsinki. Approval from the hospital authority was given. Patients were counselled about the purpose of the study. Written and verbal consent was obtained from patients. Data was used anonymously using identity numbers instead of names to protect the patient’s identity and kept securely and in a separate file. No reference to any individual participant was made in the study reports. Subject identities were known only by the study staff.
Data Collection
Data was collected via a pre-designed interview-based questionnaire containing the patients’ information, clinical data and lab results. Baseline variables were age (years), gender (male/female), occupation, city of residence, duration of the disease, blood level of vitamin D, ESR, Swollen Joint Count (SJC28), Tender Joint Count (TJC28) and the patient Visual Analogue Score for global disease activity (VAS) and Global assessment of health (marking 10 points between very good and very bad). Disease activity was measured using the following DAS-28 score.9
TJC = tender joint count
SJC = swollen joint count
Ln = log
VAS = visual analogue scale
Das 28 cut-offs were high (≥5.1), moderate (≥3.2 - <5.1), low (≥2.6 - <3.2), and remission (<2.6). Venous blood samples were collected, and the vitamin D levels were measured using COBAS e 411 analyzers [using Electrochemiluminescence technology for immunoassay analysis, similar to conventional Enzyme-linked immunosorbent assay (ELISA) but quicker], with the normal level reference being (30–100ng/mL), insufficiency (10–30ng/mL) and deficiency (less than 10 ng/mL).10–12
Data Analysis
After the data was collected through a standard questionnaire, the analysis was started by forming an Excel table; the Statistical Package for Social Sciences (SPSS) version 24 was used for the analysis, Chi-Squared test, frequency table along with Pie and Bar charts were used to exhibit the results, with the level of significance set at (P ≤ 0.05).
Results
Demographic Characteristics
This cross-sectional bicentric, hospital-based study involved 90 RA patients, of which 44 participants (48.9%) were in the age group (41–60) years old, while 33 (36.9%) were in the age group (21–40) years, illustrating younger age predominance. Seventy-nine participants (87.9%) were females, and only 11 (12.1%) were males. Seventy-four (82.2%) patients were employed, and the majority, 69 (76.9%), were from Khartoum state (Table 1).
 |
Table 1 Demographic Characteristics of the Participants |
Characters of the Patients
Thirty-six (40%) of the study participants had RA for (1–5) years. Sixty-one (67.7%) of the enrolled individuals received treatment, and only 29 (32.3%) were not on any treatment. Among those who are receiving treatment, 81 (90.1%) were on Hydroxychloroquine (HCQ), followed by 31 (34.4%) on Methotrexate; nonetheless, 67 (74.4%) of the participants had been using medication for (1–5 years). All study participants were getting the ordinary Sudanese diet, and all enrolled patients had a BMI >18.5 (malnutrition cut-off point).8 The sun exposure time was variable, as 56 (62.2%) participants were exposed for more than one hour per day (Table 2).
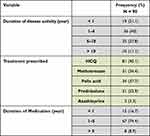 |
Table 2 Study Population Disease Activity, Treatment Lines and Duration |
Vitamin D Level Among the Participants
The majority of the study participants, 53 (58.9%), had moderate vitamin D insufficiency, 26 candidates (28.9%) had a severe deficiency, and only 11 (12.2%) participants had a normal level.
DAS 28 Score Among the Participants
Regarding the DAS 28 score, 57 (63.3%) of the study participants had a moderate score, and 22 (24.4%) had high activity. Among the participants who were found to have moderate activity, 8 (72.7%) were males, and 49 (62%) were females.
There was a significant correlation between the DAS-28 score and Vitamin D level (p-value= <0.001 [95% CI: −0.8591 to 0.0015] and r = −0.44 (moderately strong negative correlation) (Table 3) (Figure 1). There was a significant association between DAS-28 score and Gender (p-value= 0.002). No association was found between the disease duration and DAS-28 score (p-value = 0.37) or vitamin D level (p-value = 0.87). Moreover, no significant association was observed between the duration of medication usage and the DAS-28 score (p-value=0.40) or vitamin D level (p-value = 0.27).
 |
Table 3 DAS-28 Score and Vitamin D Level |
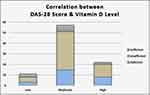 |
Figure 1 Correlation between RA activity – *DAS 28 score and vitamin D level. *P-value: <0.001 (95% CI: −0.8591 to 0.0015) and r= −0.44. |
Discussion
The current study aimed to measure the serum level of vitamin D among adult Sudanese RA patients and to correlate that to the disease activity using the DAS28 score, besides comparing results to other countries.
Ninety patients with RA diagnosed based on 2010 (ACR/EULAR) classification criteria for RA participated in the study, with female predominance of 87.9%. Blood levels of vitamin D were insufficient in 58.9% of RA patients, thus corresponding with studies from Turkey and Egypt conducted by Yagiz et al Kareem et al and Ibrahim et al respectively, that recorded significantly low Vitamin D levels in patients with RA, SLE, ankylosing spondylitis, and Behcet’s disease as compared to control population (general population).11–13 Moreover, another study from Greece by Kostoglou et al concluded that in RA, 25(OH)D3 levels were found to be low compared with the control group, 25(OH)D3 being 15.26 ± 1.07 ng/mL [mean ± standard error of the mean (SEM)] in the RA group as opposed to 25.8 ± 1.6 ng/mL in the control group (p < 0.001).14 Therefore, it broadly supports the possible role of Vitamin D in the pathogenesis, activity and treatment of various autoimmune diseases. On the contrary, another Turkish study by Turhanoğlu et al established that the mean of the 25-OH D vitamin levels of the patients with RA was not different from that of the general population control group (P = 0.936).15 A similar outcome was achieved by Satyajeet et al among Indian patients with RA.16 Nevertheless, Turhanoğlu et al concluded that Vitamin D levels significantly decreased per the disease activity and decreased functional capacity, besides a significant negative correlation between Serum 25-OH vitamin D levels and DAS-28.15 Furthermore, in the former, Satyajeet et al, the study population was 28, with only 6 RA patients enrolled, thus exhibiting minimal validity.16
Another significant relationship was observed in our study between gender and DAS 28 score, as 72.7% of the males had moderate disease activity compared with 62% of the females, contrasting a study by Radovits et al, which stated that a high DAS-28 was found to perform equally in all age groups, in men and women, despite the elevating effect of age on ESR.17 Also, an elevated ESR could underestimate the remission rate in older males with low disease activity.
Furthermore, 67.7% of the RA patients enrolled received treatment, 90.1% were taking HCQ, and only 34.4% were on Methotrexate; however, no significant association was found between the therapy prescribed and vitamin D level, similar to a study from Iran by Salesi et al.18
Conspicuously, our study showed a statistically significant and moderately strong negative correlation (p-value: <0.001 [95% CI: −0.8591 to 0.0015] and r = −0.44) between Vitamin D levels and DAS-28 score, as 57.6% of the patients with vitamin D less than 30ng/mL had moderate disease activity, 30.7% had high disease activity, and only 11.5% had low disease activity. These results were similar to studies by Yassin et al and Azzeh et al, conducted among Egyptian and Saudi patients with RA and concluded that Vitamin D insufficiency is highly prevalent and linked to disease severity in patients with RA.19,20 Another interesting study from Saudi Arabia conducted by Attar et al assessed Vitamin D deficiency in RA and the prevalence and association with disease activity among 200 participants, 100 RA patients and 100 controls (both not on Vitamin D supplements) established that patients with high disease activity had the lowest Vitamin D levels (18.25 ± 8.3 nmol/L) compared to patients with moderate (35.13 ± 15.2 nmol/L), and low (38.05 ± 7.3 nmol/L) disease activity.21 A negative correlation was noticed between Vitamin D levels and the DAS-28 score, which was statistically significant; thus, marked lower Vitamin D levels were found in patients who were poorly responding to treatment and were not achieving remission.21
Furthermore, Merlino et al, demonstrated an inverse association between greater intake of Vitamin D and RA risk. They analyzed data from a prospective cohort study of 29,368 women without a history of RA at the study baseline, and through 11 years of follow-up, 152 cases of RA were diagnosed.22 Another recent Indian study stated that 90% of RA patients were either Vitamin D deficient or insufficient, and RA patients’ mean serum Vitamin D level was significantly lower than healthy controls.23 In line with the same concept, the COMORA study, which included 1413 RA patients in 15 countries from all seven continents, concluded that serum Vitamin D levels were inversely correlated with disease activity when evaluated by DAS-28 post-adjusting for possible confounders.24
Lastly, upon comparing the prevalence of lower Vitamin D levels in our current study to the COMORA study, since it included the most extensive study population from various countries, including 2 African countries, Egypt and Morocco, besides Argentina, Austria, France, Germany, Hungary, Italy, Korea, Netherlands, Spain, Taiwan, UK, Uruguay, USA, the overall mean frequency of Vitamin D insufficiency and deficiency in Sudan were significantly higher (58.8% and 28.8% vs 26.1% and 5%, respectively).24
Limitations
A larger, longitudinal study could clarify the link between vitamin D and RA, providing a more comprehensive representation of Sudan. Dietary factors were not investigated in this research.
Conclusion
To the best of our knowledge, this is the first study looking at Vitamin D levels and Rheumatoid arthritis from Sudan. Most adult Sudanese Rheumatoid arthritis patients showed low vitamin D levels (87.8%), which was also significantly correlated with increased disease activity (P-value <0.05). Moreover, the prevalence of low vitamin D levels was significantly higher than in numerous countries worldwide.
Acknowledgments
Hospital Medical Staff and Admission offices in all Sudanese hospitals.
Disclosure
All authors report no conflicts of interest in this work.
References
1. Alamanos Y, Drosos AA. Epidemiology of adult rheumatoid arthritis. Autoimmun Rev. 2005;4(3):130–136. doi:10.1016/j.autrev.2004.09.002
2. Lundström E, Källberg H, Alfredsson L, et al. Gene-environment interaction between the DRB1 shared epitope and smoking in the risk of anti-citrullinated protein antibody-positive rheumatoid arthritis: all alleles are important. Arthritis Rheum. 2009;60(6):1597–1603. doi:10.1002/art.24572
3. Hauser B, Riches PL, Wilson JF, Horne AE, Ralston SH. Prevalence and clinical prediction of osteoporosis in a contemporary cohort of patients with rheumatoid arthritis. Rheumatology. 2014;53(10):1759–1766. doi:10.1093/rheumatology/keu162
4. Dayer JM. The pivotal role of interleukin-1 in the clinical manifestations of rheumatoid arthritis. Rheumatology. 2003;42(SUPPL. 2):3–10. doi:10.1093/rheumatology/keg326
5. Furst DE, Emery P. Rheumatoid arthritis pathophysiology: update on emerging cytokine and cytokine-associated. Rheumatology. 2014;53(9):1560–1569. doi:10.1093/rheumatology/ket414
6. Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69:1580–1588. doi:10.1136/ard.2010.138461
7. Mousavi SE, Nejadghaderi SA, Khabbazi A, et al. The burden of rheumatoid arthritis in the Middle East and North Africa region, 1990–2019. Sci Rep. 2022;12(1):19297. doi:10.1038/s41598-022-22310-0
8. Cochran WG. Sampling Techniques.
9. Prevoo M, Hof Ma VT, Kuper H, Van Leeuwen MA, Van Riel P, Van Riel PLCM. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38:44–48. doi:10.1002/art.1780380107
10. Woldeyohannes M, Girma M, Petros A, et al. Ethiopia national food and nutrition survey to inform the Ethiopian national food and nutrition strategy: a study protocol. BMJ Open. 2023;13(4):e067641. doi:10.1136/bmjopen-2022-067641
11. Yagiz AE, Ustun N, Paksoy H, et al. Association of Vitamin D with disease activity in rheumatoid arthritis and ankylosing spondylitis. J Clin Anal Med. 2015;6:486–489.
12. Kareem MI, Mohammed RH, Abozaid HS, Rayan MM, Mohamed AM, Fathi NA. Hypo-vitaminosis D in patients with rheumatoid arthritis, systemic lupus erythematosus and ankylosing spondylitis. J Clin Cell Immunol. 2015;6:1–6.
13. Ibrahim MH, Bakheet MS, Sater KA, Shakoor MA. Relationship between Vitamin D and disease activity in some rheumatic diseases. Wyno Acad J Med Sci. 2013;2:52–56.
14. Kostoglou-Athanassiou P, Raftakis I, Antoniadis C, et al. Vitamin D and rheumatoid arthritis. Ther Adv Endocrinol Metab. 2012;3(6):181–187. doi:10.1177/2042018812471070
15. Turhanoğlu AD, Güler H, Yönden Z, et al. The relationship between vitamin D and disease activity and functional health status in rheumatoid arthritis. Rheumatol Int. 2011;31(7):911–914. doi:10.1007/s00296-010-1393-6
16. Jagtap S, Turankar AV, Bankar MA, et al. Status of serum vitamin D levels in patients of rheumatoid arthritis: a pilot study. J Rational Pharmacother Res. 2014;2014(3):90–95.
17. Radovits BJ, Fransen J, van Riel PLCM, et al. Influence of age and gender on the 28-joint Disease Activity Score (DAS28) in rheumatoid arthritis. Ann Rheum Dis. 2008;67:1127–1131. doi:10.1136/ard.2007.079913
18. Huisman AM, White KP, Algra A, et al. Vitamin D levels in women with systemic lupus erythematosus and fibromyalgia. J Rheumatol. 2001;28(11):2535–2539.
19. Yassin A, Gareeb H, Mohamed NA, Samy C. The relationship between Vitamin D and disease activity in Egyptian patients with rheumatoid arthritis. Int Trends Immun. 2014;2:122–127.
20. Azzeh FS, Kensara OA. Vitamin D is a good marker for disease activity of rheumatoid arthritis disease. Dis Markers. 2015;2015:260725. doi:10.1155/2015/260725
21. Attar SM. Vitamin D deficiency in rheumatoid arthritis. Prevalence and association with disease activity in Western Saudi Arabia. Saudi Med J. 2012;33:520–525.
22. Merlino LA, Curtis J, Mikuls TR, et al. Vitamin D intake is inversely associated with rheumatoid arthritis: results from the Iowa women’s health study. Arthritis Rheum. 2004;50:72–77. doi:10.1002/art.11434
23. Sharma R, Saigal R, Goyal L, et al. Estimation of Vitamin D levels in rheumatoid arthritis patients and its correlation with the disease activity. J Assoc Physicians India. 2014;62:678–681.
24. Hajjaj-Hassouni N, Mawani N, Allali F, et al. Evaluation of vitamin D status in rheumatoid arthritis and its association with disease activity across 15 countries: “The COMORA study”. Int J Rheumatol. 2017;2017:5491676. doi:10.1155/2017/5491676
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

