Back to Journals » Drug Design, Development and Therapy » Volume 18
The Median Effective Dose of Intrathecal Hyperbaric Bupivacaine for Cesarean Section at Moderately High-Altitude
Authors Yang C , Dong W, Luo J, Ma M, Gao Y, Ni L, Liu H, Cha C, Xiao Y, Huang S
Received 17 January 2024
Accepted for publication 16 April 2024
Published 22 April 2024 Volume 2024:18 Pages 1313—1319
DOI https://doi.org/10.2147/DDDT.S455844
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Tin Wui Wong
Chen Yang,1,2,* Wangjun Dong,2,* Jianbo Luo,2 Mengzhao Ma,2 Yeyue Gao,2 Lijie Ni,2 Huixing Liu,2 Chengjun Cha,2 Yangli Xiao,2 Shaoqiang Huang1
1Department of Anesthesia, Obstetrics & Gynecology Hospital, Fudan University, Shanghai, People’s Republic of China; 2Department of Anesthesia, Yongping County People’s Hospital, Yunnan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Shaoqiang Huang, Department of Anesthesia, Obstetrics & Gynecology Hospital, Fudan University, 128# Shenyang Road, Shanghai, 200090, People’s Republic of China, Email [email protected]
Objective: Alterations in altitude can lead to an augmented requirement for local anesthesia among patients. Nevertheless, the necessity for an elevated dosage of local anesthetic for parturients at moderately high altitudes during spinal anesthesia for cesarean section remains uninvestigated. This up-down sequential study endeavors to determine the ED50 dose of bupivacaine required for spinal anesthesia during cesarean sections at moderately high-altitude.
Methods: Thirty singleton parturients at moderately high altitude underwent elective cesarean section under combined spinal-epidural anesthesia. The up-and-down sequential method was employed, starting with an initial dose of 12mg (1.6mL) of 0.75% hyperbaric bupivacaine for the first participant. The dose for the next case was adjusted up or down by 0.75mg based on the effectiveness of the previous participant. Effectiveness was defined as the bilateral sensory block reaching T6 within 15 minutes after spinal anesthesia injection, without the need for additional epidural anesthesia before fetal delivery. The ED50 dose and 95% confidence interval were calculated using the Dixon sequential method and isotonic regression, respectively. The incidence of maternal hypotension, nausea, and vomiting during the study period was also recorded.
Results: The ED50 of hyperbaric bupivacaine for spinal anesthesia in cesarean section was calculated as 8.23 mg (95% CI, 6.52– 9.32 mg) using the Dixon up-and-down method. Further validation using isotonic regression yielded a value of 8.39 mg (95% CI, 7.48– 9.30 mg), confirming the accuracy and sensitivity of the conclusion. During the operation, only 6 parturients experienced hypotension, and no adverse reactions such as nausea, vomiting, and shivering were observed.
Conclusion: The ED50 dose of 0.75% hyperbaric bupivacaine for spinal anesthesia during cesarean section at moderately high altitude is 8.23 mg, which exceeds the ED50 dose typically required by parturients at low altitude. Comprehensive investigations are warranted to ascertain the ED90 or ED95 dose of local anesthetics for cesarean section at moderately high altitudes, thereby offering enhanced guidance for clinical practice.
Keywords: bupivacaine, high altitude, spinal anesthesia, ED50 dose
Introduction
Pregnant women undergo specific physiological changes, including increased intra-abdominal pressure with advancing gestational weeks and reduced CSF volume in the lumbar region.1 The study identified ED50 estimates for motor block with intrathecal bupivacaine to be 6.9 mg in men and 5.2 mg in women undergoing limb surgery, and 3.4 mg in pregnant women undergoing cesarean delivery under combined spinal epidural block.2 These conclusions were all derived from data collected at low altitude.
The population residing in high-altitude regions experiences significant changes in respiratory, circulatory, and hematological systems due to variations in oxygen intake and delivery capacity.3 Long-term chronic hypoxia leads to increased cardiac output and cerebral blood flow, resulting in an elevated cerebrospinal fluid (CSF) volume. Additionally, excessive ventilation alters the acid-base balance of CSF, leading to lower pH values compared to individuals living at low- altitude.4,5 Study has shown that patients at high-altitude require longer onset time and achieve a lower maximum blockade level with spinal anesthesia compared to patients at low- altitude. Furthermore, they exhibit a higher demand for local anesthetics.6
Unfortunately, there is an absence of studies addressing cesarean deliveries in parturients at high-altitude. Insufficient local anesthetic dosage increases the risk of intraoperative pain, while excessive dosage significantly increases the incidence of spinal-induced hypotension (SIH).7 Therefore, a quantitative analysis of local anesthetic requirements for spinal anesthesia in high-altitude parturients undergoing cesarean section, along with further comparison to established low-altitude dosage data, is of significant clinical importance for the refinement of anesthetic protocols.
Consequently, we conducted a prospective sequential study to investigate the ED50 dose of bupivacaine for combined spinal epidural anesthesia in elective cesarean section at moderately high- altitude.
Materials and Methods
Study Design
This study was approved by the Ethics Committee of the Obstetrics and Gynecology Hospital of Fudan University(IRB2023-131) and People’s Hospital of Yongping County, Yunnan Province (ypxrmyy1120230001), registered in the Clinical Trial Registry Center (ChiCTR2300076935), and conducted at Yongping County People’s Hospital in Yunnan Province from October to December 2023, after obtaining informed consent from parturients. The study recruited singleton parturients undergoing elective cesarean section under Combined spinal- epidural anesthesia. The inclusion criteria were: age between 20 and 40 years, body mass index between 18–28 kg/m2, and living locally(altitude of 2000m). Exclusion criteria were: ASA > II, gestational age < 37 weeks, severe pregnancy complications, fetal or placental abnormalities such as premature rupture of membranes, intrauterine growth restriction, and contraindications to spinal anesthesia.
Study Procedure
The parturients including in the study received no preoperative medication. Demographic information, including height, weight, age, gestational weeks, parity, pregnancy complications, etc., was recorded upon entering the operation room. Routine monitoring included non-invasive blood pressure, pulse oximetry, and electrocardiogram monitoring. After the parturient assumed a left lateral position for 5 minutes, the average value of three consecutive measurements of blood pressure (BP) and heart rate (HR) was taken as the baseline value with a 1-minute interval between each measurement. All parturients in the study had an 18G intravenous catheter inserted into the peripheral vein of the upper limb. Combined spinal-epidural anesthesia was performed by a senior anesthesiologist who was not involved in the study, with the parturient in the left lateral position. The L3-L4 intervertebral space was punctured using a needle-in-needle technique, and a pre-determined dose of hyperbaric bupivacaine (3mL) was injected at a uniform speed after confirming the flow of cerebrospinal fluid. After the injection, 0.1 mL of cerebrospinal fluid (CSF) was aspirated back. If the CSF flow is clear, it indicated that the local anesthetic had entered the subarachnoid space, and the aspirated fluid was then injected back into the subarachnoid space. If CSF could not be aspirated smoothly, the parturient was excluded from the study, and the doctor in charge of anesthesia adjusted the medication according to the actual anesthetic effect. A 3–4 cm epidural catheter was inserted into the epidural space in a cephalad direction through the epidural needle. After confirming the absence of blood and cerebrospinal fluid, 3 mL of normal saline was used to rinse the catheter, and no epidural test dose was given. After the anesthesia was completed, the parturient returned to the left lateral by position 15 degrees left tilt of operating table, and oxygen flow at 5L/min was administered through a face mask. Lactated Ringer’s solution was infused intravenously at a dose of 10 mL/kg within 20–30 minutes, followed by a slow infusion to maintain venous patency.
The sensory block was bilaterally tested in each dermatomal level for loss to pinprick sensation every minute after spinal anesthesia. Surgery started when the sensory block level reached T6. If the sensory block level did not reach T6 after 15 minutes of spinal anesthesia or the parturient complained of pain despite reaching the T6 sensory block level before fetal delivery, additional lidocaine was administered epidurally to deepen and extend the sensory block level. Subsequent anesthesia management was carried out at the discretion of the anesthesiologist. The study continued from the time of drug administration into the subarachnoid space until fetal delivery.
During the study, the parturient’s blood pressure, heart rate, and blood oxygen saturation were recorded every 5 minutes, and adverse reactions such as nausea, vomiting, chills were noted. Hypotension was defined as a decrease in SBP of ≥20% from baseline or <90mmHg. Once hypotension occurred, intravenous injection of 50µg of ephedrine was administered for treatment. Bradycardia was defined as <50 beats/min, and intravenous injection of 0.5mg of atropine was given. Ondansetron (3mg) was administered intravenously for nausea and vomiting, and dexmedetomidine (10µg) was administered by drip for chills.
The up-and-down sequential method was used to find the ED50 of bupivacaine. Based on a previous review on dose of 0.75% hyperbaric bupivacaine for spinal anesthesia during cesarean section,8 the estimated ED50 dose ranged from 4.7 mg to 9.8 mg. Considering the higher dose estimation and the set dose change gradient of 0.75mg at high-altitude, the initial dose was set at 12mg (1.6mL) of 0.75% bupivacaine (H31022839, Shanghai Hefeng Pharmaceutical Co., Ltd.,) 0.5mL of 10% glucose solution, and diluted with preservative-free normal saline to 3mL. Effective anesthesia was defined as bilateral sensory block level at or above T6 within 15 minutes after spinal anesthesia, and no additional epidural anesthesia was required before fetal delivery. The dose of local anesthetic for the next parturient was determined based on whether the previous case was effective. If the local anesthetic dose was effective in the previous case, the dose for the next case was reduced by a gradient of 0.75mg. If it was ineffective, the dose for the next case increases by a gradient. If a parturient was excluded from the study, the dose for the next case remained unchanged.
The main outcome of the study was the ED50 of hyperbaric bupivacaine for spinal anesthesia. Secondary outcomes included the incidence of bradycardia, hypertension, hypotension, nausea, vomiting, and chills in parturients during the study period.
Statistical Analysis
The sample size of 30 parturients in each group was determined according to a previously published method, which indicated that 20–40 individuals were required to provide a stabilized estimation of the ED50 using the up-down allocation method.9 Additionally, according to prior studies, the sample size was regarded as sufficient when six pairs of reversals of sequence were obtained when the up-down allocation method was applied to evaluate the ED50.10 After 30 parturients were allocated, we also obtained more than six pairs of reversals of sequence. Thus, the sample size in the current study was sufficient to calculate the ED50.
Data analysis was performed using SPSS 22.0 (SPSS, Inc., Chicago, IL, USA) software. Data was presented as number (percentage), median (range), or mean ± SD, where appropriate. According to the statistical rules of the up-and-down sequential experiment, the cases before the first crossover point was excluded from the final statistical analysis. The Dixon up-and-down method and isotonic regression were used to calculate the ED50 and 95% confidence interval(CI). The Dixon up-and-down method is simple and intuitive, and its conclusion is the main result.11 Isotonic regression has the advantages of reducing bias and mean squared error, and is used to validate the accuracy and sensitivity of the main result.12 P<0.05 indicates statistical significance.
Results
A total of 30 parturients were approached for participation in the study(Figure 1). The parturients had a mean age of 29.07±4.15 years, gestational age of 38.25±1.48 weeks, height of 157.83±4.81 cm, and weight of 69.37±7.92 kg, including 12 primiparas and 18 multiparas. According to the rules of the up-and-down sequential trial, the cases before the first crossover were excluded, and the data of 28 parturients were included in the final statistical analysis.
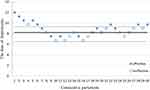 |
Figure 1 Sequences of effective and ineffective doses. As assessed using the Dixon up-down analysis the ED50 of hyperbaric bupivacaine was 8.23 mg (95% CI, 6.52–9.32 mg). |
The ED50 of hyperbaric bupivacaine was calculated as 8.23 mg (95% CI, 6.52–9.32 mg) using the Dixon up-and-down method. Further validation of the ED50 of hyperbaric bupivacaine was performed using isotonic regression, which yielded a value of 8.39 mg (95% CI, 7.48–9.30 mg).
The incidence of adverse reactions in the parturients during surgery was shown in Table 1. Six women experienced hypotension, while no cases of hypertension, bradycardia, nausea, vomiting, or shivering were observed.
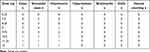 |
Table 1 Incidence of Intraoperative Adverse Reactions in Parturients |
Discussion
In the up-and-down sequential trial, we established the ED50 of hyperbaric bupivacaine for spinal anesthesia during cesarean section in parturients residing at moderately high-altitudes was 8.23 mg (95% CI, 6.52–9.32 mg). To our knowledge, this was the first study to investigate the effective dose for spinal anesthesia during cesarean section in parturients at moderately high-altitude.
We found 13 studies on the ED50 of bupivacaine for spinal anesthesia during cesarean section. Three of these studies reported the ED50 of bupivacaine at low altitude without opioids13–15, which were comparable to our findings. The altitude of the research sites, the intrathecal solution, the puncture segment and position, and the statistical methods used in the three studies were showed in Table 2. The trial sites were all located at low-altitude, and the reported ED50 of bupivacaine in the three studies were lower than that in our study based on intuitive data comparison.
 |
Table 2 Characteristics of Studies Examining ED50 of Intrathecal Bupivacaine for Cesarean Delivery |
One of the studies, by Xiao et al15 had a study design almost identical to ours (the puncture segment, the intrathecal solution, and the injection time were all consistent), and the cases were parturients living at low altitude region of China (Zhejiang Province). The study found that the ED50 of 0.75% hyperbaric bupivacaine for spinal anesthesia during cesarean section was 7.9 mg, which was significantly lower than that in our study. The only difference was 3 mL of saline injected to epidural space in our study. However, the minimum epidural saline volume that affects the level of sensory block under spinal anesthesia is 7.3 mL (95% CI, 5.5–9.9 mL).16 Therefore, the epidural administration of 3mL of saline does not have a significant effect on the results, and if it does, it is to reduce the dose of ED50,17 which narrow the difference in dose between the two studies.
The demographic characteristics of the parturients at moderately high -altitude were similar to those at low- altitude in terms of gestational age, weight, and age. The average height of parturients at moderately high-altitude was shorter than those at low-altitude. Height is a factor that affects the dose of local anesthetics, and the shorter the height, the less the dose of local anesthetics required.18 Therefore, the difference in requirement for anesthesia in parturients at moderately high- altitude of the same height may be more obvious. A randomized controlled trial comparing the outcomes of parturients at high-altitude and low-altitude is a prospective direction for our future research endeavors.
Previous study conducted a comparison of patients undergoing lower limb surgery at high-altitude versus low-altitude regions, employing spinal anesthesia.4 The results showed that compared with patients at moderately high-altitude (altitude of 1890 meters), patients at low- altitude (near sea level) had a shorter onset time of sensory and motor block, longer duration of block, and lower highest block level. It was inferred that patients at moderately high-altitude required more local anesthesia. Our conclusion just validated this inference.
The mechanism that patients at high-altitude need more local anesthetics is not yet fully understood. Long-term residence at high altitudes can cause physiological adaptations to sustain tissue oxygenation amid reduced ambient oxygen levels. These adaptive responses encompass augmented ventilation, heightened pulmonary arterial pressure,19 an accelerated heart rate, and a diminished stroke volume.20 Concomitant with the increase in hemoglobin concentration, there is an augmentation in red blood cell mass,3 a diminution in plasma volume, and a deceleration in blood flow velocity, while cerebral arterial blood flow and CSF volume rise.21,22 The CSF volume is an important factor affecting the demand for spinal anesthesia drugs. During spinal anesthesia, a larger CSF volume requires a greater dose of local anesthetic to achieve the same blockage level.23 Investigations have found that the density of cerebrospinal fluid is positively correlated with the peak level of sensory blockage, and the volume of lumbosacral cerebrospinal fluid is positively correlated with the onset time of motor blockage. Both the density and volume of CSF are determinants in the dissemination of spinal anesthesia, with the latter also bearing upon its duration.24,25 Additionally, acidification of CSF is a compensatory response to chronic respiratory alkalosis following increased ventilation. A lowered pH increases the amount of local anesthesia in the ionized cationic form, which should act as a potent blocker of sodium channels.26
The study found that blood pressure in patients significantly decreased 10 minutes after spinal administration,27 and 55% of patients experienced hypotension when the dose of hyperbaric bupivacaine exceeded 8 mg.28 In our study, the incidence of hypotension in parturient was 20%, and common adverse reactions such as nausea, vomiting, and shivering did not occur. However, in Xiao’s study,15 46% parturients experienced hypotension, and the incidence of related adverse reactions such as nausea and vomiting were 36%, and shivering was 14%. Previous studies have reported that patients at moderately high-altitude have higher mean arterial pressure values at baseline and intraoperation compared with patients at low- altitude.29 Chronic hypoxia leads to an increase in systemic arterial pressure, which is due to the significant activation of the sympathetic nervous system and adaptive changes in tissue hypoxia.30 Hypoxia also increases the secretion of renin in the body, activates the renin-angiotensin-aldosterone system, increases intraglomerular pressure, and raises mean arterial pressure.31 The higher incidence adverse reactions such as nausea and vomiting may be related to hypotension. Of course, due to the limit number of sequential trial cases, the incidence of adverse reactions may be biased and requires further analysis and comparison with a larger sample size.
There are some limitations in our study: First, there was no control group of women who lived in low- altitude area at the same time, although the comparable dose data of low- altitude area were searched, it was lack of statistical analysis and persuasive. It is necessary to make a further multi-center study on the comparison of local anesthetic dose between low-altitude and moderately high-altitude. Second, the ED90 obtained in the up-down sequential trial design may be biased, so the study only provided the ED50 dose, and exploring the ED90 dose has more clinical guidance significance. Third, due to the routine, there is no combination of opioids for spinal anesthesia in the study. There is no doubt that the ED50 of hyperbaric bupivacaine will be significantly reduced after the addition of opioids.
Conclusion
The ED50 of 0.75% hyperbaric bupivacaine for spinal anesthesia during cesarean section at moderately high-altitude is 8.23 mg, which is higher than the known ED50 required by parturient at low-altitude. Further research will determine the ED95 of spinal anesthesia for cesarean section at moderately high-altitude in order to better guide clinical practice.
Data Sharing Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics Approval
This trial was performed after receiving approval from the Ethics Committee of the Obstetrics and Gynecology Hospital of Fudan University (IRB2023-131) and People’s Hospital of Yongping County, Yunnan Province (ypxrmyy1120230001). This study was conducted in accordance with the declaration of Helsinki.
Acknowledgments
Chen Yang and Wangjun Dong are the co-first authors for this study. We would like to thank Wu Zhiyong expert grass-roots scientific research workstation for its support to the author Y.C.’s support work in Yunnan.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Ronenson AM, Sitkin SI. Effect of intra-abdominal pressure in pregnant women on level of spinal block and frequency of hypotension during cesarean section. Anesteziol Reanimatol. 2014;59(4):26–29. doi:10.18821/0201-7563-2014-59-4-26-29
2. Camorcia M, Capogna G, Columb MO. Effect of sex and pregnancy on the potency of intrathecal bupivacaine: determination of ED50 for motor block with the up–down sequential allocation method. Eur J Anaesthesiol. 2011;28(4):240–244. doi:10.1097/EJA.0b013e3283405163
3. Leissner KB, Mahmood FU. Physiology and pathophysiology at high altitude: considerations for the anesthesiologist. J Anesth. 2009;23(4):543–553. doi:10.1007/s00540-009-0787-7
4. Ainslie PN, Subudhi AW. Cerebral blood flow at high altitude. High Alt Med Biol. 2014;15(2):133–140. doi:10.1089/ham.2013.1138
5. Palmer BF. Physiology and pathophysiology with ascent to altitude. Am J Med Sci. 2010;340(1):69–77. doi:10.1097/MAJ.0b013e3181d3cdbe
6. Aksoy M, Ince I, Ahıskalıoglu A, Karaca O, Bayar F, Erdem AF. Spinal anaesthesia at low and moderately high altitudes: a comparison of anaesthetic parameters and hemodynamic changes. BMC Anesthesiol. 2015;15:123. doi:10.1186/s12871-015-0104-y
7. Helill SE, Sahile WA, Abdo RA, Wolde GD, Halil HM. The effects of isobaric and hyperbaric bupivacaine on maternal hemodynamic changes post spinal anesthesia for elective cesarean delivery: a prospective cohort study. PLoS One. 2019;14(12):e0226030. doi:10.1371/journal.pone.0226030
8. Tubog TD, Ramsey VL, Filler L, Bramble RS. Minimum Effective Dose (ED50 and ED95) of intrathecal hyperbaric bupivacaine for cesarean delivery: a systematic review. AANA J. 2018;86(5):348–360.
9. Pace NL, Stylianou MP. Advances in and limitations of up-and-down methodology: a précis of clinical use, study design, and dose estimation in anesthesia research. Anesthesiology. 2007;107(1):144–152. doi:10.1097/01.anes.0000267514.42592.2a
10. Jung H, Choi SC. Sequential method of estimating the LD50 using a modified up-and-down rule. J Biopharm Stat. 1994;4(1):19–30. doi:10.1080/10543409408835069
11. Dixon WJ. Staircase bioassay: the up-and-down method. Neuro sci Biobehav Rev. 1991;15(1):47–50. doi:10.1016/s0149-7634(05)80090-9
12. Stylianou M, Flournoy N. Dose finding using the biased coin up-and-down design and isotonic regression. Biometrics. 2002;58(1):171–177. doi:10.1111/j.0006-341x.2002.00171.x
13. Wang LZ, Zhang YF, Tang BL, Yao KZ. Effects of intrathecal and i.v. small-dose sufentanil on the median effective dose of intrathecal bupivacaine for Caesarean section. Br J Anaesth. 2007;98(6):792–796. doi:10.1093/bja/aem101
14. Geng ZY, Wang DX, Wu XM. Minimum effective local anesthetic dose of intrathecal hyperbaric ropivacaine and bupivacaine for cesarean section. Chin Med J. 2011;124(4):509–513. PMID: 21362272.
15. Xiao F, Drzymalski D, Liu L, Zhang Y, Wang L, Chen X. Comparison of the ED50 and ED95 of intrathecal bupivacaine in parturients undergoing cesarean delivery with or without prophylactic phenylephrine infusion: a prospective, double-blind study. Reg Anesth Pain Med. 2018;43(8):885–889. doi:10.1097/AAP.0000000000000850
16. Tyagi A, Kumar S, Salhotra R, Sethi AK. Minimum effective volume of normal saline for epidural volume extension. J Anaesthesiol Clin Pharmacol. 2014;30(2):228–232. doi:10.4103/0970-9185.130028
17. Lv M, Zhang P, Wang Z. ED50 of intrathecal ropivacaine for cesarean delivery with and without epidural volume extension with normal saline: a randomized controlled study. J Pain Res. 2018;11:2791–2796. doi:10.2147/JPR.S174176
18. She YJ, Liu WX, Wang LY, Ou XX, Liang HH, Lei DX. The impact of height on the spread of spinal anesthesia and stress response in parturients undergoing caesarean section: a prospective observational study. BMC Anesthesiol. 2021;21(1):298. doi:10.1186/s12871-021-01523-2
19. Penaloza D, Arias-Stella J. The heart and pulmonary circulation at high altitudes: healthy highlanders and chronic mountain sickness. Circulation. 2007;115:1132–1146.
20. Mallet RT, Burtscher J, Richalet JP, Millet GP, Burtscher M. Impact of high altitude on cardiovascular health: current perspectives. Vasc Health Risk Manag. 2021;17:317–335. doi:10.2147/VHRM.S294121
21. Feddersen B, Neupane P, Thanbichler F, et al. Regional differences in the cerebral blood flow velocity response to hypobaric hypoxia at high altitudes. J Cereb Blood Flow Metab. 2015;35(11):1846–1851. doi:10.1038/jcbfm.2015.142
22. Naeije R. Physiological adaptation of the cardiovascular system to high altitude. Prog Cardiovasc Dis. 2010;52(6):456–466. doi:10.1016/j.pcad.2010.03.004
23. Hocking G, Wildsmith JA. Intrathecal drug spread. Br J Anaesth. 2004;93:568–578. doi:10.1093/bja/aeh204
24. Higuchi H, Hirata J, Adachi Y, Kazama T. Influence of lumbosacral cerebrospinal fluid density, velocity, and volume on extent and duration of plain bupivacaine spinal anesthesia. Anesthesiology. 2004;100:106–114. doi:10.1097/00000542-200401000-00019
25. Carpenter RL, Hogan QH, Liu SS, Crane B, Moore J. Lumbosacral cerebrospinal fluid volume is the primary determinant of sensory block extent and duration during spinal anesthesia. Anesthesiology. 1998;89:24–29.
26. Hirabayashi Y, Shimizu R, Saitoh K, Fukuda H, Igarashi T. Acid-base state of cerebrospinal fluid during pregnancy and its effect on spread of spinal anaesthesia. Br J Anaesth. 1996;77(3):352–355. doi:10.1093/bja/77.3.352
27. Ferré F, Martin C, Bosch L, Kurrek M, Lairez O, Minville V. Control of spinal anesthesia-induced hypotension in adults. Local Reg Anesth. 2020;13:39–46. doi:10.2147/LRA.S240753
28. Zhang YF, Xiao F, Xu WP, Liu L. Prophylactic infusion of phenylephrine increases the median effective dose of intrathecal hyperbaric bupivacaine in cesarean section: a prospective randomized study. Medicine. 2018;97(32):e11833. doi:10.1097/MD.0000000000011833
29. Boushel R, Calbet JA, Rådegran G, Sondergaard H, Wagner PD, Saltin B. Parasympathetic neural activity accounts for the lowering of exercise heart rate at high altitude. Circulation. 2001;104:1785–1791. doi:10.1161/hc4001.097040
30. Calbet JA. Chronic hypoxia increases blood pressure and noradrenaline spillover in healthy humans. J Physiol. 2003;551:379–386. doi:10.1113/jphysiol.2003.045112
31. Stobdan T, Ali Z, Khan AP, et al. Polymorphisms of renin--angiotensin system genes as a risk factor for high-altitude pulmonary oedema. J Renin Angiotensin Aldosterone Syst. 2011;12(2):93–101. doi:10.1177/1470320310387177
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
