Back to Journals » Patient Preference and Adherence » Volume 18
The Status and Influencing Factors of COVID-19 Vaccination for 3–7-Year-Old Children Born Prematurely
Authors Shi J, Zhao F, Yang W, Zhu Y, Wang M, Yi B
Received 24 November 2023
Accepted for publication 14 March 2024
Published 29 March 2024 Volume 2024:18 Pages 787—796
DOI https://doi.org/10.2147/PPA.S451654
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jongwha Chang
Jingyun Shi,1,* Fangping Zhao,1,* Wanyin Yang,2 Yuru Zhu,1 Min Wang,1 Bin Yi1
1Department of NICU, Gansu Provincial Maternal and Child Care Hospital (Gansu Provincial Central Hospital), Lanzhou City, Gansu, 730050, People’s Republic of China; 2Department of NICU, Gansu University of Chinese Medicine, Lanzhou City, Gansu, 730050, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Min Wang; Bin Yi, Department of NICU, Gansu Provincial Maternal and Child care Hospital (Gansu Provincial Central Hospital), No. 143 of Qilihe North Street, Qilihe District, Lanzhou, 730050, People’s Republic of China, Tel +86 13919819662, Email [email protected]; [email protected]
Objective: To explore the status and influencing factors of COVID-19 vaccination for 3– 7-year-old children born prematurely.
Methods: A questionnaire was administered to parents of preterm infants born between 1 January 2016 and 31 December 2019 in Gansu Maternal and Child Health Hospital using convenience sampling.
Results: It was found that 96.81% of 282 parents had known about COVID-19 vaccines and acquired COVID-19- and vaccine-related knowledge primarily through WeChat (104/282, 36.88%) and TikTok (91/282, 32.27%). Most parents of the group whose children were vaccinated with a COVID-19 vaccine believed that this approach was effective in preventing COVID-19 (49.75%), whereas most parents of the group whose children were not vaccinated were worried about the adverse reaction and safety of the vaccine (45.88%). According to the regression analysis, the risk factors of children born prematurely receiving a COVID-19 vaccine were no vaccination against COVID-19 in the mothers (odds ratio [OR]=48.489, 95% CI: 6.524– 360.406) and in younger children (OR=12.157, 95% CI: 6.388– 23.139). Previous history of referral (OR=0.229, 95% CI: 0.057– 0.920), history of diseases (OR=0.130, 95% CI: 0.034– 0.503) and high educational level of guardians (OR=0.142, 95% CI: 0.112– 0.557) were protective factors for children born prematurely to receive COVID-19 vaccination.
Conclusion: There is a relatively high proportion of children born prematurely receiving COVID-19 vaccination, but some people still have concerns. Publicity in the later stage can be conducted through WeChat, TikTok and other social media platforms, with special attention paid to the populations with lower education levels.
Keywords: COVID-19 vaccine, vaccination willingness, children born prematurely, influencing factors
A Letter to the Editor has been published for this article.
Introduction
In 2019, an outbreak of unexplained pneumonia occurred in Wuhan, Hubei Province, China. Epidemiological surveys revealed that this cluster of cases was linked to the nearby South China Seafood Market.1,2 The World Health Organization (WHO) further confirmed that the pandemic of this acute respiratory infectious disease was caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).3 The SARS-CoV-2 virus is highly contagious and can be rapidly transmitted through the respiratory tract, resulting in the global COVID-19 pandemic.4 As of 13 May 2021, approximately 160 million people in 223 countries/regions worldwide have been infected with SARS-CoV-2, leading to over 3.32 million deaths due to severe COVID-19 complications.5
Although this infection is less common in children than in adults, there are still reports of confirmed cases of children with COVID-19.6 According to the report by SHAH,7 children with COVID-19 accounted for one tenth of the total cases of COVID-19 in the United States, and corresponding deaths for 3.31% of the total deaths from this infectious disease. The COVID-19 vaccine is a vaccine against SARS-CoV-2, and COVID-19 vaccination is the most effective means to prevent and control the pandemic.8 Moreover, successive marketing and orderly COVID-19 vaccinations are conducive to effective control of the COVID-19 pandemic in China. However, the COVID-19 vaccine is a newly developed product in a special period, with a limited total temporal span from research and development to marketing of less than one year. With the gradual increase in the number of vaccine recipients, some unexpected rare and serious adverse events emerged, such as thromboembolism caused by the AstraZeneca AZD1222 and Johnson & Johnson vaccines for COVID-19.9 In addition, the use of a new generation of mRNA-based vaccines is unprecedented among the different types of COVID-19 vaccines, and the immune response to vaccines is importantly correlated with the age, sex and disease of the vaccinated person.10 Furthermore, a growing number of studies have observed inter-individual heterogeneity of post-vaccine immune responses in specific populations,11 especially among elderly and immunocompromised individuals, while multiple studies demonstrated that the immune response of vulnerable populations is diminished in comparison with normal individuals.12,13
Premature infants are foetuses born before 37 weeks of pregnancy (≤259 days). Around 15 million premature births occur globally annually, indicating a global premature birth rate of approximately 11%. Epidemiological surveys of premature birth show a rising rate in many countries.14 According to the Global Report on Premature Infants’ released by the WHO in May 2012, there is at least one premature birth out of every 10 births, with approximately 1.2 million premature births in China, ranking second in the world.15 Premature infants are different from healthy full-term infants. Due to their premature separation from the mother, premature infants have completely different nutritional supply and growth patterns from those with normal intrauterine development. Many premature infants are unable to obtain sufficient nutritional reserves in the uterus, leading to a higher probability of intrauterine growth retardation. Moreover, premature infants have immature development of various systems of the body, resulting in poorer physical quality, underdeveloped organ systems and weakened immunity, thereby increasing the risk of infection and illness.16
Under the influence of the COVID-19 pandemic, preterm children, as a particularly vulnerable group, are more likely to be infected due to their reduced immunity. The COVID-19 vaccine has now been shown to be effective and safe for infants and children older than 6 months, reducing disease severity, hospitalisation, childhood multisystemic inflammatory syndrome and death.17 However, due to the special health conditions of preterm infants, parents will place a greater emphasis on the safety of vaccination. Public acceptance of the COVID-19 vaccine is critical to the implementation of vaccination,18 and previous studies have shown that the safety and efficacy of the vaccine, health outcomes associated with vaccination, trust in the health system and community sensitisation19 are influential factors in people’s willingness to receive the vaccine. To date, there are few reports on the status and willingness of parents of children born prematurely to vaccinate against COVID-19. In 2019, the WHO classified “vaccine hesitancy” as one of the top-10 threats to global health.20 In many parts of the world, a fair number of people are still questioning the necessity of vaccination and delaying or refusing vaccination.21 Previous studies have shown that the factors that contribute to vaccine hesitancy or willingness include socio-demographic characteristics, occupation, religious beliefs and social and environmental trust.22–24 Vaccine acceptability varies greatly among different vaccination recipients, and researchers have conducted studies with different populations. Children are a vulnerable group that needs protection, and parents may have more concerns and thoughts when considering vaccinating their children and may be more cautious about vaccinating their preterm children. The literature suggests that female parents are more concerned about the safety and efficacy of vaccines, are reluctant to vaccinate themselves and are more hesitant to vaccinate their children.24,25 At present, the COVID-19 solution in China has entered a stage of long-term prevention and control, similar to that of influenza, suggesting the importance of vaccine regulation after the national lockdown; however, there is still a poor understanding of the status of COVID-19 vaccination in children born prematurely and the related factors affecting their vaccination. Surveying the willingness of preterm children to be vaccinated and analysing the reasons for this is important for policy measures to increase the rate of vaccination. As such, this study investigates the status of COVID-19 vaccination for children aged 3–7 years who were born prematurely and discusses potential vaccination status and influencing factors to provide a reference for formulating targeted vaccination strategies.
Materials and Methods
Participants
A questionnaire survey was conducted between December 1st to 31st 2022 at Gansu Maternal and Child Health Hospital using the convenience sampling method among parents who delivered their preterm infants in the hospital. The inclusion criteria were as follows: (1) date of birth between 1 January 2016 and 31 December 2019; (2) children with a gestational age of <37 weeks; (3) children born during the mother’s first pregnancy; and (4) children aged 3–7 years. The exclusion criteria included: (1) individuals with concomitant mental/neurological disorders who were unable to express themselves autonomously; and (2) individuals with contraindications for vaccination. This study was approved by the Ethics Committee of Gansu Provincial Maternal and Child Health Care Hospital (Ethical approval number:(2022) GSFY lun shen NO.14). Written informed consent was obtained from all parents/local guardians.
Study Methods
The questionnaire used in this study was designed based on the actual situation in clinical practice and by referring to relevant literature,26,27 with a preliminary draft formed after discussion within the research group and revision by experts. The questionnaire was ultimately developed following discussion and modification by the experts based on the preliminary survey results. By employing convenience sampling, the QR code of the questionnaire generated on WJX.cn was distributed by Gansu Provincial Maternal and Child Health Care Hospital to the parents of 3–7-year-old children born prematurely. The parents of the children could participate in the survey through WeChat QR code scanning. After obtaining the informed consent of the participants, the questionnaire was completed by each WeChat account holder once. After recovery, the questionnaires were carefully checked and those with incomplete information or logical errors were eliminated. The questionnaire included 13 independent variables in total. The basic data requirement for multivariate statistical analysis is that the sample size is at least 10 times more than the independent variable. Hence, the sample size of this study had to be at least 156 considering a 20% loss rate.
Invalid questionnaires were determined according to the following criteria: (1) questionnaires with missing questions; (2) questionnaires with conflicting results in the positive and negative questions; (3) questionnaires with the same question options; (4) questionnaires with regular options, such as 1, 2, 3, 1, 2, 3, 1, 2, 3; and (5) questionnaires that were not filled out as instructed.
Data Collection
The questionnaire (see supplement1) included the following content: (1) socio-demographic characteristics of the respondents; (2) knowledge about COVID-19 and the vaccine; and (3) willingness to vaccinate with COVID-19 vaccines and the attendant reasons. After testing, the questionnaire showed good reliability and validity (the content validity index (S-CVI) was 0.86, the content validity index at the item level was 0.88–1.00, the mean S-CVI was 0.843, Cronbach’s alpha [α] coefficient was 0.761, the half-risk reliability was 0.725, the test-retest reliability of the total scale was 0.716 and the KMO value was 0.803 after an interval of 2 weeks). The demographic characteristics consisted of child’s gender, child’s age, respondent’s gender, gestational age, residence, father’s COVID-19 vaccination history, mother’s COVID-19 vaccination history, referral history, disease history, allergy/bloody stool history, education level, monthly household income and history of caesarean section. After the completion of the questionnaire, data entry was performed by double review.
Statistical Analysis
The statistical analysis of this study employed SPSS 26.0 statistical software. The Kolmogorov–Smirnov method was used for normality testing. The measurement data that met normality was represented by mean and standard deviation ( ), and the inter-group comparison applied an independent sample t-test. The counting data was expressed as frequency (n) or rate (%) and compared using the chi-squared (χ2) test. The multivariate analysis used a binary logistic regression model. The inspection level was set at α=0.05.
), and the inter-group comparison applied an independent sample t-test. The counting data was expressed as frequency (n) or rate (%) and compared using the chi-squared (χ2) test. The multivariate analysis used a binary logistic regression model. The inspection level was set at α=0.05.
Results
General Data
A total of 326 questionnaires were collected in this study, of which 282 were valid, with an effective response rate of 86.50%. A total of 282 children born prematurely were surveyed, including 135 boys and 147 girls, 197 of whom were vaccinated with a COVID-19 vaccine (69.86%). As shown in Table 1, there were statistically significant differences in age of children, gestational age, guardians’ education level, mother’s COVID-19 vaccination history, referral history, disease history, allergy/bloody stool history and guardian’s education level between children born prematurely vaccinated with COVID-19 vaccine and those not vaccinated (all P<0.05). No significant difference was observed between the two groups in gender of respondents, age of respondents, gender of children, residence, father’s COVID-19 vaccination history, proportion of caesarean sections and monthly household income (all P>0.05).
 |
Table 1 Demographic Characteristics of the Enrolled Subjects of Study |
Parents’ Awareness of COVID-19 and Vaccine
The results of the survey (Table 2) revealed that 96.81% of the parents of the 282 children had known about COVID-19 vaccines, 98.58% of the parents knew the main transmission route of COVID-19, 95.04% knew the preventive measures of COVID-19, 64.89% knew the age limit for COVID-19 vaccination and 63.83% knew that protective measures still had to be taken after vaccination. Furthermore, parents acquired COVID-19- and vaccine-related knowledge primarily through WeChat (104/282, 36.88%) and TikTok (91/282, 32.27%), as shown in Table 3.
 |
Table 2 Parents’ Awareness of COVID-19 and Vaccine |
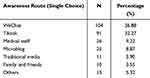 |
Table 3 Ways for Parents to Know About COVID-19 and Vaccine |
2.3 Parents’ willingness and reasons for agreeing to vaccinate children born prematurely with COVID-19 vaccine
As Table 4 shows, 69.86% of the parents and their children had received COVID-19 vaccination mainly due to their concern about the child’s infection with COVID-19 (18.27%), protecting others (6.09%), people around being vaccinated (21.83%), being affected by the news policy (4.06%) and vaccination accepted as an effective means of prevention (49.75%). However, 30.14% of parents did not take their children to receive COVID-19 vaccination because they believed that there was no risk of COVID-19 infection (8.24%), the short time interval between the development and marketing of the vaccine that needed to be considered (36.47%), concern about the adverse reaction/safety of the vaccine (45.88%) and concern about the effectiveness of the vaccine (9.41%).
 |
Table 4 Parents’ Willingness and Reasons for Children to Receive COVID-19 Vaccination |
Multivariate Analysis of Factors Influencing COVID-19 Vaccination in Children Born Prematurely
A Logistic regression analysis model was constructed by taking whether or not to vaccinate with a COVID-19 vaccine as the dependent variable (with=1, without=0), and factors with statistically significant differences in the univariate analysis as the independent variables. Table 5 shows the results of variable assignment. According to the regression analysis (Table 6), the risk factors of children born prematurely receiving a COVID-19 vaccine were no vaccination against COVID-19 in the mothers (odds ratio [OR]=48.489, 95% CI: 6.524–360.406) and children of a younger age (OR=12.157, 95% CI: 6.388–23.139). Previous history of referral (OR=0.229, 95% CI: 0.057–0.920), history of diseases (OR=0.130, 95% CI: 0.034–0.503) and high educational level of guardians (OR=0.142, 95% CI: 0.112–0.557) were protective factors for children born prematurely to receive COVID-19 vaccination.
 |
Table 5 Variable Assignment |
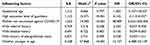 |
Table 6 Multivariate Analysis of Factors Influencing COVID-19 Vaccination in Children Born Prematurely |
Discussion
In January 2023, the National Health Commission announced the renaming of novel coronavirus pneumonia as COVID-19 and implemented the “Class A and Class B management” policy, suggesting that the focus of COVID-19 prevention and control should be transformed from “infection prevention” to “health protection and severe illness prevention”.28 Vaccination can not only prevent severe illness but can also effectively reduce the spread and outbreak of COVID-19. A study had found premature delivery was considered to be a risk factor for severe COVID-19 in premature children29,30 as this population showed poor health status and required more protection from COVID-19 vaccines compared with full-term children. In recent decades, the incidence of premature infants in China has been on the rise,31 accounting for approximately 7.8% of global premature infants, making it the second largest country globally in terms of incidence.32 Infants with younger gestational age at birth have less mature lung development and thus have a higher risk of developing lung infections as they grow up.33 Therefore, children born prematurely may need vaccine protection more urgently to avoid the infection of viruses.
In this study, 197 children born prematurely who received vaccination accounted for 69.86% of the total participants, a higher number than in other studies, which may be attributed to differences in regional economic development and educational level.34 Similar to previous studies,35 the main reason for the unwillingness for the remaining 85 parents to vaccinate against COVID-19 included their concern about the adverse reaction and safety of the vaccine and no popularisation of the vaccination in China. In another study,36 it was found that 31.9% of the negative comments on the adverse reactions of vaccination on microblogs indicated that the public still have doubts about COVID-19 vaccines.
Here, in the survey of COVID-19- and vaccine-related knowledge, the respondents showed high awareness of COVID-19-related knowledge, but low awareness of COVID-19 vaccines, which may explain the unwillingness to vaccinate against COVID-19 among some people, suggesting that more efforts should be made to publicise vaccine-related knowledge in the future to alleviate public concerns. It is crucial to choose the appropriate publicity approaches. Moreover, our study also indicated that parents obtained knowledge about COVID-19 vaccine primarily through WeChat and TikTok and rarely through traditional media. Therefore, in the current information age, publicity can be conducted through emerging publicity avenues, such as the government’s official WeChat public channel and TikTok, to increase parents’ willingness to receive COVID-19 vaccination.
In this study, in accordance with the analysis on the influencing factors of parents’ willingness to vaccinate their children against COVID-19, parents with low educational level, mothers who had not received COVID-19 vaccination, those of children without referral history and disease history and those of young children had low willingness to vaccinate their children against COVID-19. Compared with parents who received vaccines, parents who did not receive them were less willing to vaccinate their children. This is similar to a German survey.37 Parents’ attitudes towards vaccination and the susceptibility of children infected with COVID-19 are the key to improving children’s COVID-19 vaccination rate, and parents’ attitudes towards vaccination are closely related to their education level. The results of this study show that parents with lower education levels are more willing to vaccinate their children, which is consistent with a previous meta-analysis.18 It has also been shown that there is a positive correlation between parental knowledge and attitudes towards childhood vaccination and practice,38 that a high level of education is a positive factor for vaccination.39 On the one hand, this difference may be due to the deviation caused by the choice of samples, while on the other, it may also be affected by the occupation of the parents and the source of information reception. Additionally, people’s awareness of diseases may have an impact on their vaccination behaviour. People who believe that the disease is severe, that vaccines have preventive effects or that they are a susceptible population have higher willingness to vaccinate.40 According to the daily report on the official website of the China Health Commission, COVID-19 in China, predominated by mild and asymptomatic patients, shows low mortality and high cure rates. Consequently, the preventive and protective effect of vaccines on health has been weakened compared with the overemphasised vaccine risk. This may, to some extent, explain why parents of healthy children without underlying diseases were unwilling to vaccinate their children against COVID-19. Moreover, in terms of the age of children born prematurely, parents of younger children had lower willingness to vaccinate their children, indicating that most parents believe that young children are more sensitive to the potential side effects of vaccination.
This study has some limitations. First, based on a cross-sectional survey, the online self-reporting questionnaire adopted in this study could have resulted in some information bias. However, because the questionnaire was completed anonymously online it may have better ensured the authenticity of the information on this sensitive topic than a face-to-face survey. Second, the results reported in this single-centre survey with a smaller sample size might not be fully representative. There may also be other potential influencing factors that were not included in this survey, which needs to be considered in future studies. Finally, the results of this study might be applicable only to the current period as the public’s understanding and demand for COVID-19 vaccines are also changing continuously with the change of the global COVID-19 pandemic and the advancement of research on COVID-19 vaccines. Therefore, it is advisable to explore the vaccination willingness in different periods of the COVID-19 pandemic, which may be more effective in understanding the needs and concerns of the public.
Conclusions
In summary, the proportion of premature children vaccinated against COVID-19 is relatively high. Most parents of premature children know about COVID-19 from WeChat and TikTok. The concerns of parents of premature infants who are not vaccinated mainly lie in the safety and adverse reactions of vaccines. Parents’ willingness to vaccinate, education level, the mother’s vaccination history, the child’s age, referral history and disease history are the influencing factors for new coronavirus vaccination in premature infants. When conducting vaccination campaigns, WeChat, TikTok and other social media platforms could be used, with special attention paid to the populations with lower education levels. Furthermore, the relevant departments should strengthen efficient and fair implementation of vaccination while ensuring vaccine supply.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Gansu Provincial Maternal and Child Health Care Hospital (Ethical approval number:(2022) GSFY lun shen NO.14). Written informed consent was obtained from all parents/local guardians.
Funding
Key Program of Science and Technology Foundation of Gansu Province of China (Grant No. 21YF11FA004).
Disclosure
None of the authors have any personal, financial, commercial, or academic conflicts of interest.
References
1. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi:10.1056/NEJMoa2001316
2. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi:10.1056/NEJMoa2001017
3. World Health Organization. Naming the coronavirus disease (COVID-19) and the virus that causes it; 2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus.
4. World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19-11; 2020. Available from: https://www.who.int/directorgeneral/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
5. World Health Organization. COVID-19 Weekly Epidemiological Update; 2021. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/.
6. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) Outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1239–1242. doi:10.1001/jama.2020.2648
7. Shah S. Children and the American Rescue Plan: countering COVID-19 vaccine hesitancy during a global pandemic. Pediatr Res. 2021;90(2):237–239. doi:10.1038/s41390-021-01590-8
8. Norman FF, Comeche B, Martínez-Lacalzada M, et al. Seroprevalence of vaccine-preventable and non-vaccine-preventable infections in migrants in Spain. J Travel Med. 2021;28(4):taab025. doi:10.1093/jtm/taab025
9. Cines DB, Bussel JB. SARS-CoV-2 Vaccine-Induced Immune Thrombotic Thrombocytopenia. N Engl J Med. 2021;384(23):2254–2256. doi:10.1056/NEJMe2106315
10. Notarte KI, Ver AT, Velasco JV, et al. Effects of age, sex, serostatus, and underlying comorbidities on humoral response post-SARS-CoV-2 Pfizer-BioNTech mRNA vaccination: a systematic review. Crit Rev Clin Lab Sci. 2022;59(6):373–390. doi:10.1080/10408363.2022.2038539
11. Salmerón Ríos S, Mas Romero M, Cortés Zamora EB, et al. Immunogenicity of the BNT162b2 vaccine in frail or disabled nursing home residents: COVID-A study. J Am Geriatr Soc. 2021;69(6):1441–1447. doi:10.1111/jgs.17153
12. Notarte KI, Catahay JA, Peligro PJ, et al. Humoral response in hemodialysis patients post-SARS-CoV-2 mRNA vaccination: a systematic review of literature. Vaccines. 2023;11(4):724. doi:10.3390/vaccines11040724
13. Notarte KI, Guerrero-Arguero I, Velasco JV, et al. Characterization of the significant decline in humoral immune response six months post-SARS-CoV-2 mRNA vaccination: a systematic review. J Med Virol. 2022;94(7):2939–2961. doi:10.1002/jmv.27688
14. Deindl P, Diemert A. From structural modalities in perinatal medicine to the frequency of preterm birth. Semin Immunopathol. 2020;42(4):377–383. doi:10.1007/s00281-020-00805-0
15. Blencowe H, Cousens S, Oestergaard MZ, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379(9832):2162–2172. doi:10.1016/S0140-6736(12)60820-4
16. Zaidi S, Bhutta Z, Hussain SS, et al. Multisector governance for nutrition and early childhood development: overlapping agendas and differing progress in Pakistan. BMJ Glob Health. 2018;3(Suppl 4):e000678. doi:10.1136/bmjgh-2017-000678
17. Jantarabenjakul W, Chantasrisawad N, Nantanee R, et al. Global COVID-19 Vaccination in Infants and Children: effectiveness, Safety, and Challenges. Asian Pac J Allergy Immunol. 2023;41(4):292–303. doi:10.12932/AP-300423-1596
18. Ma Y, Ren J, Zheng Y, et al. Chinese parents’ willingness to vaccinate their children against COVID-19: a systematic review and meta-analysis. Front Public Health. 2022;10:1087295. doi:10.3389/fpubh.2022.1087295
19. Kaplan RM, Milstein A. Influence of a COVID-19 vaccine’s effectiveness and safety profile on vaccination acceptance. Proc Natl Acad Sci U S A. 2021;118(10):e2021726118. doi:10.1073/pnas.2021726118
20. Dubé E, Laberge C, Guay M, et al. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9(8):1763–1773. doi:10.4161/hv.24657
21. Siddiqui M, Salmon DA, Omer SB. Epidemiology of vaccine hesitancy in the United States. Hum Vaccin Immunother. 2013;9(12):2643–2648. doi:10.4161/hv.27243
22. Lin Y, Hu Z, Zhao Q, et al. Chinese parents’ intentions to vaccinate their children against SARS-CoV-2 infection and vaccine preferences. Hum Vaccin Immunother. 2021;17(12):4806–4815. doi:10.1080/21645515.2021.1999143
23. Chen F, He Y, Shi Y. Parents’ and guardians’ willingness to vaccinate their children against COVID-19: a systematic review and meta-analysis. Vaccines. 2022;10(2):179. doi:10.3390/vaccines10020179
24. Umakanthan S, Bukelo MM, Bukelo MJ, et al. Social environmental predictors of COVID-19 vaccine hesitancy in India: a population-based survey. Vaccines. 2022;10(10):1749. doi:10.3390/vaccines10101749
25. Galanis P, Vraka I, Siskou O, et al. Willingness, refusal and influential factors of parents to vaccinate their children against the COVID-19: a systematic review and meta-analysis. Prev Med. 2022;157:106994. doi:10.1016/j.ypmed.2022.106994
26. Yang Y, Hu H, Ai YT, et al. Analysis of parents’ willingness to vaccinate their children against COVID-19 and its influencing factors. J Med Pest Control. 2022;38:390–393. doi:10.7629/yxdwfz202204020
27. Guo W, Wang WN, Yang X, et al. Analysis on the willingness to vaccinate against COVID-19 and its influencing factors among children aged 3-6 in dezhou city. Strait J Prevent Med. 2022;28(05):31–33.
28. Xu SX. Epidemic prevention and control transformed from infection prevention and control to medical treatment. China Hospital CEO. 2023;19(Z1):2.
29. Woodruff RC, Campbell AP, Taylor CA, et al. Risk factors for severe COVID-19 in children. Pediatrics. 2022;149(1):e2021053418. doi:10.1542/peds.2021-053418
30. Choi JH, Choi SH, Yun KW. Risk factors for severe COVID-19 in children: a systematic review and meta-analysis. J Korean Med Sci. 2022;37(5):e35. doi:10.3346/jkms.2022.37.e35
31. Deng K, Liang J, Mu Y, et al. Preterm births in China between 2012 and 2018: an observational study of more than 9 million women. Lancet Glob Health. 2021;9(9):e1226–e1241. doi:10.1016/S2214-109X(21)00298-9
32. Chawanpaiboon S, Vogel JP, Moller AB, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. 2019;7(1):e37–e46. doi:10.1016/S2214-109X(18)30451-0
33. Azab SF, Sherbiny HS, Saleh SH, et al. Reducing ventilator-associated pneumonia in neonatal intensive care unit using ”VAP prevention Bundle”: a cohort study. BMC Infect Dis. 2015;15:314. doi:10.1186/s12879-015-1062-1
34. Zhao CY, Shi J, Zhang GF, et al. Willingness and associated factors of novel coronavirus vaccination among parents of primary and middle school students in Tongzhou District of Beijing. Chin J Sch Health. 2021;42(3):371–374. doi:10.16835/j.cnki.1000-9817.2021.03.013
35. Sinuraya RK, Kusuma ASW, Pardoel ZE, et al. Parents’ knowledge, attitude, and practice on childhood vaccination during the COVID-19 pandemic in Indonesia. Patient Prefer Adherence. 2022;16:105–112. doi:10.2147/PPA.S339876
36. Yin F, Wu Z, Xia X, et al. Unfolding the Determinants of COVID-19 Vaccine Acceptance in China. J Med Internet Res. 2021;23(1):e26089. doi:10.2196/26089
37. Brandstetter S, Böhmer MM, Pawellek M, et al. Parents’ intention to get vaccinated and to have their child vaccinated against COVID-19: cross-sectional analyses using data from the KUNO-Kids health study. Eur J Pediatr. 2021;180(11):3405–3410. doi:10.1007/s00431-021-04094-z
38. Maneesriwongul W, Butsing N, Deesamer S. Parental hesitancy on COVID-19 vaccination for children under five years in Thailand: role of attitudes and vaccine literacy. Patient Prefer Adherence. 2023;17:615–628. doi:10.2147/PPA.S399414
39. Zhu YF, Shi Y. Analysis of willingness and influencing factors of EV71 vaccination among parents of 6-5-year-old children in Changyuan City, Henan Province in 2020. Clin Med. 2022;42(3):60–62. doi:10.19528/j.issn.1003-3548.2022.03.023
40. Lin S, Guo X, Li J, et al. Analysis on pneumonia vaccination willingness and its influential factors among the elderly people in Shanghai City. Chin J Dis Cont Prevent. 2015;19(10):975–978. doi:10.16462/j.cnki.zhjbkz.2015.10.002
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
