Back to Journals » Journal of Healthcare Leadership » Volume 15
Unveiling the Impact of Lean Leadership on Continuous Improvement Maturity: A Scoping Review
Authors Hilverda JJ, Roemeling O , Smailhodzic E, Aij KH, Hage E, Fakha A
Received 22 June 2023
Accepted for publication 29 September 2023
Published 10 October 2023 Volume 2023:15 Pages 241—257
DOI https://doi.org/10.2147/JHL.S422864
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Pavani Rangachari
Jesse Jorian Hilverda,1 Oskar Roemeling,2 Edin Smailhodzic,2 Kjeld Harald Aij,3 Eveline Hage,2 Amal Fakha2
1Department of Audit & Risk Management, University Medical Center Groningen, Groningen, the Netherlands; 2Department of Innovation, Management & Strategy, University of Groningen, Groningen, the Netherlands; 3Dijkzigt, Erasmus MC, Rotterdam, the Netherlands
Correspondence: Oskar Roemeling, Department of Innovation, Management & Strategy, University of Groningen, P.O. Box 800, 9700 AV, Groningen, the Netherlands, Tel +31 05 363 2025, Email [email protected]
Purpose: Lean Management (LM) is a process improvement approach with growing interest from healthcare organizations. Obtaining a culture of continuous improvement is a primary objective of LM, and a culture of continuous improvement indicates a mature LM approach, and here leadership plays a central role. However, a comprehensive overview of leadership activities influencing LM maturity is lacking. This study aims to identify leadership activities associated with continuous improvement and, thus, LM, maturity.
Methods: Following the PRISMA guidelines, a scoping literature review of peer-reviewed articles was conducted in twenty healthcare management journals. The search provided 466 articles published up until 2023. During the selection process, 23 studies were included in the review. The leadership activities related to continuous improvement maturity were identified using the grounded theory approach and data coding.
Results: The analysis highlighted a total of 58 leadership activities distributed across nine themes of LM leadership. Next, analysing leadership activities concerning the different maturity levels revealed three maturity stages: beginner, intermediate, and expert. Based on the findings, we propose a framework that guides suitable leadership activities at the various stages of LM maturity. The framework provides leaders in healthcare with a practical overview of actions to facilitate the growth of the LM approach, and the related propositions offer academics a theoretical basis for future studies.
Conclusion: This review presents the first comprehensive overview of LM leadership activities in relation to continuous improvement and LM maturity. To enhance LM maturity, leaders are encouraged to consider their leadership style, (clinical) stakeholder involvement, alignment with the organizational strategy, and their role in promoting employee autonomy.
Keywords: lean management, lean healthcare, continuous improvement, lean leadership, leadership activities, lean adoption
Introduction
Leaders in healthcare organizations (HCOs) are increasingly confronted with external pressures that require changes to become more efficient at lower costs whilst maintaining or improving the quality of care.1,2 To cope with these pressures in the long term, HCOs apply quality improvement methods.3 As care pathways and patient journeys are similar to a production process, with units creating value for the patient through multiple steps, lean management (LM) offers a framework to guide process improvement.4,5 LM can be defined as a management practice aimed at enhancing organizational efficiency through a process of continuous improvement (CI) aimed at maximizing value-adding activities and eliminating waste.6 LM has roots in the manufacturing environment and has been successfully applied by and adapted to HCOs in recent years.7
LM is used to facilitate strategic change, to improve quality, and to reduce costs.8 One of the main objectives of LM is to develop a culture of continuous improvement (CI). In such a culture, improvement activities are championed by employees and recognized as part of everyday work rather than being seen as discrete improvement-related projects.9 CI is defined as the ongoing change process to improve quality and reduce waste for overall performance.2,10 To better understand the depth of LM applications in HCOs, a structured assessment of the deployment of LM is required.11 Liker12 suggests that this application depth can be measured by the extent to which LM principles are present, known as the level of LM maturity. In addition, Bessant et al13 developed a five-level CI-model to assess the degree of application of LM, in which LM maturity is recognized as full integration of CI. In our research, we use these ideas to establish if a culture of CI is present, which implies that we have reached LM maturity.
Prior research focused on LM in healthcare aimed to explore factors that influence LM maturity; studies recognize strong leadership and high commitment of managers and physicians, continuous training, and the hospital’s involvement in CI as examples of facilitators.7,14,15 Examples that inhibit maturity are lack of knowledge by LM leaders, insufficient resource availability, and provision of training not tailored to the healthcare context.15–18 In addition, the Center for Lean Engagement and Research in Healthcare (CLERH) recognized leadership, commitment, standard work, communication and a daily management system as overarching factors influencing LM maturity.11 Moreover, leadership is important in LM approaches.19–23 LM leaders are coaches who create the strategy, build the team, and help employees develop their skills within the LM initiative.24 Hence, leadership is central to LM and, thus, LM maturity.
Previous studies on LM leadership in healthcare identified various leadership activities influencing LM maturity, such as adopting a hybrid leadership style, empowering employees to become Lean leaders, involving them in decision-making processes, and establishing LM as a long-term CI program.25–30 The previous studies underline the importance of leadership in LM maturity. Yet, a clear overview of LM leadership activities in relation to LM maturity and the culture of CI has come to pass. To the best of our knowledge, this research is the first to systematically review the literature on LM in the healthcare setting to address this gap. Our work relates to the study of Aij et al,24 who reported on the role of LM leadership and servant leadership in relation to LM transitions.
The primary objective of this study is to develop a growth model that connects leadership activities identified in the literature to specific LM maturity phases. By doing so, the model offers a guideline for organizational leaders to spur the adoption, and thus maturity, of LM within HCOs. In line with these objectives, this study seeks to answer the following research question: “How do leadership activities facilitate a culture of continuous improvement and, thus, lean management maturity?”
Identifying leadership activities in relation to LM maturity can contribute to the success of LM initiatives. The proposed framework guides leaders in the transition to a mature LM approach. From an academic perspective, this study contributes to existing research within the LM leadership domain by aggregating empirical LM leadership activities in relation to the levels of CI maturity and furthering our understanding through the development of propositions.
Methods
This scoping literature review has been conducted using empirical research that reported on LM in health care. We identified leadership activities influencing LM maturity, and we related these LM leadership activities to different levels of maturity.14 A literature review focuses on identifying, evaluating and synthesizing literature systematically, reproducibly and comprehensively,31 argued appropriately to answer the research question. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines32 were followed to report on the literature selection and guide the review process. The search strategy was three-pronged: 1) defining inclusion and exclusion criteria; 2) composing a search string; and 3) assessing remaining articles on eligibility through full-text review. Ultimately, this resulted in the final set of 23 articles included in this review. Coding supported the analysis of the included studies. In the remainder of this section, we further elaborate on the applied methodology.
Databases
As LM is a popular approach in various domains (eg, manufacturing, services), and we were explicitly interested in healthcare management, we required a focused approach for our data selection. Moreover, we aimed to arrive at a diverse dataset that offers a global perspective on leadership and avoids ethnocentrism. To that end, we follow Meese et al, who asked healthcare management or public health academic experts from all high-income Organisation for Economic Co-operation and Development (OECD) countries to list the most influential journals in the healthcare management domain.33 For this review, we selected the 20 top journals on the Meese-ranking. The resulting list is of highl quality, geographically diverse and differs substantially from pre-existing US or European rankings. This approach ensures the relevance of our findings for healthcare, and conducting the literature review on this subset of journals reduces possible viewpoint biases.33 In addition, it enhances the validity and accuracy of the current study.34 The specific databases were directly accessed for the identification and collection of articles, an overview of the included journals is added to Supplementary Table 1.
Inclusion and Exclusion Criteria
Following the research objectives, initial inclusion and exclusion criteria were established to include relevant articles (Table 1). Exclusively, English-written articles were included, as this is the most common language of LM healthcare research,7 and it is common amongst review articles to be limited to English.35 Only empirical studies reporting on LM in a healthcare context were included. We searched for articles that reported on the application of LM in the broadest sense, as we are interested in identifying relevant leadership activities in all the possible LM stages. Moreover, we did not apply any specific leadership inclusion criteria in order to be able to search as broadly as possible within the articles for leadership activities during later screening. In other words, we were careful not to exclude articles that might not specifically mention leadership but did report on activities that could be related to leadership.
 |
Table 1 Inclusion and Exclusion Criteria to Assess Eligibility Through Abstract Screening |
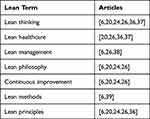 |
Table 2 Lean Search Terms Based on Lean in Healthcare Literature Reviews |
Keywords
LM is known by multiple names; therefore, several literature reviews on LM in healthcare were consulted to establish a comprehensive set of LM search terms. An overview of the various LM terms based on these literature reviews is presented in Table 2. Consequently, we applied the following search terms to identify as many LM studies as possible: lean thinking, lean management, lean healthcare, lean philosophy, continuous improvement, lean methods, and lean principles. We used no specific keywords concerning leadership activities, as we did not want to rule out studies that might not explicitly report on leadership but did report valuable activities that could be attributed to leadership.
As the selected journals (mainly) publish healthcare management research,33 the concept of healthcare was not included in the search string. However, during some preliminary search trials, we observed that the Academy of Management Journal and BMJ Quality & Safety did not exclusively publish articles within the healthcare domain. Hence, this resulted in an arguably inflated number of potential articles. Consequently, the search string for these two journals was adjusted slightly to obtain articles in the healthcare domain. The search strings in Table 3 were directly applied to the twenty journals, which led to the identification of 466 unique articles. The search was conducted in April 2023, ensuring that articles published until this month are included in the identification phase of this review.
 |
Table 3 Applied Search Strings |
Screening and Selection
Four hundred and sixty-six unique articles were taken to the screening phase, aiming to assess articles that relate to the research objective: identifying leadership activities relevant to reaching LM maturity. The abstracts of these 466 articles were screened with the inclusion and exclusion criteria, resulting in 45 eligible articles. Access to 40 of these articles was obtained via the journals and for five articles via direct request to authors. To determine the final set of articles included in this study, the 45 articles were assessed through a full-text review to determine if they matched the inclusion criteria and if leadership activities could be identified. The full-text review highlighted eleven articles found to be in an inappropriate study setting, six articles did not report on or link with leadership, four did not report on empirical research, and one did not report on LM, amounting to the exclusion of 22 articles. Following the PRISMA guidelines, our final set consisted of 23 articles, as shown in Figure 1. The 23 articles hold information on 34 unique HCOs that applied LM, as four reported on multiple case settings.
 |
Figure 1 PRISMA Diagram. |
Data Extraction and Analysis
The descriptive information was obtained using a data extraction form based on Okoli and Schabram (2010). The form was piloted before data extraction and aggregated after completion. The overview has been added to Supplementary Table 2. The collected descriptive information comprised the author(s), year of publication, journal, study context, research objective, and main findings. We applied the grounded theory approach to obtain the data that indicated the level of LM maturity and infer the leadership activities that were relevant in obtaining this level of maturity.40 To establish the LM maturity level, the articles were thoroughly read and categorized into one of the five maturity levels.13 To facilitate this process, we applied a maturity decision tree, which we added to the overview of the classification in Supplementary Table 3 and Supplementary Figure 1.
The extraction of LM leadership activities was supported by the software program Atlas.ti. Here, we proceeded as follows: articles were scanned to understand the concept of LM leadership.11,21,23,24,26,41 Through axial coding, excerpts of LM leadership activities were retrieved from the articles. New codes emerged during this inductive coding process, leading to the establishment of the codebook, which has been added in Supplementary Table 4. After completion of the coding, the coded excerpts were transferred to Excel. The excerpts indicating leadership activities were reviewed to merge similar activities. This resulted in a total of 58 different identified leadership activities. Subsequently, these activities were reviewed and adjusted to create LM leadership themes, resulting in the emergence of nine LM leadership themes.
Results
In this section, we provide the results of our literature review, and we begin with the presentation of the PRISMA-diagram, depicted in Figure 1, that shows the literature selection process.
Characteristics of Included Studies
In total, 23 unique articles were included in this review. An overview of the journals in which the studies were published is presented in Table 4, and the distribution of studies over countries is presented in Table 5. Supplementary Table 5 provides an overview of the descriptive information of the articles, the assessed level of LM maturity, including justification for this classification and other descriptive information deemed relevant. Through the included studies, we were able to identify 34 unique HCOs. As one of the HCOs39 reported on two stages of the LM implementation process, which were found to be in different levels of LM maturity, the two stages of LM implementation were considered as separate instances (labelled HCO 1a and 1b). This implies that we identify 35 unique cases taken to the analysis phase. An overview of the countries in which the 34 HCOs are based is shown in Table 4. The publication years of the studies are shown in Figure 2. The years of publication vary from 2010 to 2022, in which no identifiable trend was observed. The observation that HCOs from the United Kingdom (UK) and the United States (US) both account for one-third part of this literature review is in line with the finding that the UK and the US account for the largest number of publications on Lean healthcare.42
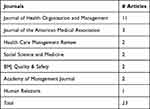 |
Table 4 Distribution of Articles by Journal |
 |
Table 5 Distribution of HCOs by Country |
 |
Figure 2 Distribution of publications over the years. |
Leadership Themes
During the analysis of the 58 leadership activities, nine themes of LM leadership emerged: Motivation, engagement, trust and support, Workforce involvement, Leadership style, Focus and vision, Learning, Training, Collaboration, Deployment and management, and Facilitating leadership. An overview of these themes and the underlying leadership activities has been added in Table 6.
 |
Table 6 Overview of LM Leadership Themes and Underlying Leadership Activities |
In the next step of our analysis, we aimed to offer insight into the occurrence of leadership activities across the levels of LM maturity. Through the use of cross-tables, it became apparent that HCOs in levels 1 and 2, as well as HCOs in levels 4 and 5, were typified by similar leadership activities. Hence, HCOs in levels 1 and 2 and those in 4 and 5 were grouped, resulting in three stages of LM maturity. The stages have been labelled Beginner (maturity levels 1 and 2), Intermediate (maturity level 3), and Expert (maturity levels 4 and 5). Next, we provide an overview of the identified leadership theme and the related leadership activities across the three stages of maturity.
Stage 1: Beginner (n=18)
The Beginner stage entails the findings from eighteen HCOs categorized in LM maturity level 1 or 2. Typical for this stage is that articles describing these HCOs tend to report negatively on the leadership activities or the absence of them. In the following subsections, the results of HCOs that operate at the maturity stage Beginner are presented per the theme.
Motivation, Engagement, Trust and Support
HCOs operating in the Beginner stage of maturity reported resistance among the workforce.2,16,36,39,43–47 Furthermore, HCOs reported scepticism among the workforce,2,16,39,46,48 which leaders did not take the initiative to dispel. In line with this, we identify that their employees feel jeopardized36,45,48,49 and do not trust the LM leader.16,43,45 This indicates that these leaders have difficulties creating trust and safety. Lastly, HCOs reported that some leaders succeeded in engaging higher management in the LM initiative.43,46,48–50
Workforce Involvement
HCOs operating in this stage of maturity commonly reported a lack of workforce involvement. Some of these HCOs specifically mentioned the absence of direct involvement of departmental managers, observed in cases where the LM initiative consisted of ad hoc efforts.16 Alternatively, we identified HCOs reporting a lack of frontline workforce involvement, particularly in cases where LM was approached as a structured initiative rather than an ad hoc approach.2,36,39,46,48 Hence, it seems that the more structured approach amounts to possible limited frontline worker involvement, and ad hoc approaches appear to limit manager input.
Leadership Style
In this stage, a notable proportion of HCOs reported that their leaders tended to adopt a hierarchical leadership style.2,16,36,39,45,49 This finding is consistent with the typical leadership characteristics we identified in this stage, as hierarchical leadership was highly uncommon in the Intermediate stage50,51 and absent in the Expert stage of maturity.
Focus and Vision
In most HCOs operating in the Beginner stage of maturity, LM is not perceived as a culture of CI.39,41–44,48,50 This contrasts with the other two stages, where leaders successfully fostered awareness of CI as a process of cultural development in 75% and 80% of the cases, respectively. Furthermore, leaders commonly emphasized using LM to achieve quick wins, indicating a short-term vision.36,43–46,52 Lastly, leaders commonly encountered difficulties involving multiple silos in LM activities44–46,48,52 and aligning LM initiatives with the organizational strategy.2,36,44–46
Learning
Just under half of the HCOs in the Beginner stage reported that their leaders use visual tools to enhance learning LM skills.16,36,43–45,47,52 Moreover, leaders utilized regular meetings as a mechanism for learning, where they could openly discuss problems.2,36,39,43,45,47,50 However, HCOs reported difficulty maintaining shared knowledge due to staff turnover.16,47
Training
It is typical for leaders to initially implement LM in a smaller portion of the organization rather than implementing it across multiple departments. In alignment with this observation, leaders in the Beginner stage frequently conducted LM training locally.16,39,44,45,48,52 Furthermore, certain HCOs reported that only a small proportion of their staff participated in these training initiatives.16,45
Collaboration
The main leadership activity associated with collaboration was focused on enhancing learning and facilitating discussions within teams, which was reported by 28% of HCOs. This finding contrasts with the Intermediate and Expert stage of maturity, where a greater percentage (75% and 60%, respectively) reported leaders actively promoting learning and fostering discussions within teams.
Deployment and Management
In the Beginner stage of LM maturity, several HCOs reported that employees perceive LM as an additional task or responsibility2,16,43,45–48 rather than an integrated way of working. This perception contradicts the principle of a CI culture, which emphasizes LM as an inherent part of the work process rather than an add-on. Furthermore, concerning the perceived skills of leaders in LM, some HCOs in this stage expressed concerns about inexperienced LM leaders.16
Facilitating Leadership
Several HCOs in this stage reported that leaders inadequately facilitated resources like time, money, or IT.16,43,49 This contrasts the other two stages, where HCOs did not report a lack of facilitating leadership in these areas.
Stage 2: Intermediate (n=12)
The Intermediate stage of LM maturity includes findings based on twelve HCOs categorized as maturity level 3. These HCOs exhibited leadership activities within a structured application of LM, as opposed to the absence or negative perception of leadership activities in the Beginner stage. While some similarities were observed with the Expert stage, the HCOs in the Intermediate stage displayed a lesser degree of development in terms of autonomous adherence to LM principles and shared responsibility in fostering a culture of CI. The following subsections comprehensively analyse the results obtained from HCOs in the Intermediate stage, distributed over the nine leadership themes.
Motivation, Engagement, Trust and Support
In the Intermediate stage, 25% of HCOs reported resistance,29 showing a notable contrast with 78% of HCOs in the Beginner stage. Further illustrating the contrast, HCOs in the Intermediate stage do not report on scepticism among the workforce and employees feeling jeopardized by LM. Regarding engagement, most HCOs reported active engagement of leaders in LM practices, including high-level management support.15,16,29,30,39,50,53,54 Lastly, leaders of HCOs in this stage commonly used previously achieved results to demonstrate LM’s ability to enhance staff commitment and participation in LM.15,29,30,50,51
Workforce Involvement
Half of the HCOs in this stage of maturity indicated that LM leaders could disseminate LM organization-wide29,39,50,54 rather than focusing on specific departments or involving staff locally in the HCO. Furthermore, half of the HCOs in this stage indicate that employees are offered freedom of choice in participating in LM,15,29,30,54 which is typical for the Intermediate stage of maturity.
Leadership Style
In the Intermediate stage of maturity, a small portion of HCOs reported leaders exhibiting a hierarchical leadership style.50,51 This is in contrast to the Beginner stage, where almost half of HCOs reported the presence of a hierarchical leadership style. Instead, this stage is characterized by a predominant bottom-up leadership approach, observed in two-thirds of the HCOs,15,29,30,39,50,54 and visible leadership, visible in one-third of the HCOs.15,29 Lastly, four HCOs reported employing a pull-based authority leadership style in this stage, where leaders empower staff to implement their ideas.29,30
Focus and Vision
Most HCOs in this stage reported that their leaders successfully created awareness of CI as a cultural development.15,29,30,50,53,54 Additionally, leaders in two-thirds of the HCOs aligned the implementation of LM with the organization’s strategy.29,30,50,53,54 Regarding integration through LM, a significant proportion of leaders in this stage aimed to achieve cross-sectional alignment with LM activities29,39,50,53,54 and involve multiple silos during LM activities.15,30,50,54 However, in contrast to the Expert stage, HCOs in the Intermediate stage did not report a shared responsibility for LM outcomes and developing a culture of CI.
Learning
Leaders of half of the HCOs operating in the Intermediate stage reported utilizing visual learning methods and conducting regular meetings to discuss problems,29,50,53 slightly more than in the Beginner stage. Moreover, a notable distinction from the first stage is that leaders in most HCOs in the Intermediate stage focused on enhancing the autonomous problem-solving abilities of staff,15,16,29,30,39,50,53,54 a result similar to the Expert stage.
Training
In this stage, half of the HCOs reported that their leaders implemented LM training throughout the entire organization,15,29,30,53 contrasting with the local deployment observed in the Beginner stage. Moreover, leaders in 25% of the HCOs customized learning programs to align with current projects, enhancing the relevance of the training.29 This tailored approach was not observed in the Beginner stage and was found in 40% of the HCOs in the Expert stage, indicating that this practice evolves with the maturity of CI.
Collaboration
In the Intermediate stage, leaders of most HCOs have actively enhanced learning and fostered discussions within teams,15,29,30,50,52,54 indicating a higher prevalence compared to the Beginner stage. Additionally, it is common in this stage for leaders to involve clinical management and appoint mid-level/frontline leaders as project leaders.15,29,30,39,50,51,53 Furthermore, approximately half of HCOs reported successfully establishing clear roles within their teams15,29,30,39,51 and achieving shared agreement on project goals.29,51,54
Deployment and Management
While half of the HCOs in stages 1 and 2 reported struggling to establish LM as a culture, leaders in most HCOs operating in the Intermediate stage successfully achieved standardization in managing their LM initiative.29,30,50,51,53 Most of the HCOs in this stage also employed a full-time LM specialist.29,30,50,51 Lastly, a few HCOs reported on managerial consistency, indicating reliable management throughout the implementation of the LM initiative over time.29,50
Facilitating Leadership
While HCOs in the Beginner stage reported insufficient resource facilitation by leaders during LM activities, no HCO in the Intermediate stage reported this. Forty-two percent of HCOs reported the presence of sufficient resource facilitation.
Stage 3: Expert (n=5)
This section presents the findings related to the Expert stage of maturity, comprising five HCOs initially classified at CI maturity levels 4 or 5. These HCOs were distinguished by implementing an organization-wide, structured LM initiative aligned with the HCO strategy. Notably, the Expert stage differed from the Intermediate stage regarding higher levels of autonomous utilization of LM principles, shared responsibility in cultivating a culture of CI, and the overall presence of a CI culture. The subsequent subsections provide a detailed exploration of the results obtained from HCOs in this stage, focusing on the nine leadership themes.
Motivation, Engagement, Trust and Support
In the Expert stage of maturity, all HCOs emphasized leaders’ active engagement of the entire workforce,16,55–58 demonstrating a higher level of dedication towards workforce engagement compared to the Intermediate stage. Additionally, HCOs in this stage displayed visible engagement by higher management and using the achieved results of LM to enhance staff engagement,16,55,56,58 which was more prevalent than in the Intermediate stage.
Workforce Involvement
In this stage, a notable portion of HCOs reported on leaders infusing LM throughout the organization55–57 and granting employees the freedom to participate in LM practices.16,58 These observations align with the findings in the Intermediate stage. However, HCOs in the Expert stage emphasized the inclusion of all relevant stakeholders in LM initiatives,55–57 setting the Expert stage apart from the Intermediate stage.
Leadership Style
In contrast to the Begin and Intermediate stages of maturity, the Expert stage is characterized by the consistent presence of visible leadership (Gemba) in all HCOs.16,55–58 Leaders in this stage actively engage in practices by being physically present in the workplace, demonstrating their commitment and involvement. Additionally, a subset of HCOs in the Expert stage reported on leaders displaying a hands-on management leadership style.16,56 This style is characterized by leaders actively participating in daily LM practices, reinforcing their dedication to driving CI.
Focus and Vision
The majority of HCOs operating in this stage reported on leaders deploying LM in alignment with the organization’s strategy,16,55,56,58 creating awareness of CI as cultural development16,55–57 and focusing on cross-sectional alignment through performing LM practices.55–58 These percentages are slightly higher than in the Intermediate stage. Furthermore, what distinguishes the Expert stage from the Intermediate stage is that leaders were found to create shared responsibility for LM outcomes and the development of CI.55–57
Learning
Concerning this theme, leaders of almost all HCOs in the Expert stage were found to enhance the autonomous problem-solving abilities of staff,16,55,56,58 comparable with the Intermediate stage. However, leaders in this stage enhanced staff experimenting during LM practices,55,57,58 distinguishing the Expert stage from the Intermediate stage.
Training
A notable portion of HCOs in the Expert stage were found to deploy training in LM and LM tools organization-wide16,55,56 and tailor learning programs to ongoing projects.16,57 This portion is slightly higher than in the Intermediate stage.
Collaboration
Regarding collaboration, leaders in HCOs operating in the Expert stage of maturity displayed a comprehensive approach, as all leaders were found to involve clinical management and appoint mid-level and frontline leaders as project leaders in LM projects.16,55–58 Additionally, most HCOs reported that leaders successfully established clear roles within teams.55–58 These portions reflect a notable increase of around 20% compared to the Intermediate stage. Another distinguishing feature of the Expert stage is the active involvement of stakeholders throughout the entire process to secure commitment to proposed changes,16,55,57,58 ensuring that stakeholders are more likely to commit to the solutions presented later in the project.
Deployment and Management
Most of the ones operating in the Expert maturity stage reported on the employment of a full-time LM specialist16,55,58 and the management of the LM initiative being standardized,16,55,56 which is comparable with the Intermediate stage. However, all HCOs in the Expert stage reported on managerial consistency throughout the implementation and adoption process of LM (50, 5, which was only 33% in the Intermediate stage.
Facilitating Leadership
Concerning facilitating resources within the LM initiative, 40% of HCOs operating in the Expert stage report on sufficient resource facilitation.16,56 This degree of resource facilitation is comparable to that of the Intermediate stage. However, what distinguishes the Expert stage is that HCOs also reported on leaders facilitating the minimization of disruptions to the staff’s clinical work,57).
Ultimately, the three stages of LM maturity show differences in activities. Based on these findings, we provide a framework that shows leadership activities that LM leaders in practice can adopt to increase LM maturity, and the framework is depicted in Figure 3. The leadership activities titled “Begin to Intermediate” typify HCOs in the Intermediate stage of maturity, which leaders in the Beginner stage can adopt. Alternatively, leaders of HCOs in the intermediate stage of maturity can adopt activities under the title “Intermediate to Expert” to facilitate their process towards the Expert stage.
 |
Figure 3 Lean Maturity Framework. |
Most leadership activities in the middle column are also present in the Expert stage of maturity. However, leadership activities in the right column are activities found to be common only in the Expert stage of maturity, thus distinguishing activities in the Expert stage from the Intermediate stage. Therefore, on top of evaluating or adopting the activities in the right column, leaders in the Intermediate stage can also consider the activities in the column Beginner to Intermediate to facilitate their maturity process towards the Expert stage.
Discussion
This literature review aimed to identify and analyse the activities of LM leadership in relation to LM maturity. In our analysis, we used 23 articles representing 34 unique cases of LM usage, in which 58 leadership activities and nine themes of LM leadership were identified. Furthermore, three stages of maturity were identified within the results: Beginner, Intermediate, and Expert. Leadership activities that strongly influence LM’s maturity are the adopted leadership style(s), the degree of workforce involvement in LM activities, the extent to which the workforce is promoted to engage in LM throughout the organization, and the ability to enhance autonomous problem-solving abilities.
After identifying and aggregating 58 leadership activities, nine themes of LM leadership emerged, depicted in Table 6. Our overview extends the previous study by Dombrowski & Mielke,59 which identified five leadership principles. The nine themes cover these earlier identified leadership principles and extend these ideas. In addition, we add to our understanding of leadership as previous literature on LM leadership23,26,59 tends to focus on leaders’ qualities and behavioural traits (eg, autonomy and honesty). In our study, we report on the activities of leaders (eg, tailoring training to ongoing projects and enhancing experimenting).
Consequently, as opposed to previous literature, this review depicts the activities of LM leaders rather than the qualities and behavioural traits of leaders. Our findings relate to earlier reviews that focus on leadership activities,60,61 illustrating similarities and extending earlier work. Our research agrees with earlier findings, previous work that found hierarchical leadership, scepticism62,63 and inadequate resource facilitation17 act as barriers to LM implementation in healthcare, and we identify similar activities solely in the Beginner stage. In turn, this implies that as LM maturity grows, these behaviours become obsolete.
The results concerning the occurrence of leadership activities among the five levels of LM showed similarities, resulting in the proposition of three stages of LM maturity. This is in accordance with a revised model of CI maturity, which also consists of three stages.14 The main leadership activities that impede or facilitate CI maturity the most are adopted leadership styles, the extent of stakeholder involvement, resource facilitation, and the extent to which the responsibility of creating a CI culture is shared. Previous literature found that leaders adopting a hierarchical leadership style impede LM implementation.62,63 In addition, previous studies acknowledged visible leadership as a facilitator in LM implementation,63,64 which aligns with our findings. Furthermore, findings of relevant clinical stakeholder involvement, resource facilitation by leaders, and the extent of sharing responsibility to create a culture of CI agree with the results of our study.26,62,65,66
Overall, our research adds to our knowledge of LM and is a timely addition to the existing literature base. Recent review studies highlighted the roles of LM practices in improving care quality,67 the effects on patient flow and efficiency outcomes,68 and overall lean implementations in healthcare.7 Here, our study adds a human-centred perspective with special attention towards the role of leadership and the maturity (or development) of a lean approach. Our study fits with the existing work of Tortorella, van Dun, and de Almeida,61 which focuses on leadership behaviours during implementation. We extend this line of research by focusing on both the implementation of LM principles and the later stage of LM maturity. In addition, our study is aligned with the work of Kunnen, Roemeling and Smailhodzic,69 which focuses on barriers and facilitators for sustaining LM practices. The authors acknowledge the importance of leadership. Here, we can extend the notion of importance and, more specifically, address actual leadership activities relevant to LM’s sustainment (maturity). Based on the findings of this review, the following three propositions are formulated:
Proposition 1
Leaders of HCOs operating in the Beginner stage of maturity will show leadership activities typified by a hierarchical leadership approach, lack of involving relevant stakeholders, lack of initiatives to overcome resistance, scepticism and fear, insufficient resource facilitation, deploying LM as a temporary program instead of a culture, and misaligning LM with the strategy.
Proposition 2
Leaders of HCOs operating in the Intermediate stage of maturity will show leadership activities typified by a bottom-up leadership approach, increasing organization-wide participation and commitment and showing gained results to achieve this, involving relevant clinical stakeholders and enhancing employees’ autonomy in problem-solving and creating a culture of CI.
Proposition 3
Leaders of HCOs operating in the Expert stage of maturity will show leadership activities typified by a visible leadership and/or a hands-on leadership approach, engaging the entire workforce, including relevant clinical stakeholders, to gain commitment for proposed changes, creating visible management engagement, aligning LM with the organizational strategy, enhancing the autonomy of staff and creating a system of shared responsibility to achieve a culture of CI.
Theoretical Implications
This study identified LM leadership activities in relation to LM maturity. Though previous literature reviews have been conducted on LM leadership attributes26 and the effects of leadership styles,24 no literature review has focused on the relation between the activities of LM leadership and maturity. The overview of the leadership activities concerning maturity, the provided framework, and the propositions form the theoretical contribution of this research. First, the overview of common leadership activities per stage of maturity and the emerging themes can be used to structure thinking in future research. Furthermore, it provides a starting point for studies to relate leadership to LM maturity. Lastly, this research contributes to the literature by offering a framework which offers practical leadership activities that leaders of HCOs can adopt to improve the maturity of their LM initiative.
Furthermore, HCOs planning to deploy LM can consult the framework to structure the implementation of LM prospectively. Lastly, Dombrowski & Mielke59 state that the self-development of LM leaders demands new leadership skills and that, by using these skills, leaders should behave as role models. To achieve the self-development of leaders regarding LM leadership, leaders can evaluate their role by consulting the proposed framework and the suitable leadership activities across the stages of maturity.
Managerial Implications
Our findings have profound managerial implications. First, as indicated by proposition 1, the early stages of LM implementation are characterized not only by the immaturity of the LM culture and mindset but also by the immaturity of its LM leadership. Managers aiming to implement and mature LM in their organizations are therefore advised to bring in or appoint experienced LM leaders perceived as legitimate and trustworthy by affected staff members and capable of fostering bottom-up ownership and initiative while ensuring top-management support and alignment. Failing to do so is likely to cut the LM implementation process short, as our findings highlight the indispensable nature of these specific leadership activities at this stage. Second, the leadership activities that benefit LM implementation in Stage 2 highlight the importance of defusing and reinforcing a CI culture throughout the organization. Our findings indicate that bottom-up leadership activities aiming to create organisational commitment and support are key to this stage. Managers are advised to reserve resources for leadership activities at this stage. The bottom-up cultural change processes tend to involve numerous people throughout the organization and are typically time-consuming. Finally, to stimulate the leadership activities found to contribute to LM implementation at Stage 3 and sustain CI maturity, managers are advised to ensure institutionalization of these lean leadership activities, eg, through evaluation and reward systems.
Limitations
There are several limitations to this study. The results of this review are based on case studies that reported on their LM initiative. Whilst various leadership activities are found, not all leadership activities present in practice may be identified because the studies did not specifically aim to report on leadership activities. In addition, a large proportion of HCOs included in this study consists of hospitals. This might limit generalizability to other healthcare institutions. Furthermore, as only organizations in the healthcare context were included, the results may not hold in other contexts, albeit that extending our study focus beyond healthcare was not our objective. The results of the current study could be extended by broadening this set of journals to include a wider set of (clinical) health-related journals, operations management journals, and/or academic databases. More than half of the HCOs were found to be in the UK or US, which could influence the findings as healthcare systems differ between countries. Though we were able to provide insight into the current state of LM maturity, it appears as if few HCOs are in the Expert stage of maturity, a certain bias in published works could have a role here. Finally, the coding process was performed independently. Whilst collaborative coding can induce coding variance, joint code interpretation and grouping these into leadership themes could have strengthened the process.
Directions for Future Research
Future research directions include testing whether the proposed framework’s leadership activities contribute to improving LM’s maturity in practice through quantitative or action research. Furthermore, future research could expand the proposed framework to HCOs other than hospitals. Lastly, as few studies in this review reported on HCOs achieving a high level of LM maturity, future research could expand the literature on leadership activities being common in HCOs that operate at high maturity levels, as few HCOs in this study reported on high LM maturity.
Conclusions
In this study, we were interested in leadership activities and how these activities played a role in achieving LM maturity. Through a scoping review based on high-quality healthcare management journals, we identified 23 relevant studies covering 34 HCOs. Our in-depth analysis uncovered nine themes of LM leadership, and we identified three stages of LM maturity. The results of our study provide an extensive overview of LM activities across the nine leadership themes, which in turn are linked to the three identified stages of maturity. The results show that leadership activities differ across stages of LM maturity, thus illustrating a relation between leadership activities and LM maturity. The focus on leadership activities in various stages of maturity adds to our current understanding and builds upon previous research focused on the implementation and sustainment of LM. Our study furthers the thinking on LM by offering a framework with related propositions. Healthcare leaders can consult the framework to facilitate their LM initiatives. In addition, the propositions provide future studies with testable ideas to further develop. This study mainly contributes to the literature by addressing LM maturity, extending existing research lines on LM leadership, and offering a clear framework for practice and academia. Ultimately, leaders of HCOs should reconsider their leadership style, determine which (clinical) stakeholders are relevant to involve in LM practices, how to align LM with the organizational strategy, and how to create shared responsibility for achieving a culture of CI; these steps should improve the maturity of LM initiatives and in addition to that organizational performance.
Abbreviations
LM, Lean Management; HCO(s), Healthcare Organization(s); CI, Continuous Improvement.
Data Sharing Statement
The datasets used in this review are available from the corresponding author upon reasonable request.
Funding
The authors did not receive funding for this study.
Disclosure
The authors declare no competing interests in this work.
References
1. Hanft K. Lean hospitals: improving quality, patient safety, and employee engagement 2nd edition. HERD. 2013;7(1):124–125. doi:10.1177/193758671300700111
2. Waring JJ, Bishop S. Lean healthcare: rhetoric, ritual and resistance. Soc Sci Med. 2010;71(7):1332–1340. doi:10.1016/j.socscimed.2010.06.028
3. van den Heuvel J. The effectiveness of ISO 9001 and six sigma in healthcare; 2007. Available from: https://repub.eur.nl/pub/8465/.
4. Chan H, Lo S, Lee L, et al. Lean techniques for the improvement of patients’ flow in the emergency department. World J Emerg Med. 2014;5(1):24–28. doi:10.5847/wjem.j.issn.1920-8642.2014.01.004
5. Ciulla J, Knights D, Mabey C, Tomkins L. Guest editors’ introduction: philosophical contributions to leadership ethics. Bus Ethics Q. 2018;28:1–14. doi:10.1017/beq.2017.48
6. Mahmoud Z, Angelé-Halgand N, Churruca K, Ellis L, Braithwaite J. The impact of lean management on frontline healthcare professionals: a scoping review of the literature. BMC Health Serv Res. 2021;21. doi:10.1186/s12913-021-06344-0
7. Akmal A, Greatbanks R, Foote J. Lean thinking in healthcare - Findings from a systematic literature network and bibliometric analysis. Health Policy Amst Neth. 2020;124(6):615–627. doi:10.1016/j.healthpol.2020.04.008
8. Tsasis P, Bruce-Barrett C. Organizational change through lean thinking. Health Serv Manage Res. 2008;21(3):192–198. doi:10.1258/hsmr.2007.007023
9. Morduchowicz S, Lee JS, Choi L, et al. Utilizing lean leadership principles to build an academic primary care practice of the future. J Gen Intern Med. 2020;35(12):3650–3655. doi:10.1007/s11606-020-06246-7
10. Womack JP, Jones DT, Roos D. Citation: the machine that changed the world - BibGuru guides. Bibguru; 2004. Available from: https://www.bibguru.com/b/how-to-cite-The-machine-that-changed-The-world/.
11. Reponen E, Jokela R, Blodgett JC, et al. Validation of the Lean Healthcare Implementation Self-Assessment Instrument (LHISI) in the Finnish healthcare context. BMC Health Serv Res. 2021;21(1):1289. doi:10.1186/s12913-021-07322-2
12. Liker JK. The Toyota Way, 14 Management Principles from the World’s Greatest Manufacturer. New York: McGraw-Hill; 2004.
13. Bessant J, Caffyn S, Gallagher M. An evolutionary model of continuous improvement behaviour. Technovation. 2001;21(2):67–77. doi:10.1016/S0166-4972(00)00023-7
14. Fryer K, Ogden S, Antony J. Bessant’s continuous improvement model: revisiting and revising. Int J Public Sect Manag. 2013;26:481–494. doi:10.1108/IJPSM-05-2012-0052
15. Radcliffe E, Kordowicz M, Mak C, et al. Lean implementation within healthcare: imaging as fertile ground. J Health Organ Manag. 2020;34(8):869–884. doi:10.1108/JHOM-02-2020-0050
16. Harrison MI, Paez K, Carman KL, et al. Effects of organizational context on lean implementation in five hospital systems. Health Care Manage Rev. 2016;41(2):127–144. doi:10.1097/HMR.0000000000000049
17. Rundall TG, Shortell SM, Blodgett JC, Henke RM, Foster D. Adoption of lean management and hospital performance: results from a national survey. Health Care Manage Rev. 2021;46(1):E10–9. doi:10.1097/HMR.0000000000000287
18. Santos AC, De SG, Reis A, Souza CG, Santos IL, Ferreira LAF. The first evidence about conceptual vs analytical lean healthcare research studies. J Health Organ Manag. 2020;34(7):789–806. doi:10.1108/JHOM-01-2020-0021
19. Aij KH, Aernoudts RLMC, Joosten G. Manager traits and quality-of-care performance in hospitals. Leadersh Health Serv Bradf Engl. 2015;28(3):200–215. doi:10.1108/LHS-07-2014-0053
20. Al-Balushi S, Sohal AS, Singh PJ, Al Hajri A, Al Farsi YM, Al Abri R. Readiness factors for lean implementation in healthcare settings--A literature review. J Health Organ Manag. 2014;28(2):135–153. doi:10.1108/JHOM-04-2013-0083
21. Dombrowski U, Mielke T. Lean leadership – 15 rules for a sustainable lean implementation. Procedia CIRP. 2014;17:565–570. doi:10.1016/j.procir.2014.01.146
22. Ghosh M, Sobek Ii DK. A problem-solving routine for improving hospital operations. J Health Organ Manag. 2015;29(2):252–270. doi:10.1108/JHOM-09-2013-0191
23. Aij KH, Visse M, Widdershoven GAM. Lean leadership: an ethnographic study. Leadersh Health Serv Bradf Engl. 2015;28(2):119–134. doi:10.1108/LHS-03-2014-0015
24. Aij KH, Rapsaniotis S. Leadership requirements for Lean versus servant leadership in health care: a systematic review of the literature. J Healthc Leadersh. 2017;9:1–14. doi:10.2147/JHL.S120166
25. van Elp B, Roemeling O, Aij KH. Lean leadership: towards continuous improvement capability in healthcare. Health Serv Manage Res. 2022;35(1):7–15. doi:10.1177/09514848211001688
26. Aij KH, Teunissen M. Lean leadership attributes: a systematic review of the literature. J Health Organ Manag. 2017;31(7–8):713–729. doi:10.1108/JHOM-12-2016-0245
27. Kaltenbrunner M, Mathiassen S, Bengtsson L, Engström M. Lean maturity and quality in primary care. J Health Organ Manag. 2019;33:141–154. doi:10.1108/JHOM-04-2018-0118
28. Knol WH, Slomp J, Schouteten RLJ, Lauche K. The relative importance of improvement routines for implementing lean practices. Int J Oper Prod Manag. 2018;39(2):214–237. doi:10.1108/IJOPM-01-2018-0010
29. Régis TKO, Santos LC, Gohr CF. A case-based methodology for lean implementation in hospital operations. J Health Organ Manag. 2019;33(6):656–676. doi:10.1108/JHOM-09-2018-0267
30. Schouten H, Heusinkveld S, van der Kam W, Benders J. Implementing lean-led hospital design; lessons gained at a pioneer. J Health Organ Manag. 2020;35:1–16. doi:10.1108/JHOM-08-2019-0250
31. Okoli C, Schabram K. A guide to conducting a systematic literature review of information systems research. SSRN Electron J. 2010;10:1.
32. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi:10.1136/bmj.n71
33. Meese KA, O’Connor SJ, Borkowski N, Hernandez SR. Journal rankings and directions for future research in health care management: a global perspective. Health Serv Manage Res. 2017;30(2):129–137. doi:10.1177/0951484817696213
34. Delgado-Rodríguez M, Llorca J. Bias. J Epidemiol Community Health. 2004;58(8):635–641. doi:10.1136/jech.2003.008466
35. Rasmussen L, Montgomery P. The prevalence of and factors associated with inclusion of non-English language studies in Campbell systematic reviews: a survey and meta-epidemiological study. Syst Rev. 2018;7(1):129. doi:10.1186/s13643-018-0786-6
36. Mazzocato P, Thor J, Bäckman U, et al. Complexity complicates lean: lessons from seven emergency services. J Health Organ Manag. 2014;28(2):266–288. doi:10.1108/JHOM-03-2013-0060
37. D’Andreamatteo A, Ianni L, Lega F, Sargiacomo M. Lean in healthcare: a comprehensive review. Health Policy Amst Neth. 2015;119(9):1197–1209. doi:10.1016/j.healthpol.2015.02.002
38. Winner LE, Reinhardt E, Benishek L, Marsteller JA. Lean Management Systems in Health Care: a Review of the Literature. Qual Manag Health Care. 2022;31(4):221–230. doi:10.1097/QMH.0000000000000353
39. Hung D, Gray C, Martinez M, Schmittdiel J, Harrison MI. Acceptance of lean redesigns in primary care: a contextual analysis. Health Care Manage Rev. 2017;42(3):203–212. doi:10.1097/HMR.0000000000000106
40. Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Transaction Publishers; 2009:283.
41. Millar R. Framing quality improvement tools and techniques in healthcare: the case of improvement leaders guides. J Health Organ Manag. 2013;27(2):209–224. doi:10.1108/14777261311321789
42. Terra JDR, Berssaneti FT. Application of lean healthcare in hospital services: a review of the literature (2007 to 2017). Production. 2018;28(1). doi:10.1590/0103-6513.20180009
43. McCann L, Hassard JS, Granter E, Hyde PJ. Casting the lean spell: the promotion, dilution and erosion of lean management in the NHS. Hum Relat. 2015;68(10):1557–1577. doi:10.1177/0018726714561697
44. McDermott AM, Kidd P, Gately M, et al. Restructuring of the diabetes day centre: a pilot lean project in a tertiary referral centre in the West of Ireland. BMJ Qual Saf. 2013;22(8):681–688. doi:10.1136/bmjqs-2012-001676
45. Hasle P, Starheim L, Jensen PL, Diekmann BJ. Value stream mapping as a tool for systematic employee based improvement of the psychosocial work environment in hospitals. Acad Manag Proc. 2017;2017:1.
46. Radnor ZJ, Holweg M, Waring J. Lean in healthcare: the unfilled promise? Soc Sci Med. 2012;74(3):364–371. doi:10.1016/j.socscimed.2011.02.011
47. Ulhassan W, Westerlund H, Thor J, Sandahl C, von Thiele Schwarz U. Does lean implementation interact with group functioning? J Health Organ Manag. 2014;28(2):196–213. doi:10.1108/JHOM-03-2013-0065
48. Taylor S, McSherry R, Cook S, Giles E. Exploring the emotional experience of lean. J Health Organ Manag. 2020;35(1):34–52. doi:10.1108/JHOM-01-2020-0002
49. Timmons S, Coffey F, Vezyridis P. Implementing lean methods in the emergency department: the role of professions and professional status. J Health Organ Manag. 2014;28(2):214–228. doi:10.1108/JHOM-10-2012-0203
50. Marchand JS, Breton M, Saulpic O, Côté-Boileau É. Lessons from mandated implementation of a performance management system. J Health Organ Manag. 2021;35:579–595. doi:10.1108/JHOM-08-2020-0352
51. Valsangkar NP, Eppstein AC, Lawson RA, Taylor AN. Effect of lean processes on surgical wait times and efficiency in a tertiary care veterans affairs medical center. JAMA Surg. 2017;152(1):42–47. doi:10.1001/jamasurg.2016.2808
52. Grove AL, Meredith JO, Macintyre M, Angelis J, Neailey K. Lean implementation in primary care health visiting services in national health service UK. Qual Saf Health Care. 2010;19(5):e43–e43. doi:10.1136/qshc.2009.039719
53. Drei S, Ignacio P. Lean healthcare applied systematically in a medium-sized medical clinic hospitalization. J Health Organ Manag. 2022;2022:1.
54. van Rossum L, Aij KH, Simons FE, van der Eng N, ten Have WD. Lean healthcare from a change management perspective: the role of leadership and workforce flexibility in an operating theatre. J Health Organ Manag. 2016;30(3):475–493. doi:10.1108/JHOM-06-2014-0090
55. Erthal A, Marques L, Marques L. Cultural tensions in lean healthcare implementation: a paradox theory lens. Acad Manag Proc. 2019;2019(1):17988. doi:10.5465/AMBPP.2019.17988abstract
56. Armstrong S, Fox E, Chapman W. To meet health care’s triple AIM, lean management must be applied across the value stream: comment on “management practices and the quality of care in cardiac units. JAMA Intern Med. 2013;173(8):692–694. doi:10.1001/jamainternmed.2013.4080
57. Ibrahim A, Ndeti K, Bur A, et al. Association of a lean surgical plan of the day with reduced operating room time for head and neck free flap reconstruction. JAMA Otolaryngol Neck Surg. 2019;145(10):926–930. doi:10.1001/jamaoto.2019.2250
58. Hayes J, Reed K, Fitzgerald N, Watt A. Applying lean flows in pathology laboratory remodelling. J Health Organ Manag. 2014;28(2):229–246. doi:10.1108/JHOM-03-2013-0064
59. Dombrowski U, Mielke T. Lean leadership – fundamental principles and their application. Procedia CIRP. 2013;7:569–574. doi:10.1016/j.procir.2013.06.034
60. Maijala R, Eloranta S, Reunanen T, Ikonen TS. Successful implementation of lean as a managerial principle in health care: a conceptual analysis from systematic literature review. Int J Technol Assess Health Care. 2018;34(2):134–146. doi:10.1017/S0266462318000193
61. Tortorella G, van Dun DH, de Almeida AG. Leadership behaviors during lean healthcare implementation: a review and longitudinal study. J Manuf Technol Manag. 2019;31(1):193–215. doi:10.1108/JMTM-02-2019-0070
62. de Souza LB, Pidd M. Exploring the barriers to lean health care implementation. Public Money Manag. 2011;31(1):59–66. doi:10.1080/09540962.2011.545548
63. Mohd Daril MA, Nuraina S, Subari K. The barriers in lean healthcare implementation. Test Eng Manag. 2020;82:1972–1981.
64. Bourgault AM, Upvall MJ, Graham A. Using gemba boards to facilitate evidence-based practice in critical care. Crit Care Nurse. 2018;38(3):e1–7. doi:10.4037/ccn2018714
65. Aij KH, Simons FE, Widdershoven GAM, Visse M. Experiences of leaders in the implementation of lean in a teaching hospital—barriers and facilitators in clinical practices: a qualitative study. BMJ Open. 2013;3(10):e003605. doi:10.1136/bmjopen-2013-003605
66. Melo C, Berssaneti F, Rampini G, Martinez I. Exploring barriers and facilitators to lean implementation in healthcare organizations.
67. Rooslanda E, Ayuningtyas D. Implementation of lean management in improving the quality of hospital services: literature review. J Int Soc Res. 2023;2(8):2488–2496.
68. Zepeda-Lugo C, Tlapa D, Baez-Lopez Y, et al. Assessing the impact of lean healthcare on inpatient care: a systematic review. NT J Env Res Pub Health. 2020;17(15):5609. doi:10.3390/ijerph17155609
69. Kunnen YS, Roemeling OP, Smailhodzic E. What are barriers and facilitators in sustaining lean management in healthcare? A qualitative literature review. BMC Health Serv Res. 2023;23(1):1–13. doi:10.1186/s12913-023-09978-4
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
