Back to Journals » Infection and Drug Resistance » Volume 17
Trends of Drug-Resistant Tuberculosis in an Urban and a Rural Area in China: A 10-Year Population-Based Molecular Epidemiological Study
Authors Xu P, Li M, Jiang Q , Yang C , Liu X, Takiff H, Gao Q
Received 15 September 2023
Accepted for publication 23 February 2024
Published 8 March 2024 Volume 2024:17 Pages 919—926
DOI https://doi.org/10.2147/IDR.S436563
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Zhi Ruan
Peng Xu,1 Meng Li,1,2 Qi Jiang,3 Chongguang Yang,4 Xiangxiang Liu,1 Howard Takiff,5 Qian Gao1,2
1National Clinical Research Center for Infectious Diseases, Shenzhen Clinical Research Center for Tuberculosis, Shenzhen Third People’s Hospital, Shenzhen, Guangdong, People’s Republic of China; 2Key Laboratory of Medical Molecular Virology (MOE/NHC/CAMS), School of Basic Medical Science, Shanghai Medical College, Shanghai Institute of Infectious Disease and Biosecurity, Fudan University, Shanghai, People’s Republic of China; 3Department of Epidemiology and Biostatistics, School of Public Health, Wuhan University, Wuhan, People’s Republic of China; 4School of Public Health (Shenzhen), Shenzhen Campus of Sun Yat-Sen University, Shenzhen, People’s Republic of China; 5Laboratorio de Genética Molecular, CMBC, IVIC, Caracas, Venezuela
Correspondence: Qian Gao, National Clinical Research Center for Infectious Diseases, Shenzhen Clinical Research Center for Tuberculosis, Shenzhen Third People’s Hospital, No. 29 Bulan Road, Longgang District, Shenzhen, Guangdong, People’s Republic of China, Tel +86-21-5423-7195, Fax +86-21-5423-7971, Email [email protected]
Objective: Drug resistance is the critical determinant for appropriate tuberculosis (TB) treatment regimens and an important indicator of the local TB burden. We aimed to investigate and compare trends in TB drug resistance in the urban Songjiang District of Shanghai from 2011 to 2020, and the rural Wusheng County of Sichuan Province from 2009 to 2020, to assess the effectiveness of local TB control and treatment programs.
Methods: Whole-genome sequencing data of Mycobacterium tuberculosis were used to predict drug-resistance profiles and identify genomic clusters. Clustered, retreated cases of drug-resistant TB with identical resistance mutations, as well as all new resistant cases, were defined as transmitted resistance. The Cochran-Armitage trend test was used to identify trends in the proportions. Differences between groups were tested using the Wilcoxon rank sum or chi-square tests.
Results: The annual proportions of rifampicin-resistant (RR), isoniazid-resistant (INH-R) and multidrug-resistant (MDR) TB cases did not change significantly in Songjiang. In Wusheng, however, the percentage of total TB cases that were RR decreased from 13.2% in 2009 to 3.7% in 2020, the INH-R cases decreased from 16.5% to 7.3%, and the MDR cases decreased from 10.7% to 3.7%. In retreated cases, the percentage of drug resistance decreased in both Songjiang and Wusheng, suggesting improved treatment programs. Transmitted resistance accounted for more than two thirds of drug-resistant cases over the entire study periods, and in recent years this proportion has increased significantly in Songjiang.
Conclusion: In both urban Songjiang and rural Wusheng, drug-resistant TB is mostly the result of transmission of drug resistant strains and the percentage of transmitted resistance will likely increase with on-going improvements in the TB treatment programs. Reducing the prevalence of drug resistance depends principally upon decreasing transmission through the prompt diagnosis and effective treatment of drug-resistant TB cases.
Keywords: tuberculosis, trends of drug resistance, whole-genome sequencing, urban and rural China
Introduction
Tuberculosis (TB), an infectious disease caused by Mycobacterium tuberculosis (M. tuberculosis), is a major problem in global public health. As the COVID-19 pandemic subsides, TB is again the leading cause of death from a single infectious agent, surpassing even HIV/AIDS and malaria.1 Drug-resistance, especially multidrug-resistance (MDR) is an important risk factor for TB treatment failure and death.2–4 Among global MDR/RR-TB cases that began treatment in 2019, the success rate was only 60%.1 China is one of the countries with the highest TB burdens. In 2021, China had about 780,000 new TB cases and 33,000 MDR/RR-TB cases, both exceeding 7% of the global totals for these categories.
The World Health Organization (WHO) recommends that countries monitor local trends in drug-resistant TB because the percentage of TB cases that are drug-resistant TB is an important indicator of both the local TB burden and the quality of the local TB control program. As early as 1994, WHO and the International Union Against Tuberculosis and Lung Disease (IUATLD) launched a global drug-resistance surveillance project to monitor drug-resistant TB,5 and several countries have subsequently published data from national surveys of drug-resistant TB.6–10 In 2007, China conducted a national sampling survey on the prevalence of resistance to the four first-line anti-TB drugs (rifampicin, isoniazid, ethambutol and streptomycin) and two second-line drugs (ofloxacin and kanamycin).11 Since this survey, China has made a concerted effort to improve the control of drug-resistant TB. Although the trends in the prevalence of drug-resistant TB have been evaluated in several individual regions of China, including Beijing, Zhejiang, Henan, and Guizhou,12–17 most of these studies were based on hospitalized TB patients and therefore the reported prevalence of drug resistance may have been higher than would be found in population-based studies.
Molecular Drug Susceptibility Testing (DST) is less affected by laboratory quality than phenotypic testing, and therefore more suitable for long-term monitoring and comparisons of TB drug resistance in different regions. Whole-genome sequencing (WGS) based molecular DST has been widely used in epidemiologic studies18–20 because it provides nearly complete genomic information and can predict the susceptibility to all anti-TB drugs.21,22 We previously established population-based epidemiological study sites in Songjiang District, an urban area in Shanghai, and Wusheng County, a rural area in Sichuan Province, and obtained WGS data from the clinical M. tuberculosis strains isolated in both sites over periods of at least 10 years.23,24 Here, we report our analysis of this WGS data to identify trends in TB drug resistance in both Songjiang and Wusheng.
Materials and Methods
Patients and WGS Data
All patient information and WGS data on clinical strains analyzed in this study were obtained from previous population-based studies conducted in the urban Songjiang District of Shanghai (population 1.9 million in the 2020 census) and in the rural Wusheng County of Sichuan Province (population 0.55 million).23,25 There were 2225 pulmonary TB cases diagnosed in Songjiang from 2011 to 2020, and 1333 pulmonary TB cases diagnosed in Wusheng from 2009 to 2020.
Analysis of WGS Data
A previously validated pipeline was used to identify single nucleotide polymorphisms (SNPs) based on the WGS data.26 Briefly, WGS fastq files were trimmed using the Sickle tool and sequencing reads with Phred base quality greater than 20 and reads length longer than 35 were mapped to the reference genome (H37Rv, NC000962.3) using Bowtie 2 (v2.2.9).27 The SAMtools (v1.6)/VarScan (v2.3.6)28,29 suite was used for SNP calling with mapping quality greater than 30. Repetitive regions of the genome, including the proline-glutamic acid (PE) and proline-proline-glutamic acid/polymorphic guanine-cytosine-rich sequence (PPE-PGRS) family genes, phage sequences, insertions, and mobile genetic elements were excluded from the SNP analysis. SNPs with a frequency ≥10% were used to predict the drug-resistance profiles with SAM-TB.30 The genomic clusters were identified in a previous study.25 Pairwise SNP distances were calculated based on the fixed SNPs with a frequency ≥75%, and strains within a threshold distance of twelve or fewer SNPs were defined as genomic clusters.
Rifampicin resistance (RR) and isoniazid resistance (INH-R) were defined as any resistance to rifampicin (RIF) and isoniazid (INH), respectively. MDR-TB was defined as resistance to at least RIF and INH. We designated transmitted resistance as previously defined:31 retreated cases of drug-resistant TB that belong to a genomic cluster and have the same resistance mutations as the other isolates in the cluster; and also all new, previously untreated cases of drug-resistant TB.
Statistical Analysis
Categorical variables were described using proportions while non-normal continuous data were expressed as medians with interquartile ranges (IQR). Differences between groups were tested using the Wilcoxon rank sum or the chi-square tests. The Cochran-Armitage trend test was used for identifying trends in the proportions. All analyses were performed with Stata version 14.0 and results with a p-value less than 0.05 were considered statistically significant.
Results
Drug Resistance Trends of Songjiang and Wusheng
We analyzed strains with RR, INH-R and MDR to assess trends of drug resistant TB in Songjiang and Wusheng. The overall RR, INH-R and MDR proportions were 6.6% (236/3558), 10.8% (383/3558) and 4.9% (176/3558), respectively, with no significant differences between the two study sites (Table 1). However, in the early half of the study period the proportion of cases with drug resistance was significantly higher in Wusheng than in Songjiang (Table 1). The trends of drug resistance in Songjiang were also distinct from those in Wusheng (Figure 1). Whereas the proportions of RR, INH-R and MDR were relatively stable in Songjiang, they showed a significant downward trend in Wusheng, where the percentage of RR decreased from 13.2% in 2009 to 3.7% in 2020 (Z=−3.05, p=0.002); INH-R from 16.5% to 7.3% (Z=−3.61, p<0.001); and MDR-TB from 10.7% to 3.7% (Z=−3.12, p=0.002).
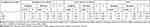 |
Table 1 Drug-Resistance Profile in Songjiang and Wusheng |
Changes in the Proportion and Drug Resistance Rate of Retreated Cases
TB patients that fail treatment and require retreatment have a high risk of harboring drug resistant strains. To identify trends, we analyzed changes over time in the proportion of retreated cases and the percentage of these cases that had drug resistant isolates. The proportion of retreated cases in Songjiang showed a significant downward trend (Z=−4.29, p<0.001), decreasing from 9.9% in 2011 to 4.3% in 2020 (Figure S1). In contrast, Wusheng showed no significant trend (p=0.365), and the total percentage of retreated cases in Wusheng was 9.9% over 12 years (Figure S1). Due to the small number of retreated cases each year, it was statistically challenging to assess trends in drug resistance by year, so we divided the study periods into two halves and compared the drug resistance rates between the early and latter halves of the study. With this analysis, we found that the prevalence of RR, INH-R and MDR-TB among retreated cases decreased in both Songjiang and Wusheng (Figure 2A and B). In Songjiang, the percentage of RR-TB among retreated cases decreased from 27.0% to 8.1% (χ2=5.64, p=0.018) and in Wusheng the change was from 35.1% to 16.0% (χ2=6.42, p=0.011).
Trends in Transmitted Drug-Resistance
Amongst all cases with drug resistance, 77.8% of RR, 87.4% of INH-R and 79.6% of MDR-TB cases in Songjiang, and 68.3% of RR, 78.6% of INH-R and 69.9% of MDR cases in Wusheng, were new, untreated cases, presumably due to transmission of resistant strains (Table S1). Of the retreated resistant cases, 13.3% to 25.8% were clustered with strains that had identical resistance mutations and were therefore the result of transmitted resistance (Table S2). Overall, 83.0% of RR, 89.1% of INH-R, and 83.5% of MDR-TB cases in Songjiang, and 73.3% of RR, 84.1% of INH-R, and 76.7% of MDR-TB cases in Wusheng were the result of transmitted resistance (Table S3).
There was no significant change in the proportion of transmitted resistance over the 12-year study period in Wusheng (Figure 3B). In Songjiang, however, the proportion of cases with transmitted RR increased from 74.7% (59/79) in 2011–2015 to 94.6% (53/56) in 2016–2020 (χ2=9.24, p=0.002), among cases with INH-R, from 83.8% (114/136) to 96.1% (98/102) (χ2=9.00, p=0.003), and among cases with MDR-TB, from 73.7% (42/57) to 95.7% (44/46) (χ2=8.91, p<0.003) (Figure 3A).
Trends of Drug-Resistant TB Among Local and Internal Migrant Cases in Songjiang
In Songjiang, 74.6% of TB cases occurred in internal migrants--individuals who move from one region to another within China, generally for employment opportunities. There was a significant age difference between local resident TB patients and migrant TB patients, with median ages of 59 (IQR, 39–72) and 27 (IQR, 23–38) years (p<0.001), respectively. The 9.2% (52/566) of local resident TB cases who were retreated was significantly greater than the 5.1% (85/1659) of migrant retreated cases (χ2=12.06, p<0.001), although the proportions of both the local (Z=−3.97, p<0.001) and migrant retreated cases (Z=−2.75, p=0.006) showed significant downward trends. The percentages of local and migrant cases in Songjiang with RR-TB were 4.9% and 6.4% (χ2=1.67, p=0.196), with INH-R were 8.7% and 11.4% (χ2=3.31, p=0.069), and with MDR-TB were 2.5% and 5.4% (χ2=7.99, p=0.005), respectively. Among all cases with drug-resistant TB, 79.3% with RR, 79.4% with INH-R and 86.4% with MDR-TB were migrants. Among migrant cases with drug resistance, transmitted resistance was observed in 81.3% (87/107) of cases with RR, 87.8% (166/189) of cases with INH-R and 83.1% (74/89) of cases with MDR-TB. There were no significant changes in the annual drug-resistance percentages in either the local residents or internal migrant TB patients in Songjiang.
Discussion
This study used data collected over at least 10 years to analyze trends in the prevalence of drug-resistant TB in the urban Songjiang District of Shanghai and rural Wusheng County in Sichuan Province. To our knowledge, this is the first long-term study of drug-resistance trends in China using representative, population-based WGS data. In Wusheng, there were significantly decreasing trends for RR, INH-R and MDR, while no significant changes were found in Songjiang. The proportion of drug resistance in retreated cases decreased in both Songjiang and Wusheng. Most of the resistance was the result of primary, transmitted resistance, especially in Songjiang, where the percentage of transmitted resistance amongst all cases with drug resistance increased to 95% in recent years.
In this study, we found a significant downward trend for drug-resistant TB in Wusheng, which is consistent with WHO estimates of MDR/RR-TB in China.32 This decrease presumably reflects the improvements to TB control associated with the implementation of new diagnostic techniques, standardized treatment regimens, and other improvements in TB control and treatment strategies. In Songjiang, however, there was no significant decline in drug-resistant TB over a 10-year period. One possible explanation is that approximately 80% of drug-resistant cases in Songjiang were internal migrants who were mostly new, untreated, TB cases with transmitted resistance. Because most their TB strains were not clustered with other strains isolated in Songjiang over the ten years of the study, it is likely that these drug-resistant migrant TB patients were infected with drug-resistant strains in their home towns and brought their infections with them to Songjiang.33
Kendall et al used a population-based MDR-TB transmission model to estimate that more than 80% (median 96%) of all global incident MDR-TB cases resulted from the transmission of drug resistant strains.34 Similarly, the current study found that more than 2/3 of drug-resistant cases were the result of transmitted drug-resistance. This trend was especially notable in the Songjiang district of Shanghai, where these proportions increased to 94.6%-96.1%, presumably because Songjiang’s effective TB control and treatment programs have greatly reduced the proportion of retreated cases and acquired resistance. In 2021, there were an estimated 33,000 cases of MDR/RR-TB in China, but only about 17,000 cases were laboratory-confirmed.35 This implies that a large number of MDR/RR-TB cases were not detected or treated and may therefore have been transmitting their resistant strains over a considerable time period. Decreasing the burden of drug resistant TB will require improved efforts to reduce transmission by detecting and effectively treating drug-resistant patients as early as possible.
This study had several limitations. Due to the low rates of drug resistance and retreatments, the number of yearly resistant and retreated cases in each area was limited. This made it difficult to statistically analyze these cases on an annual basis and unlikely that small differences would achieve statistical significance. In addition, this study collected cases from TB-designated hospitals but could not obtain the data and strains from patients who were not diagnosed at these hospitals. Some retreated or drug-resistant TB patients may have gone to municipal hospitals with more medical resources and would not have been captured in our population-based study.
Conclusion
In summary, this study analyzed 10 years of population-based genomic epidemiological data to identify trends in drug-resistant TB in the urban Songjiang district of Shanghai and rural Wusheng County in Sichuan Province. The data showed that drug-resistant TB is predominantly caused by the transmission of resistant strains in both Songjiang and Wusheng. Moreover, as treatment programs and treatment regimens improve, the proportion of drug resistant cases attributable to transmitted drug-resistance will likely increase. Therefore, the way to decrease the prevalence of drug-resistant TB is by reducing the transmission of drug-resistant strains through the early detection and effective treatment of patients with drug resistant TB.
Research Ethics
All patient information and WGS data in this study were obtained from previous studies, which were conducted in accordance with the Declaration of Helsinki and approved by the institutional review board of Biomedical Sciences, Fudan University. Written informed consent was obtained from all enrolled patients.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Shenzhen High-level Hospital Construction Fund (No. G2022157) and Shenzhen Clinical Research Center for Tuberculosis (No. 20210617141509001). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. WHO. Global Tuberculosis Report 2022. Geneva, Switzerland: World Health Organization; 2022.
2. Lefebvre N, Falzon D. Risk factors for death among tuberculosis cases: analysis of European surveillance data. Eur Respir J. 2008;31(6):1256–1260. doi:10.1183/09031936.00131107
3. Mathew TA, Ovsyanikova TN, Shin SS, et al. Causes of death during tuberculosis treatment in Tomsk Oblast, Russia. Int J Tuberc Lung Dis. 2006;10(8):857–863.
4. Santha T, Garg R, Frieden TR, et al. Risk factors associated with default, failure and death among tuberculosis patients treated in a DOTS programme in Tiruvallur District, South India, 2000. Int J Tuberc Lung Dis. 2002;6(9):780–788.
5. Cohn DL, Bustreo F, Raviglione MC. Drug-resistant tuberculosis: review of the worldwide situation and the WHO/IUATLD Global Surveillance Project. International Union Against Tuberculosis and Lung Disease. Clin Infect Dis. 1997;24 Suppl 1:S121–S130. doi:10.1093/clinids/24.supplement_1.s121
6. Sylverken AA, Kwarteng A, Twumasi-Ankrah S, et al. The burden of drug resistance tuberculosis in Ghana; results of the First National Survey. PLoS One. 2021;16(6):e0252819. doi:10.1371/journal.pone.0252819
7. Quispe N, Asencios L, Obregon C, et al. The fourth national anti-tuberculosis drug resistance survey in Peru. Int J Tuberc Lung Dis. 2020;24(2):207–213. doi:10.5588/ijtld.19.0186
8. Diande S, Badoum G, Combary A, et al. Multidrug-Resistant Tuberculosis in Burkina Faso from 2006 to 2017: results of National Surveys. Eur J Microbiol Immunol. 2019;9(1):23–28. doi:10.1556/1886.2018.00029
9. Nhung NV, Hoa NB, Sy DN, Hennig CM, Dean AS. The fourth national anti-tuberculosis drug resistance survey in Viet Nam. Int J Tuberc Lung Dis. 2015;19(6):670–675. doi:10.5588/ijtld.14.0785
10. Bojorquez-Chapela I, Backer CE, Orejel I, et al. Drug resistance in Mexico: results from the National Survey on Drug-Resistant Tuberculosis. Int J Tuberc Lung Dis. 2013;17(4):514–519. doi:10.5588/ijtld.12.0167
11. Zhao Y, Xu S, Wang L, et al. National survey of drug-resistant tuberculosis in China. New Engl J Med. 2012;366(23):2161–2170. doi:10.1056/NEJMoa1108789
12. Li Z, Liu F, Chen H, et al. A five-year review of prevalence and treatment outcomes of pre-extensively drug-resistant plus additional drug-resistant tuberculosis in the Henan Provincial Tuberculosis Clinical Medicine Research Center. J Global Antimicrob Resist. 2022;31:328–336. doi:10.1016/j.jgar.2022.09.010
13. Pang Y, Lu J, Huo F, et al. Prevalence and treatment outcome of extensively drug-resistant tuberculosis plus additional drug resistance from the National Clinical Center for Tuberculosis in China: a five-year review. J Infect. 2017;75(5):433–440. doi:10.1016/j.jinf.2017.08.005
14. Chen L, Wang X, Jia X, et al. Investigation of 3-year inpatient TB cases in Zunyi, China: increased TB burden but improved bacteriological diagnosis. FRONT PUBLIC HEALTH. 2022;10:941183. doi:10.3389/fpubh.2022.941183
15. Song WM, Li YF, Ma XB, et al. Primary drug resistance of mycobacterium tuberculosis in Shandong, China, 2004-2018. Respir Res. 2019;20:223. doi:10.1186/s12931-019-1199-3
16. Zhou M, Liu S, Li Q, et al. Drug resistance characteristics of Mycobacterium tuberculosis isolates between 2014 and 2017 in Sichuan, China: a retrospective study. PLoS One. 2018;13(12):e0209902. doi:10.1371/journal.pone.0209902
17. Wu B, Zhang L, Liu Z, et al. Drug-resistant tuberculosis in Zhejiang Province, China: an updated analysis of time trends, 1999-2013. Glob Health Action. 2017;10:1293925. doi:10.1080/16549716.2017.1293925
18. Bouzouita I, Cabibbe AM, Trovato A, et al. Whole-Genome Sequencing of Drug-Resistant Mycobacterium tuberculosis Strains, Tunisia, 2012-2016. Emerging Infect Dis. 2019;25:538–546. doi:10.3201/eid2503.181370
19. Edokimov K, Yamada Y, Dary C, et al. Whole-genome sequencing of Mycobacterium tuberculosis from Cambodia. Sci Rep. 2022;12(1):7693. doi:10.1038/s41598-022-10964-9
20. Zhao B, Liu C, Fan J, et al. Transmission and Drug Resistance Genotype of Multidrug-Resistant or Rifampicin-Resistant Mycobacterium tuberculosis in Chongqing, China. MICROBIOL SPECTR. 2022;10(5):e0240521. doi:10.1128/spectrum.02405-21
21. Phelan JE, O’Sullivan DM, Machado D, et al. Integrating informatics tools and portable sequencing technology for rapid detection of resistance to anti-tuberculous drugs. Genome Med. 2019;11(1):41. doi:10.1186/s13073-019-0650-x
22. Dohal M, Porvaznik I, Prso K, Rasmussen EM, Solovic I, Mokry J. Whole-genome sequencing and Mycobacterium tuberculosis: challenges in sample preparation and sequencing data analysis. Tuberculosis. 2020;123:101946. doi:10.1016/j.tube.2020.101946
23. Li M, Guo M, Peng Y, et al. High proportion of tuberculosis transmission among social contacts in rural China: a 12-year prospective population-based genomic epidemiological study. Emerg Microbes Infect. 2022;11(1):2102–2111. doi:10.1080/22221751.2022.2112912
24. Li M, Lu L, Jian Q, et al. Genotypic and Spatial Analysis of Transmission Dynamics of Tuberculosis in Shanghai, China: A 10-Year Prospective Population-Based Surveillance Study. Lancet Reg Health West Pac; 2024.
25. Li M, Lu L, Guo M, et al. Discrepancy in the transmissibility of multidrug-resistant mycobacterium tuberculosis in urban and rural areas in China. Emerg Microbes Infect. 2023;12(1):2192301. doi:10.1080/22221751.2023.2192301
26. Chen Y, Ji L, Liu Q, et al. Lesion Heterogeneity and Long-Term Heteroresistance in Multidrug-Resistant Tuberculosis. J Infect Dis. 2021;224(5):889–893. doi:10.1093/infdis/jiab011
27. Langmead B, Wilks C, Antonescu V, Charles R. Scaling read aligners to hundreds of threads on general-purpose processors. Bioinformatics. 2019;35(3):421–432. doi:10.1093/bioinformatics/bty648
28. Li H, Handsaker B, Wysoker A, et al. The Sequence Alignment/Map format and Samtools. Bioinformatics. 2009;25(16):2078–2079. doi:10.1093/bioinformatics/btp352
29. Koboldt DC, Zhang Q, Larson DE, et al. VarScan 2: somatic mutation and copy number alteration discovery in cancer by exome sequencing. Genome Res. 2012;22(3):568–576. doi:10.1101/gr.129684.111
30. Yang T, Gan M, Liu Q, et al. SAM-TB: a whole genome sequencing data analysis website for detection of Mycobacterium tuberculosis drug resistance and transmission. Brief Bioinform. 2022;23(2). doi:10.1093/bib/bbac030
31. Yang C, Luo T, Shen X, et al. Transmission of multidrug-resistant Mycobacterium tuberculosis in Shanghai, China: a retrospective observational study using whole-genome sequencing and epidemiological investigation. Lancet Infect Dis. 2017;17(3):275–284. doi:10.1016/S1473-3099(16)30418-2
32. World Health Organization. MDR_RR_TB_burden_estimates.csv. Global tuberculosis report; 2022. https://www.who.int/teams/global-tuberculosis-programme/data.
33. Yang C, Lu L, Warren JL, et al. Internal migration and transmission dynamics of tuberculosis in Shanghai, China: an epidemiological, spatial, genomic analysis. Lancet Infect Dis. 2018;18(7):788–795. doi:10.1016/S1473-3099(18)30218-4
34. Kendall EA, Fofana MO, Dowdy DW. Burden of transmitted multidrug resistance in epidemics of tuberculosis: a transmission modelling analysis. Lancet Respir Med. 2015;3(12):963–972. doi:10.1016/S2213-2600(15)00458-0
35. World Health Organization. Tuberculosis profile: china; 2022. https://worldhealthorg.shinyapps.io/tb_profiles/?_inputs_&entity_type=%22country%22&lan=%22EN%22&iso2=%22CN%22.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



