Back to Journals » Patient Preference and Adherence » Volume 18
The Effects of Pharmacist-Led Medication Therapy Management on Medication Adherence and Use of Non-Steroidal Anti-Inflammatory Drug in Patients with Pre-End Stage Renal Disease
Authors Wang T, Kang HC, Chen CC, Lai TS, Huang CF, Wu CC
Received 28 August 2023
Accepted for publication 23 January 2024
Published 1 February 2024 Volume 2024:18 Pages 267—274
DOI https://doi.org/10.2147/PPA.S436952
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Ting Wang,1 Hao-Cheng Kang,1 Chia-Chi Chen,1 Tai-Shuan Lai,2 Chih-Fen Huang,1,3 Chien-Chih Wu1,3
1Department of Pharmacy, National Taiwan University Hospital, Taipei, Taiwan; 2Department of Internal Medicine, National Taiwan University Hospital, Taipei, Taiwan; 3School of Pharmacy, College of Medicine, National Taiwan University, Taipei, Taiwan
Correspondence: Chien-Chih Wu, Department of Pharmacy, National Taiwan University Hospital, College of Medicine, National Taiwan University, 7 Chung Shan S. Road, Taipei, Taiwan, Tel/Fax +886-2-23123456 ext. 63702 ; +886-2-23310930, Email [email protected]; [email protected]
Purpose: Patients with chronic kidney disease (CKD) are particularly vulnerable to the risks of polypharmacy, largely owing to various comorbid conditions. This vulnerability is further compounded by an escalated risk of renal function deterioration when exposed to nephrotoxic medications. As part of the national health insurance program in Taiwan, the pre-end-stage kidney disease patient care and education plan has included pharmaceutical care since October 2021. This study aims to explore the effect of pharmacist involvement in a multidisciplinary care team for patients with kidney disease in outpatient settings.
Patients and Methods: This retrospective observational study was conducted at a single center. It analyzed data from May 2022 to May 2023, focusing on patients who received medication therapy management in the kidney disease pharmacist-managed clinic. The study assessed changes in patient medication adherence, non-steroidal anti-inflammatory drugs (NSAIDs) usage, CKD stage, and urine protein-to-creatinine ratio (UPCR) after pharmacist intervention. It also documented pharmacists’ medication recommendations and the rate of acceptance by physicians.
Results: A total of 202 patients who had at least two clinic visits were included in the study. After pharmacist intervention, the proportion of poor medication adherence reduced significantly from 67.8% to 43.1% (p< 0.001). The proportion of NSAID users also decreased significantly from 19.8% to 8.4% (p=0.001). CKD stage showed a significant reduction (p=0.007), and the average UPCR improved from 2828.4 to 2111.0 mg/g (p< 0.001). The pharmacists provided a total of 56 medication recommendations, with an acceptance rate of 86%.
Conclusion: The involvement of pharmacists in the multidisciplinary care team can effectively provide medication-related recommendations, ensuring the effectiveness and safety of patients’ medication use, and lead to better kidney function and lower proteinuria.
Keywords: pharmaceutical care, medication therapy management, chronic kidney disease, medication adherence, non-steroidal anti-inflammatory drugs
Introduction
Chronic kidney disease (CKD) is a prevalent global health issue, with significant economic implications, contributing to a substantial burden on health systems worldwide.1,2 Globally, CKD prevalence is estimated to range between 10–14%, with stage three kidney disease being the most common.1 Despite significant strides in medical technology, the global age-standardized mortality rate for CKD have not exhibited a declining trend.3 The pharmacotherapy for patients with CKD is often complex and multifaceted. These treatment regimens typically encompass drugs aimed at decelerating the progression of the disease, including angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs), and sodium–glucose cotransporter 2 (SGLT2) inhibitors. Additionally, they involve medications to manage associated comorbidities and complications. Such comprehensive therapeutic strategies often lead to polypharmacy, characterized by the regular administration of five or more medications daily. This, in turn, frequently presents challenges in terms of patient adherence to medication schedules.4
Poor adherence to medication regimes may impact health-related quality of life, and even correlate with deteriorating kidney function.5,6 CKD patients are also at elevated risk of using nephrotoxic drugs, notably non-steroidal anti-inflammatory drugs (NSAIDs), which may exacerbate kidney function, cause acute kidney injury (AKI), and heighten hospitalization risk.7–9 In East Asia, the situation may be further complicated due to the habitual use of traditional Chinese herbal remedies among the populace and the potential drug-herb interactions and adverse reactions.10,11 As CKD care necessitates precise control of multiple factors, including medication, diet, and lifestyle habits, international guidelines endorse a multidisciplinary collaborative model for kidney disease care and advise consultation with a pharmacist before the utilization of over-the-counter (OTC) drugs or dietary supplements.12–14 Incorporating medication therapy management (MTM) through pharmacists has demonstrated potential to enhance patient medication adherence, mitigate healthcare costs, and improve CKD patients’ quality of life.15 Prior research has indicated that pharmacist interventions for both inpatients and outpatients with CKD can resolve medication-related problems (MRPs), promote medication adherence, and improve disease control.16,17
Taiwan initiated a multidisciplinary team care and health education program for pre-end-stage renal disease (pre-ESRD) patients in 2006, which included nephrologists, nurses, dieticians, and social workers, but notably excluded pharmacists. Following several years of this program’s implementation, studies suggested that it optimized the prescription of erythropoiesis-stimulating agents and cholesterol-lowering statin drugs, leading to enhanced anemia treatment and post-dialysis survival rates. However, a significant proportion of patients (≥20%) reportedly continued NSAID use before dialysis.18 Furthermore, medication adherence among this patient population remains undetermined. Pharmacists were integrated into the Pre-ESRD program’s multidisciplinary care team in October 2021. However, the effectiveness of pharmacist-led MTM for this patient population in Taiwan is yet to be fully examined due to lack of relevant data. This study aimed to investigate the effect of pharmacist-led MTM on improving adherence and reducing the use of potentially nephrotoxic NSAIDs among patients with CKD. Additionally, we also explored its effect on renal function deterioration.
Materials and Methods
This was a single-center retrospective study. Adult patients (aged ≥18 years) diagnosed with CKD stages 3b, 4, or 5, without dialysis, were eligible for pre-ESRD multidisciplinary care at National Taiwan University Hospital (NTUH). Inclusion criteria also encompassed individuals with significant proteinuria (24-hour urine total protein excretion > 1000 mg or urine protein and creatinine ratio [UPCR] > 1000 mg/g), and those who had an estimated glomerular filtration rate (eGFR) by the Modification of Diet in Renal Disease (MDRD) formula < 45 mL/min/1.73 m2 following AKI leading to acute kidney disease (AKD). Patients newly enrolled in the Pre-ESRD program at NTUH were referred to the kidney disease pharmacist-managed clinic (PMC). The study involved individuals who voluntarily engaged in at least two pharmacist-led MTM sessions, with a minimum interval of three months between sessions, conducted between May 2022 and May 2023. This study was conducted in compliance with the Declaration of Helsinki and received approval from the Research Ethics Committee of National Taiwan University Hospital (approval number: 202307205RIND; 2023). Patient informed consent was waived due to the retrospective nature of the study, and all collected data was anonymized and kept confidential.
The pre-ESRD multidisciplinary team included nephrologist, nurse, dietician, and pharmacist (Table 1). The team provided comprehensive care through personalized guidance, including daily life, diet, and medication use, with the goal of delaying kidney function deterioration, avoiding CKD-related complications, and improving the overall quality of CKD care. Each professional provided care within the same day. The patient received basic self-care information from the nurse, nutritional assessment and diet guidance from the dietician, and was then referred to the PMC. Two pharmacists were certificated to provide MTM and three major dimensions were focused. First, medication adherence was assessed based on the patient’s compliance with their medication regimen in the past month, and potential causes of poor adherence were identified and addressed. Medication adherence was evaluated using the Adherence to Refills and Medications Scale (ARMS), scored by the pharmacists. The scale ranged from 12 to 48, with a score of 12 signifying complete adherence to medication instructions. Conversely, higher scores (>12) indicated a more severe degree of non-adherence, reflective of increased instances of non-compliance with prescribed medication regimens or missed refills.19 Second, medication reconciliation was provided and pharmacist integrated prescription drugs from all hospitals, over-the-counter medications, nutritional supplements, and Chinese herbal remedies used by the patient. These encompassed both traditional Chinese medicines prescribed by traditional Chinese physicians and those independently acquired by the patient, which could include purchases from Chinese medicine shops, pharmacies, or from other sources. If MRPs were identified, the pharmacist directly contacted the physician by phone or used a medication recommendation sheet to solve the problems. These MRPs were also documented in the electronic record system. Special attention was paid to NSAID assessment, with NSAID exposure assessed by tracking usage in the past three months, including prescription and OTC drugs. If any NSAID was used, the appropriateness of the usage was assessed and alternative treatments were explored for avoidance. Third, medication counseling education included knowledge about disease self-caring, medications, and education to avoid drug related kidney injury.
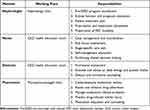 |
Table 1 Members of the Pre-ESRD Multidisciplinary Team and Respective Responsibilities |
Data on baseline demographics, eGFR, UPCR, ARMS score and NSAID use were collected from the electronic medical records of the enrolled patients. Categorical variables were expressed as number with percentage and continuous variables are expressed as mean ± standard deviation or median with range. The study evaluated changes in kidney function by comparing the most recent CKD stage and UPCR values obtained within the three months before inclusion with the latest values acquired at the second visit. Analysis of CKD stage changes was limited to patients admitted with CKD (excluding AKD) and an eGFR ≤ 45 mL/min/1.73 m2. Evaluation of proteinuria changes was restricted to individuals with significant proteinuria (UPCR > 500 mg/g). Continuous variables (such as ARMS score and UPCR) were subjected to analysis employing paired t-tests, whereas categorical variables (specifically ARMS categorization as > or = 12, CKD stage, and NSAID use) were evaluated utilizing McNemar’s test, with a predetermined level of statistical significance set at p<0.05. All statistical analyses were performed using STATA v.14.0 (StataCorp, College Station, TX, USA).
Results
Between May 1, 2022, and May 31, 2023, we enrolled a total of 202 patients. Patient demographics are detailed in Table 2. The cohort comprised more males (61.9%), with an average age of 68 years. CKD cases constituted the majority (91.6%), including significant proteinuria cases (UPCR > 1000 mg/g) which accounted for 11.4% of the total. AKD cases were 17 in number (8.4%). In terms of renal function at enrollment, CKD Stage 3b was most common, accounting for 47.0% of the cases, followed by stage 4 at 26.7%. Regarding medication, the median number of currently used prescription drugs was nine (range 1–25), with 179 (88.6%) patients taking five or more different medications, and 86 (42.6%) patients taking 10 or more different medications. 40 (19.8%) patients had used NSAIDs in the previous three months.
 |
Table 2 Patient Demographics |
We observed a significant reduction of patient numbers and proportion in poor medication adherence (ARMS score > 12) from 137 (67.8%) to 87 (43.1%) of the patients (p<0.001, Figure 1), accompanied by a significant decrease in the average score from 15.1±2.9 to 13.5±2.3 (p<0.001). The main factors affecting medication adherence were patients modifying medications independently and forgetting to take medicine due to high frequency of doses. The utilization of NSAIDs among patients exhibited a significant decrease, declining from 40 (19.8%) to 17 (8.4%) individuals (p=0.001). (Figure 2) Concerning MRPs, pharmacists made a total of 56 medication recommendations to physicians, 48 of which were accepted (an acceptance rate of 86%). The most common recommendation category was dosage or frequency (23%), followed by medication reconciliation (21%), suggestion of more appropriate medication (20%), and duration (13%).
 |
Figure 1 Comparison of medication adherence before and after pharmacist intervention by Adherence to Refills and Medications Scale (ARMS). |
 |
Figure 2 Non-steroidal anti-inflammatory drugs (NSAID) use evaluation. |
Among 164 CKD patients with eGFR ≤ 45 mL/min/1.73 m² at the time of inclusion, a significant reduction in CKD stage was observed in 34 patients (20.7%). This was statistically significant (p=0.007). The average time interval between evaluations of CKD stage was 103 days. Among 109 patients with a UPCR > 500 mg/g at enrollment, 37 were excluded due to lack of a second UPCR value. Analysis of the remaining 72 patients showed that the UPCR value significantly decreased from 2828.4 to 2111.0 mg/g (p<0.001), with an average interval of 102 days between UPCR evaluations.
Discussion
The majority of studies on the CKD population focus on dialysis patients or inpatient pharmacist interventions.16 This study focused on ambulatory care for pre-ESRD patients who had not yet started dialysis to investigate the effect of pharmacist intervention on medication adherence and avoidance of exposure to NSAIDs. Prior to the involvement of pharmacists in this multidisciplinary care approach, patients primarily received conventional medical care, with various specialists providing prescriptions independently. These prescriptions were subject to pharmacist review, focusing on their suitability in terms of indications, dosages, and potential drug interactions, prior to being dispensed to patients. However, this process did not sufficiently integrate different departments, nor did it evaluate aspects such as medication adherence, use of self-administered medications, or dietary supplements. With the introduction of pharmacist-led MTM, comprehensive evaluations became a routine part of care. These evaluations include assessments of medication adherence, medication reconciliation, and patient education, ensuring a holistic approach for every pre-ESRD patient. Our study shows that the involvement of pharmacists in pre-ESRD care in Taiwan can significantly enhance medication adherence and decrease NSAID use rate. CKD patients are high risk group of polypharmacy issue.20–22 A study in Germany found that as many as 80% of CKD patients belong to the polypharmacy group with five or more daily medications, with a median of eight total daily medications (range 0–27). Factors such as higher CKD stage, age, diabetes, and cardiovascular disease may contribute to polypharmacy.4 In our study, the prevalence of polypharmacy was notably higher, at 88.6%. Therefore, medication adherence would be a problem in CKD patients. Studies on medication adherence in pre-ESRD patients showed that patients’ medication adherence is only about 67.4%, and that as kidney function declines and CKD stage increases, patients’ medication adherence worsens.23 Poor medication adherence, particularly concerning medications like renin-angiotensin-aldosterone system inhibitors, not only increases the risk of cardiovascular events and mortality but also correlates with heightened progression of CKD.24,25 To improve the quality of pharmaceutical care for pre-ESRD patients, we adopted a MTM model proven abroad to effectively improve the clinical disease control, medication adherence, and quality of life of CKD patients.15 The factors affecting medication adherence include patient-related factors (such as misconceptions about medication information and lack of medication-related self-efficacy), medication-related factors (such as polypharmacy), health care system-related factors (such as lack of trust in doctors by patients), and socio-economic factors (such as lack of social support and low education levels), all of which may lead to a decline in medication compliance.23,26 Previous research has found that health care professionals can help patients improve their medication compliance by incorporating medication administration into regular daily life.27 Providing reminder tools (like dosette boxes) can assist patients in avoiding forgetting to take their medications.28 Helping patients dispel myths about pharmacotherapy and increasing patients’ knowledge about medication and how to deal with side effects can also be beneficial for medication compliance.23,27 In this study, pharmacists identified and resolved individual issues affecting patients’ medication adherence during consultations, successfully improved their medication adherence.
Preventing nephrotoxic drug exposure such as NSAID is another important issue in patients with kidney disease.29,30 However, NSAIDs are still widely used worldwide. In the United States, about 19% of the population has used at least one type of NSAID in a year, and studies in Sweden and the United Kingdom have shown that about 15–17% of the elderly population over 60–65 years old use NSAIDs long term.9,31,32 In our study, the NSAID use rate was 19.8%, similar to other countries, and pharmacist-led MTM could significantly reduce NSAID use rate in this high risk group of patients which is consistent to other studies.33,34 Pharmacists can help the patients to understand the risks of using NSAIDs, choose a substitutional pain management and further avoid to use NSAIDs, which could prevent renal function deterioration. Our study also found a trend of CKD stage and UPCR improving, which might be attributed to improved medication adherence and reduced NSAID use.
The incidence of MRPs in this study was comparatively lower than that reported in prior research focusing on outpatient nephrology pharmaceutical care.35–37 This reduced incidence can likely be attributed to the comprehensive Clinical Decision Support System (CDSS) implemented in our hospital. The CDSS rigorously evaluates each prescription, scrutinizing potential drug interactions, duplications, renal function-based dosing, and maximum dosage limits, thereby effectively preventing inappropriate prescriptions at the initial stage.38 Additionally, each prescription is required to undergo verification and approval by our pharmacists prior to being administered by nurses or dispensed to patients, which entailed a second review subsequent to the CDSS assessment. As such, the medication review conducted by pharmacists in the PMC functioned as an advanced, tertiary level of scrutiny, further minimizing the likelihood of inappropriate prescriptions.
This study has some limitations. First, this study was performed in a single medical center nephrology clinic in Taiwan. Therefore, this may limit the application of our results to other countries. However, because the results corresponded to studies conducted in different countries, the beneficial effects are probably similar in other clinical settings by the implementation of pharmacist-led MTM. Second, because the MRP data were documented in the electronic medical records by pharmacists, inadvertent omissions were likely to occur due to time constraints. Therefore, the actual count of MRPs identified by pharmacists may surpass what is documented in this study. This discrepancy arises, for instance, from the pharmacists’ recommendations for modifying prescriptions prescribed by external physicians which cannot document in our ambulatory recording system. Such modifications include dosage adjustments based on renal function (eg, for atenolol), advising against certain medications like metformin due to deteriorating renal function, or suggesting more suitable medications, such as SGLT2 inhibitors, to slow renal function decline. Therefore, it is plausible that the tangible impact and benefits of MTM are potentially undervalued or underestimated in our results. Third, the follow-up time of medication adherence, NSAID use rate and renal function is relatively short (~3 month), long term follow-up is warranted to confirm the persistent effect of pharmacist intervention. Last, the retrospective design of our study and the small sample size present challenges in definitively attributing the observed decrease in CKD stage and proteinuria improvements solely to pharmacist intervention. Additional studies are essential to conclusively determine the clinical impact of such interventions.
Conclusion
Pharmacist-led MTM can enhance medication adherence and reduce NSAID usage rates in pre-ESRD patients, which might consequently lead to an improvement in renal function.
Acknowledgments
We would like to express our gratitude to the case managers for their assistance in facilitating the referral of patients to the pharmacist clinic for pharmaceutical care.
We would also like to extend our thanks to the National Health Insurance for their reimbursement of pharmaceutical care 4 times annually. This enables patients to receive optimal pharmaceutical management and enhance pharmacist role in Pre-ESRD care.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl. 2022;12(1):7–11. doi:10.1016/j.kisu.2021.11.003
2. United States Renal Data System. USRDS annual data report: epidemiology of kidney disease in the United States; 2022. Available from: https://adr.usrds.org/2022.
3. Cockwell P, Fisher LA. The global burden of chronic kidney disease. Lancet. 2020;395(10225):662–664. doi:10.1016/S0140-6736(19)32977-0
4. Schmidt IM, Hubner S, Nadal J, et al. Patterns of medication use and the burden of polypharmacy in patients with chronic kidney disease: the German chronic kidney disease study. Clin Kidney J. 2019;12(5):663–672. doi:10.1093/ckj/sfz046
5. Tangkiatkumjai M, Walker DM, Praditpornsilpa K, Boardman H. Association between medication adherence and clinical outcomes in patients with chronic kidney disease: a prospective cohort study. Clin Exp Nephrol. 2017;21(3):504–512. doi:10.1007/s10157-016-1312-6
6. Tesfaye WH, McKercher C, Peterson GM, et al. Medication adherence, burden and health-related quality of life in adults with predialysis chronic kidney disease: a prospective cohort study. Int J Environ Res Public Health. 2020;17(1):371. doi:10.3390/ijerph17010371
7. Griffin BR, Wendt L, Vaughan-Sarrazin M, et al. Nephrotoxin exposure and acute kidney injury in adults. Clin J Am Soc Nephrol. 2023;18(2):163–172. doi:10.2215/CJN.0000000000000044
8. Luyckx VA, Tuttle KR, Garcia-Garcia G, et al. Reducing major risk factors for chronic kidney disease. Kidney Int. 2017;7(2):71–87. doi:10.1016/j.kisu.2017.07.003
9. Wehling M. Non-steroidal anti-inflammatory drug use in chronic pain conditions with special emphasis on the elderly and patients with relevant comorbidities: management and mitigation of risks and adverse effects. Eur J Clin Pharmacol. 2014;70(10):1159–1172. doi:10.1007/s00228-014-1734-6
10. Parvez MK, Rishi V. Herb-drug interactions and hepatotoxicity. Curr Drug Metab. 2019;20(4):275–282. doi:10.2174/1389200220666190325141422
11. Britza SM, Byard RW, Musgrave IF. Traditional Chinese medicine-associated nephrotoxicity and the importance of herbal interactions–An overview. Pharmacol Res Mod Chin Med. 2022;3:100099. doi:10.1016/j.prmcm.2022.100099
12. Levin A, Stevens PE, Bilous RW, et al.; Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3(1):1–150.
13. Macedo E, Bihorac A, Siew ED, et al. Quality of care after AKI development in the hospital: consensus from the 22nd Acute Disease Quality Initiative (ADQI) conference. Eur J Intern Med. 2020;80:45–53. doi:10.1016/j.ejim.2020.04.056
14. de Boer IH, Khunti K, Sadusky T, et al. Diabetes management in chronic kidney disease: a consensus report by the American Diabetes Association (ADA) and kidney disease: improving global outcomes (KDIGO). Diabetes Care. 2022;45(12):3075–3090. doi:10.2337/dci22-0027
15. Shivaprasad S, Mateti UV, Shenoy P, Shastry CS, Dharmagadda S. Clinical pharmacists’ scope of knowledge for medication therapy management in chronic kidney disease patients. Pharm Educ. 2021;21(1):781–788. doi:10.46542/pe.2021.211.781788
16. Al Raiisi F, Stewart D, Fernandez-Llimos F, Salgado TM, Mohamed MF, Cunningham S. Clinical pharmacy practice in the care of chronic kidney disease patients: a systematic review. Int J Clin Pharm. 2019;41(3):630–666. doi:10.1007/s11096-019-00816-4
17. Khokhar A, Khan YH, Mallhi TH, et al. Effectiveness of pharmacist intervention model for chronic kidney disease patients; a prospective comparative study. Int J Clin Pharm. 2020;42(2):625–634. doi:10.1007/s11096-020-00982-w
18. Lin MY, Chang MY, Wu PY, et al. Multidisciplinary care program in pre-end-stage kidney disease from 2010 to 2018 in Taiwan. J Formos Med Assoc. 2022;121 Suppl 1:S64–S72. doi:10.1016/j.jfma.2021.12.008
19. Kripalani S, Risser J, Gatti ME, Jacobson TA. Development and evaluation of the Adherence to Refills and Medications Scale (ARMS) among low-literacy patients with chronic disease. Value Health. 2009;12(1):118–123. doi:10.1111/j.1524-4733.2008.00400.x
20. Hayward S, Hole B, Denholm R, et al. International prescribing patterns and polypharmacy in older people with advanced chronic kidney disease: results from the European Quality study. Nephrol Dial Transplant. 2021;36(3):503–511. doi:10.1093/ndt/gfaa064
21. Kimura H, Tanaka K, Saito H, et al. Association of polypharmacy with kidney disease progression in adults with CKD. Clin J Am Soc Nephrol. 2021;16(12):1797–1804. doi:10.2215/CJN.03940321
22. van Oosten MJ, Logtenberg SJ, Hemmelder MH, et al. Polypharmacy and medication use in patients with chronic kidney disease with and without kidney replacement therapy compared to matched controls. Clin Kidney J. 2021;14(12):2497–2523. doi:10.1093/ckj/sfab120
23. Seng JJB, Tan JY, Yeam CT, Htay H, Foo WYM. Factors affecting medication adherence among pre-dialysis chronic kidney disease patients: a systematic review and meta-analysis of literature. Int Urol Nephrol. 2020;52(5):903–916. doi:10.1007/s11255-020-02452-8
24. Santoro A, Perrone V, Giacomini E, Sangiorgi D, Alessandrini D, Degli Esposti L. Association between hyperkalemia, RAASi non-adherence and outcomes in chronic kidney disease. J Nephrol. 2022;35(2):463–472. doi:10.1007/s40620-021-01070-6
25. Cedillo-Couvert EA, Ricardo AC, Chen J, et al. Self-reported medication adherence and CKD progression. Kidney Int Rep. 2018;3(3):645–651. doi:10.1016/j.ekir.2018.01.007
26. Tesfaye WH, Erku D, Mekonnen A, et al. Medication non-adherence in chronic kidney disease: a mixed-methods review and synthesis using the theoretical domains framework and the behavioural change wheel. J Nephrol. 2021;34(4):1091–1125. doi:10.1007/s40620-020-00895-x
27. Anderson LJ, Nuckols TK, Coles C, et al. A systematic overview of systematic reviews evaluating medication adherence interventions. Am J Health Syst Pharm. 2020;77(2):138–147. doi:10.1093/ajhp/zxz284
28. Mechta Nielsen T, Frojk Juhl M, Feldt-Rasmussen B, Thomsen T. Adherence to medication in patients with chronic kidney disease: a systematic review of qualitative research. Clin Kidney J. 2018;11(4):513–527. doi:10.1093/ckj/sfx140
29. Zhang X, Donnan PT, Bell S, Guthrie B. Non-steroidal anti-inflammatory drug induced acute kidney injury in the community dwelling general population and people with chronic kidney disease: systematic review and meta-analysis. BMC Nephrol. 2017;18(1):256. doi:10.1186/s12882-017-0673-8
30. Jeon N, Park H, Segal R, Brumback B, Winterstein AG. Non-steroidal anti-inflammatory drug-associated acute kidney injury: does short-term NSAID use pose a risk in hospitalized patients? Eur J Clin Pharmacol. 2021;77(9):1409–1417. doi:10.1007/s00228-021-03121-0
31. Seager JM, Hawkey CJ. ABC of the upper gastrointestinal tract: indigestion and non-steroidal anti-inflammatory drugs. BMJ. 2001;323(7323):1236–1239. doi:10.1136/bmj.323.7323.1236
32. Ljung R, Lu Y, Lagergren J. High concomitant use of interacting drugs and low use of gastroprotective drugs among NSAID users in an unselected elderly population: a nationwide register-based study. Drugs Aging. 2011;28(6):469–476. doi:10.2165/11589070-000000000-00000
33. Pai AB. Keeping kidneys safe: the pharmacist’s role in NSAID avoidance in high-risk patients. J Am Pharm Assoc. 2015;55(1):e15–23; quiz e24–5. doi:10.1331/JAPhA.2015.15506
34. Rashid R, Chang C, Niu F, et al. Evaluation of a pharmacist-managed nonsteroidal anti-inflammatory drugs deprescribing program in an integrated health care system. J Manag Care Spec Pharm. 2020;26(7):918–924. doi:10.18553/jmcp.2020.26.7.918
35. Cypes IN, Prohaska ES, Melton BL. Pharmacist impact on medication dosing and billable coding accuracy in outpatients with chronic kidney disease. J Am Pharm Assoc. 2021;61(2):e153–e158. doi:10.1016/j.japh.2020.10.009
36. Schutze A, Hohmann C, Haubitz M, Radziwill R, Benohr P. Medicines optimization for patients with chronic kidney disease in the outpatient setting: the role of the clinical pharmacist. Int J Pharm Pract. 2021;29(6):587–597. doi:10.1093/ijpp/riab033
37. van Berlo-van de Laar IRF, Sluiter HE, Riet EV, Taxis K, Jansman FGA. Pharmacist-led medication reviews in pre-dialysis and dialysis patients. Res Social Adm Pharm. 2020;16(12):1718–1723. doi:10.1016/j.sapharm.2020.02.006
38. Roumeliotis N, Sniderman J, Adams-Webber T, et al. Effect of electronic prescribing strategies on medication error and harm in hospital: a systematic review and meta-analysis. J Gen Intern Med. 2019;34(10):2210–2223. doi:10.1007/s11606-019-05236-8
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
