Back to Journals » Patient Preference and Adherence » Volume 18
The Effect of Health Literacy on Disease Management Self-Efficacy in Chronic Disease Patients: The Mediating Effects of Social Support and the Moderating Effects of Illness Perception
Authors Zou H , Liu J, Jiang D, Hou L, Wang W, Zhang L
Received 30 October 2023
Accepted for publication 1 March 2024
Published 12 March 2024 Volume 2024:18 Pages 657—666
DOI https://doi.org/10.2147/PPA.S447320
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Hao Zou,1 Jianrong Liu,1 Dongxu Jiang,2 Linlin Hou,3 Weiliang Wang,4 Linlin Zhang5
1Nursing Department, The Second Affiliated Hospital of Xi’an Medical University, Shanxi, People’s Republic of China; 2Department of Nursing, Harbin Medical University, Heilongjiang, People’s Republic of China; 3Nursing Department, The second Affiliated Hospital of Xi’an Jiaotong University, Shanxi, People’s Republic of China; 4Nursing Department, Xuzhou Medical university, Jiangsu, People’s Republic of China; 5Department of Nursing, School of Pharmacy, Changzhou University, Jiangsu, People’s Republic of China
Correspondence: Jianrong Liu; Linlin Zhang, Email [email protected]; [email protected]
Purpose: To test a hypothetical pathway model to estimate the links between health literacy, social support, illness perception, and disease management self-efficacy.
Methods: This cross-sectional study, conducted from June to October 2022, involved the recruitment of 210 patients with chronic diseases at two primary care facilities. Participants completed the Health Literacy Management Scale, Self-Efficacy for Managing Chronic Disease 6-Item Scale, Social Support Rating Scale and Brief Illness Perception Questionnaire. We used the PROCESS macro for R to determine the hypothetical pathway model.
Results: The direct effect of health literacy on self-efficacy was significant (β=0.1792, 95% CI: 0.0940– 0.2644), and social support played a partial mediating role between health literacy and self-efficacy (ES=0.0761, 95% CI: 0.0398– 0.1204). Illness perception moderated the relationship between social support and self-efficacy (β=− 0.0153, 95% CI: − 0.0268- − 0.0039).
Conclusion: Proposed a conceptual model including the mediating effect of social support and the moderating effect of illness perception, which helps to clarify the underlying mechanisms between health literacy and self-efficacy.
Keywords: health literacy, self efficacy, moderated mediation analysis
Introduction
A well-known key approach to scientifically manage chronic diseases, reduce morbidity and mortality, reduce health care expenditures, and improve the quality of life of chronic disease patients is to encourage patients to self-manage. This process requires patients to conduct behavior management of their lifestyle, physiology, psychology and other aspects to reduce the adverse effect of disease.1 Studies have shown that self-management plays a positive role in maintaining and improving patients’ health behaviors and conditions, as well as in reducing healthcare service utilization rates.2 Therefore, an increasing number of researchers are interested in identifying the factors that determine self-management ability.
Health literacy is considered to be the core basis for determining self-management ability and is significantly associated with patient health outcomes.3–5 The Institute of Medicine of the National Academies defines Health literacy as the ability to obtain, understand and process health-related information.6 Nutbeam believes that it comprises functional, communicative, and critical literacy in ascending order of difficulty.7 Functional literacy refers to reading and writing skills; interactive literacy refers to the ability to extract meaning from different sources of information and share information; and critical literacy refers to the ability to analyze health information obtained using critical thinking.5,7 These skills are necessary for patients to understand symptoms and problems, make appropriate health decisions and act accordingly.
Paasche-Orlow and Wolf proposed a framework for health literacy and health outcomes and hypothesized that self-efficacy might link health literacy and self-management behaviors.8 Self-efficacy refers to an individual’s confidence in his or her ability to complete tasks.9 Abundant evidence has shown that self-efficacy can independently predict self-management behavior.10–12 Health literacy and self-efficacy play an important role in patient self-management as they provide the foundational skills to implement self-management for patients and reinforce their general belief in their ability to overcome difficulties and complete tasks. However, different results have emerged regarding the impact of health literacy on self-efficacy. Several studies have found that health literacy can improve patients’ self-management through the role of self-efficacy. Patients with higher health literacy may have more confidence in their own abilities, which may ultimately have a positive effect on self-management. For example, among elderly diabetic patients in Iran, self-efficacy was linked to medication adherence and physical activity, with health literacy being a predictive factor of self-efficacy.13 Similarly, a study in the United States indicated that self-efficacy mediates the relationship between health literacy and adherence to diabetes medication. Patients with higher numeracy skills may exhibit elevated levels of self-efficacy, which in turn result in a higher level of diabetes medication adherence and a lower level of glycated hemoglobin.14 However, other studies have not confirmed this relationship between health literacy, self-efficacy and health outcomes.5,15 These inconsistent conclusions may be attributed to different measurement tools or ignoring other variables that may affect the specific direction of the relationship between health literacy and self-efficacy.
Social support is a promising mediating variable to explain the relationship between health literacy and self-efficacy. Social support generally refers to the social resources or help that persons perceive and receive, which can be reflected in three aspects: the perception of support, the provision of support and the structure of social networks.16 Studies have shown that good social support means having a reliable social network (such as family and friends) and being able to make full use of these resources to alleviate the negative emotions caused by the disease, thereby increasing patients’ confidence in engaging in healthy behaviors.17–19 A previous study showed that low health literacy is associated with lower social networks and may lead to the loss of necessary social support.20 Liu’s study recently supported this finding:16 people with lower health literacy are more likely to hide their plight and avoid social interactions, while people with better health literacy are more likely to receive sufficient support and devote their resources to solving their health problems. In the Geboers et al study, older adults with low health literacy were associated with loneliness, low participation in social activities, and few regular social contacts, which limited their ability to maintain social networks and may have lost some social support.21
Illness perception plays a key role in chronic disease management. Illness perception refers to the emotions and thoughts that individuals form about their disease, and maintaining or developing positive illness perceptions can enhance disease management self-efficacy.22 A cohort study of managed rehabilitation in trauma patients showed that patients’ confidence in their adherence to rehabilitation exercise varied by different levels of illness perception; maintaining a negative illness perception undermined patients’ confidence in their adherence to exercise.23 In addition, the level of illness perception differs with different levels of social support. Studies have shown24,25 that patients with high social support seem to have more positive illness perceptions than patients with low support because they show better emotional control and perceive less pain caused by the disease. Generally speaking, disease management self-efficacy tends to be weaker in individuals with negative illness perception but stronger in individuals with high social support. This connection has attracted our attention: can social support also significantly improve the self-efficacy of individuals with negative illness perception?
Although many studies have been interested in the relationship between health literacy, self-efficacy and self-management, few have focused on the factors that link health literacy and self-efficacy. Therefore, this study aimed to explore the link between health literacy, social support, illness perception and self-efficacy, which is of great significance for developing specific interventions to improve patients’ self-efficacy and thus their self-management abilities. Based on the above findings, we hypothesized that (H1) health literacy is related to self-efficacy; (H2) social support has a mediating effect between health literacy and self-efficacy; and (H3) illness perception has a moderating effect between social support and self-efficacy.
Methods
Study Design and Sample
A cross-sectional survey was performed in this study by using convenience sampling. Participants were recruited from a community hospital in Daqing City and a health center in Lanxi County from June to October 2022. Participants were invited to participate in the study after their physical examination or visit. The inclusion criteria were adult patients who (i) currently suffered from at least 1 chronic disease, (ii) had a disease duration ≥ 3 months, and (iii) provided written informed consent. Patients were excluded if they met one of the following criteria: (i) nonchronic diseases (eg, acute inflammation, fractures) or (ii) aphasia, deafness, dementia, depression, or taking antidepressants. Chronic disease in this study refers to the presence of any disease or condition that has lasted for three months or longer and may worsen over time. To minimize potential confounders and ensure the reliability of the results, patients with dementia and depression were excluded from the study.
After obtaining the consent of the participants and their caregivers, face-to-face interviews were conducted with the participants to understand their general information, including age, education level, and current diseases. The participants were then introduced to the instructions for filling out the scale and allowed to complete the scale by themselves. If participants were unable to complete the scales themselves, researchers read each scale item and recorded their responses. All data were collected one-on-one with the investigator. Consent for the study was obtained from the ethics committee of the Daqing campus of Harbin Medical University (HMUDQ20211210003) and conducted in compliance with the ethical guidelines of the Declaration of Helsinki.
Measures
Health Literacy
HL was measured using the Health Literacy Management Scale (HeLMS) developed by Jordan et al and translated into Chinese by Sun et al26,27 It is the most commonly used scale to evaluate the level of health literacy in patients with chronic diseases. The HeLMS comprehensively evaluates three skills of health literacy, including 24 items in 4 domains: information acquisition ability, communication interaction ability, health improvement willingness, and economic support willingness. Examples of items included “understanding the doctor’s orders”, “reading usage information of medications”, “evaluating and discerning health information encountered”, “inquiring about unclear aspects of treatment with the doctor”, “discussing health problems with others”, “willing to invest time and resources in health problems”, etc. These items are rated on a five-point Likert scale (from 1 to 5). The higher scores are, the better the respondent’s health literacy. The Cronbach’s α of HL in this study was 0.920.
Self-Efficacy
SE was measured using the Self-Efficacy for Managing Chronic Disease 6-Item Scale (SES6) developed by Lorig et al,28 which measures multiple aspects of self-efficacy, including emotional control, communication with doctors, symptom management, role function, and perceived adaptability to different aspects of chronic diseases, such as pain, fatigue, and trust. Each item is scored from 1 (no confidence at all) to 10 (full confidence). The final score for SES6 was the total sum of the scores of the six items. A higher number indicated higher SE. The Cronbach’s α of the SE in this study was 0.916.
Social Support
SS was measured using the Social Support Rating Scale (SSRS) developed by Xiao,29 which is a commonly used assessment tool for social support in China. The SSRS includes 10 items and 3 dimensions: objective support, subjective support and support utilization. The items included “residential situation in the recent year (living with family or friends, living alone, living with strangers)”, “sources of solace and concern during times of distress”, “relationship with neighbors and colleagues”, “level of support and care received from family”, “frequency of participation in group activities”, “methods of seeking help faced with troubles” and so on. Higher subscale and total scores indicating better social support. The Cronbach’s α of the SS in this study was 0.705.
Illness Perception
IP was measured using the Brief Illness Perception Questionnaire (BIPQ) developed by Broadbent et al.30 The Brief IPQ consists of 9 items. The first 8 items evaluate the following dimensions: identity (symptoms), timeline, consequences, control, emotions, concerns, and illness understanding. The last item is an open-ended response item asking the participants to list the three most important factors that they perceive as causes of their illness. Items 1–8 are measured with a 0–10 Likert-type response scale. The total score ranges from 0 to 80 points. A higher BIPQ score indicates a greater perceived psychological burden of illness. The Cronbach’s α of the IP in this study was 0.788.
Data Analysis
Descriptive statistics (mean, standard deviation, median, interquartile range and frequency distributions) were conducted to show the demographic characteristics. Independent t-tests and analysis of variance (ANOVA) were used to examine the differences in self-efficacy by sample characteristics. Pearson correlation and Spearman correlation analysis were used to examine the relationship between variables.
In our conceptual model (Figure 1), path c represents the total effect of the predictor variable health literacy on the outcome variable self-efficacy. The total effect includes the direct effect of health literacy on self-efficacy (path c’) and the indirect effect on self-efficacy through social support (path a*b).
The mediation and moderated mediation models were analyzed using the PROCESS macro 4.0.1 for R compiled by Hayes (http://processmacro.org/index.html). The bias corrected 95% confidence interval (CI) was calculated with 5000 bootstrapping resamples. First, we tested whether the association between health literacy and self-efficacy was mediated by social support using Model 4. If the 95% CI of the indirect effect (path a*b) did not contain 0, it indicated that the mediating effect was significant. Next, Model 14 was used to test whether illness perception has a moderating effect on path b. Likewise, if the 95% CI of the interaction did not contain 0, a significant moderated mediation effect could be established. Finally, simple slope analyses were used to aid interpretation of the interaction plots. All statistical analyses were conducted using R-Studio. Statistical significance was defined as a two-tailed p value of <0.05.
Results
Sociodemographic Characteristics and Self-Efficacy
A total of 210 patients with chronic diseases participated in this study. Of these, 46% had more than one disease. Most patients had cardiovascular and cerebrovascular diseases (117 cases), and the fewest patients had rheumatic immune diseases (13 cases). The median age of participants was 63 years. Most of the participants were married (92%), had a primary school education or below (43%), had a per capita monthly household income of 3000–5000 yuan (38%), and currently lived in rural areas (56%). After data analysis, it was found that there were significant differences in the self-efficacy scores of participants with different ages, education levels, monthly household income, residence and multimorbidity (all P<0.01) (Table 1).
 |
Table 1 Sociodemographic Characteristics and the Distribution of Self-Efficacy (n=210) |
Bivariate Correlations Among All the Variables
Correlation analysis showed that health literacy was significantly positively correlated with social support (r=0.395, P<0.01) and self-efficacy (r=0.479, P<0.01). Social support was significantly positively correlated with self-efficacy (r=0.528, P<0.01). However, illness perception was not significantly associated with health literacy or self-efficacy (Table 2).
 |
Table 2 Statistical Description and Related Analysis Results |
Mediation Analyses
The regression results (Table 3) show that the total effect (path c) of health literacy on self-efficacy is significant (β=0.2553, P<0.01) after controlling for age, education level, monthly household income, residence and multimorbidity. In addition, the significant coefficients of path a (β=0.1393, P<0.01) indicate that there is a significant correlation between health literacy and social support. Similarly, the significant coefficients of b (β=0.5464, P<0.01) indicate that there is a significant correlation between social support and self-efficacy.
 |
Table 3 Mediation Analysis |
Bootstrap analysis was used to further test the mediation effect. The results show that the direct effect of health literacy on self-efficacy is significant (Boot 95% CI=0.0940~0.2644). The mediating effects of social support (path a*b=0.0761, Boot 95% CI=0.0398~0.1204) are also significant (Table 4).
 |
Table 4 Bootstrap Analysis for Total, Direct, and Mediation Effects |
Moderated Mediation Analyses
The regression results (Table 5) show that health literacy (β=0.1793, P<0.01) and social support (β=0.5147, P<0.05) can significantly affect self-efficacy, and health literacy can significantly affect social support (β=0.1393, P<0.01), indicating that health literacy can affect self-efficacy through the mediating effect of social support. Finally, the product term of illness perception and social support (β=−0.0153, P<0.01) has a significant effect on self-efficacy (Figure 2).
 |
Table 5 Moderated Mediation Analysis |
 |
Figure 2 The final moderated mediation model. Note: **P<0.01. |
The mediating effect size and 95% Bootstrap CI of social support are calculated when the mean of illness perception minus one standard deviation, the mean, and the mean plus one standard deviation, respectively (Table 6). Specifically, the mediating effect of social support between health literacy and self-efficacy is moderated by illness perception, and the mediating effect is weakened with the increase in illness perception (the corresponding 95% Boot CI did not contain 0). Figure 3 visually shows the effect of social support on self-efficacy in patients with different illness perceptions. The line for patients with low illness perception is steeper, indicating that social support is more predictive of self-efficacy in patients with low disease perception.
 |
Table 6 The Mediating Effect of Social Support on Different Levels of Illness Perception |
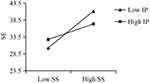 |
Figure 3 Moderating effects of illness perception on the relationship between social support and self-efficacy. Abbreviations: IP, illness perception; SS, social support. |
Discussion
This research found that among these three variables (HL, SP and SE), any two groups of variables are related and, as expected, social support plays a partial mediating role between health literacy and self-efficacy. Furthermore, illness perception can modulate the second half of the mediating process of social support in health literacy and self-efficacy. Hypotheses 1, 2, and 3 were proven.
Both health literacy and self-efficacy can promote patients to be more active and better at managing their disease and maintaining health.31 But health literacy plays a more foundational role in self-management, as they are necessary skills to improve one’s health, such as mastering the correct way of taking medicines, consulting doctors about exercise methods that improve symptoms, and analyzing the correctness of health information obtained.7,32 Mastering these skills increases the likelihood of successfully managing one’s own disease.33,34 The formation of self-efficacy is influenced by direct experience (past experience of self-success or failure), indirect experience (demonstration of others, role model), and verbal persuasion (persuading to have the ability to complete a certain task).35 Therefore, in terms of self-management, individuals with high health literacy may have more successful direct experience to improve their confidence in self-management. The health literacy scale used in the study assesses not only functional and critical literacy but also interactive literacy, which is defined as the ability to communicate with others in daily life to gain information about one’s own health.7 Due to age and disease, older adults with chronic diseases have gradually narrowed their social circles and reduced their social networks and support.20 However, patients with high health literacy indicate a higher ability to communicate with others, which may increase the times of interactions with others, thereby helping them to better reshape their social networks and increase sources of social support. As mentioned above, more support from family, friends or society may increase an individual’s indirect experience and exposure to more verbal persuasion about engaging in healthy behaviors, thus improving the individual’s self-efficacy. The above discussion may explain the link between health literacy and self-efficacy and the mediating role played by social support. Of course, the causal link between these variables still needs to be verified in the future through specialized study designs.
Another key finding of this study is that illness perception can moderate the relationship between social support and self-efficacy. Specifically, compared with patients with low illness perception, the effect of social support on the self-efficacy of disease management is attenuated in patients with high illness perception. High illness perception means that patients perceive more threats from disease and show more negative emotions such as worry, fear and depression.36 Emotional support from social network members (family, friends, etc.) can alleviate patients’ physical and mental discomfort caused by the disease, encourage patients to actively cope with the disease, and improve their confidence in coping with the disease.37 However, negative illness perception is often accompanied by the deterioration of the disease.38 At this time, the physical discomfort experience intensifies, and negative emotions increase. Only a small part of this physical and mental pain is compensated by the emotional support of family members or friends, and pain reduces patients’ ability to manage the disease. Assessing differences in illness perceptions among people with chronic diseases is important because these differences can be used to guide community interventions. The complex relationship among social support, self-efficacy, and illness perception indicates that a single social support intervention may not significantly improve self-efficacy in groups with high illness perception. Integrated and personalized strategies are waiting to be developed.
We constructed a conceptual model with health literacy as the foundation, social support as the core, and illness perception as the entry point. This pathway model linking different concepts can help to optimize the design of interventions to improve patient outcomes. Overall, the health literacy and social support of patients in this study were at a moderate level, but confidence in their own disease management was not strong, suggesting that particular attention should be paid to moderating effect of illness perception on self-efficacy. Based on these findings of this study, We suggest that community nurses build a free communication platform for patients with chronic diseases to strengthen nurse-patient communication and improve patients’ health literacy and social support. In addition, special attention should be paid to nursing psychological education of comorbid patients to make up for the fact that single social support or disease education cannot significantly improve the self-efficacy of patients with high illness perception.
Limitations
First, this is a cross-sectional study, so it cannot explain cause-and-effect relationships between variables. Second, all participants were from primary care settings in China. It is unclear whether the findings can be generalized to patients from other regions. Finally, the participants in our study were all patients who spontaneously visited a doctor or underwent a physical examination. Those who were unable to ambulate freely due to illness were excluded, which may have led to potential sample selection bias. Some patients received help from researchers in completing the questionnaire, which may have affected the authenticity of the questionnaire results.
Conclusion
In this study, we found that health literacy can directly affect disease management self-efficacy and can indirectly affect self-efficacy through the mediating effect of social support. In addition, the predictive role of social support on self-efficacy was attenuated in patients with high illness perception.
Acknowledgment
We thank all the participants in this study.
Funding
The study was financially supported by the Research Fund of Changzhou University (ZMF22020015).
Disclosure
The authors have no conflicts of interest to report in this work.
References
1. Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2013;26(1):1–7. doi:10.1207/S15324796ABM2601_01
2. Fu D, Fu H, McGowan P, et al. Implementation and quantitative evaluation of chronic disease self-management programme in Shanghai, China: randomized controlled trial. Bull World Health Organ. 2003;81(3):174–182. PMCID: PMC2572423.
3. Geboers B, de Winter AF, Spoorenberg SL, Wynia K, Reijneveld SA. The association between health literacy and self-management abilities in adults aged 75 and older, and its moderators. Qual Life Res. 2016;25(11):2869–2877. doi:10.1007/s11136-016-1298-2
4. Wu WL, Yu LW, Wu L. Health literacy and health outcomes in China’s floating population: mediating effects of health service. BMC Public Health. 2021;8. doi:10.1186/s12889-021-10662-7
5. Lee YJ, Shin SJ, Wang RH, Lin KD, Lee YL, Wang YH. Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitus. Patient Educ Couns. 2016;99(2):287–294. doi:10.1016/j.pec.2015.08.021
6. Institute of Medicine (US). Committee on Health Literacy. Health Literacy: A Prescription to End Confusion. Washington (DC): National Academies Press (US); 2004.
7. Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21 st century. Health Promot Int. 2000;15(3):259–267. doi:10.1093/heapro/15.3.259
8. Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31(Suppl 1):S19–S26. doi:10.5555/ajhb.2007.31.supp.S19
9. Bandura A. Social cognitive theory: an agentic perspective. Ann Rev Psychol. 2001;52(1):1–26. doi:10.1146/annurev.psych.52.1.1
10. Lim KE, Kim SR, Sung YH, Oh SY, Kim MS, Chung SJ. Factors influencing self-management in Parkinson’s disease: a cross-sectional study. Geriatr Nurs. 2020;41(3):254–260. doi:10.1016/j.gerinurse.2019.10.005
11. Suarilah I, Lin CC. Factors influencing self-management among Indonesian patients with early-stage chronic kidney disease: a cross-sectional study. J Clin Nurs. 2022;31(5–6):703–715. doi:10.1111/jocn.15930
12. Tsamlag L, Wang H, Shen Q, et al. Applying the information-motivation-behavioral model to explore the influencing factors of self-management behavior among osteoporosis patients. BMC Public Health. 2020;20(1). doi:10.1186/s12889-020-8292-x
13. Roshan AG, Hosseinkhani SN, Norouzadeh R. Health literacy and self-efficacy of the elderly with diabetes. J Diabetes Metab Disord. 2023;22(1):611–617. doi:10.1007/s40200-023-01181-w
14. Huang YM, Shiyanbola OO, Chan HY. A path model linking health literacy, medication self-efficacy, medication adherence, and glycemic control. Patient Educ Couns. 2018;101(11):1906–1913. doi:10.1016/j.pec.2018.06.010
15. Fransen MP, von Wagner C, Essink-Bot ML. Diabetes self-management in patients with low health literacy: ordering findings from literature in a health literacy framework. Patient Educ Couns. 2012;88(1):44–53. doi:10.1016/j.pec.2011.11.015
16. Liu Y, Meng H, Conner KO, Qiao M, Liu D. The influence of health literacy and social support on loneliness among patients with severe mental illness in Rural Southwest China. Front Psychol. 2021;12:564–666. doi:10.3389/fpsyg.2021.564666
17. Tovar EG, Dekker RL, Chung ML, et al. Self-efficacy mediates the relationship of depressive symptoms and social support with adherence in patients with heart failure. J Health Psychol. 2016;21(11):2673–2683. doi:10.1177/1359105315583369
18. Al-Dwaikat TN, Rababah JA, Al-Hammouri MM, Chlebowy DO. Social support, self-efficacy, and psychological wellbeing of adults with type 2 diabetes. West J Nurs Res. 2021;43(4):288–297. doi:10.1177/0193945920921101
19. Smallheer BA, Dietrich MS. Social support, self-efficacy, and helplessness following myocardial infarctions. Crit Care Nurs Q. 2019;42(3):246–255. doi:10.1097/CNQ.0000000000000265
20. Yang Y, Zhang B, Meng H, Liu D, Sun M. Mediating effect of social support on the associations between health literacy, productive aging, and self-rated health among elderly Chinese adults in a newly urbanized community. Medicine. 2019;98(16):e15162. doi:10.1097/MD.0000000000015162
21. Geboers B, Reijneveld SA, Jansen CJ, de Winter AF. Health literacy is associated with health behaviors and social factors among older adults: results from the lifelines cohort study. J Health Commun. 2016;21(sup2):45–53. doi:10.1080/10810730.2016.1201174
22. Rahimi Kordshooli K, Rakhshan M, Ghanbari A. The effect of family-centered empowerment model on the illness perception in heart failure patients: a randomized controlled clinical trial. J Caring Sci. 2018;7(4):189–195. doi:10.15171/jcs.2018.029
23. Connolly FR, Aitken LM, Tower M, Macfarlane B. Factors associated with self-efficacy for managing recovery in the trauma intensive care population: a prospective cohort study. Injury. 2014;45(1):272–278. doi:10.1016/j.injury.2013.05.005
24. Ding YM, Liu CP, Xu HX, et al. Effect of social support on illness perception in patients with atrial fibrillation during “Blanking Period”: mediating role of sense of mastery. Nurs Open. 2022;10(1):115–122. doi:10.1002/nop2.1284
25. Weichih Chen D, Tsai YF, Chung SC, Hsu KY, Yeh WL, Chen CY. Development and validation of a caregiving needs inventory for family members before their older relative’s knee joint-replacement surgery. Disabil Rehabil. 2021;43(6):853–860. doi:10.1080/09638288.2019.1643414
26. Jordan JE. Conceptualizing and Measuring Health Literacy from the Patient Perspective [PhD Thesis]. Department of Medicine, Universityof Melbourne; 2009.
27. Sun HL, Peng H, Fu H. The reliability and consistency of health literacy scale for chronic patients. Fudan Univ J Med Sci. 2012;39(3):
28. Lorig K, Stewart A, Ritter P, Gonzalez V, Laurent D, Lynch J. Outcome Measures for Health Education and Other Health Care Interventions. Thousand Oaks CA: Sage Publications; 1996.
29. Xiao SY. Psychological health scale: social support questionnaire. China J Psychol Health. 1998;12:127–131.
30. Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60(6):631–637. doi:10.1016/j.jpsychores.2005.10.020
31. Ong-Artborirak P, Seangpraw K, Boonyathee S, Auttama N, Winaiprasert P. Health literacy, self-efficacy, self-care behaviors, and glycemic control among older adults with type 2 diabetes mellitus: a cross-sectional study in Thai communities. BMC Geriatr. 2023;23(1):297. doi:10.1186/s12877-023-04010-0
32. Leger LS. Health literacy and public health: possibilities and challenges. Health Promotion Int. 2001;16(2):197–205. doi:10.1093/heapro/16.2.197
33. Osborn CY, Paasche-Orlow MK, Bailey SC, Wolf MS. The mechanisms linking health literacy to behavior and health status. Am J Health Behav. 2011;35(1):118–128. doi:10.5993/AJHB.35.1.11
34. Shi D, Li J, Wang Y, et al. Association between health literacy and hypertension management in a Chinese community: a retrospective cohort study. Intern Emerg Med. 2017;12(6):765–776. doi:10.1007/s11739-017-1651-7
35. Bandura A. Social Foundation of Thought and Action: Asocial Cognitive Theory. New Jersey: Prentice-Hall; 1986.
36. Joshi S, Dhungana RR, Subba UK. Illness perception and depressive symptoms among persons with type 2 diabetes mellitus: an analytical cross-sectional study in clinical settings in Nepal. J Diabetes Res. 2015;2015:908374. doi:10.1155/2015/908374
37. Wang L, Luo J, Li Y, Zhou Y, Wang W. Social support, anxiety, and depression in patients with prostate cancer: complete mediation of self-efficacy. Support Care Cancer. 2022;30(8):6851–6856. doi:10.1007/s00520-022-07065-8
38. Guo YC, Yan R, Lv YM. Longitudinal trajectories of illness perceptions among stroke patients and decision tree analysis of core determinants. J Nurs Sci. 2022;37(03):20–24.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

