Back to Journals » ClinicoEconomics and Outcomes Research » Volume 15
Use of Conditionally Essential Amino Acids and the Economic Burden of Postoperative Complications After Fracture Fixation: Results from a Cost Utility Analysis
Authors Shafrin J , Than KS, Kanotra A, Kerr KW, Robinson KN, Willey MC
Received 15 March 2023
Accepted for publication 19 July 2023
Published 25 October 2023 Volume 2023:15 Pages 753—764
DOI https://doi.org/10.2147/CEOR.S408873
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Giorgio Colombo
Jason Shafrin,1 Kyi-Sin Than,1 Anmol Kanotra,1 Kirk W Kerr,2 Katie N Robinson,2 Michael C Willey3
1FTI Consulting, Center for Healthcare Economics and Policy, Los Angeles, CA, USA; 2Abbott Laboratories, Columbus, OH, USA; 3Department of Orthopedics & Rehabilitation, University of Iowa, Iowa City, IA, USA
Correspondence: Jason Shafrin, Center for Healthcare Economics and Policy, FTI Consulting, Los Angeles, CA, USA, Tel +1 213-452-6483, Email [email protected]
Objective: To measure the economic impact of conditionally essential amino acids (CEAA) among patients with operative treatment for fractures.
Methods: A decision tree model was created to estimate changes in annual health care costs and quality of life impact due to complications after patients underwent operative treatment to address a traumatic fracture. The intervention of interest was the use of CEAA alongside standard of care as compared to standard of care alone. Patients were required to be aged ≥ 18 and receive the surgery in a US Level 1 trauma center. The primary outcomes were rates of post-surgical complications, changes in patient quality adjusted life years (QALYs), and changes in cost. Cost savings were modeled as the incremental costs (in 2022 USD) of treating complications due to changes in complication rates.
Results: The per-patient cost of complications under CEAA use was $12,215 compared to $17,118 under standard of care without CEAA. The net incremental cost savings per patient with CEAA use was $4902, accounting for a two-week supply cost of CEAA. The differences in quality-adjusted life years (QALYs) under CEAA use and no CEAA use was 0.013 per person (0.739 vs 0.726). Modeled to the US population of patients requiring fracture fixations in trauma centers, the total value of CEAA use compared to no CEAA use was $316 million with an increase of 813 QALYs per year. With a gain of 0.013 QALYs per person, valued at $150,000, and the incremental cost savings of $4902 resulted in net monetary benefit of $6852 per patient. The incremental cost-effectiveness ratio showed that the use of CEAA dominated standard of care.
Conclusion: CEAA use after fracture fixation surgery is cost saving. Level of Evidence: Level 1 Economic Study.
Plain Language Summary: Postoperative complications after fracture fixation adversely impact clinical outcomes and impose substantial economic burden. Conditionally essential amino acids (CEAA) have been shown to reduce postoperative complication rates, but the economic impact is unclear.
In this study, we quantify the impact of CEAA on health care costs and quality of life related to postoperative complications.
The model demonstrates significant cost savings ($4902 per year per patient with operative treatment for fracture fixation) from the use of CEAA supplementation. Improving health outcomes and reducing health care costs for patients undergoing operative treatment for fracture fixation will be increasingly important for health systems as US payers increasingly shift provider reimbursement towards value-based care.
Keywords: postoperative complications, orthopedic surgery, fracture fixation, oral nutritional supplement, economic impact postoperative complications
Introduction
Despite significant advancements in surgical treatment of pelvis and extremity fractures, injury-related complications continue to adversely impact clinical outcomes.1–3 Nonunion complications more than double the total cost of care for fractures;4 venous thromboembolism approximately doubles the inpatient costs3 and causes significant economic burden associated with absenteeism and short-term disability.5 Surgical site infections result in almost twice the cost of orthopedic surgery, although some estimates indicate they more than triple the cost.6
Malnutrition is a common risk factor for complications following fracture fixation. Insufficient calorie and protein intake as a result of trauma, subsequent surgery, side effects of medications, and extended NPO (nothing by mouth) status may further compound baseline malnutrition.7,8 Underfeeding, combined with surgical stress and prolonged immobilization, often results in a catabolic state with decreased muscle protein synthesis and increased skeletal muscle wasting.9–12
Conditionally essential amino acids (CEAA) supplementation has the potential to reduce muscle atrophy and complications during the recovery phase after trauma.7,8,13 CEAA supplementation reduces overall complications, postoperative skeletal muscle loss, nonunion, and mortality.13 Additionally, CEAA supplementation improves length of stay in rehabilitation wards, number of infection episodes, fracture-related complications, and recovery of plasma proteins.7,8,14
Although there is clinical evidence of the benefits of CEAA supplementation to reduce complications after pelvic or extremity fracture,7,8,14 there are no existing studies that evaluated the economic impact of CEAA on postoperative complications to the best of our knowledge. To better understand the economic impacts of CEAA use, this study aims to quantify the economic value of CEAA use among patients that underwent operative fixation using a cost utility analysis.
Methods
Eligible Population
The model population was patients aged ≥18 years that underwent operative fixation of pelvis, lower extremity, or upper extremity fractures in the US.15 This study conducted a cost-utility analysis of the use of CEAA on operative fracture fixation treated in an inpatient setting.
Intervention and Comparators
This analysis evaluated the economic impact of CEAA use in addition to postoperative standard of care (CEAA scenario) compared to standard of care alone with no CEAA use (baseline scenario). CEAA was administered twice a day; patients drank two packets of CEAA mixed with water or juice daily in addition to their regular diet. In this study, standard of care may have included physical therapy and standard nutrition (but no CEAA).
Study Outcomes
The model estimated the clinical, health economic, and quality of life impact of CEAA use over a one (1)-year time horizon. Clinical impact outcomes include the number of patients with at least one complication (“overall complications”) and the number of patients by complication type (ie, medical complications, nonunion, surgical site infection (SSI), and reoperation). Medical complications include cardiovascular events, thromboembolism, pneumonia, urinary tract infection (UTI), and others. Health economic impact outcomes include total costs associated with each complication type and gains in quality-adjusted life years (QALYs).
Model Structure
The model relied on a decision tree to estimate the impact of CEAA use on complication rates by comparing rates between CEAA supplementation and baseline scenarios for patients that underwent operative fixation of fractures at hospitals in the US and associated health economic outcomes (Figure 1). ISPOR good practice guidance notes that decision trees are especially useful models with short-time horizons, a limited set of outcomes and with decisions known with more certainty as they allow for more model transparency and simplicity.16 These criteria apply to this model. The health economic outcomes are modeled as the direct cost savings from changes in complication rates as a result of CEAA intake.
 |
Figure 1 Economic Model Structure Overview. |
Efficacy of CEAA and Standard of Care
The likelihood that an individual develops a complication for the CEAA and baseline scenarios was estimated based on Hendrickson (2022) (Table 1), which included a broad range of fractures and examined specific post-surgical complication rates at a single level 1 trauma center.13 The Hendrickson paper was selected for two reasons. First, it was a randomized controlled trial which allowed for a valid estimate of the causal impact of CEAA on complications. Second, the study’s sample size was fairly large, with 400 subjects enrolled and randomized 50:50 between CEAA and control group. Other studies that evaluated the impact of CEAA on complications were not selected because they reported only overall complication rates or infections,7 were conducted outside of the US,8 or were not a randomized controlled trial or had smaller sample size. Hendrickson (2022) described medical complications to include cardiovascular events, thromboembolism, pneumonia, urinary tract infections, and other, but specific rates of these complications were not reported. Thus, rates for these specific medical complications were derived using the breakdown of medical complication post hip fracture surgery from Carpintero.17 Hendrickson13 did not report the proportion of patients that experience more than one complication; thus, we took a conservative approach of assuming that each patient developed only one complication. To do this, we rescaled the individual complication rates to match the overall complication rate.
 |
Table 1 Model Parameters |
Model Parameters
Parameters used to estimate the economic impact and quality of life impact were derived from the literature using a targeted literature review approach. Titles and abstracts of relevant articles from keyword searches were screened. Relevant full-text articles were reviewed, and additional searches were conducted by examining study references and forward citations of abstracts and articles, known as the pearl-growing approach.29
Economic Impact
The economic impact of CEAA supplementation was estimated via treatment costs for each complication obtained from the literature. The cost for each complication was the total medical costs to treat per occurrence of the respective complication, for which we provide details on the units and sources used in the Table S1. Due to limited cost data that capture specific complications across all fracture types, costs for nonunion and reoperation following common fracture types were used.4,17 Costs for each type of medical complication and surgical site infection were obtained from the literature (Table 1).18–22, The retail price of CEAA is estimated to be $37.80 per patient per week,30 and the course of CEAA was 2 weeks,13 resulting in a total of $76 (Table 1). All costs were adjusted for inflation to 2022 dollars using the Bureau of Labor Statistics’ Consumer Price Index (CPI).31
The likelihood of developing each complication was multiplied by the cost to treat each complication to estimate the economic impact. The impact of CEAA on complications was derived by taking the difference in resulting economic impact between baseline and CEAA scenarios net of CEAA cost. The per-person incremental costs of CEAA vs no CEAA were applied to the population of patients that underwent operative fixation.
Quality of Life
The negative quality of life impact of each complication was estimated using QALYs over a one-year time horizon. QALYs are a mathematical construct that allow economists to compare changes in health outcomes in a numerical manner after accounting for morbidity and mortality impacts of different health interventions.32 QALYs are calculated from health state utility values ranging from 0 (death) to 1 (perfect health) and the number of years spent in each state. In our model, two different health states with different quality of life values were possible to account for the utility impact of complications: (1) acute state of complications after surgery and (2) chronic state after the acute period. For the acute state, the decrement of a complication was applied to the utility of orthopedic surgery for the excess number of inpatient days due to complications. For example, an orthopedic surgery without complications would have a utility of 0.79 in the month following surgery. However, the decrement in utility from a cardiovascular event was calculated as percent decrement of utility associated with cardiovascular events (0.72) from utility of perfect health (1.0), which is 28%. Thus, a fracture fixation surgery patient with a cardiovascular event would have a 28% decrease in their orthopedic surgery utility resulting in a utility of 0.57 (1–0.28*0.79) during the acute state, applied to the excess 6.25 inpatient days in the first month. For the remaining months of the year (in the chronic state), the utility value of the complication was applied (eg, 0.72 for cardiovascular complications). Utility values associated with each complication were obtained from the literature, which were based on a variety of methodologies including time tradeoff,33,34 EQ-5D scores,35 Medical Outcome Study Short Form 36,36 and systematic literature reviews of health utilities(Table S2).37 Mortality was significantly less with CEAA,13 but due to the small number of deaths in each group, we assumed no mortality benefit of using CEAA in our baseline approach, but in the sensitivity analysis we do incorporate the reported mortality impact. Quality of life parameters are available in the Supplement (Table S2, Supplemental Content, which shows the value and methodology associated with each complication).
Cost-effectiveness of CEAA
Cost-effectiveness of CEAA use was estimated using the incremental cost-effectiveness ratio, calculated as the difference in the total incremental net costs of CEAA vs no CEAA divided by the changes in total QALY. The net monetary benefit of CEAA was calculated as the sum of cost savings and monetary benefit of QALYs gained per person.
Extrapolating per Person Results to US Population
To derive the number of operative treatments for fracture fixation in the US, data from the Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample (NIS), 2018 was used.25 Specifically, we used counts of admissions for the following admission types (ie, DRGs): Fractures of the Hip and Pelvis with and without major complication or comorbidity (MCC) (535, 536); Fractures of Femur with and without MCC (533, 534), Fracture, Sprain, Strain and Dislocation Except Femur, Hip, Pelvis, and Thigh with and without MCC (562, 563). The proportion of fracture discharges that received operative treatment was estimated using data from the literature.23 The most recently available and comprehensive literature on specific types of fractures was used to approximate the proportion of patients that underwent operative fixation of fractures because estimates that capture a broad category of fractures are not available. Population parameters are shown in Table 1.
Sensitivity Analysis
A series of sensitivity analyses were performed to test the robustness of the model estimates. First, we incorporated the mortality impact of CEAA. Hendrickson13 found statistically significant differences in mortality between CEAA and control groups, but to be conservative, we did not include this benefit in the baseline model structure. Second, we also tested the sensitivity of the model to key parameters by performing a deterministic sensitivity analysis of varying parameter estimates from low (−20%) to high (+20%) for key parameter values (Table S3). The specific parameter values varied included: overall complication rate and costs of complications for each complication type. For overall complication rates, we ran two sensitivity analyses: 1) varying the overall complication rates for standard of care (ie, no CEAA) only, and 2) varying the relative decrease in complications for CEAA. Third, we tested the uncertainty in our key parameters – complication rates and cost of each complication – by performing a probabilistic sensitivity analysis. Fourth, we varied the cost-effectiveness threshold with a $50,000 and $100,000 per QALY thresholds.
Results
The per-patient cost of complications under CEAA use was $12,215 compared to $17,118 under standard of care without CEAA (Table 2). The incremental cost savings per patient with CEAA use were estimated to be $4902, with the largest savings driven by reductions in nonunion complication ($1731) followed by reductions in reoperation ($1326), medical complications ($1003), and surgical site infections ($918) (Table 2 and Figure 2). Cost savings from reduction of medical complications were driven by reductions in thromboembolism and cardiovascular events, $409 and $361, respectively (see Figure S1, which shows cost of medical complications by type).
 |
Table 2 Per Person Incremental Costs Comparing CEAA Use and Standard of Care (No CEAA Use) |
 |
Figure 2 Per Person Incremental Costs Comparing CEAA Use and Standard of Care (No CEAA Use). |
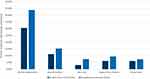 |
Figure 3 Clinical Complications Parameters Overall and by Type. |
The likelihood of a patient developing complications in our model matched findings from Hendrickson (2022), 43.8% under standard of care with no CEAA and 30.5% with CEAA use (Table 1). Under the conservative assumption that each patient developed only one complication, the rescaled probability of developing complications from Hendrickson (2022) under no CEAA and CEAA scenarios were: medical complications (15.3% vs 11.2%), nonunion (7.5% vs 3.1%), surgical site infection (9.4% vs 6.1%), and reoperation (7.4% vs 6.1%), respectively (Figure 3).
During the year, patient quality of life increased by 1.8% with CEAA use. Specifically, the QALYs under CEAA use and no CEAA use were 0.739 and 0.726 per person, respectively (Table 3). The monetary benefit of QALYs gained per person was estimated to be $110,850 under CEAA use and $108,900 without CEAA use, thus adding a net value of $1950 (Table 3). Taking this into account along with the incremental cost savings of $4902 resulted in the net monetary benefit of $6852 per patient with operative treatment for fracture fixation.
 |
Table 3 Quality of Life Impact per Person and Total Population of Fracture Patients with Operative Treatment for Fracture Fixation |
In the model, the total number of pelvis and extremity fracture patients with operative treatment for fracture fixation in the US was 64,507. The total number of complications was estimated to be 28,254 under standard of care (ie, no CEAA) and 19,675 with CEAA use. The estimated number of complications with CEAA use is lower when compared to care without CEAAs for all complication types considered in the study, with the largest reduction in patients that developed non-union (2963), followed by medical (2657), surgical site infection (2209), and reoperation (866) complications (Figure S2, which shows the total number of complications by type). The largest reduction in medical complications was due to the decrease in the number of patients with cardiovascular events (930), followed by thromboembolism (755), other medical complications (468), UTI (319), and pneumonia (186) (Figure S3, which shows the total number of medical complications by type).
The total value of CEAA use compared to no CEEA use for US patients with pelvis and extremity fractures was $316 million with an increase of 813 QALYs. With an incremental cost-effectiveness ratio of -$395,174, the use of CEAA dominates the standard of care because the use of CEAA resulted in net cost savings and improves quality of life.
In the sensitivity analysis, the mortality benefit was included to assess the impact on costs alone. The QALY gain without mortality benefit from CEAA use was 0.013 per person compared to 0.031 per person when mortality benefit was incorporated. Consequently, the net monetary benefit of reduction in mortality rate in the CEAA scenario was $8513 compared to $6892 in the no CEAA scenario. The results of the model were most sensitive to improved overall complication rates for CEAA and least sensitive to changes in the cost of UTI events (Figure 4). The lower and upper bound of overall complication rates resulted in an 85% decrease ($667) and a 56% increase ($11,254) in cost savings, respectively, from our baseline estimate of $4902. Due to the scale of UTI costs, the model was least sensitive to changes in these costs, fluctuating between ± 0.21% in total cost savings from the baseline model. Sensitivity parameters are available in Table S1, which shows low, base, and high-sensitivity parameter values. The probabilistic sensitivity analysis estimated an average net monetary benefit of $5535 (95% credible interval: $2213, $8858). Using a $50,000/QALY and $100,000/QALY thresholds resulted in a net monetary benefit of $5552 and $6202, respectively.
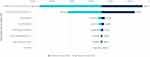 |
Figure 4 Deterministic Sensitivity Analysis Results – Total Costs Per Patient with Operative Treatment for Fracture Fixation. |
Discussion
This economic model quantifies the impact of CEAA on health care costs and quality of life related to postoperative complications after fracture fixation in the US. Our model predicts that CEAA use would decrease the total annual number of complications from 28,254 to 19,675 among patients that require operative fixation for fractures. Per patient costs net of CEAA costs decreased by an average of $4902 due to the reduction in cost of complications. The monetary benefit of gains in QALYs from reductions in complications was estimated to be valued at $1926 per patient.
Despite evidence supporting the benefit of CEAA supplementation, CEAA supplementation is not routinely utilized after orthopedic surgery, potentially due to lack of reimbursement by health insurance as part of an inpatient stay. Thus, hospitals (or patients) must fund the use of CEAA from their own budget, which could hinder use and adherence of CEAA after operative treatment for fracture fixation. Depending on where post-discharge complications are treated, hospitals may not realize the benefits of using CEAA. However, value-based bundled payments within reimbursement schemes such as the Centers for Medicare and Medicaid Services, Comprehensive Care for Joint Replacement (CJR) program could potentially better align incentives for both hospitals and providers to reduce costs through reductions in complications and associated readmissions or more intensive post-acute care, as well as improve quality of care metrics such as the Hospital-Level Risk-Standardized Complication Rate (RSCR) Following Elective Primary THA and/or TKA (NQF#1550). Further, bundled payment programs such as CJR include fraud and abuse waivers to provide TKA/THA episode beneficiaries with in-kind items or services during an episode of care that would be preventive or advance a clinical goal.
To our knowledge, this is the first study to quantify the economic impact of CEAA use among patients indicated for operative fracture fixation. The economic impact is quantified in terms of reduction in cost and increase in QALYs. Further, changes in complication rates due to CEAA were estimated from a recent clinical impact study.13 Furthermore, most studies estimating the impact of CEAA supplementation on complications only include general complication rates without specifying the types of complications.7,8 This study disaggregated overall complications by medical, non-union, surgical site infection, and reoperation, as well as specific types of medical complications for a more granular analysis.
This study has a number of limitations. First, the types of complications included only those described in Hendrickson,13 which did not report results for specific types of medical complications. We obtained a distribution of specific types of medical complications from Carpintero (2014) to fill this gap.17 Therefore, medical complication rates by type may not necessarily be the same as those that would have been found in the clinical impact study. Second, the impact of CEAA on postoperative SSI was not statistically significant in the clinical impact study.13 However, we included the impact of CEAA on SSI in our economic model because of the potential increased risk of SSI among undernourished patients and the trends suggesting CEAA use decreased SSIs.38,39 Furthermore, excluding the benefit of CEAA on SSI did not materially alter the qualitative findings that CEAA is cost saving. Third, for the proportion of patients receiving operative treatment within the upper and lower extremity categories, proportions for common types of within-category fractures were used when general proportions were not available. Fourth, the results described were under the baseline assumption that only one type of complication occurred per patient, and so we do not consider the case for potential multiple complications. Nevertheless, this assumption is conservative as CEAA may be more beneficial if it can also reduce the likelihood of multiple complications. Fifth, the model did not incorporate whether real-world adherence to CEAA differed from Hendrickson. Because the current model was limited to the inpatient setting, however, this is less problematic than would be the case for outpatient administration of CEAA. Thus, our estimate may be conservative. Fifth, this model was created from a payer perspective, and so did not consider productivity and caregiver burden improvements due to reduced complications from CEAA supplementation. Sixth, the Hendrickson et al study used in the model as a basis for CEAA efficacy is set in a single level-1 trauma center in American Midwest, which has limitations in terms of generalizability, but the study included all adult patients undergoing operative fixation of acute fractures, covering a wide range of trauma to increase generalizability.13 Other studies have also found similar results, with CEAA supplementation reducing muscle loss post-elective orthopedic surgery, as well as maintenance of lean muscle mass in chronic disease and management of wounds.40–46 Seventh, this model did not consider the impact of reduced loss of skeletal muscle mass on function and quality of life seen with CEAA supplementation.13 Since these factors affect quality of life, the current estimates are likely conservative. Open areas of research for the future include the economic impact of prophylactic use of CEAA since this study was limited to postoperative CEAA use.
Conclusion
This study finds that the use of CEAA after operative treatment for fracture fixation can realize both cost savings and improve quality of life. The economic result was driven by the fact that CEAA has been shown to reduce complications after surgery. The cost saving from reduced complications more than offset the additional cost of CEAA. Health care providers and professional associations should evaluate the value of CEAA use as part of surgical recovery in the development of Enhanced Recovery After Surgery (ERAS) guidelines. Health care systems and payers should consider incorporating CEAA supplementation into orthopedic trauma surgical protocols as a proactive step to reduce costs and improve patient outcomes. Reducing overall costs and complications through use of CEAA supplementation will be increasingly attractive under alternative payment models where systems bear the risk of additional costs due to complications and are consistent with increased focus on treatment value linked to both quality of care and cost.
Acknowledgments
An abstract containing preliminary results from this project was presented at the ISPOR 2023 conference.
Disclosure
Dr Jason Shafrin, Ms Kyi-Sin Than and Ms. Anmol Kanotra are employees of FTI Consulting which received funding from Abbott Laboratories. Dr Kirk W Kerr and Dr Katie N Robinson are employees of Abbott Nutrition. Dr Michael C Willey reports grants from Orthopaedic Trauma Association, Centers for Disease Control, Arthritis Foundation, Department of Defense, and Excere Inc, outside the submitted work; and this secondary analysis of a previous clinical trial was supported by Abbott Laboratories that produces the nutrition supplement (Juven) used as the intervention. The authors report no other conflicts of interest in this work.
References
1. Delanois RE, Mistry JB, Gwam CU, Mohamed NS, Choksi US, Mont MA. Current epidemiology of revision total knee arthroplasty in the United States. J Arthroplasty. 2017;32(9):2663–2668. doi:10.1016/j.arth.2017.03.066
2. Ekegren CL, Edwards ER, de Steiger R, Gabbe BJ. Incidence, costs and predictors of non-union, delayed Union and Mal-union following long bone fracture. Int J Environ Res Public Health. 2018;15(12):1–11. doi:10.3390/ijerph15122845
3. Trivedi NN, Abola MV, Kim CY, Sivasundaram L, Smith EJ, Ochenjele G. The incremental cost of inpatient venous thromboembolism after hip fracture surgery. J Orthop Trauma. 2020;34(4):169–173. doi:10.1097/bot.0000000000001675
4. Antonova E, Le TK, Burge R, Mershon J. Tibia shaft fractures: costly burden of nonunions. BMC Musculoskelet Disord. 2013;14(1):42. doi:10.1186/1471-2474-14-42
5. Bonafede M, Espindle D, Bower AG. The direct and indirect costs of long bone fractures in a working age US population. J Med Econ. 2013;16(1):169–178. doi:10.3111/13696998.2012.737391
6. Wise BT, Connelly D, Rocca M, et al. Are deep infections that present before and after 90 days from orthopaedic trauma different? An analysis of the validity of the recent change in CDC criteria for infections. Injury. 2022;53(3):912–918. doi:10.1016/j.injury.2021.10.020
7. Myint MW, Wu J, Wong E, et al. Clinical benefits of oral nutritional supplementation for elderly hip fracture patients: a single blind randomised controlled trial. Age Ageing. 2013;42(1):39–45. doi:10.1093/ageing/afs078
8. Eneroth M, Olsson UB, Thorngren KG. Nutritional supplementation decreases hip fracture-related complications. Clin Orthop Relat Res. 2006;451:212–217. doi:10.1097/01.blo.0000224054.86625.06
9. Deutz NE, Pereira SL, Hays NP, et al. Effect of beta-hydroxy-beta-methylbutyrate (HMB) on lean body mass during 10 days of bed rest in older adults. Clin Nutr. 2013;32(5):704–712. doi:10.1016/j.clnu.2013.02.011
10. Wall BT, Dirks ML, Snijders T, Senden JM, Dolmans J, van Loon LJ. Substantial skeletal muscle loss occurs during only 5 days of disuse. Acta Physiol. 2014;210(3):600–611. doi:10.1111/apha.12190
11. Glover EI, Phillips SM, Oates BR, et al. Immobilization induces anabolic resistance in human myofibrillar protein synthesis with low and high dose amino acid infusion. J Physiol. 2008;586(24):6049–6061. doi:10.1113/jphysiol.2008.160333
12. Puthucheary ZA, Rawal J, McPhail M, et al. Acute skeletal muscle wasting in critical illness. JAMA. 2013;310(15):1591–1600. doi:10.1001/jama.2013.278481
13. Hendrickson NR, Davison J, Glass NA, et al. Conditionally essential amino acid supplementation reduces postoperative complications and muscle wasting after fracture fixation: a randomized controlled trial. J Bone Joint Surg Am. 2022;104(9):759–766. doi:10.2106/jbjs.21.01014
14. Botella-Carretero JI, Iglesias B, Balsa JA, Arrieta F, Zamarron I, Vazquez C. Perioperative oral nutritional supplements in normally or mildly undernourished geriatric patients submitted to surgery for Hip fracture: a randomized clinical trial. Clin Nutr. 2010;29(5):574–579. doi:10.1016/j.clnu.2010.01.012
15. Wu A-M, Bisignano C, James SL; Global Burden of Disease 2019 Fracture Collaborators. Global, regional, and national burden of bone fractures in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev. 2021;2(9):e580–e592. doi:10.1016/S2666-7568(21)00172-0
16. Roberts M, Russell LB, Paltiel AD, Chambers M, McEwan P, Krahn M. Conceptualizing a model. Med Decis Making. 2012;32(5):678–689. doi:10.1177/0272989x12454941
17. Carpintero P, Caeiro JR, Carpintero R, Morales A, Silva S, Mesa M. Complications of hip fractures: a review. World J Orthop. 2014;5(4):402–411. doi:10.5312/wjo.v5.i4.402
18. Chapman RH, Liu LZ, Girase PG, Straka RJ. Determining initial and follow-up costs of cardiovascular events in a US managed care population. BMC Cardiovasc Disord. 2011;11(1):11. doi:10.1186/1471-2261-11-11
19. Shahi A, Chen AF, Tan TL, Maltenfort MG, Kucukdurmaz F, Parvizi J. The incidence and economic burden of in-hospital venous thromboembolism in the United States. J Arthroplasty. 2017;32(4):1063–1066. doi:10.1016/j.arth.2016.10.020
20. Tong S, Amand C, Kieffer A, Kyaw MH. Trends in healthcare utilization and costs associated with pneumonia in the United States during 2008–2014. BMC Health Serv Res. 2018;18(1):715. doi:10.1186/s12913-018-3529-4
21. Simmering JE, Tang F, Cavanaugh JE, Polgreen LA, Polgreen PM. The increase in hospitalizations for urinary tract infections and the associated costs in the United States, 1998–2011. Open Forum Infect Dis. 2017;4(1). doi:10.1093/ofid/ofw281
22. Zimlichman E, Henderson D, Tamir O, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173(22):2039–2046. doi:10.1001/jamainternmed.2013.9763
23. Gwam CU, Mistry JB, Mohamed NS, et al. Current epidemiology of revision total hip arthroplasty in the United States: national inpatient sample 2009 to 2013. J Arthroplasty. 2017;32(7):2088–2092. doi:10.1016/j.arth.2017.02.046
24. U.S. Census Bureau. Data from Age and Sex S0101. 2020
25. HCUPnet. Healthcare cost and utilization project. Rockville, MD; 2018.
26. Woon CYL, Moretti VM, Schwartz BE, Goldberg BA, Total Hip Arthroplasty and Hemiarthroplasty: US National Trends in the Treatment of Femoral Neck Fractures. Am J Orthop. Nov/Dec 2017;46(6):E474–e478.
27. Sporer SM, Weinstein JN, Koval KJ, The geographic incidence and treatment variation of common fractures of elderly patients. J Am Acad Orthop Surg. Apr 2006;14(4):246–55. doi:10.5435/00124635-200604000-00006
28. Bell J-E, Leung BC, Spratt KF, et al. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. The Journal of Bone and Joint Surgery-American Volume. 2011;93(2):121–131
29. Sandieson R. Pathfinding in the research forest: the Pearl harvesting method for effective information retrieval. Educ Train Dev Disabil. 2006;41(4):401–409.
30. Abbott Laboratories. Juven powder. Available from: https://abbottstore.com/therapeutic-nutrition/juven/juven/juven-powder/juven-fruit-punch-1-02-oz-packet-30-pack-66680p30.html.
31. CPI Inflation Calculator. U.S. Bureau of Labor Statistics. Available from: https://www.bls.gov/data/inflation_calculator.htm.
32. Torrance GW, Feeny D. Utilities and quality-adjusted life years. Int J Technol Assess Health Care. 2009;5(4):559–575. doi:10.1017/s0266462300008461
33. Schottel PC, O’Connor DP, Brinker MR. Time trade-off as a measure of health-related quality of life: long bone nonunions have a devastating impact. J Bone Joint Surg Am Vol. 2015;97(17):1406–1410. doi:10.2106/jbjs.N.01090
34. Matza LS, Kim KJ, Yu H, et al. Health state utilities associated with post-surgical Staphylococcus aureus infections. Eur J Health Econ. 2019;20(6):819–827. doi:10.1007/s10198-019-01036-3
35 Sullivan PW, Ghushchyan V. Preference-based EQ-5D index scores for chronic conditions in the United States. Med Decis Making. 2016;26(4):410–420. doi:10.1177/0272989x06290495
36. Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sexton DJ. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol. 2015;23(4):183–189. doi:10.1086/502033
37. Shiri T, Khan K, Keaney K, Mukherjee G, McCarthy ND, Petrou S. Pneumococcal disease: a systematic review of health utilities, resource use, costs, and economic evaluations of interventions. Value Health. 2019;22(11):1329–1344. doi:10.1016/j.jval.2019.06.011
38. Blumetti J, Luu M, Sarosi G, et al. Surgical site infections after colorectal surgery: do risk factors vary depending on the type of infection considered? Surgery. 2007;142(5):704–711. doi:10.1016/j.surg.2007.05.012
39. Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF. Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the National VA Surgical Risk Study. Arch Surg. 1999;134(1):36–42. doi:10.1001/archsurg.134.1.36
40. Aquilani R, Zuccarelli Ginetto C, Rutili C, et al. Supplemented amino acids may enhance the walking recovery of elderly subjects after Hip fracture surgery. Aging Clin Exp Res. 2019;31(1):157–160. doi:10.1007/s40520-018-0941-x
41. Rondanelli M, Guido D, Faliva MA, et al. Effects of essential amino acid supplementation on pain in the elderly with Hip fractures: a pilot, double-blind, placebo-controlled, randomised clinical trial. J Biol Regul Homeost Agents. 2020;34(2):721–731. doi:10.23812/19-452-L-46
42. Muyskens JB, Foote DM, Bigot NJ, et al. Cellular and morphological changes with EAA supplementation before and after total knee arthroplasty. J Appl Physiol. 2019;127(2):531–545. doi:10.1152/japplphysiol.00869.2018
43. Ueyama H, Kanemoto N, Minoda Y, Taniguchi Y, Nakamura H. Ranawat award: perioperative essential amino acid supplementation suppresses rectus femoris muscle atrophy and accelerates early functional recovery following total knee arthroplasty. Bone Joint J. 2020;102(6_Supple_A):10–18. doi:10.1302/0301-620X.102B6.BJJ-2019-1370.R1
44. Dreyer HC, Owen EC, Strycker LA, et al. Essential amino acid supplementation mitigates muscle atrophy after total knee arthroplasty: a randomized, double-blind, placebo-controlled trial. JB JS Open Access. 2018;3(2):e0006. doi:10.2106/JBJS.OA.18.00006
45. Clark RH, Feleke G, Din M, et al. Nutritional treatment for acquired immunodeficiency virus-associated wasting using beta-hydroxy beta-methylbutyrate, glutamine, and arginine: a randomized, double-blind, placebo-controlled study. JPEN J Parenter Enteral Nutr. 2000;24(3):133–139. doi:10.1177/0148607100024003133
46. Williams JZ, Abumrad N, Barbul A. Effect of a specialized amino acid mixture on human collagen deposition. Ann Surg. 2002;236(3):369–374. doi:10.1097/00000658-200209000-00013
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
