Back to Journals » International Journal of Women's Health » Volume 16
Values of Caprini Risk Assessment Scale and D-Dimer for Predicting Venous Thromboembolism During Puerperium
Received 25 October 2023
Accepted for publication 28 December 2023
Published 12 January 2024 Volume 2024:16 Pages 47—53
DOI https://doi.org/10.2147/IJWH.S443245
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Hongmei Liu,1,* Lamei Li,2,* Zhe Zhao3
1Department of Gynaecology, the First Affiliated Hospital of Shihezi University, Shihezi, 832000, People’s Republic of China; 2Department of Gynaecology and Obstetrics, Shihezi University School of Medicine, Shihezi, 832000, People’s Republic of China; 3Department of Gynaecology and Obstetrics, Bingtuan Sishi Hospital, Yining, 835000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hongmei Liu, Department of Gynaecology, the First Affiliated Hospital of Shihezi University, No. 107, Beier Road, Shihezi, 832000, People’s Republic of China, Tel +86-9932850000, Email [email protected]
Purpose: To evaluate the predictive value of the combination of the Caprini risk assessment model (RAM) and D-dimer for venous thromboembolism (VTE) during puerperium.
Patients and Methods: This was a retrospective case–control study. Thirty-one puerperium patients with VTE were included as cases, and 279 puerperium women without VTE were matched to cases according to age, number of fetuses, birth day and delivery mode at the ratio of 9:1. Demographic data, clinical data and laboratory parameters within postpartum 24 h were collected. Multivariate analysis, employing the forward stepwise model, was conducted to identify independent factors associated with VTE during puerperium. The predictive values of Caprini RAM, D-dimer and their combination were evaluated using receiver operating characteristic (ROC) curve, and the area under curve (AUC) was compared using Z test.
Results: Univariate analysis demonstrated that there were significant differences in D-dimer levels, Caprini score, scarred uterus, adherent placenta, postpartum hemorrhage and intrauterine infection between cases and controls (P< 0.05). Multivariate analysis demonstrated that D-dimer levels (OR: 1.754, 95% CI: 1.237– 3.182), Caprini score (OR: 1.209, 95% CI: 1.058– 2.280), scarred uterus (OR: 1.978, 95% CI: 1.258– 3.794), postpartum hemorrhage (OR: 2.276, 95% CI: 1.334– 4.347) and intrauterine infection (OR: 2.575, 95% CI: 1.463– 4.618) were independently associated with VTE during puerperium with adjustment for adherent placenta and fetal birth weight. The AUCs of D-dimer levels, Caprini score and their combination were 0.748 (SE: 0.030, 95% CI: 0.688– 0.807), 0.647 (SE: 0.035, 95% CI: 0.578– 0.716) and 0.840 (SE: 0.025, 95% CI: 0.791– 0.888). Combination prediction had a higher AUC compared with that of independent prediction (0.840 vs 0.748, Z=2.356, P= 0.009; 0.840 vs 0.647, Z=4.487, P< 0.001) with a sensitivity of 83.9% and specificity of 80.3%.
Conclusion: The combination of the Caprini RAM and D-dimer could significantly elevate the predictive value for VTE during puerperium, and this new tool had the potential in the prediction of VTE during puerperium.
Keywords: venous thromboembolism, puerperium, caprini risk assessment model, D-dimer, prediction
Introduction
Venous thromboembolism (VTE), including deep venous thrombosis (DVT) and pulmonary embolism (PE), is a severe maternal complication around delivery.1 Its incidence during pregnancy and puerperium is 1.0 to 1.8/1000,2 significantly higher than that of nonpregnant women.3–5 Although the absolute risk of VTE associated with pregnancy was low, it has gradually become one of the major causes of maternal death instead of postpartum hemorrhage.6 Accurate prediction of VTE risk during pregnancy and puerperium is therefore crucial for its prevention and treatment.
The Caprini risk assessment model (RAM) has been extensively validated in VTE risk identification of different patients.7–12 However, its application to VTE risk identification during peripartum showed a limited performance.13
D-dimer levels upregulate gradually during pregnancy and peaked at the first day after delivery.14 Most of healthy pregnant women demonstrate higher D-dimer levels compared with the normal reference range.15 A recent study found that abnormally high levels of D-dimer (≥3.70 mg/L) was independently correlated with VTE during puerperium and could serve as an independent predictor.16 Thus, the combination of the Caprini risk assessment model and D-dimer was used to predict VTE during puerperium in order to improve predictive performance in this study, and the aim was to provide a new tool for the prediction of VTE during puerperium.
Patients and Methods
Patients
This was a retrospective case–control study, including all puerperium patients with DVT or PE meeting inclusion and exclusion criteria in The First Affiliated Hospital of Shihezi University and Bingtuan Sishi Hospital between March 2012 and December 2022. The inclusion criteria included ①puerperium patients with DVT or PE, ②complete medical records, and ③having D-dimer testing results. The exclusion criteria included ①a previous history of VTE, ②superficial VTE, and ③other cardiovascular diseases or any malignant tumor. The diagnosis of PE was objectively confirmed with computed tomography pulmonary angiography, and the diagnosis of DVT was confirmed with Doppler ultrasound and/or computed tomographic (CT) venography.
Controls, defined as women without VTE during puerperium, were randomly sampled from women who had delivered in The First Affiliated Hospital of Shihezi University and Bingtuan Sishi Hospital between March 2012 and December 2022. They were matched to cases according to age, number of fetuses, birth day and delivery mode at the ratio of 9:1.
This study received the approval of the Ethics Committee of The First Affiliated Hospital of Shihezi University and was performed according to the guidelines of the Declaration of Helsinki, and all participants provided informed consents.
Data Collection
Demographic data, clinical data and laboratory parameters within postpartum 24 h were collected, including age, height, weight, gestational age at delivery, fetal birth weight, previous obstetric history, parity, in vitro fertilization, scarred uterus, placenta previa, adherent placenta, premature birth, postpartum hemorrhage, pregnancy complications, D-dimer, platelet, and fibrinogen.
Caprini score was evaluated for all participants before delivery and within postpartum 24 h, and the highest score was chosen in this study. Supplementary Table 1 provided the raw scores and D-dimer results of each of the patients who developed VTE. Supplementary Table 2 provided a complete list of all the questions that were asked and the number of positive and negative responses for each specific question in those with and without thrombosis.
Statistical Analysis
The SPSS version 22.0 (SPSS Inc., USA) was employed to conduct statistical analysis, and statistical significance was set at two-sided P< 0.05. Continuous variables were evaluated for normality using Kolmogorov–Smirnov test. Variables with normal distribution were compared for intergroup differences using Student’s t test, and variables without normal distribution were compared for intergroup differences using Mann–Whitney U-test. Categorical variables were compared for intergroup differences using Chi-square test or Fisher exact test. Multivariate analysis, employing the forward stepwise model, was conducted for the variables with two-sided P<0.10 in univariate analysis. The predictive values of Caprini RAM, D-dimer and their combination were evaluated using receiver operating characteristic (ROC) curve, and the area under curve (AUC) was compared using Z test.
Results
Univariate Analysis Between the Case Group with Control Group
In this study, 31 puerperium patients with VTE were included according to the inclusion and exclusion criteria, and 279 puerperium women without VTE were matched to cases according to age, number of fetuses, birth day and delivery mode. Univariate analysis results (Table 1) demonstrated that there were significant differences in D-dimer levels, Caprini score, scarred uterus, adherent placenta, postpartum hemorrhage and intrauterine infection between the case and control group (P< 0.05), and there were no significant differences in the rest variables (P > 0.05).
 |
Table 1 Univariate Analysis Results Between the Case Group with Control Group |
Multivariate Analysis Between the Case Group with Control Group
Multivariate analysis was conducted for D-dimer levels, Caprini score, scarred uterus, adherent placenta, postpartum hemorrhage, intrauterine infection and fetal birth weight. The results demonstrated that D-dimer levels, Caprini score, scarred uterus, postpartum hemorrhage and intrauterine infection were independently associated with VTE during puerperium with adjustment for adherent placenta and fetal birth weight (Table 2).
 |
Table 2 Multivariate Analysis Results Between the Case Group with Control Group |
Predictive Value for VTE During Puerperium
As shown in Figure 1, the AUC of D-dimer levels was 0.748 (SE: 0.030, 95% CI: 0.688–0.807) when applied in predicting VTE during puerperium and Caprini score was 0.647 (SE: 0.035, 95% CI: 0.578–0.716). In order to elevate the predictive value for VTE during puerperium, the combination of D-dimer levels and Caprini score was used in this study. The results showed that the AUC of combination prediction was up to 0.840 (SE: 0.025, 95% CI: 0.791–0.888), which was significantly higher than that of independent prediction (0.840 vs 0.748, Z=2.356, P=0.009; 0.840 vs 0.647, Z=4.487, P<0.001). Clinical utility indexes of D-dimer levels, Caprini score and combination prediction for VTE during puerperium are shown in Table 3.
 |
Table 3 Clinical Utility Indexes of D-Dimer Levels, Caprini Score and Combination Prediction for VTE During Puerperium |
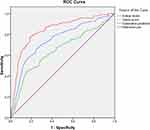 |
Figure 1 ROC curves of D-dimer levels, Caprini score and their combination in predicting VTE during puerperium. Abbreviations: ROC, receiver-operating characteristic; VTE, venous thromboembolism. |
Discussion
Originally, the Caprini RAM was developed for assessing thrombosis risk in both surgical and medical patients.17 Although many reports have demonstrated its validity in identifying VTE risk among surgical patients,7–12 its performance in identifying VTE risk during peripartum was limited.13 Tran et al showed that the Caprini RAM would define a large proportion of pregnant women as high VTE risk during peripartum and was correlated with high the number needed to treat,13 and the limitation of this study was a small sample size of VTE patients with only three. In our study, 31 women who experienced a VTE event during puerperium were retrospectively enrolled. Through a relatively large sample size, we confirmed that the Caprini RAM was independently associated with VTE during puerperium. We also evaluated the predictive value of the Caprini RAM for VTE during puerperium using the ROC curve, and the results showed that its predictive value was low with an AUC of less than 0.700.
In order to elevate the predictive value for VTE during puerperium, we combined the Caprini RAM with D-dimer for the prediction of VTE during puerperium. As the product of cross-linked fibrin degradation, D-dimer mainly reflects the global coagulation activation and fibrinolysis. D-dimer is one of the most accurate and reliable biomarkers, and the elevation of D-dimer levels has been confirmed an association with the increased risk of VTE.18–20 The American College of Chest Physicians has recommended that D-dimer can be applied in predicting VTE.21
Studies on non-pregnant women have demonstrated that the negative predictive value (NPV) of D-dimer is helpful when employed to exclude PE through the combination with a low Wells score.22–25 D-dimer levels upregulate gradually during pregnancy and peaked at the first day after delivery,14 and most of healthy pregnant women demonstrate higher D-dimer levels compared with the normal reference range.15 Therefore, the “normal range” of non-pregnant women cannot be appropriate for pregnant women.26,27
The role of D-dimer in the prediction of VTE associated with pregnancy is still controversial. Hedengran et al demonstrated that the D-dimer level fluctuated by more than 50% among healthy pregnant women, and thus concluded that it might not be valuable for the prediction of VTE during pregnancy.27 Damodaram et al demonstrated that the sensitivity and specificity of D-dimer in predicting suspected PE among pregnant women was 73% and 15%, respectively, and the negative likelihood ratio was up to 1.8.28 Therefore, they suggested that a negative D-dimer result should not be used to exclude the diagnosis of PE among pregnant women. O’Connor et al showed that D-dimer was significantly less effective than the modified Wells score in prediction of PE.29 Hassanin et al showed that the sensitivity of D-dimer for the prediction of PE among postpartum women with symptoms suggestive of PE was up to 100.0%.30 Hu et al showed that D-dimer ≥3.70 mg/L was independently associated with VTE during puerperium, and the sensitivity and specificity of D-dimer for the prediction of VTE were 73.7% and 75.5%, respectively.16 These previous studies have been limited by small sample sizes. Our results were consistent with Hu et al. Furthermore, we evaluated the predictive value of the combination of the Caprini RAM and D-dimer for VTE during puerperium, and the ROC curves showed that the AUC of combination prediction was 0.840, significantly higher than individual prediction. The sensitivity and specificity of combination prediction were 83.9% and 80.3%, respectively. Therefore, the combination of the Caprini RAM and D-dimer could significantly elevate the predictive value for VTE during puerperium, and this new tool had the potential in the prediction of VTE during puerperium.
The main limitation of our study was that the study group represented a highly selected population because we excluded the patients with a history of DVT, superficial venous thrombosis, other cardiovascular diseases or tumors. These excluded complications are quite important in calculating a proper Caprini score and often these questions are not asked in clinical practice. Additionally, our sample size was still small for puerperium patients with VTE, although it was greater than those of previous studies.
Conclusion
The combination of the Caprini RAM and D-dimer could significantly elevate the predictive value for VTE during puerperium, and this new tool had the potential in the prediction of VTE during puerperium.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; agreed on the journal to which the article will be submitted; and agreed to be accountable for all aspects of the work.
Disclosure
All the authors do not have any conflict of interest.
References
1. Nichols KM, Henkin S, Creager MA. Venous Thromboembolism Associated With Pregnancy: JACC Focus Seminar. J Am Coll Cardiol. 2020;76(18):2128–2141. doi:10.1016/j.jacc.2020.06.090
2. Meng K, Hu X, Peng X, et al. Incidence of venous thromboembolism during pregnancy and the puerperium: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2015;28(3):245–253. doi:10.3109/14767058.2014.913130
3. Virkus RA, Løkkegaard EC, Bergholt T, et al. Venous thromboembolism in pregnant and puerperal women in Denmark 1995-2005. A national cohort study. Thromb Haemost. 2011;106(2):304–309. doi:10.1160/TH10-12-0823
4. Jackson E, Curtis KM, Gaffield ME. Risk of venous thromboembolism during the postpartum period: a systematic review. Obstet Gynecol. 2011;117(3):691–703. doi:10.1097/AOG.0b013e31820ce2db
5. Henriksson P, Westerlund E, Wallén H, et al. Incidence of pulmonary and venous thromboembolism in pregnancies after in vitro fertilisation: cross sectional study. BMJ. 2013;346:e8632. doi:10.1136/bmj.e8632
6. Abe K, Kuklina EV, Hooper WC, et al. Venous thromboembolism as a cause of severe maternal morbidity and mortality in the United States. Semin Perinatol. 2019;43(4):200–204. doi:10.1053/j.semperi.2019.03.004
7. Fu Y, Liu Y, Chen S, et al. The combination of Caprini risk assessment scale and thrombotic biomarkers to evaluate the risk of venous thromboembolism in critically ill patients. Medicine (Baltimore). 2018;97(47):e13232. doi:10.1097/MD.0000000000013232
8. Grant PJ, Greene MT, Chopra V, et al. Assessing the Caprini score for risk assessment of venous thromboembolism in hospitalized medical patients. Am J Med. 2016;129(5):528–535. doi:10.1016/j.amjmed.2015.10.027
9. Bilgi K, Muthusamy A, Subair M, et al. Assessing the risk for development of venous thromboembolism (VTE) in surgical patients using adapted Caprini scoring system. Int J Surg. 2016;30:68–73. doi:10.1016/j.ijsu.2016.04.030
10. Hachey KJ, Hewes PD, Porter LP, et al. Caprini venous thromboembolism risk assessment permits selection for postdischarge prophylactic anticoagulation in patients with resectable lung cancer. J Thorac Cardiovasc Surg. 2016;151(1):37–44.e1. doi:10.1016/j.jtcvs.2015.08.039
11. Lobastov K, Barinov V, Schastlivtsev I, et al. Validation of the Caprini risk assessment model for venous thromboembolism in high-risk surgical patients in the background of standard prophylaxis. J Vasc Surg Venous Lymphat Disord. 2016;4(2):153–160. doi:10.1016/j.jvsv.2015.09.004
12. Wu ZQ, Li KX, Zhu Q, et al. Application value of D-dimer testing and Caprini risk assessment model (RAM) to predict venous thromboembolism (VTE) in Chinese non-oncological urological inpatients: a retrospective study from a tertiary hospital. Transl Androl Urol. 2020;9(5):1904–1911. doi:10.21037/tau-20-320
13. Tran JP, Stribling SS, Ibezim UC, et al. Performance of Risk Assessment Models for Peripartum Thromboprophylaxis. Reprod Sci. 2019;26(9):1243–1248. doi:10.1177/1933719118813197
14. Wang M, Lu S, Li S, et al. Reference intervals of D-dimer during the pregnancy and puerperium period on the STA-R evolution coagulation analyzer. Clin Chim Acta. 2013;425:176–180. doi:10.1016/j.cca.2013.08.006
15. Réger B, Péterfalvi A, Litter I, et al. Challenges in the evaluation of D-dimer and fibrinogen levels in pregnant women. Thromb Res. 2013;131(4):e183–187. doi:10.1016/j.thromres.2013.02.005
16. Hu W, Wang Y, Li J, et al. The Predictive Value of d-Dimer Test for Venous Thromboembolism During Puerperium: a Prospective Cohort Study. Clin Appl Thromb Hemost. 2020;26:1076029620901786. doi:10.1177/1076029620901786
17. Caprini JA. Thrombosis risk assessment as a guide to quality patient care. Dis Mon. 2005;51(2–3):70–78. doi:10.1016/j.disamonth.2005.02.003
18. Ay C, Vormittag R, Dunkler D, et al. D-dimer and prothrombin fragment 1 + 2 predict venous thromboembolism in patients with cancer: results from the Vienna Cancer and Thrombosis Study. J Clin Oncol. 2009;27(25):4124–4129. doi:10.1200/JCO.2008.21.7752
19. Tian B, Song C, Li H, et al. The significance of perioperative coagulation and fibrinolysis related parameters after lung surgery for predicting venous thromboembolism: a prospective, single center study. J Thorac Dis. 2018;10(4):2223–2230. doi:10.21037/jtd.2018.03.174
20. Streiff MB, Agnelli G, Connors JM, et al. Guidance for the treatment of deep vein thrombosis and pulmonary embolism. J Thromb Thrombolysis. 2016;41(1):32–67. doi:10.1007/s11239-015-1317-0
21. Gould MK, Garcia DA, Wren SM, et al. Prevention of VTE in nonorthopedic surgical patients: antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e227S–e277S. doi:10.1378/chest.11-2297
22. Wells PS, Anderson DR, Rodger M, et al. Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer. Ann Intern Med. 2001;135(2):98–107. doi:10.7326/0003-4819-135-2-200107170-00010
23. Stein PD, Hull RD, Patel KC, et al. D-dimer for the exclusion of acute venous thrombosis and pulmonary embolism: a systematic review. Ann Intern Med. 2004;140(8):589–602. doi:10.7326/0003-4819-140-8-200404200-00005
24. Crawford F, Andras A, Welch K, et al. D-dimer test for excluding the diagnosis of pulmonary embolism. Cochrane Database Syst Rev. 2016;2016(8):CD010864. doi:10.1002/14651858.CD010864.pub2
25. van der Hulle T, Cheung WY, Kooij S, et al. YEARS study group. Simplified diagnostic management of suspected pulmonary embolism (the YEARS study): a prospective, multicentre, cohort study. Lancet. 2017;390(10091):289–297. doi:10.1016/S0140-6736(17)30885-1
26. Browne AM, Cronin CG, NiMhuircheartaigh J, et al. Evaluation of imaging quality of pulmonary 64-MDCT angiography in pregnancy and puerperium. AJR Am J Roentgenol. 2014;202(1):60–64. doi:10.2214/AJR.12.9917
27. Hedengran KK, Andersen MR, Stender S, et al. Large D-Dimer fluctuation in normal pregnancy: a longitudinal cohort study of 4117 Samples from 714 Healthy Danish Women. Obstet Gynecol Int. 2016;2016:3561675. doi:10.1155/2016/3561675
28. Damodaram M, Kaladindi M, Luckit J, et al. D-dimers as a screening test for venous thromboembolism in pregnancy: is it of any use? J Obstet Gynaecol. 2009;29(2):101–103. doi:10.1080/01443610802649045
29. O’Connor C, Moriarty J, Walsh J, et al. The application of a clinical risk stratification score may reduce unnecessary investigations for pulmonary embolism in pregnancy. J Matern Fetal Neonatal Med. 2011;24(12):1461–1464. doi:10.3109/14767058.2011.614652
30. Hassanin IM, Shahin AY, Badawy MS, et al. D-dimer testing versus multislice computed tomography in the diagnosis of postpartum pulmonary embolism in symptomatic high-risk women. Int J Gynaecol Obstet. 2011;115(2):200–201. doi:10.1016/j.ijgo.2011.05.024
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
