Back to Journals » International Journal of Women's Health » Volume 16
The Risk of Cervical Cancer in Women Among Han, Bai, Dai and Hani Ethnic Minorities in Yunnan Province of China
Authors Zhao M, Gao MZ, Gu RY, Luo L, Ding SR, He L, Jia Y, Zhang HP , Yang HY, Li GF
Received 19 October 2023
Accepted for publication 6 February 2024
Published 5 March 2024 Volume 2024:16 Pages 373—384
DOI https://doi.org/10.2147/IJWH.S445471
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Everett Magann
Min Zhao,1,* Ming-Zhu Gao,1,* Rong-yan Gu,1,* Lei Luo,1 Song-rui Ding,1 Liang He,2 Yue Jia,3 Hong-ping Zhang,3 Hong-ying Yang,3 Gao-feng Li1
1Medical Administration Department, The Third Affiliated Hospital of Kunming Medical University (Yunnan Cancer Hospital, Yunnan Cancer Center), Kunming, Yunnan, People’s Republic of China; 2Medical Laboratory Department, The Third Affiliated Hospital of Kunming Medical University (Yunnan Cancer Hospital, Yunnan Cancer Center), Kunming, Yunnan, People’s Republic of China; 3Gynecological Department, The Third Affiliated Hospital of Kunming Medical University (Yunnan Cancer Hospital, Yunnan Cancer Center), Kunming, Yunnan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hong-ying Yang; Gao-feng Li, Email [email protected]; [email protected]
Background: Research on the risk factors for cervical cancer in Yunnan Province’s four characteristic ethnic groups (Han, Bai, Dai, and Hani) is lacking.
Objective: To study the risk factors of cervical cancer in four ethnic women in Yunnan Province, and to provide evidence for its prevention.
Methods: The cervical cancer patients of Han, Bai, Dai and Hani ethnic groups in Yunnan Province who were first diagnosed in the Third Affiliated Hospital of Kunming Medical University (Yunnan Cancer Hospital, Yunnan Cancer Center) from January 2011 to December 2020 were selected as the research objects. The 1:1 matched case-control study method was used, and single factor and conditional logistic regression were used for statistical analysis.
Results: HPV types 16, 18 and 58 are mostly related with cervical cancer, the younger the age of the last pregnancy, the more times of pregnancy, childbirth and abortion, especially the younger the first marriage age of Bai and Dai, are the risk factors of cervical cancer; the infection of genital tract bacteria, mycoplasma and chlamydia is closely related to the incidence of cervical cancer in four ethnicities. Multifactorial analysis showed that demographic characteristics and environment/behavior were not included in the influencing factors of cervical cancer; among Han, Bai, Dai and Hani ethnic minorities, contraception (OR=0.29, OR=0.03, OR=0.09, OR=0.16, P< 0.05) was positive factor, HPV infection (OR=64.77, OR=128.71, OR=71.89, OR=40.07, P< 0.01) was a causative factor of cervical cancer.
Conclusion: Risk of high parity with cervical cancer could be due to a complex interplay of factors, it is very important to formulate prevention strategies and measures in line with the cervical cancer of Han, Bai, Dai and Hani ethnic groups women in Yunnan Province.
Keywords: cervical cancer, risk factors, case-control study, Han, Bai, Dai and Hani ethnic minorities, Yunnan Province
Introduction
The exact cause and pathophysiology of cervical cancer are still unknown, however it is a multifaceted, multistep, complicated, and progressive biological process.1,2 Studies have shown that the incidence rate of cervical cancer in China (10.7/100,000) is significantly higher than the World Health Organization’s threshold (less than 4/100,000),3 In 2017, the crude incidence rate of cervical cancer in women in Yunnan Province was 15.04/100,000, and the crude mortality rate was 5.94/100,000.4 There are 26 ethnic groups in Yunnan Province, with Han Chinese as the main ethnic group (about 66.6%) and 25 other ethnic minorities (about 33.4%) living in the province, and Bai, Dai and Hani are the top three ethnic minorities, accounting for 28.77% of the total ethnic population in Yunnan Province.5 Ethnic minority women have a unique living environment and ethnic customs,6 and various factors may have different effects on the incidence of cervical cancer in this population. Early identification of the precancerous lesion and its risk factors is paramount in preventing cervical cancer. An overview of the risk factors for cervical cancer in ethnic minorities was provided in the authors’ prior study,7 and the aim of this study is to further analyze the causes of cervical cancer among the Han Chinese, the three unique ethnic minorities (Bai, Dai, and Hani) who are the top three in terms of population size for comparative analysis, so as to put forward targeted measures and recommendations for the prevention of cervical cancer in different ethnic groups.
Materials and Methods
Research Subjects
A hospital-based 1:1 matched case-control study was conducted in selected health facilities in the Third Affiliated Hospital of Kunming Medical University (Yunnan Cancer Hospital, Yunnan Cancer Center) from January 2011 to December 2020, the subjects of the study were women of Han, Bai, Dai and Hani ethnicities in Yunnan Province who were treated in the hospital in strict accordance with the inclusion/exclusion criteria.
Case Group
Inclusion Criteria
- Cases originated from Han, Bai, Dai and Hani women in various regions of Yunnan Province;
- Diagnosed as cervical cancer by pathological histology;
- New cases diagnosed on first admission and HPV testing;
- A primary malignant tumor of the cervix.
Exclusion Criteria
- Patients with cervical cancer of other ethnicities (except Han, Bai, Dai and Hani) of Yunnan Province origin;
- Patients with a history of uterine or cervical surgery;
- Not tested for HPV and reproductive tract infection indicators;
- Patients with combined malignant tumors of other sites.
Control Group
Inclusion Criteria
- Han, Bai, Dai and Hani women originating from various regions of Yunnan Province;
- Matching cases with each group originated from the same area, the same ethnicity, with an individual age-matching (± 3 years);
- The results of gynecological examination and cervical cytology were “no malignant cells or intraepithelial lesion cells”;
- HPV and reproductive tract infection indicators have been examined.
Exclusion Criteria
- Women of other ethnic groups with origins in Yunnan Province;
- Patients with severe cervical erosion and/or precancerous cervical lesions (cervical intraepithelial neoplasia);
- Those with abnormal cervical cytology;
- Those with HPV antiviral treatment.
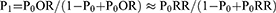
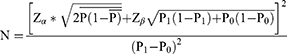
Determination of Sample Size
The sample size was calculated according to the sample size calculation method of case-control studies. According to the relevant studies,8 the relative risk ratio (RR) of HPV infection and cervical cancer development was 2.9, the infection rate (P0) of HPV in the general population was about 16%, the α and β values were checked in the table, Zα was 1.64 and Zβ was 1.28, and the calculation formula was as follows:
The formula calculated that 81 individuals were required for each case and control group, and the sample size of each case and control group was not less than 100 individuals per ethnic group, taking into account the 5–20% non-response rate and the lost visit rate.
Research Content and Methodology
The self-designed medical record data collection table and follow-up questionnaire were used to investigate the basic demographic situation, host factors, environmental / behavioral factors and biological factors of the subjects by consulting the medical records, telephone follow-up and on-site investigation of the patients. Logistic regression analysis was used to establish a multi-factor prediction model affecting the incidence of cervical cancer in four ethnic women in Yunnan Province.
Statistical Methods
A database was established using Epidata 3.0, and all survey data were double-entered, logically corrected for errors after review, and statistically analyzed using SPSS 26.0. The measurement data were described by mean ± standard deviation, and the count data were described by composition ratio (%), and t-test, ANOVA and χ² test, corrected χ² test or rank sum test were used for the analysis of single factors; after single factor analysis, statistically significant variables were screened out, and then conditional logistic regression was used for multi-factor analysis. Stepwise regression was used to screen the independent variables in the model. The inclusion criteria was α≤0.05, the exclusion criteria was α≥0.10, and the test level was α=0.05. For all statistical tests, two-sided p-value of <0.05 was considered statistically significant.
Results
Basic Demographics of the Four Ethnic Groups
In this study, Dai and Hani ethnic minorities’ cervical cancer was diagnosed at a younger age (F=4.35, P < 0.01). In the same case control group, there was no statistically significant difference in the age of each nationality (t=−1.61, t=−1.01, t=−0.43, t=−0.51, P > 0.05), all of which were comparable. In the case groups of Han, Bai, Dai and Hani ethnic groups, the differences in medical insurance, occupation, body mass index and education level were statistically significant (χ2=13.15, χ2=53.54, χ2 = 29.56, χ2 = 29.20, P < 0.05); the proportions of married patients were: 94.1%, 92.3%, 95.3% and 91.7% respectively (χ2= 2.23, P > 0.05).
The composition of health insurance type (χ2 =135.32, P<0.01), occupation (χ2 =89.34, P<0.01), and marital status (χ2 =4.25, P <0.05) were statistically significant differences between the Han ethnicity case group and the control group. The type of medical insurance was predominantly resident medical insurance in both case and control groups among the Bai, Dai and Hani ethnic groups (χ2 =7.15, P <0.05; χ2 =0.42, P >0.05; χ2 =12.07, P >0.05). See Table 1.
 |
Table 1 Basic Demographic Information of the Four Ethnic Groups [ |
Environmental / Behavior Factors of the Four Ethnic Groups
In the case groups of all four ethnic groups: in the composition of passive smoking, passive smoking intensity and use of contraception (χ2=74.19, χ2=105.46, χ2=18.47, P<0.01); the oldest age of menarche was 14.82±1.91 years in Hani patients (F=6.93, P<0.01); the age of first sexual intercourse, age of first marriage, age of first pregnancy and age of last pregnancy were the youngest ethnic groups were 18.82 ± 1.72 years (F = 3.12, P < 0.05) for Dai, 21.06 ± 3.04 years (F = 2.95, P < 0.05) for Dai, 21.52 ± 3.51 years (F = 0.31, P > 0.05) for Hani, and 25.32 ± 10.71 years (F = 10.11, P < 0.05) for Han; the higher percentages of pregnancies ≥3 times and deliveries ≥2 times were 69.4% for Hani and 73.4% for Dai, respectively (χ2= 0.41, χ2 = 0.40, P > 0.05); among patients of the four ethnic groups, the highest proportion of ethnic groups with the number of abortions ≥2 was 39.7% for Hani (χ2 = 16.33, P < 0.01), ever the family history of tumor has not kept a significant association with cervical cancer (χ2=5.14, P>0.05).
Except for the case group of the Hani ethnic group, which differed from the control group in the proportion of alcohol consumption (3.3% vs 0.0%) (χ2 = 4.07, P < 0.05). The proportion of contraceptive use was lower in all four ethnic case groups than in the control group (χ2 =102.51, χ2 = 26.23, χ2 = 30.42, χ2 = 22.59, P <0.01).
Menstruation, marriage, pregnancy and family history of tumors (Whether any of the close relatives had malignant tumors of the female reproductive system, such as cervical cancer, endometrial cancer, ovarian cancer, etc.): Age at last pregnancy, number of pregnancies, and number of deliveries statistically significant differences between the Han ethnicity case group and the control group (t = 3.01, χ2 = 13.89, χ2 = 31.06, P < 0.01); Age at menarche (t= 2.73, P < 0.01) and age at first marriage (t= −2.03, P < 0.05) were statistically significant differences between the Bai case group and the control group. The age at first marriage (t= 2.62, P < 0.05), age at first pregnancy (t= 2.06, P < 0.05), number of pregnancies (χ2 = 5.12, P < 0.05), and number of deliveries (χ2 = 6.29, P < 0.01) between the Dai case group and the control group See Table 2.
 |
Table 2 Environmental / Behavior Factors of the Four Ethnic Groups [n (%), |
HPV and Other Microbial Infections in Four Ethnic Groups
HPV Infection in Four Ethnic Groups
In terms of the composition of HPV infection, the difference was no statistically significant difference in the case group of the four ethnic groups (χ2 = 6.23, P > 0.05), while a difference with regard to HPV infection was observed between the case and control groups of the four ethnic groups (χ2 = 1263.57, χ2 = 1186.09, χ2 = 144.32, χ2 = 103.19, P < 0.001).The genotypes of HPV infection in patients with cervical cancer were predominantly type 16, 18 and 58, and there was no statistically significant difference in the proportion of patients from the four ethnic groups infected with the above three HPV genotypes (χ2 =1.06, χ2 =0.78, χ2 =4.57, P>0.05).The proportions of Han ethnicity case group and control group infected with HPV 16, HPV 18 and HPV 58 were 57.9% and 15.0% (χ2 =36.63, P < 0.01), 13.0% and 15.0% (χ2 =2.01, P > 0.05), 8.5% and 0.0% (χ2 =3.83, P < 0.01), respectively. See Table 3.
 |
Table 3 HPV Infection in the Four Ethnic Groups[n (%)] |
Classification of HPV High-Risk Infection and Multiple Infections in Cervical Cancer Patients of Four Ethnic Groups
Among cervical cancer patients with HPV infection in Han, Bai, Dai and Hani ethnicities, there were statistically significant differences in the composition of HPV high-risk infection, HPV single genotype infection, and HPV dual genotype infection (P < 0.01); there were 10 cases of HPV multiple genotype infection in Han patients only, accounting for: 2.4%. See Table 4.
 |
Table 4 Classification of HPV High-Risk Infection and Multiple Infections in Cervical Cancer Patients of Four Ethnic Groups [n (%)] |
Other Microbial Infections in Four Ethnic Groups
In the case groups of Han, Bai, Dai and Hani ethnic groups in patients’ infection with viral hepatitis, AIDS/syphilis, cervicitis and pelvic infections (χ2 =0.34, χ2 =6.30, χ2 =4.25, χ2 =4.56, P > 0.05). The proportion of urinary tract infection was the highest in Bai patients at 50.5% and the lowest in Hani at 29.8% (χ2 =15.6, P <0.01); the proportion of vaginal fungal infection was the highest in Hani patients at 5.8% (χ2 =15.23, P <0.01); vaginal bacterial infection, mycoplasma/chlamydia infection proportion were the highest in Han ethnicity, 75.8% and 18.8%, respectively, and there was statistically significant difference between the two infections in patients of the four ethnic groups (χ2 =260.23, χ2 =230.43, P <0.01).
The proportion of urinary tract infection, vaginal bacterial infection, mycoplasma/chlamydia infection, AIDS/syphilis, endometritis and pelvic infection were higher in the Han case group than in the control group (χ2 =44.72, χ2 =49.29, χ2 =184.2, χ2 =16.52, χ2 =4.57, χ2 =11.46, P < 0.01). The percentage of viral hepatitis, urinary tract infection, vaginal bacterial infection, and HIV/syphilis infection were higher in the Bai case group than in the control group (χ2 =4.68, χ2 =9.38, χ2 =44.08, χ2 =4.59, P <0.05). The proportion of urinary tract infection and HIV/syphilis infection in the Dai case group was higher than that in the control group (χ2 =11.13, χ2 =7.69, P <0.01). The proportion of vaginal fungal infection and vaginal trichomonas infection in the Hani case group was higher than that in the control group (χ2 =9.53, χ2 =11.30, P <0.05). See Table 5.
 |
Table 5 Other Microbial Infections in the Four Ethnic Groups [n (%)] |
Analysis of Influencing Factors of Cervical Cancer in Four Ethnic Groups
Those variables tested with P ≤ 0.05 in the bivariate logistic regression analysis were entered into multivariate logistic regression analysis. Controlling for the effect of other confounding factors, later age at last pregnancy (OR=0.97, P=0.001) and contraception (OR=0.29, P<0.01) were protective factors, while HPV infection (OR=64.77, P< 0.01), urinary tract infection (OR=1.62, P= 0.03), vaginal bacterial infection (OR=1.89, P= 0.004), mycoplasma /chlamydia infection (OR=8.94, P<0.01), and pelvic infection (OR=5.31, P= 0.001) were risk factors for cervical cancer in Han ethnicity.
For cervical cancer in Bai ethnicity, later age at first marriage (OR=0.80, P= 0.02) and contraception (OR=0.03, P<0.001) showed significant association as protective factors, later age at menarche (OR=1.47, P=0.03), HPV infection (OR=128.71, P<0.001), vaginal bacterial infection (OR=17.85, P<0.001) were risk factors.
The number of childbirth ≤1 (OR=0.31, P=0.02) and contraception (OR=0.09, P<0.001) were protective factors, HPV infection (OR=71.89, P<0.001) and urinary tract infection (OR=4.07, P= 0.004) showed significant association as risk factors for cervical cancer in Dai ethnicity.
For cervical cancer in Hani ethnicity, contraception (OR=0.16, P=0.02) was a protective factor, HPV infection (OR=40.67, P<0.01) was a risk factor. see Table 6.
 |
Table 6 Multifactorial Analysis of Cervical Cancer Development in Four Ethnic Groups |
Discussion
Main Findings of the Study
In terms of HPV DNA typing, patients with cervical cancer from four ethnic groups, Han, Bai, Dai, and Hani, were predominantly infected with high-risk types of HPV 16, 18, and 58. From the 31 high-risk HPV infections, high-risk HPV infection was the main cause of cervical cancer in four ethnic groups, the risk of HPV infection was highest among the Bai (OR=128.71), followed by Dai (OR=71.89), Han (OR=64.77), and Hani (OR=40.67).
In this study, it was analyzed that: later age at last pregnancy (OR=0.97) was a protective factor for cervical cancer among Han ethnicity; later age at first marriage (OR=0.80) was a protective factor for cervical cancer development among Bai; later age at first marriage and later age at first pregnancy may be a protective factor for cervical cancer among Dai. In the univariate analysis of this study, the number of pregnancies, deliveries, and abortions were not associated with the occurrence of cervical cancer in Bai and Hani; the proportion of pregnancies ≥3 and deliveries ≥2 were higher in the case groups of Han and Dai than in the control group, which could be considered to be associated with cervical cancer, and fewer deliveries would reduce the risk of cervical cancer in Dai (OR=0.31).
In this study, the highest proportion of mycoplasma/chlamydia infection was found in Han ethnicity cervical cancer patients, which was a major risk factor of cervical cancer in Han ethnicity (OR=8.94). The proportion of urinary tract infection was higher in all four ethnic groups of cervical cancer cases than in the control group, and the difference in composition among the three case controls of Han, Bai, and Dai had a difference, which can be considered that there is an significant association between the occurrence of cervical cancer and urinary tract infection. Upon further multifactorial analysis, it can be concluded that urinary tract infection is a risk factor for cervical cancer patients of Han and Dai ethnic groups (OR=1.62, OR=4.07).
Multifactorial analysis showed that demographic characteristics and environment/behavior were not included in the influencing factors of cervical cancer; among Han, Bai, Dai and Hani ethnic minorities, contraception (OR=0.29, OR=0.03, OR=0.09, OR=0.16, P<0.05) was positive factor, HPV infection (OR=64.77, OR=128.71, OR=71.89, OR=40.07, P<0.01) was a causative factor of cervical cancer.
Strengths and Limitations
Currently, there are no studies on the risk factors of cervical cancer among the three ethnic minorities and the Han Chinese in Yunnan Province. In this study, cervical cancer patients of four ethnic groups in Yunnan Province, namely Han, Bai, Dai and Hani, were studied using a 1:1 matched case-control study to conduct an all-encompassing, multifactorial and comprehensive study of cervical cancer risk factors in terms of demographic characteristics, environmental/behavioral factors, menstruation, marriage, pregnancy and family history of the tumors, HPV infections, and infections by other microorganisms. Previous related studies have shown that general demographics such as age, occupation, and marital status are strongly associated with the occurrence of cervical cancer;9 however, the above factors were not included as influencing factors in the multifactorial in this study, which may be caused by the multifactorial analysis that excludes the influence of confounding factors, and may be related to the fact that this study was a single-center study with a small sample size, and there were problems of loss of interviews and bias in the survey.
Comparison with Existing Literature
A significant association between cervical cancer and reproductive tract infections has been confirmed by numerous studies.10 In the study of Huang Jianlan,11 the infection rate of bacteria in cervical cancer patients was concluded to be 29.27%. In the present study, the bacterial infection rate in cervical cancer patients was higher, up to 75.80% in Han patients, and vaginal bacterial infection was a risk factor in Han (OR=1.89) and Bai (OR=17.85) cervical cancer patients. Considering that the population in this study were all Yunnan household, with a predominantly rural population, ethnic minorities are located in remote mountainous areas, with lagging medical, economic and educational conditions, and with poorer nutritional status and resistance, there is a lack of education about gender hygiene, combined with long-term menstruation, sexual intercourse and puerperium without good hygienic practices,12 which may be a major causative factor of female reproductive tract bacterial infections.
In this study, Mycoplasma/Chlamydia infection was a risk factor for cervical cancer in Han Chinese, and reproductive tract infections were not associated with cervical cancer in Dai and Hani ethnic groups in multifactorial analysis, but Trichomonas vaginalis infection was correlated with the incidence of cervical cancer in these two ethnic groups in unifactorial analysis, so that the influence of reproductive tract infections in Dai and Hani ethnic groups cannot be ignored. In previous studies it has also been shown,13,14 that mycoplasma and chlamydia infections are potential factors for various diseases such as infertility, ectopic pregnancy, cervicitis, pelvic inflammatory disease and cervical cancer. Panatto, Zhu et al showed15,16 that chlamydia infection affects HPV infection status and increases the incidence, leading to a cellular immune response of the autoimmune system to HPV, which leads to persistent infection. On the other hand, chlamydial infection causes segregation defects on chromosomes, contributing to multipolar differentiation and causing chromosomal instability, which in turn develops into tumors.17
Future Directions for Research
HPV persistence is one of the most important factors predicting the risk of the risk of developing recurrent recurrence,18 and HPV persistence is the main factor influencing the process of carcinogenesis.19 The question of how HPV affects the development of cervical cancer and postoperative recurrence will be the focus of further prospective studies. The exploration in the direction of the effect of interaction between HPV and other risk factors, such as genital tract infections, on the development of cervical cancer, the relationship between multiple infections of different subtypes of HPV and the development of cervical cancer, and the evaluation of the effect of the use of the HPV vaccine in different ethnic groups will also continue.
Conclusion
The interaction of multiple factors has led to a high prevalence of cervical cancer among women of four ethnic groups in Yunnan Province. The results of this study can guide the relevant authorities in formulating preventive strategies and measures for cervical cancer among ethnic minority women in Yunnan Province.
Data Sharing Statement
The data in this study are true and reliable.The datasets generated and/or analysed during the current study are not publicly available due because they are related to patients but are available from the corresponding author on request.
Ethics Approval and Consent to Participate
This study is in line with the requirements of moral ethics. All participants signed informed consent. We confirm that all methods were carried out in accordance with the “cervical cancer clinical practice guidelines” from national comprehensive cancer network (NCCN) of the United States. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the Third Affiliated Hospital of Kunming Medical University.
Acknowledgments
We are thankful to the Yunnan Cancer Center for providing valuable investigation field and data resources for this research. We are grateful to all the staff and volunteers who participated in the data collection. We also thank all the patients with cervical lesions who participated in the face-to-face questionnaire survey for their active cooperation and strong support.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by grants from the Major Union Specific Project Foundation of Yunnan Provincial Science and Technology Department and Kunming Medical University (202201AY070001-167), Yunnan Cancer Hospital (The Third Affiliated Hospital of Kunming Medical University) General Subject of Undergraduate Education and Teaching Research of Teaching Union (JXYJ20230220), Innovative Research Team of Yunnan Province (202305AS350020), the Kunming Medical University Joint Special Project of Applied Basic Research, Science and Technology Department of Yunnan Province (202201AY070001-138), the Key Project of Basic Research, Science and Technology Department of Yunnan Province (202001AS070033), the National Cancer Center Oncology Research Program (NCC2017A33) and (NCC2017A34), the“Famous Doctor” Special Project of Ten Thousand People Plan of Yunnan Province (No.CZ0096) and Medical Leading Talents Training Program of Yunnan Provincial Health Commission (No.L-2019028). The funders had no role in the study design, decision to publish, or preparation of the manuscript.
Disclosure
The authors declare that there are no conflicts of interest.
References
1. Zhang S, Xu H, Zhang L, et al. Cervical cancer: epidemiology, risk factors and screening. Chin J Cancer Res. 2020;32(6):9. doi:10.21147/j.issn.1000-9604.2020.06.05
2. Tanjun L. A case-control study of risk factors associated with cervical cancer and precancerous lesions. Chin Drug Clin. 2018;18(S1):69–70.
3. Singh D, Vignat J, Lorenzoni V, et al. Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO global cervical cancer elimination initiative. Lancet Glob Health. 2023;11(2):e197–206. doi:10.1016/S2214-109X(22)00501-0
4. Jinyao W, Nianping Z, Zhiqiang B, et al. Age-period-cohort modeling analysis of long-term trends in cervical cancer incidence and mortality in China, 1993–2017. Chin Family Med. 2022;25(13):5. doi:10.12114/j.issn.1007-9572.2022.0074
5. National Bureau of Statistics. Bulletin on Main Data of the Sixth National Population Census in Yunnan Province in 2010. Available from: http://www.stats.gov.cn/tjsj/tjgb/rkpcgb/dfrkpcgb/201202/t20120228_30408.html.
6. Cun-Fen L. Analysis of human papillomavirus detection and characteristics of infected population in An Ning City. Laborat Med Clin. 2017;14(3):370–372.
7. Zhao M, Gu RY, Ding SR, et al. Risk factors of cervical cancer among ethnic minorities in Yunnan Province, China: a case-control study. Eur J Cancer Prev. 2022;31(3):287–292. doi:10.1097/CEJ.0000000000000704
8. Li N, Dai M. A multicenter cross-sectional study of human papillomavirus infection in Chinese women. Chin J Dis Cont. 2008;12(5):5.
9. Yu Q. Analysis of breast and cervical cancer screening in women and the factors influencing It. Chin Sci Technol J Datab. 2022;7:5.
10. Li X, Yang A-F, Du Z, et al. Analysis of pathogenic characteristics and preventive measures of combined genital tract infections in patients with cervical cancer. Chin J Hosp Infec. 2017;27(15):3544–3547.
11. Huang J-L. Analysis of the correlation between reproductive tract infection and cervical precancer and cervical cancer. Elect J Clin Med Literat. 2018;5(22):48.
12. Lin X. Research progress on the causes associated with urinary retention after radical cervical cancer surgery and clinical care. Chin Commu Phys. 2017;33(19):9–13.
13. Yan WJ. Study on the relationship between human papillomavirus and common pathogenic microbial infections in gynecology. Chin Mater Child Health Care. 2015;30(5):696–697.
14. Zhao J, Yang JH, Zhang WF, Li WG, Wang R. Meta-analysis of the correlation between mycoplasma, chlamydia and human papillomavirus infections in the female reproductive tract and cervical carcinogenesis in China from 2009 to 2020. J Tianjin Med Univ. 2021;27(04):396–400.
15. Panatto D, Amicizia D, Bianchi S, et al. Chlamydia trachomatis prevalence and chlamydial/HPV co-infection among HPV-unvaccinated young Italian females with normal cytology. Hum Vaccin Immunother. 2015;11(1):270. doi:10.4161/hv.36163
16. Zhu H, Shen Z, Luo H, et al. Chlamydia trachomatis infection-associated risk of cervical cancer: a meta-analysis. Medicine. 2016;95(13):e3077. doi:10.1097/MD.0000000000003077
17. Knowlton AE, Brown HM, Richards TS, et al. Chlamydia trachomatis infection causes mitotic spindle pole defects independently from its effects on centrosome amplification. Traffic. 2011;12(7):854. doi:10.1111/j.1600-0854.2011.01204.x
18. Bogani G, Sopracordevole F, Ciavattini A, et al. Duration of human papillomavirus persistence and its relationship with recurrent cervical dysplasia. Eur J Cancer Prev. 2023;32(6):525–532. doi:10.1097/CEJ.0000000000000822
19. Bogani G, Sopracordevole F, Ciavattini A, et al. HPV persistence after cervical surgical excision of high-grade cervical lesions. Cancer Cytopathol. 2023. doi:10.1002/cncy.22760
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.