Back to Journals » Integrated Blood Pressure Control » Volume 16
The Magnitude of Hypertension and Its Contributing Factors Among Patients Receiving Antiretroviral Therapy in Public Hospitals in Harar City, Eastern Ethiopia: A Cross-Sectional Study
Authors Dechasa M , Nigussie S , Jambo A , Sime ML, Tamire A , Kitessa M , Degefu N , Dereje J , Demeke H, Legese N
Received 4 August 2023
Accepted for publication 3 November 2023
Published 11 November 2023 Volume 2023:16 Pages 81—93
DOI https://doi.org/10.2147/IBPC.S433907
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Turgay Celik
Mesay Dechasa,1 Shambel Nigussie,1 Abera Jambo,1 Mekdes Lueleseged Sime,2 Aklilu Tamire,3 Monas Kitessa,4 Natanim Degefu,5 Jerman Dereje,6 Henok Demeke,7 Nanati Legese7
1Department of Clinical Pharmacy, School of Pharmacy, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 2Department of Pharmacy, Hiwot Fana Comprehensive Specialized Hospital, Harar, Ethiopia; 3School of Public Health, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 4Department of Pharmacology, School of Pharmacy, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 5Department of Pharmaceutics, School of Pharmacy, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 6School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 7School of Pharmacy, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Correspondence: Mesay Dechasa, Department of Clinical Pharmacy, School of Pharmacy, College of Health and Medical Sciences, Haramaya University, P.O. Box 235, Harar, Ethiopia, Email [email protected]; [email protected]
Background: Although people living with HIV (PLHIV) are surviving longer due to the development of highly active antiretroviral therapy (HAART), hypertension continues to be a significant obstacle for human immunodeficiency virus (HIV) positive patients.
Purpose: This study aims to determine the prevalence of hypertension and its contributing factors among patients receiving HAART in public hospitals in Harar City, Eastern Ethiopia.
Patients and Methods: A hospital-based cross-sectional study was conducted among adult PLHIV who receive HAART in public hospitals in Harar City, Eastern Ethiopia, from 20 March to 14 April 2023. A simple random sampling technique was employed to select a total of 406 clients (382 participated in the study). Data were collected through patient interview and chart review using a questionnaire. The binary logistic regression was used for data analysis. The association was declared statistically significant at a p-value less than 0.05.
Results: The magnitude/prevalence of hypertension was 23% (95% CI: 19.1, 27.5) in study settings from a total of 382 adults who participated in this study. Factors significantly associated with hypertension in a multivariable binary logistic regression model include residence (rural residence, AOR = 1.95, 95% CI: 1.04, 3.65); body mass index (obese, AOR = 4.35, 95% CI: 1.08, 16.77); cigarette smoking (past cigarette smoking, AOR = 4.7, 95% CI: 1.10, 21.8); and HAART regimen change (AOR = 0.44, 95% CI: 0.20, 0.97).
Conclusion: The prevalence of hypertension observed among adult PLHIV in the study settings was high. Adults from rural areas, with a history of past smoking cigarette, and obesity need close attention during their clinic visits for more health education to reduce risk factors. The changed HAART regimen was associated with a reduced risk of hypertension. Generally, hypertensive PLHIV need consideration for their double burden of communicable and non-communicable diseases during disease management and hospital guideline development.
Keywords: hypertension, associated factors, people living with HIV, Eastern Ethiopia
Introduction
Hypertension, also known as high or raised blood pressure, is a condition in which the blood vessels have persistently raised pressure.1 Out of the 38.4 million people living with human immunodeficiency virus (PLHIV) globally in 2021, 36.7 million were adults 15 or more years of age.2 Sub-Saharan Africa is the most affected region, with 25.6 million people living with HIV in the region, sharing two-thirds of all cases worldwide.2 In Ethiopia, 722,248 people were living with HIV, of which approximately 23,000 were newly infected by annual AIDS-related deaths 11,000, and prevalence and incidence were 0.4% and 1%, respectively.3
Antiretroviral Therapy (ART) has contributed to significant progress in improving the longevity and quality of life of PLHIV; the treatment, however, is not without risk. The most frequent ART side effects are dyslipidemia and the associated elevated blood pressure, and there is well-established evidence that HIV-infected individuals who use ART have an increased risk of cardiovascular morbidity.4–6 In people living with HIV who receive ART, death results from cardiovascular complications such as hypertension related to the virus, host, and ART factors.5–8
Of all the comorbidities in PLHIV, hypertension appeared among the main causes of non-AIDS-related mortality.9 The prevalence of hypertension among PLHIV is 4.7–54.4% in high-income countries and 8.7–45.9% in low- and middle-income countries.10 Besides common behavioral and lifestyle-related risk factors, adult PLHIV had an additional risk of hypertension due to HIV infection and ART use. An increased risk of hypertension was observed to be related to combination therapy with Lamivudine and Tenofovir as opposed to Lamivudine and Zidovudine in a prospective cohort analysis of PLHIV without hypertension at baseline.11–13
The prevalence of hypertension by status of ART use varied significantly with PLHIV using ART having a higher prevalence compared to the ART naïve group: 27.1% versus 16.9%.14 A meta-analysis reported a global prevalence of hypertension among PLHIV to be 25.2% with a rate higher among the ART-experienced group (34.7%) versus the ART-naïve group (12.7%).15 Variation in the prevalence of hypertension among PLHIV who initiated ART was observed in different pocket studies in Ethiopia and elsewhere. For example, a study in southern Ethiopia in 2010 reported a prevalence of 15.9%.16 A hospital-based study in Harar, Eastern Ethiopia, estimated the prevalence of hypertension among PLHIV and diabetic patients at 12.7%.8
Few studies have demonstrated that ART has had a negative impact, even though the burden of non-communicable diseases, particularly hypertension, is high in people living with HIV/AIDS. Very few attempts have been made to date in Eastern Ethiopia, particularly in the study area to show the prevalence of hypertension and its causes in ART patients with diabetics.8 As a result, strategies to prevent hypertension among adult PLHIV received less attention. The focus on risk reduction among adult PLHIV who receive ART has not been applied to the diagnosis, prevention, or management of hypertension up to this point. Hence, this study aimed to assess the magnitude of hypertension and its associated factors among adult PLHIV receiving ART in public hospitals at Harari Regional State, Eastern Ethiopia.
The findings of this study will inform healthcare providers and bring to the attention of the regional health bureau the extent of hypertension among adult PLHIV for necessary action to be taken and for future planning on issues. In this regard, our study will also contribute to identifying factors associated with hypertension among this particular segment of the population and shed light on the associated prevention efforts. Finally, it may serve researchers as a baseline for further studies.
Materials and Methods
Study Design, Settings, and Period
A hospital-based cross-sectional study was conducted at Jugel General Hospital and Hiwot Fana Specialized University Hospitals in Harar City, Eastern Ethiopia. Harar is located 526 kilometres from Addis Ababa, the country’s capital city. The Harari Regional State’s total projected population, according to the 2007 Central Statistical Agency census report, is 183,415. There are two nonprofit hospitals and four government hospitals in the town. All of these facilities provided HAART, which was subsidized by the government, as part of their free HIV/AIDS care.17 The study period of this study was from March 20 to April 14, 2023.
Population
The source population are all adult PLHIV who received ART in Harari Regional State public hospitals. The study population was all adult PLHIV who had been receiving ART in public hospitals at Harari Regional State and who fulfilled inclusion criteria.
Inclusion and Exclusion Criteria
Adult PLHIV who are aged 18 years or more; current users of ART in the past 6 months before the survey; and lived in Harari regional state for at least 6 months were included in the study. Adult patients who are severely ill patients (cannot give a response) were excluded from the study.
Sample Size Determination
Sample size calculation considered a single population proportion formula for the prevalence estimate and a double population proportion for the second objective. The following parameters are considered to compute the sample size for the first objective: 95% confidence level, 5% margin of error, 12.7% prevalence of hypertension among PLHIV,7 and it resulted in a sample size of 170.
For the second objective, the duration of ART is used as a main exposure variable and assumed prevalence of hypertension among controls to be 8.2% and odds ratio of 2.3 for the exposure of ART for a duration above five years,7 with power of 80% and 95% confidence limit. Plugging the parameters in the following formula shown below, the resulting sample size is 486. We selected the sample size estimated for the second objective, which is higher than the 170 calculated for the first objective. Using a finite population proportion correction, the final sample estimate is 406.
Sampling Procedure/Technique
Based on the information obtained from the two hospitals, a total of 1112 adult PLHIV (500 and 612 patients were from HFCSH, and JGH, respectively) had regular follow at ART clinic one year before the study period at a similar period.
A simple random sampling technique was used to collect data from 406 adult HIV-positive patients from HFCSH (n = 223) and JGH (n = 182) of ART clinic follow-up using the list of patients from each hospital. Patients were recruited from each hospital based on the proportion of HIV/AIDS patients who flow to each hospital one year before the study period at that similar time.
Data Collection Methods
A data collection tool was developed following a review of previous literature guided by the study objectives.14,18,19 The data collection tool has sections covering socio-demographic characteristics, behavioral and lifestyle-related factors, and clinical variables. Data was collected by four nurses and a supervisor did a daily supervision of data collection. Data was collected using a face-to-face interview and by selecting the medical record patients from the registration manual of the ART clinic. After selecting the medical record number of patients, the chart was obtained from the medical record room. Then, the necessary information was extracted by using a data abstraction format.
Variables
Dependent Variable
A diagnosis of elevated blood pressure defining hypertension (≥140/90 mmHg).
Independent Variables
Socio-demographic variables include age, sex, education level, marital status, and occupation. Behavioral and biomedical variables include smoking status, alcohol use, insufficient fruit and vegetable consumption, and physical inactivity. Clinical variables include WHO stage, CD4 count, viral load count; and drug-related factors include current ART regimen, duration on ART, and adherence to ART medication.
Outcome Measurement
First, each hypertensive patient living with HIV was identified based on an evaluation of an average of 3 consecutive measurements by healthcare professionals during the same visit to ART clinics during their follow-up in both hospitals. Then, healthcare professionals recorded this information and we took recorded patients’ information from their charts. Finally, the magnitude of hypertension among patients receiving antiretroviral therapy in public hospitals in Harar City was measured by the percentage of total participants with a 95% confidence interval.
Data Quality Control
Data was collected using a pretested on 5% of sample size at Haramaya General Hospital. One-day training was also given for data collectors. Supervision was performed daily, and data was checked onsite for consistency and completeness.
Method of Data Analysis
The Epi-Data software (version 3.1) was used for data processing, and the Statistical Package for Social Science (SPSS®) (version 22.0) software was exploited for the data analysis. Descriptive data were presented using numerical summary measures for continuous variables in tables. Tables and graphs were also used to present categorical data. The percentage of hypertensive cases was computed from the total study subjects based on the definition used to define hypertension in clinical practice. A chi-square test was conducted to see a bi-variable correlation between different independent and dependent variables.
To identify factors associated with hypertension among adult PLHIV, bivariable and multivariable logistic regression analyses were conducted. In binary logistic regression, the variables having a p-value less than 0.25 were identified as a candidate for the multivariable analysis. Multicollinearity was checked by variance inflation factor and model goodness of fit was checked by Hosmer-Lemeshow before multivariate analysis. Then, the factors associated with hypertension were identified in the final model of analysis, and the statistical significance was declared at a p-value less than 0.05. The adjusted odds ratio with the corresponding 95% confidence interval was used to measure the strength of the association.
Operational Definitions
Hypertension: in this study, hypertension is defined as a blood pressure measure of systolic equal to or greater than 140 mmHg and/or diastolic equal to or greater than 90 mmHg.
Cigarette Smoker: A study participant is considered a cigarette smoker if he or she smokes now or has smoked cigarettes in the past, daily or less than daily.
Adherence to ART-: if he or she did not miss even a single dose of the prescribed regimens in the past month, as the refill time of study settings is monthly.
Results
Socio-Demographic Characteristics
A total of 382 adults who were using ART participated in this study with a response rate of 94.09%. Among them, 53.7% were females and the mean age of participants was 35.9 years with a 9.79 standard deviation (35.92 ± 9.79). In terms of marital status, 41.5% of the study participants were married adults. Less than a quarter, 22.3%, of the study participants were rural residents; and 51% of total respondents reported that they had a family income of less than 1500 Ethiopian Birr (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Patients Receiving Antiretroviral Therapy in Public Hospitals in Harar City, Harar, Eastern Ethiopia, 2023 (n = 382) |
The Prevalence of Hypertension
The prevalence of hypertension among current ART users was 23.0% (95% CI: 19.1, 27.5). The observed prevalence of hypertension was higher among males compared to females, 26% (95% CI: 20.0, 33.0) versus 20.5% (95% CI: 15.5, 26.6) (Figure 1).
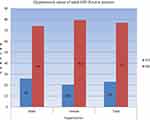 |
Figure 1 Prevalence of hypertension among patients receiving antiretroviral therapy in public hospitals in Harar City, Harar, Eastern Ethiopia, 2023. |
Of the total participants, 80.4% (307/382) had ever measured their blood pressure, and 19.6% (75/382) had never gotten their blood pressure measured. Of the total participants who never had measured their blood pressure, 18.7% (14/75) were identified with hypertension; and 24.1% (74/307) who ever had measured their blood pressure were identified with hypertension (Figure 2).
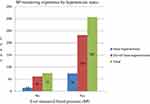 |
Figure 2 Hypertension status of adult people living with HIV and who were receiving antiretroviral therapy in public hospitals in Harar City, Harar, Eastern Ethiopia, 2023. |
Clinical and Behavioral Characteristics
Study participants who had been using ART for over 2 years constituted 55.2% of the study sample and the majority, 78.3%, had experienced regimen changes. AZT/3TC/DTG and AZT/3TC/EFV were the two common regimens that study participants were using during the study period, 32.1% versus 26.2%. Adherence to ART measured based on self-report, taking ART in the past seven days without interruption, was 74.4%. Thirteen percent of adult HIV-positive patients had a recent viral load copy over 1000/mL of blood and the majority, 64.1%, had viral copies within the range of 600 to 999 copies/mL. Regarding overweight and obesity based on body mass index measurement, 23.3% were overweight and 16.2% were obese. Moreover, 43.7% were physically inactive and 7.9% were current or past cigarette smokers. HAART regimen change, BMI status, and presence of opportunistic infections were associated with hypertension based on chi-square-test results (Table 2).
 |
Table 2 Clinical and Behavioral Characteristics by Hypertension Status Among Patients Receiving Antiretroviral Therapy in Public Hospitals in Harar City, Harar, Eastern Ethiopia, 2023 (n = 382) |
Factors Associated with Hypertension among HIV-Positive Patients
In the bivariable logistic regression, four factors were identified to have some association with hypertension among adult people living with HIV. These factors included residence, HAART regimen change, opportunistic infections, and body mass index. Except for the HAART regimen change, which was associated with a reduction in the odds of being hypertensive (COR = 0.53, 95% CI: 0.31, 0.91), the other three factors were shown to increase the odds of being hypertensive: rural residence (COR = 1.80, 95% CI: 1.05, 3.08); the presence of opportunistic infection (COR = 1.72, 95% CI: 1.07, 2.79); obesity (COR = 4.84, 95% CI: 1.31, 17.89) (Table 3).
 |
Table 3 Binary Logistic Regression Outputs for Factors Associated with Hypertension Among Patients Receiving ART in Public Hospitals in Harar City, Harar, Eastern Ethiopia, 2023 (n = 382) |
Factors in the bivariable model with a p-value of less than 0.25 were entered into the multivariable binary logistic regression model. In the multivariable binary logistic regression, the observed association between opportunistic infection and hypertension was lost. Otherwise, the observed associations for others were maintained with cigarette smoking showing up as an association in the multivariable model. Adult PLHIV who reside in rural areas had 1.95 times higher odds of being hypertensive compared to those who live in urban areas (adjusted odds ratio (AOR) = 1.95, 95% CI (confidence interval): 1.04, 3.65). Likewise, obese adults had 4.35 times higher odds of being hypertensive compared to underweight adults (AOR = 4.35, 95% CI: 1.08, 16.77). The association observed between hypertension and smoking status was only marginal where past cigarette smokers had 4.7 times higher odds of being hypertensive compared to never-smokers (AOR = 4.66, 95% CI: 1.00, 21.75). Regime change of the HAART medication had a protective association with hypertension among adults PLHIV (AOR = 0.44, 95% CI: 0.20, 0.97) (Table 4).
Discussion
The current healthcare system requires effective strategies to reduce the alarming burden of hypertension among PLHIV, particularly in developing countries, which face the double burden of communicable and non-communicable diseases.14 The current study aimed to estimate the extent of hypertension among adult people living with HIV and to identify the associated factors in public hospitals of Harar City, Eastern Ethiopia. The observed prevalence of hypertension in this study was 23% and four factors associated with hypertension in this particular population were identified. These factors included cigarette smoking, obesity, HAART regimen change, and rural residence.
The prevalence of hypertension among adult PLHIV was 23.0% (95% CI: 19.1, 27.5). A consistent result was reported in a systematic review that included 194 studies (conducted from 2007 to 2018) in 61 countries where the estimated global burden of hypertension was 23.6% with regional variations.14 For example, in western and central Europe, 28.1% of PLHIV had hypertension followed by 19.9% in eastern and southern Africa.20 In small pocket studies in eastern Africa, a higher prevalence was reported ranging from 26.2% in Tanzania21 to 29% in Uganda.20 In Ethiopia, different studies in the southern,22 eastern,8 and northwestern parts of the country19 reported a prevalence lower than that observed in the current study ranging from 12.7% to 15.9%. In contrast, a higher level was reported from northeastern Ethiopia with a value of 29.7%.23 The differences observed in the prevalence of hypertension among PLHIV in different parts of Ethiopia and settings other than Ethiopia could be due to differences in life risk factors including physical activity and the presence of comorbid conditions such as diabetes.
In this study, we did not find a significant association between both age and sex with the odds of hypertension among adults with PLHIV. Previous studies on the association between age and hypertension were mixed as Mateen et al reported that the distribution of hypertension was similar across age groups except men experienced a higher burden among older age groups compared to the younger, 18–39 years.24 Similarly, reports mounted that being a male adult and increasing in age is associated with hypertension.25,26 On the contrary, others reported that there was no difference in hypertension burden among men and women.27 There was a study that showed being female and age over the age of 45 years is associated with higher odds of hypertension among adult PLHIV.28 The younger population dominance in the current study where the average age was 35 years and 80.6% were below the age of 45 years may explain the inconsistency observed as this population could be physically more active.
The adult PLHIV residing in rural areas had 1.95 times higher odds of being hypertensive compared to those who live in urban areas (AOR = 1.95, 95% CI: 1.04, 3.65). Contrary to previous findings that urban residence was associated with hypertension;29 our study report indicated that rural residence is associated with hypertension. This might be explained by that HIV-associated stigma could be more pronounced and induce more among adult HIV-positive patients, thereby increasing blood pressure.
In the current finding, BMI is associated with hypertension and in obese adults PLHIV had 4.35 times higher odds of being hypertensive compared to underweight adult patients (AOR = 4.35, 95% CI: 1.08, 16.77). This finding is consistent with previous reports from low- and middle-income countries.29 An increase in BMI (from overweight to obesity) is reported to be a three to seven-fold increase in the risk of hypertension.30 The underlying pathophysiological mechanism for the link between changes in BMI and blood pressure was not clear31 except that weight gain stimulates sympathetic activation and also the renin-angiotensin system linking body weight and blood pressure.32,33
The research evidence on the association between cigarette smoking and elevated blood pressure was mixed, our finding on this was against some reports and also consistent with others which reported that past cigarette smokers had 4.7 times higher odds of being hypertensive compared to nonsmokers (AOR = 4.66, 95% CI: 1.00, 21.75). For example, in a 30-year prospective longitudinal study, cigarette smoking was reported to increase pulse pressure in younger adults but not systolic blood pressure.34 There are similar reports from previous research evidence that blood pressure did not differ between smokers (both current and former) and non-smokers.35,36 A global meta-analysis revealed that the association between smoking cigarettes with hypertension was varied by geographies studied where it showed a significant association in Asia, the Pacific, and sub-Saharan Africa but not in Europe and the Americas.29 While the conventional risk factors are shared between HIV-infected and non-infected adults, there is an additional effect of HIV infection as evidenced in previous reports.37 Though we did not claim a causal link, the observed association between smoking and hypertension status in our study might be confounded by the HIV status.
Regime change of the HAART medication was associated with a 56% reduction in the odds of being identified with hypertension among adults in PLHIV (AOR = 0.44, 95% CI: 0.20, 0.97) present study. Similarly, variations in the effect of ART on hypertension were also observed from another study by the types of ART used. For example, the Efavirenz-based regimen had a reduced risk of hypertension compared to the o Nevirapine-based regimen.20 Besides the effect of HIV infection on blood pressure, our report consistently supports the effect of ART on the increase in blood pressure as evidenced by a study on the pathophysiologic mechanism of hypertension in HIV-infected adults.37 ART was implicated in inducing mechanisms related to hypertension including renin-angiotensin activation, immune reconstitution, lipodystrophy, endothelial dysfunction and stiffness, and dyslipidemia and adipokines.37
Limitations of the Study
Our study estimated the burden of hypertension and the associated factors which were often explored in adult PLHIV. However, it was not without limitations: first, since this study is a cross-sectional study, it cannot establish causal relationships. Second, the study participants are combination drug users to treat patient conditions and the effects of drugs may over or underestimate the magnitude of hypertension and should be interpreted with causation. Third, this study did not include individual ART regimens in the logistic model and it cannot show whether the individual ART regimen has an association with hypertension or not. Thus, the authors recommend further studies with stronger study design by addressing these limitations.
Conclusion
The prevalence of hypertension among adult PLHIV was high in the study settings. Adults from rural areas, past cigarette smokers, and obese patients need close attention during their clinic visits for more health education to reduce risk factors. The changed HAART regimen is associated with a reduced risk of hypertension, and clinicians could use it to inform patients when discussing adverse effects. Generally, a nationwide study with a stronger design regarding these specific populations is urgently needed to give attention to national guideline development and policy making.
Abbreviations
AIDS, Acquired Immunodeficiency Syndrome; ART, Antiretroviral Therapy; BMI, Body Mass Index; HAART, Highly Active Antiretroviral Therapy; HFCSH, Hiwot Fana Comprehensive Specialized Hospital; HIV, Human Immunodeficiency Virus; JGH, Jugel General Hospital; PLHIV, People Living with HIV.
Data Sharing Statement
All data generated or analyzed during this study are included in this manuscript. Data collection tools and raw data can be accessible upon request from the authors.
Ethics Approval and Consent to Participate
An ethical clearance letter was obtained from Haramaya University, College of Health and Medical Sciences, Institutional Health Research Ethics Review Committee (IHRERC) with the reference number of IHRERC/145/2023 and the study complies with the Declaration of Helsinki. In addition, permission was sought from the respective managers of each hospital to conduct the study. Informed, volunteer and written consent were obtained from participants and the head of each hospital before data collection. Confidentiality was secured through coding of the questionnaire without writing the names of patients and they got a right to stop participation in the study at any time.
Acknowledgments
Firstly, we would like to give special thanks to all our friends for their kindness and moral support through proposal development to finalizing this research. Secondly, we appreciate the data collectors who showed the utmost effort in acquiring appropriate information. Lastly, we want to give special gratitude to the study participants and all staff members of the study settings for their cooperation during data collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Brouwers S, Sudano I, Kokubo Y, Sulaica EM. Arterial hypertension. Lancet. 2021;398(10296):249–261. doi:10.1016/S0140-6736(21)00221-X
2. Laelago T, Yohannes T, Lemango F. Prevalence of herbal medicine use and associated factors among pregnant women attending antenatal care at public health facilities in Hossana Town, Southern Ethiopia: facility based cross-sectional study. Arch Public Health. 2016;74(1):1–8. doi:10.1186/s13690-015-0113-9
3. Kibret GD, Ferede A, Leshargie CT, Wagnew F, Ketema DB, Alebel A. Trends and spatial distributions of HIV prevalence in Ethiopia. Infect Dis Poverty. 2019;8(1):90. doi:10.1186/s40249-019-0594-9
4. Grover SA, Coupal L, Gilmore N, Mukherjee J. Impact of dyslipidemia associated with Highly Active Antiretroviral Therapy (HAART) on cardiovascular risk and life expectancy. Am J Cardiol. 2005;95(5):586–591. doi:10.1016/j.amjcard.2004.11.004
5. Rhee MS, Hellinger JA, Sheble-Hall S, Cohen CJ, Greenblatt DJ. Relationship Between Plasma Protease Inhibitor Concentrations and Lipid Elevations in HIV Patients on a Double-Boosted Protease Inhibitor Regimen (Saquinavir/Lopinavir/Ritonavir). J Clin Pharmacol. 2010;50(4):392–400. doi:10.1177/0091270009339739
6. Shahmanesh M, Jaleel H, DeSilva Y, Ross JDC, Caslake M, Cramb R. Protease inhibitor-related to type III hyperlipoproteinemia is common and not associated with apolipoprotein-E E2/E2 phenotype. Sex Transm Infect. 2001;77(4):283. doi:10.1136/sti.77.4.283
7. Ataro Z, Ashenafi W, Fayera J, Abdosh T. Magnitude and associated factors of diabetes mellitus and hypertension among adult HIV-positive individuals receiving highly active antiretroviral therapy at Jugal Hospital, Harar, Ethiopia. HIV/AIDS-Res Palliat Care. 2018:181–92. (Print). doi”:10.2147/HIV.S176877
8. Ataro Z, Ashenafi W, Fayera J, Abdosh T. Magnitude and associated factors of diabetes mellitus and hypertension among adult HIV-positive individuals receiving highly active antiretroviral therapy at Jugal Hospital, Harar, Ethiopia. HIV/AIDS. 2018;10:181–192.
9. Sackoff JE, Hanna DB, Pfeiffer MR, Torian LV. Causes of death among persons with AIDS in the era of highly active antiretroviral therapy: new York City. Ann Intern Med. 2006;145(6):397–406. doi:10.7326/0003-4819-145-6-200609190-00003
10. Nguyen KA, Peer N, Mills EJ, Kengne AP. Burden, determinants, and pharmacological management of hypertension in HIV-positive patients and populations: a systematic narrative review. AIDS Rev. 2015;17(2):83–95.
11. Cherfan M, Vallée A, Kab S, et al. Unhealthy behaviours and risk of uncontrolled hypertension among treated individuals-The CONSTANCES population-based study. Sci Rep. 2020;10(1):1925.
12. Odukoya O, Badejo O, Sodeinde K, Olubodun T. Behavioral risk factors for hypertension among adults living with HIV accessing care in secondary health facilities in Lagos State, Nigeria. J Fam Med Prim Care. 2020;9(7):3450. doi:10.4103/jfmpc.jfmpc_544_20
13. Rajkumar E, Romate J. Behavioural risk factors, hypertension knowledge, and hypertension in rural India. Int J Hypertens. 2020;2020:8108202. doi:10.1155/2020/8108202
14. Bigna JJ, Ndoadoumgue AL, Nansseu JR, et al. Global burden of hypertension among people living with HIV in the era of increased life expectancy: a systematic review and meta-analysis. J Hypertens. 2020;38(9):1659–1668. doi:10.1097/HJH.0000000000002446
15. Xu Y, Chen X, Wang K. Global prevalence of hypertension among people living with HIV: a systematic review and meta-analysis. J Am J Hypertens. 2017;11(8):530–540. doi:10.1016/j.jash.2017.06.004
16. Sachithananthan V, Loha E, Gose M. Prevalence of diabetes mellitus, hypertension, and lipodystrophy in HAART receiving HIV patients in Southern Ethiopia. Int STD Res Rev. 2013;1(1):11. doi:10.9734/ISRR/2013/1897
17. Shama AT, Roba HS, Abaerei AA, Gebremeskel TG, Baraki N. Assessment of quality of routine health information system data and associated factors among departments in public health facilities of Harari region, Ethiopia. BMC Med Inform Decis Mak. 2021;21(1):1–12. doi:10.1186/s12911-021-01651-2
18. Pangmekeh PJ, Awolu MM, Gustave S, Gladys T, Cumber SN. Association between highly active antiretroviral therapy (HAART) and hypertension in persons living with HIV/AIDS at the Bamenda regional hospital, Cameroon. Pan Afr Med J. 2019;33:87.
19. Gebrie A. Hypertension among people living with human immunodeficiency virus receiving care at referral hospitals of Northwest Ethiopia: a cross-sectional study. PLoS One. 2020;15(8):e0238114. doi:10.1371/journal.pone.0238114
20. Lubega G, Mayanja B, Lutaakome J, Abaasa A, Thomson R, Linden C. Prevalence and factors associated with hypertension among people living with HIV/AIDS on antiretroviral therapy in Uganda. Pan Afr Med J. 2021;38(1). doi:10.11604/pamj.2021.38.216.28034
21. Kagaruki GB, Mayige MT, Ngadaya ES, et al. Magnitude and risk factors of non-communicable diseases among people living with HIV in Tanzania: across-sectional study from Mbeya and Dar es Salaam regions. BMC Public Health. 2014;14(1):1–9. doi:10.1186/1471-2458-14-904
22. Sachithananthan V, Loha E, Gose M. Prevalence of diabetes mellitus, hypertension, and lipodystrophy in HAART receiving HIV patients in Southern Ethiopia. Methodology. 2009;2010:1–11.
23. Fiseha T, Belete AG, Dereje H, Dires A. Hypertension in HIV-infected patients receiving antiretroviral therapy in Northeast Ethiopia. Int J Hypertens. 2019;2019:1–7. doi:10.1155/2019/4103604
24. Mateen FJ, Kanters S, Kalyesubula R, et al. Hypertension prevalence and Framingham risk score stratification in a large HIV-positive cohort in Uganda. J Hypertens. 2013;31(7):1372–1378. doi:10.1097/HJH.0b013e328360de1c
25. Denue BA, Muazu PJ, Gashau W, Nkami D, Ajayi NA. Effects of highly active antiretroviral therapy (HAART) on blood pressure changes and its associated factors in HAART naive HIV-infected patients in northeastern Nigeria. Arch Appl Sci Res. 2012;4(3):1447–1452.
26. de Arruda Junior ER, Lacerda HR, Moura LCRV, et al. Risk factors related to hypertension among patients in a cohort living with HIV/AIDS. Braz J Infect Dis. 2010;14(3):281–287. doi:10.1016/S1413-8670(10)70057-X
27. Medina-Torne S, Ganesan A, Barahona I, Crum-Cianflone NF. Hypertension is common among HIV-infected persons, but not associated with HAART. J Int Assoc Physicians AIDS Care. 2012;11(1):20–25. doi:10.1177/1545109711418361
28. Chiwandire N, Zungu N, Mabaso M, Chasela C. Trends, prevalence and factors associated with hypertension and diabetes among South African adults living with HIV, 2005–2017. BMC Public Health. 2021;21(1):1–14. doi:10.1186/s12889-021-10502-8
29. Sarki AM, Nduka CU, Stranges S, Kandala N-B, Uthman OA. Prevalence of hypertension in low-and middle-income countries: a systematic review and meta-analysis. Medicine. 2015;94(50):e1959. doi:10.1097/MD.0000000000001959
30. A-l L, Peng Q, Shao Y-Q, Fang X, Zhang Y-Y. The effect of body mass index and its interaction with a family history on hypertension: a case-control study. Clin Hypertens. 2019;25:1–8. doi:10.1186/s40885-018-0104-6
31. Drøyvold W, Midthjell K, Nilsen T, Holmen J. Change in body mass index and its impact on blood pressure: a prospective population study. Int J Obes. 2005;29(6):650–655. doi:10.1038/sj.ijo.0802944
32. Masuo K, Mikami H, Ogihara T, Tuck ML. Weight gain–induced blood pressure elevation. Hypertension. 2000;35(5):1135–1140. doi:10.1161/01.HYP.35.5.1135
33. Hall J, Brands M, Hildebrandt D, Kuo J, Fitzgerald S. Role of the sympathetic nervous system and neuropeptides in obesity hypertension. Braz J Med Biol. 2000;33:605–618. doi:10.1590/S0100-879X2000000600001
34. Luehrs RE, Zhang D, Pierce GL, Jacobs DR Jr, Kalhan R, Whitaker KM. Cigarette smoking and longitudinal associations with blood pressure: the CARDIA Study. J Am Heart Assoc. 2021;10(9):e019566. doi:10.1161/JAHA.120.019566
35. Lan R, Bulsara MK, Pant PD, Wallace HJ. Relationship between cigarette smoking and blood pressure in adults in Nepal: a population-based cross-sectional study. PLOS Global Public Health. 2021;1(11):e0000045. doi:10.1371/journal.pgph.0000045
36. Allen C, Mbonye M, Seeley J, et al. ABC for people with HIV: responses to sexual behavior recommendations among people receiving antiretroviral therapy in Jinja, Uganda. Cult Health Sex. 2011;13(05):529–543. doi:10.1080/13691058.2011.558593
37. Fahme SA, Bloomfield GS, Peck R. Hypertension in HIV-infected adults: novel pathophysiologic mechanisms. Hypertension. 2018;72(1):44–55. doi:10.1161/HYPERTENSIONAHA.118.10893
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

