Back to Journals » Integrated Pharmacy Research and Practice » Volume 12
The Extent of Antibiotic Dispensing in Self-Medication Encounters in Sudan: A Simulated Patient Study Focusing on Cefixime Sale
Authors Hamadouk RM , Alshareif EM, Ibrahim OM, Albashair ED , Yousef BA
Received 13 September 2023
Accepted for publication 18 November 2023
Published 24 November 2023 Volume 2023:12 Pages 227—237
DOI https://doi.org/10.2147/IPRP.S440010
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Walid Al-Qerem
Riham M Hamadouk,1,2 Einass M Alshareif,1 Omnia M Ibrahim,3 Esra D Albashair,1 Bashir A Yousef4
1Department of Clinical Pharmacy, Faculty of Pharmacy, University of Khartoum, Khartoum, Sudan; 2Department of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmacy, Almughtaribeen University, Khartoum, Sudan; 3Faculty of Pharmacy, Al-Neelain University, Khartoum, Sudan; 4Department of Pharmacology, Faculty of Pharmacy, University of Khartoum, Khartoum, Sudan
Correspondence: Bashir A Yousef, Department of Pharmacology, Faculty of Pharmacy, University of Khartoum, Al-Qasr Ave, Khartoum, 11111, Sudan, Tel +249155662037, Fax +249183780696, Email [email protected]
Background: Antibiotics play an important role in decreasing morbidity and mortality worldwide. However, inappropriate use of them by patients or healthcare professionals contributes to their resistance rendering them less efficacious. Community pharmacists (CPs) have a significant part in reducing antibiotic resistance. Therefore, this study aimed to investigate the dispensing of antibiotics without prescription in community pharmacies with an emphasis on cefixime dispensing.
Methods: A cross-sectional, simulated patient (SP) study was conducted in the Khartoum locality. A total of 238 community pharmacies were randomly chosen using simple random sampling. One scenario of uncomplicated urinary tract infection was designed, and six female pharmacy students who were trained to act as SPs presented the scenario. Descriptive statistics were applied to report the study outcomes.
Results: In the 238 pharmacy visits, at least one antibiotic was dispensed without a prescription in 69.3% of the simulated visits. Among the dispensed antibiotics, ciprofloxacin was the most dispensed antibiotic followed by cefixime representing 51.5% and 41.8%, respectively, of total dispensed antibiotics. Cefixime was dispensed as a first choice by CPs in 29% of the visits, and in the rest of the visits, only 37.3% of CPs refused to dispense cefixime after SP demand.
Conclusion: The findings revealed a high rate of antibiotics dispensing without prescription by CPs in Khartoum state, and cefixime was obtained with ease before and after the patient’s demand. Urgent corrective actions such as imposing strict regulations, monitoring pharmacists’ practice, and endorsing educational programs for pharmacists are needed to prevent inappropriate antibiotic dispensing practices.
Keywords: antibiotics, cefixime, community pharmacists, simulated patient, self-medication
Introduction
Since their discovery in the 20th century, antibiotics have contributed significantly to the decrease in morbidity and mortality in diseases caused by microorganisms.1 Their importance can be noticed more in developing countries, where the leading causes of death are infectious diseases.2 The countless lives that have been saved by antibiotics reflect the significance of these drugs, and because no new generations of antibiotics have been developed, appropriate use of them is essential to ensure effective treatment for infectious diseases.3
The global expansion of antibiotic use has been accompanied by the rapid and ongoing spread of antimicrobial resistance.1 The World Health Organization (WHO) stated that around 35% of human infections are resistant to the existing antimicrobials, and unfortunately in low- and middle-income countries the resistance rate is even higher, almost up to 90%.4 The major cause of antimicrobial resistance is the inappropriate use of antibiotics, through unnecessary prescribing by healthcare providers, or patient self-medication.5 It is known that self-medication puts patients at the hazard of adverse drug reactions, inappropriate dosing, incorrect self-diagnosis, inadequate treatment of a disease, and incomplete treatment courses which all lead to serious harmful results, and one of them is antimicrobial resistance.6
Alongside antimicrobial resistance, inappropriate use of antibiotics has other consequences including increased incidence of antibiotics adverse reactions and increased healthcare-associated costs.6 Many studies showed that the spread of antibiotic resistance is strongly affected by the dispensing of antibiotics without prescription and self-medication.7,8 Moreover, a systematic review study estimated that 62% of antibiotic sales were without prescription worldwide.9
Cefixime is a semisynthetic third-generation cephalosporin, and it is useful in treating many bacterial infections including urinary tract infections, pneumonia, tonsillitis, otitis media, Lyme disease, and gonorrhea.10 Thus, physicians prescribe it as a first-line choice against a diversity of common infections encountered.11 It is considered one of the important oral antibiotics owing to its extreme stability in the presence of β-lactamase enzymes. It is superior to aminopenicillins and the orally administered first-generation cephalosporins in β-lactamase stability, therefore it can be used in treating infections caused by organisms resistant to them.12 Cefixime is one of the antibiotics that has been noticed to be dispensed without prescriptions.13
Community pharmacists (CPs) are the healthcare members whom people approach when they need medical and wellness advice. They are in a unique position that allows them to reduce antibiotic resistance as they can advise patients to supply prescriptions for antibiotics or provide information about antibiotic resistance.14 Further, global self-medication has become a growing issue in CPs’ daily counseling practice,15 providing appropriate over-the-counter drugs, or non-pharmacological treatments, and referring the patient to a physician are appropriate actions that can be taken by community pharmacists in managing common infections during counseling self-medicated patients.16
While the practice of dispensing antibiotics without prescription is very rare in Western countries, it is a major concern in low- and middle-income countries.17 Several studies have reported the frequent provision of antibiotics without prescription. In a study from Saudi Arabia, 97.9% of the community pharmacists in the study recommended antibiotics for patients or dispensed antibiotics upon patients’ request, even though this practice is against the country’s laws and regulations.18 Also, in Pakistan despite the legislation, the dispensing of antibiotics without prescription is still common.19 These studies used the simulated patient technique.
The simulated patients technique has been used since the 1940s to evaluate service quality and is frequently used to assess many aspects of pharmacy practice due to its advantages over other assessment strategies. Basically, it involves an individual who trained to deliver a certain scenario which is previously prepared to present a particular condition to be investigated.20
In Sudan, one study explored the knowledge, attitude, and practice of community pharmacists regarding dispensing antibiotics without prescriptions,21 and another explored the reasons for this improper practice,22 but none of them investigated the actual practice of CPs. Further, in part of Sudan, it was found that the prevalence of self-medication is high, and those with lower incomes appeared more predisposed to self-medicate as they cannot afford to consult medical practitioners.23 Therefore, this study aimed to investigate the dispensing of antibiotics without prescription in community pharmacies with an emphasis on cefixime sales.
Methods
Study Design
A cross-sectional design was used in this study to investigate the practice of CPs in dispensing antibiotics in general and cefixime specifically without prescription in Khartoum locality. The study is following the STROBE statement that must be included in reports of cross-sectional studies. The STROBE Statement is a checklist designed to provide guidance on the method of reporting observational research, it contains 22 items that considered fundamental for good reporting of observational studies.24
The simulated patient (SP) method was applied in this study as it is an internationally well-accepted effective method for evaluating community pharmacists’ professional performance.20 The main justification for using this approach is minimizing the Hawthorne effect (changing behavior upon awareness of observation).25
Scenario Details
One scenario was designed by the authors in consultation with a pharmacy practice educationalist. The content of this scenario was validated by showing it to four members of the University of Khartoum, two pharmacists specialized in clinical pharmacy and pharmacy practice, and two physicians. The scenario was a case of uncomplicated urinary tract infection (Cystitis). The simulated patients were females, as females are more prone to urinary tract infection,26 she will complain to the pharmacist that she has discomfort with urination with a burning sensation and the need to urinate more frequently and the symptoms started yesterday. If the pharmacist asked about other symptoms that indicate referral-like fever, nausea/vomiting, loin pain or tenderness, blood in the urine, vaginal discharge, or pregnancy, the simulated patient will reply that she did not experience any of them.
Initially, the SP will present the symptoms and ask the pharmacist if something could be given to alleviate them, the medications that will be dispensed will be documented (either antibiotics or other medications). Then, regardless of the medication/antibiotic that is given except for cefixime, the simulated patient will tell the pharmacists that this medication is not very strong and request specifically for cefixime and insist. The response of the pharmacists toward the patients’ demand will be recorded. Figure 1 demonstrates the flowchart of the SP visit and action.
 |
Figure 1 The flowchart of the simulated patient visit and process. |
Sample Size and Sampling
A list containing all registered community pharmacies in the Khartoum locality was obtained from The Sudanese General Directorate of Pharmacy, from which we select the community pharmacies included in this study. Two hundred thirty-eight community pharmacies were the sample size obtained by using the formula n = N/1 + N(e)2, where N is the study population which was 587 pharmacies, and (e) an error margin of 0.05, the formula is based on a degree of variability (p) of 0.5, and a 95% confidence interval. A simple random sampling technique was performed to select the community pharmacies in this study.
Data Collection Form
The authors designed a data collection form specifically for this study to record the information collected during the simulated visits. The form consists of two parts, the first contains three questions regarding the response of the CP to the scenario. The second part contains questions pertaining to the response of the CP when the patient requests cefixime (Table 1). The data collection form was approved by three faculty members in the Faculty of Pharmacy University of Khartoum, who had excellent experiences in pharmacy practice. Further, to test the validity of the data collection form, it has been piloted in thirty community pharmacies.
 |
Table 1 The Data Collection Form |
Data Collection
To carry out this study, six fourth-year female students from the Faculty of Pharmacy agreed to act as simulated patients (SPs), and to keep the confidentiality of the study written informed consents were obtained from the participants in which they agreed to keep the simulated patient, training sessions, and the simulated scenario confidential. All collected information will remain confidential to the research team, and they will not use or disclose any confidential data to any third party before, during, or after the study.
The principles of the methodology were well explained to them, and they were trained for two weeks to familiarize themselves with the scenario. Also, several rehearsals were performed under the supervision of a physician to ensure consistency in the illness simulation. After that, a pilot study was conducted to ensure the abilities of the SPs in performing the scenario and to check the appropriateness of the data collection form. Thirty community pharmacies were visited as each SP has visited five pharmacies, these pharmacies and the data collected from them were excluded from the study. Each SP was handled a list contains the names and locations of the pharmacies assigned to her. The list also includes five extra pharmacies named as alternatives which were chosen randomly prior to the study. These alternatives were listed to replace the pharmacies understudy in case the SP was recognized by any member of the pharmacy staff, or if the pharmacy that was selected for the study was going out of business.
The study visits were conducted between November 2022 and January 2023. All the SPs approached the pharmacies only after ensuring that they were empty and requested a pharmacist before starting the simulation as the study targeted only pharmacists. Five SPs made 40 visits and one made 38 to end up with 238 pharmacy visits. Immediately after leaving each pharmacy, the SP recorded the obtained information on a paper data collection form, thus minimizing the recall bias and to ensure that the simulation was not observed by pharmacy staff.
Data Management and Analysis
The data were analyzed using Statistical Package for Social Sciences software, version 26.0 (IBM SPSS Inc., Chicago, IL). The main outcome was the percentage of antibiotics in general and cefixime precisely that dispensed without prescriptions. Descriptive statistics were applied to describe community pharmacists’ demographic characteristics and their responses to the scenario. The results were presented as tables containing frequencies and percentages. The relationship between variables was tested using an appropriate statistical method (the Chi-square test) with a p-value of less than 0.05 being considered statistically significant.
Ethical Approval
The study was approved by the Ethical Committee of the Faculty of Pharmacy, University of Khartoum, Khartoum, Sudan (FPEC-19-2022). Additional approval was obtained from the scientific research authority Ministry of Health and The Sudanese General Directorate of Pharmacy. Written informed consent was collected from all community pharmacists involved in the study, and to protect the integrity of the design the informed consent was obtained two months prior to the study. It informed CPs that their dispensing practice will be assessed in an observational study, the name of the study and the method of the assessment kept hidden from them. Fortunately, all CPs accepted to participate in the study. Confidentiality was ensured throughout the study.
Results
Demographic Characteristics of the Community Pharmacists
All the planned visits were completed resulting in 238 visits. The majority of the CPs were female (64.7%), and the predominant age category was 26–30 years old representing (43.3%) of the study population. A bachelor’s degree was the highest qualification of the majority of the CPs (84.9%), while most of them (57.6%) had experience as community pharmacists for 2 to 5 years. The rest of the pharmacists’ characteristics are reported in Table 2.
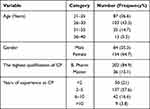 |
Table 2 Demographic Characteristics of the Community Pharmacists (CPs) (n = 238) |
The Community Pharmacists’ Practice Regarding the Simulated Scenario
Regarding patient assessment before dispensing, of the 238 CPs in this study, 45.4% asked at least one question before making any decision. Thirty (12.6%) CPs recommended visiting a doctor after hearing the scenario and no medications were dispensed during these visits, while at least one antibiotic was dispensed in 69.3% of the visits (Table 3). There is no significant association between the dispensing of antibiotic by community pharmacists and their gender, level of education, and years of experience as community pharmacist.
 |
Table 3 Dispensing Decisions, Information and Type of Medications Provided by the Community Pharmacists (CPs) (n = 238) |
Different classes of antibiotics were observed, among them, fluoroquinolones were highly dispensed followed by cephalosporins, while combinations of two antibiotics were also observed. Ciprofloxacin was the most dispensed antibiotic (51.5%) followed by cefixime (41.8%), and the least dispensed (0.6%) were nitrofurantoin, co-trimoxazole, and some antibiotic combinations (Table 4).
 |
Table 4 Types of Antibiotics Dispensed During the Visits (n = 165) |
The Dispensing of Cefixime Before and After Demand
Out of 238 community pharmacists, 69 (29%) dispensed cefixime in response to the scenario before the SP requested cefixime. Among the rest 169 (71%), only 37.3% refused to dispense cefixime after demand and all provided reasons for their refusal. Regarding the explanations provided by the community pharmacists, 19 (30.2%) CPs recommended taking the medication suggested by them. Details are presented in Table 5.
 |
Table 5 The Response of CPs After Cefixime Demand and Their Explanations for Not Dispensing It |
Discussion
Community pharmacies are centered in the heart of the communities making them a principal point of accessing many medications including antibiotics.27 In this study, the scenario was developed without naming any antibiotic first to allow the pharmacist to assess before making his/her judgment, and encourage him/her to investigate before the SP demand for cefixime. The results showed that 45.4% of the CPs did ask at least one question before their dispensing, despite that the current study demonstrates that antibiotics are being sold without a prescription.
Even though one scenario was used in this study, an antibiotic was dispensed in 69.3% of the visits. As uncomplicated urinary tract infection (cystitis) was the case of our scenario, it is difficult to compare the results of the study with the existing literature as few had discussed this particular scenario. A similar high result was noticed in one comparable study from Spain with a similar methodology which found that in the uncomplicated urinary tract infection (UTI) scenario, 79.7% of the CPs have sold antibiotics without a prescription.28 Also, a study conducted in Eritrea to determine the extent of dispensing antibiotics without prescription has reported that for uncomplicated UTI scenario antibiotics were dispensed in 89.2% of the simulated visits.29 Whereas in a study from South Africa with a similar UTI scenario, 26.4% of the CPs have dispensed antibiotics without a prescription.30
This high rate of dispensing antibiotics that was found in our study was also noticed in many countries with different study scenarios like Syria (87%),31 Ethiopia (93.5%),32 and Pakistan (82.7%).19 In contrast, some countries have reported considerably lower rates of antibiotic dispensing without prescription, such as Lebanon (30.8%),33 Saudi Arabia (12.5%),34 and Zimbabwe (7%).35
Ciprofloxacin (51.5%) and cefixime (41.8%), were the antibiotics that were commonly dispensed in this study. This result was consistent with the results from a South African study where the most sold antibiotic for UTIs was ciprofloxacin (42.9%).30 A. Ntizala et al also found that ciprofloxacin (74.3%) and cefixime (72.5%) were the most dispensed antibiotics without prescription regardless of whether they were requested by the patients or recommended by dispensers.13 Additionally, findings from other simulation studies conducted in Lebanon,36 India,37 Sri Lanka,38 and China showed that ciprofloxacin was the most dispensed antibiotic.39
As attempt to adjust the utilization of antibiotics and to enhance their appropriate use, the WHO has classified antibiotics to three different groups which are Access, Watch and Reserve (AWaRe) antibiotics. The Access group includes antibiotics with activity against many frequently encountered pathogens and recommended as first or second line choices for empiric treatment of most infectious diseases. The Watch group includes antibiotics which have higher resistance potential, and their use is limited to certain patients. While the Reserve group includes antibiotics that reserved for multi-drug-resistant organisms and should be used as last treatment options, both ciprofloxacin and cefixime are from the Watch group antibiotics.40
Ciprofloxacin belongs to the class of antibiotics called fluoroquinolones. This class has many side effects that can seriously affect the patient’s health, and some of these side effects include irreversible nerve damage, peripheral neuropathy, and tendon rupture.41 Moreover, an association was found between the increased appearance of MRSA (methicillin-resistant staphylococcus aureus) and the augmented consumption of fluoroquinolones.42 On the other hand, cefixime is a third-generation cephalosporin, and this class of antibiotic has the strongest association with Clostridium difficile–associated diarrhea.43
In our study, before cefixime was requested by name, 29% of the community pharmacists already dispensed it, responding to the scenario, and from the rest (71%), 62.7% of them sold cefixime after demand. Cefixime belongs to an important broad-spectrum pharmacological class of antibiotics used in different pathological conditions.44 It has activity against a wide spectrum of bacteria like Haemophilus influenzae, Salmonella, Streptococcus pneumoniae, Streptococcus pyogenes, Shigella, Staphylococcus aureus, Neisseria gonorrhoeae, and E. coli.45 However, the high rate of its dispensing that was noticed in our study eventually will lead to its resistance if it does not exist.
Already one study has shown that there is a relatively high rate of clinical failure after treatment of Neisseria gonorrhoeae infections with cefixime.46 Further, another study reported that the antibiotic misuse found in their study was consistent with the city profile of antibiotic resistance.13 In Sudan, O. Abdellatif et al47 has reported that some bacteria including Klebsiella pneumonia, Staphylococcus aureus, and E. coli were highly resistant to cefixime by more than 90% of the total cases of the study. Also, a study conducted in Khartoum state has documented an increased resistance of the isolated bacteria to penicillin, cephalosporins, macrolide, and fluoroquinolones.48
Counseling self-medicated patients has a crucial impact on the emergence of bacterial resistance. A qualitative exploratory study conducted in Sudan has found that one of the reasons pharmacists dispense antibiotics without prescriptions in Khartoum state is the lack of care in providing counseling for self-medicated patients with antibiotics.22 In our study, after cefixime was demanded, 37.3% of the CPs refused to dispense it, and all explained to the patients during their counseling why they could not dispense it. The majority of them advised the patients to visit a physician for further investigation, and few asked for a prescription.
This study revealed that many CPs dispense antibiotics without prescription and cefixime specifically was highly dispensed. Our study was conducted in Khartoum locality, one of the three modern localities of the capital Khartoum where hospitals and community pharmacies are abundant. However, as in many low- and middle-income countries, Sudanese patients have limited income, and after the economic reforms that led to the introduction of user fees in health centers and public healthcare facilities, access and utilization of basic health services became unaffordable.6 And although health insurance has been introduced in Sudan more than 20 years ago, it has never reach universal coverage, and even its sustainability is questionable.49 Therefore, it might be a logical more preferable choice for the patients to purchase medicines including antibiotics from community pharmacies to avoid any additional medical fees.
In a Sudanese study that evaluated community pharmacists’ knowledge, attitude, and practice regarding antibiotics dispensing without prescriptions, 93.4% of the CPs were either always or sometimes dispensing antibiotics without prescriptions.21 The question of why community pharmacists dispense antibiotics without prescription in Sudan has already been answered by Anas M.A. Salim et al where patients’ low socioeconomic status and their inability to pay for medical consultation, was the main reason that drove pharmacists to this practice. Other reasons like pharmacists’ commercial interest, health authorities’ absence in supervising and regulating community pharmacies dispensing practices, and patient pressure were also common.22 In addition, an exploratory study from Africa has found many factors that affect antibiotic dispensing without prescription including weak regulation, poor inspection and training, community pharmacy owners’ economic interest, inadequate patient knowledge, and the inability of patients to access health facilities.50
It was found that the non-prescribed dispensing of antibiotic can be minimized if community pharmacies run by qualified will trained pharmacists, especially in areas where pharmacist considered the only available healthcare member.51 Additionally, a study from Kenya has attributed the low levels of self-medication with antibiotics that found in their study to the qualification and the high levels of training the pharmacy personnel had.52 This reflect the importance of pharmacy education. In Sudan, pharmacy education places a greater emphasis on product with solid foundation in pharmaceutical sciences and less on clinical issues,53 and one study has already mentioned that all pharmacy schools in Sudan need to update their curricula to incorporate patient-centered teaching and training.54
Law enforcement, public awareness campaigns, and effective supervision and training of healthcare members were found to be contributors in reducing self-medication with antibiotics in high income European countries.55 According to Sudan pharmaceutical country profile, there is no national medicine information center that is supported by the government or private sector provides information on rational use of medicine. Also, there is no formalized national policy to control antibiotic resistance, and antibiotics are dispensed without prescription.54 In 2018, a national action plan against antimicrobial resistance was introduced to achieve better antimicrobial utilization in humans and animal, and to increase the awareness regarding antimicrobial resistance.56 Despite that, pharmacists still dispense antibiotic without prescription.
The study has some limitations. Firstly, only the pharmacies located in Khartoum locality were visited. Consequently, our findings cannot be generalized to the entire country. Secondly, the data was collected depending only on the SPs’ recall abilities as the audio recording was not used in this study, thus there is a possibility of recall bias. Finally, pharmacists’ factors like training courses and experience in hospital and clinical settings which might affect their performance were not included in our study.
Conclusion
The study revealed that the malpractice of dispensing antibiotics without prescription by community pharmacists is highly prevalent in Khartoum state, and cefixime was obtained with ease before and after the patient’s demand. Hence, urgent action is needed to minimize or prevent this inappropriate sale of antibiotics, starting by facilitating the accessibility to medical consultation and this can be done by improving the quality of the governmental medical services. Also, the health authorities should provide clear guidelines and regulations regarding antibiotics dispensing, and monitor pharmacists’ practice. Further, It is essential to adopt strict penalties on pharmacies and pharmacists who do not follow these regulations. Moreover, pharmacist training may affect pharmacists’ practice in antibiotic dispensing, and the quality of their advice when educating self-medicated patients. Thus, stakeholders should endorse effective training and educational programs to improve pharmacists’ practice.
Acknowledgments
The authors express appreciation to pharmacy students who participated in this study as simulated patients.
Disclosure
All authors declare that there are no conflicts of interest in this work.
References
1. World Health Organization. Antimicrobial Resistance: Global Report on Surveillance. World Health Organization; 2014. Available from: https://apps.who.int/iris/handle/10665/112642.
2. Mathers C, Fat DM, Boerma JT. The Global Burden of Disease: 2004 Update. World Health Organization; 2008. Available from: https://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/.
3. Muhie OA. Antibiotic use and resistance pattern in Ethiopia: systematic review and meta-analysis. Int J Microbiol. 2019;1(2489063):56.
4. Yimenu DK, Emam A, Elemineh E, Atalay W. Assessment of Antibiotic Prescribing Patterns at Outpatient Pharmacy Using World Health Organization Prescribing Indicators. J Prim Care Community. Health. 2019;10:2150132719886942.
5. Abdelaziz AI, Tawfik AG, Rabie KA, et al. Quality of Community Pharmacy Practice in Antibiotic Self-Medication Encounters: a Simulated Patient Study in Upper Egypt. Antibiotics. 2019;8(2):35. doi:10.3390/antibiotics8020035
6. Awad AI, Eltayeb IB, Capps PA. Self-medication practices in Khartoum State, Sudan. Eur J Clin Pharmacol. 2006;62(4):317–324. doi:10.1007/s00228-006-0107-1
7. Grigoryan L, Monnet DL, Haaijer-Ruskamp FM, Bonten MJ, Lundborg S, Verheij TJ. Self-medication with antibiotics in Europe: a case for action. Curr Drug Saf. 2010;5(4):329–332. doi:10.2174/157488610792246046
8. Lescure D, Paget J, Schellevis F, van Dijk L. Determinants of Self-Medication With Antibiotics in European and Anglo-Saxon Countries: a Systematic Review of the Literature. Front Public Health. 2018;6(370). doi:10.3389/fpubh.2018.00370
9. Auta A, Hadi MA, Oga E, et al. Global access to antibiotics without prescription in community pharmacies: a systematic review and meta-analysis. J Infect. 2019;78(1):8–18. doi:10.1016/j.jinf.2018.07.001
10. Arumugham VB, Gujarathi R, Cascella M. Third-Generation Cephalosporins. Treasure Island (FL): StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549881/.
11. Adam D. Overview of the clinical features of cefixime. Chemotherapy. 1998;1:1–5. doi:10.1159/000048455
12. Shigi Y, Matsumoto Y, Kaizu M, Fujishita Y, Kojo H. Mechanism of action of the new orally active cephalosporin FK027. J Antibiot. 1984;37(7):790–796. doi:10.7164/antibiotics.37.790
13. Ntizala AB, Mulume TY, Runyeruka BL, Kishabongo AS. Antibiotic Dispensing Practices in Community Pharmacies: a Major Health Concern in the Eastern Democratic Republic of Congo. J Pharm Res Int. 2020;32(14):33–44. doi:10.9734/jpri/2020/v32i1430603
14. Bianco A, Licata F, Trovato A, Napolitano F, Pavia M. Antibiotic-Dispensing Practice in Community Pharmacies: results of a Cross-Sectional Study in Italy. Antimicrob Agents Chemother. 2021;65(6):2729. doi:10.1128/AAC.02729-20
15. Seiberth JM, Moritz K, Kücükay N, Schiek S, Bertsche T. What is the attitude towards and the current practice of information exchange during self-medication counselling in German community pharmacies? An assessment through self-report and non-participant observation. PLoS One. 2020;15(10):e0240672. doi:10.1371/journal.pone.0240672
16. Zawahir S, Lekamwasam S, Aslani P. Community pharmacy staff’s response to symptoms of common infections: a pseudo-patient study. Antimicrob Resist Infect Control. 2019;8(1):60. doi:10.1186/s13756-019-0510-x
17. Bennadi D. Self-medication: a current challenge. J Basic Clin Pharm. 2014;5(1):19–23. doi:10.4103/0976-0105.128253
18. Al-Mohamadi A, Badr A, Bin Mahfouz L, Samargandi D, Al Ahdal A. Dispensing medications without prescription at Saudi community pharmacy: extent and perception. Saudi Pharm J. 2013;21(1):13–18. doi:10.1016/j.jsps.2011.11.003
19. Saleem Z, Hassali MA, Godman B, et al. Sale of WHO AWaRe groups antibiotics without a prescription in Pakistan: a simulated client study. J Pharm Policy Pract. 2020;13(26):020–00233. doi:10.1186/s40545-020-00233-3
20. Björnsdottir I, Granas AG, Bradley A, Norris P. A systematic review of the use of simulated patient methodology in pharmacy practice research from 2006 to 2016. Int J Pharm Pract. 2020;28(1):13–25. doi:10.1111/ijpp.12570
21. Abdelrahman Hussain M A, Osman Mohamed A, Sandel Abkar A, Siddig Mohamed F, Knowledge KEH. Attitude and Practice of Community Pharmacists in Relation to Dispensing Antibiotics Without Prescription in Sudan: a Cross-sectional Study. Integr Pharm Res Pract. 2022;11:107–116. doi:10.2147/IPRP.S363079
22. Salim AM, Elgizoli B. Exploring the reasons why pharmacists dispense antibiotics without prescriptions in Khartoum state, Sudan. Int J Pharm Pract. 2017;25(1):59–65. doi:10.1111/ijpp.12317
23. Hussain MA, Mohamed AO, Abdelkarim OA, et al. Prevalence and Predictors of Antibiotic Self-Medication in Sudan: a Descriptive Cross-Sectional Study. Antibiotics. 2023;12(3):612. doi:10.3390/antibiotics12030612
24. Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007;147(8):W163–94. doi:10.7326/0003-4819-147-8-200710160-00010-w1
25. Bouter S, van Weel-Baumgarten E, Bolhuis S. Construction and validation of the Nijmegen Evaluation of the Simulated Patient (NESP): assessing simulated patients’ ability to role-play and provide feedback to students. Acad Med. 2013;88(2):253–259. doi:10.1097/ACM.0b013e31827c0856
26. Czajkowski K, Broś-Konopielko M, Teliga-Czajkowska J. Urinary tract infection in women. Prz Menopauzalny. 2021;20(1):40–47. doi:10.5114/pm.2021.105382
27. Nepal A, Hendrie D, Robinson S, Selvey LA. Survey of the pattern of antibiotic dispensing in private pharmacies in Nepal. BMJ Open. 2019;9(10):2019–032422. doi:10.1136/bmjopen-2019-032422
28. Llor C, Cots JM. The sale of antibiotics without prescription in pharmacies in Catalonia, Spain. Clin Infect Dis. 2009;48(10):1345–1349. doi:10.1086/598183
29. Bahta M, Tesfamariam S, Weldemariam DG, et al. Dispensing of antibiotics without prescription and associated factors in drug retail outlets of Eritrea: a simulated client method. PLoS One. 2020;15(1):e0228013. doi:10.1371/journal.pone.0228013
30. Mokwele RN, Schellack N, Bronkhorst E, Brink AJ, Schweickerdt L, Godman B. Using mystery shoppers to determine practices pertaining to antibiotic dispensing without a prescription among community pharmacies in South Africa - a pilot survey. JAC-Antimicrobial Resist. 2022;4(1):1–10. doi:10.1093/jacamr/dlab196
31. Al-Faham Z, Habboub G, Takriti F. The sale of antibiotics without prescription in pharmacies in Damascus, Syria. J Infect Dev Ctries. 2011;5(5):396–399. doi:10.3855/jidc.1248
32. Erku DA, Mekuria AB, Surur AS, Gebresillassie BM. Extent of dispensing prescription-only medications without a prescription in community drug retail outlets in Addis Ababa, Ethiopia: a simulated-patient study. Drug Healthc Patient Saf. 2016;8:65–70. doi:10.2147/DHPS.S106948
33. Yaacoub SG, Lahoud NA, Francis NJ, et al. Antibiotic prescribing rate in Lebanese community pharmacies: a nationwide patient-simulated study of acute bacterial rhinosinusitis. J Epidemiol Glob Health. 2019;9(1):44–49. doi:10.2991/jegh.k.190305.001
34. Al-Tannir M, Altannir Y, Altannir M, AlFayyad I. Community pharmacy sales of non-prescribed antibiotics in Riyadh, Saudi Arabia: a simulated patient study. Int J Clin Pharm. 2020;42(2):341–346. doi:10.1007/s11096-020-01033-0
35. Nyazema N, Viberg N, Khoza S, et al. Low sale of antibiotics without prescription: a cross-sectional study in Zimbabwean private pharmacies. J Antimicrob Chemother. 2007;59(4):718–726. doi:10.1093/jac/dkm013
36. Yaacoub SG, Koyess V, Lahoud N, et al. Antibiotic prescribing for acute uncomplicated cystitis in Lebanese community pharmacies using a simulated patient. Pharm Pract (Granada). 2019;17(4):1–8. doi:10.18549/PharmPract.2019.4.1604
37. Shet A, Sundaresan S, Forsberg BC. Pharmacy-based dispensing of antimicrobial agents without prescription in India: appropriateness and cost burden in the private sector. Antimicrob Resist Infect Control. 2015;4(1):1–7. doi:10.1186/s13756-015-0098-8
38. Zawahir S, Lekamwasam S, Aslani P. Antibiotic dispensing practice in community pharmacies: a simulated client study. Res Soc Adm Pharm. 2019;15(5):584–590. doi:10.1016/j.sapharm.2018.07.019
39. Chang J, Xu S, Zhu S, et al. Articles Assessment of non-prescription antibiotic dispensing at community pharmacies in China with simulated clients: a mixed cross-sectional and longitudinal study. Lancet Infect Dis. 2019;3099(19):1–10. doi:10.1016/S1473-3099(19)30324-X
40. Moja L, Huttner B. Selection and Use of Essential Medicines. In: Raviglione MCB, Tediosi F, Villa S, Casamitjana N, Plasència A, editors. Global Health Essentials. Cham: Springer International Publishing; 2023:321–325.
41. Malik UR, Chang J, Hashmi F, et al. A simulated client exploration of nonprescription dispensing of antibiotics at drugstores for pediatric acute diarrhea and upper respiratory infection in Lahore, Pakistan. Infect Drug Resist. 2021;14:1129–1140. doi:10.2147/IDR.S301812
42. Parienti J, Cattoir V, Thibon P, Lebouvier G, Verdon R, Daubin C. Hospital-wide modification of fluoroquinolone policy and meticillin-resistant Staphylococcus aureus rates: a 10-year interrupted time-series analysis. J Hosp Infect. 2011;78(2):118–122. doi:10.1016/j.jhin.2011.03.008
43. Wilcox MH, Chalmers JD, Nord CE, Freeman J, Bouza E. Role of cephalosporins in the era of Clostridium difficile infection. J Antimicrob Chemother. 2017;72(1):1–18. doi:10.1093/jac/dkw385
44. Onanuga A, T TC. Multidrug-resistant intestinal Staphylococcus aureus among self-medicated healthy adults in Amassoma, South-South, Nigeria. J Heal Popul Nutr. 2011;29(5):446–453.
45. Chaudhary MK, Ghyanshyam P, Mahendra G, Ramesh G, Subash G. Efficacy of cefixime in the treatment of urinary tract infection. World J Pharm Pharm Sci. 2015;4(4):987–994.
46. Allen VG, Mitterni L, Seah C, et al. Neisseria gonorrhoeae treatment failure and susceptibility to cefixime in Toronto, Canada. JAMA. 2013;309(2):163–170. doi:10.1001/jama.2012.176575
47. Abdellatif O, Ali AN, Mohamed IA. Evaluation of the Antibiotic Resistance Pattern at the Medical Services Administration Hospital in Khartoum, Sudan, 2021. J Res Appl Sci Biotechnol. 2022;1(4):50–56. doi:10.55544/jrasb.1.4.6
48. Moglad EH. Antibiotics Profile, Prevalence of Extended-Spectrum Beta-Lactamase (ESBL), and Multidrug-Resistant Enterobacteriaceae from Different Clinical Samples in Khartoum State, Sudan. Int J Microbiol. 2020;2020:8898430. doi:10.1155/2020/8898430
49. Salim AMA, Hamed FHM. Exploring health insurance services in Sudan from the perspectives of insurers. SAGE Open Med. 2018;6:2050312117752298. doi:10.1177/2050312117752298
50. Bahta M, Weldemariam DG, Tesfamariam S, Tesfamariam EH, Russom M. Determinants of dispensing antibiotics without prescription in Eritrea: a mixed-method qualitative study on pharmacy professionals’ perspective. BMJ Open. 2021;11(8):e049000. doi:10.1136/bmjopen-2021-049000
51. Marković-Peković V, Grubiša N, Burger J, Bojanić L, Godman B. Initiatives to Reduce Nonprescription Sales and Dispensing of Antibiotics: findings and Implications. J Res Pharm Pract. 2017;6(2):120–125. doi:10.4103/jrpp.JRPP_17_12
52. Mukokinya MMA, Opanga S, Oluka M, Godman B. Dispensing of Antimicrobials in Kenya: a Cross-sectional Pilot Study and Its Implications. J Res Pharm Pract. 2018;7(2):77–82. doi:10.4103/jrpp.JRPP_17_88
53. Mohamed SSE, Mahmoud AA, Ali AA. Sudanese community pharmacy practice and its readiness for change to patient care. Int J Pharm Pract. 2015;23(4):266–273. doi:10.1111/ijpp.12156
54. Mohamed SS, Mahmoud AA, Ali AA. The role of Sudanese community pharmacists in patients’ self-care. Int J Clin Pharm. 2014;36(2):412–419. doi:10.1007/s11096-013-9911-8
55. Napolitano F, Izzo MT, Di Giuseppe G, Angelillo IF. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS One. 2013;8(12):e84177. doi:10.1371/journal.pone.0084177
56. Abdelrahman Hussain M, Osman Mohamed A, Sandel Abkar A, Siddig Mohamed F, Knowledge KEH. Attitude and Practice of Community Pharmacists in Relation to Dispensing Antibiotics Without Prescription in Sudan: a Cross-sectional Study. Integr Pharm Res Pract. 2022;11:107–116.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
