Back to Journals » ClinicoEconomics and Outcomes Research » Volume 16
The Economic Burden of the COVID-19 Pandemic in State of Kuwait
Authors Nur AM , Aljunid SM , Almari M
Received 21 November 2023
Accepted for publication 28 February 2024
Published 4 March 2024 Volume 2024:16 Pages 111—122
DOI https://doi.org/10.2147/CEOR.S442913
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Dean Smith
Amrizal Muhammad Nur,1 Syed Mohamed Aljunid,2 Mohammad Almari1
1Department of Health Policy and Management, College of Public Health, Health Sciences Center, Kuwait University, Shadadiya, Kuwait; 2Department of Public Health and Community Medicine, International Medical University, Kuala Lumpur, Malaysia
Correspondence: Amrizal Muhammad Nur, Department of Health Policy and Management, College of Public Health, Health Sciences Center, Kuwait University, Shadadiya, Kuwait, Tel +965-55186373, Fax +965-24633632, Email [email protected]
Purpose: The main aim of this study is to estimate the provider’s cost, patients’ cost (home and institutional quarantine cost) and the total economic burden of COVID-19 for patients with PCR positive in Kuwait.
Patients and Methods: This cross-sectional and retrospective study identified the cost incurred for treating COVID-19 inpatients admitted to a General Hospital in Kuwait, a designated COVID-19 treatment center by the Kuwait Government during pandemic. A total of 485 COVID-19 patients were randomly selected from May 1st to September 31st, 2021. Data on sociodemographic information, length of stay (LOS), discharge status, and comorbidities were obtained from the patients’ medical records. A step-down approach was done to estimate the healthcare provider cost per patient per admission. Patient cost (loss of productivity due to hospitalization, institutional and home quarantine) was calculated using human capital approach. The national economic burden of COVID-19 was estimated using costing data from a general hospital for the entire nation. The data were analyzed using the statistical software package SPSS version 25.
Results: In all, 485 COVID-19 patients were involved in the research. KD 2216 (USD 7,344) was the average cost per patient per admission. The ICU accounted for 20.6% of the total cost, the physician and nursing staff for 42.1%, and the laboratory services for 10.2%. The estimated annual cost of care for COVID-19 patients in Kuwait was KD 147.4 (USD 488.5) million, or 5.5% of the MOH budget for 2021, given that 9.03% (383,731) of the population had positive COVID-19 PCR results in 2021. The range of the estimated national economic burden, considering both the best and worst-case scenarios, is KD 73.6 (USD 244.2) million to KD 221.0 (USD 732.7) million.
Conclusion: COVID-19 poses a substantial financial strain on the healthcare system, estimated at 5.9% to 8.8% of the MOH’s annual budget and 0.2% to 0.7% of Kuwait’s GDP in 2021. To mitigate costs, prioritizing prevention and health education is crucial. Targeted strategies, such as workforce optimization, are needed to address high expenses. Policymakers and administrators should leverage these insights for enhanced efficiency and sustainability in future epidemic responses.
Keywords: COVID-19, coronavirus, economic burden, provider costs, patient cost
Introduction
The World Health Organization received its first report on COVID-19 at the end of 2019, which was caused by the newly discovered severe acute respiratory syndrome coronavirus 2 (SARS-CoV2).1 The COVID-19 pandemic was officially declared by the World Health Organization (WHO) on March 11, 2020. Since that time, the illness has been rapidly spreading, impacting over 5 million people, and killing over 350,000, underscoring the threat it poses to the health of the entire world.2 The State of Kuwait officially confirmed three travelers from outside the State of Kuwait had come into contact with the virus on February 24, less than a month later. This marked the beginning of the outbreak within the nation.3 The first COVID-19 patient was admitted to the intensive care unit (ICU) by March 3rd, 2020. Over two months later, the ICU saw the admission of over 100 COVID-19 cases that had been verified.4 The WHO has reported that there have been 614,385,693 confirmed cases of COVID-19 worldwide, including 6,522,600 deaths and 325,602 new cases. There had been 12,677,499,928 vaccination doses given as of September 27, 2022.5 Kuwait was one of the Gulf Cooperation Council (GCC) nations hit by COVID-19 infections, with 658,520 cases and 2,563 fatalities. As of September 30, 2022, WHO reported that 8,214,656 vaccine doses had been administered in Kuwait.6
From an economic standpoint, patients, the health system, and the government have all had to bear significant direct and indirect medical costs as a result of the COVID-19 pandemic, the disease’s complications, and the growing number of patients.7 Regarding the financial strain of direct medical expenses, the expenses fluctuate based on several factors such as the quantity of afflicted individuals, the intensity of the illness, duration of hospitalization, duration of intensive care unit stay, and so on. International studies have demonstrated that COVID-19 patients have medical costs that are significantly higher than those of patients with other infectious diseases.8,9 This is attributed to the higher probability of hospitalization and mortality associated with the virus, particularly for high-risk groups.10 Regarding the need for and associated expenses of special care services for COVID-19 patients, these circumstances are also accurate.11–13
According to statistics, 3% of COVID-19 cases worldwide require special care services due to their critical condition.14 A study conducted in Wuhan, China, on 138 patients infected with COVID-19 revealed that 26.1% of the patients required special care services, with 41.6% and 47.2% of them requiring invasive ventilation as well as non-invasive ventilation.15 88% of patients admitted to the intensive care unit in Lombardy, Italy, received invasive ventilation, while 11% received non-invasive ventilation.16 ICU hospital stays typically have daily costs that are three to four times higher than those of regular wards.17 Furthermore, the disease-related death, forced home rest, or loss of income could all be categorized as indirect costs.18–20 A nation’s Gross Domestic Product (GDP) would decline as a result of the COVID-19 outbreak and the closure of numerous industries.21,22 The global GDP will drop by 2.5–3% per month as a result of the disease’s spread, findings indicate.23 Moreover, the highest fifteen economies in the world have suffered greatly as a result of the COVID-19 pandemic.24 When comparing the economic impact of this illness to that of previous pandemics, it becomes clear that the current global economic crisis is far worse than any previous history. Calculating the economic impact of COVID-19 disease appears vital given the high costs of treating COVID-19 patients, the financial strain this place on the nation’s healthcare system and economy as a whole, and the approaching economic crisis. The essential requirement that will assist physicians, researchers, policy makers, and health planners in managing the pandemic with conflicting priorities is an estimate of the cost of treating COVID-19 infected patients. By examining the resources employed in Kuwaiti healthcare, this study seeks to estimate the economic burden and management costs of COVID-19 infected patients (PCR positive) based on their severity. The doctor in-charge of treating the Covid-19 patient decided the severity level of the disease based on the criteria classification guideline provided by the WHO.
Mild disease: Symptomatic COVID-19 patient without evidence of viral pneumonia or hypoxia.
Moderate disease: Adolescent or adult with clinical signs of pneumonia (fever, cough, dyspnea, fast breathing) but no signs of severe pneumonia, including SpO2 ≥ 90% on room air.
Severe diseases: Adolescent or adult with clinical signs of pneumonia (fever, cough, dyspnea) plus one of the following: respiratory rate > 30 breaths/min; severe respiratory distress; or SpO2 < 90% on room air.
Materials and Methods
To estimate the cost of COVID-19 among patients admitted to a general hospital in Kuwait, a cross-sectional and retrospective study were carried out. The study included patients who were discharged between February 1st and April 30th of 2021, and data collection was conducted between May 1st and September 30th of that same year. The research population consisted of all patients with confirmed COVID-19 cases who were admitted to a general hospital in Kuwait, which is the primary designated hospital for treating COVID-19 patients by MOH Kuwait. With 1,168 beds, this hospital serves a population estimated to be 600,000 and is thought to be the largest in Kuwait and the Middle East. It also has the newest and most sophisticated medical technology. A random sampling procedure has been employed to select 485 patients. This study only included hospitalized COVID-19 patients who tested positive for the virus by PCR. The Kuwait Ministry of Health’s Research and Ethics Committee gave its approval to the study (Approval Code: 1502–2020). There were two types of data collected in this study; 1) Sociodemographic and Clinical data was extracted directly from electronic medical record database such as gender, age, length of stay, discharge status, primary, secondary diagnosis etc. (Appendix-1). 2) Hospital costing data was extracted using hospital costing template from hospital finance department and finance unit in Kuwait MOH (Appendix-2). Meanwhile, there were three types of data collected from patient perspective, such as loss of productivity cost due to hospitalization, home quarantine and institutional quarantine. A General Hospital is a 1,168-bed public hospital run by the Ministry of Health. The government provides full funding for patients under management at this hospital.
Provider Cost (Hospitalization Cost)
The step-down technique was used to conduct a costing analysis. For the hospital costing analysis, adherence was maintained to the standards established by Shepard et al.25 To extract financial information from hospital records, a costing template was provided to the hospital’s finance staff. Three levels of cost centers are identified by the template: final cost centers (all wards and all clinics), intermediate cost centers (eg, radiology, pharmacy), and overhead cost centers (eg, administration, utilities, maintenance). There were 18 cost centers for overhead, 12 cost centers for intermediate, and 31 cost centers for final costs in our costing template. For every cost center, records were kept of the financial outlays and production. The cost of labor, supplies, infrastructure, and machinery is included in the budget for each cost center. The total cost, total number of discharges, total number of inpatient days, total number of outpatient clinic patient visits, and total floor space are among the recoded data. To ensure proper cost allocation, all the data on workload-related activities, including the quantity of discharges, inpatient days, floor space, and outpatient visits, was gathered. While the average useful life of equipment was assumed to be five years, the average useful life of the building was assumed to be twenty years and the depreciation cost of capital asset using a 5% discount rate.25 To estimate the cost for each cost center, both capital costs (such as the cost of the building, equipment, and furniture) and recurrent costs (such as staff salaries and other recurrent costs) were combined. The cost of providing services on a per-patient per-day of stay basis, or unit cost, was then calculated by dividing the final allocated costs for each inpatient cost center by the total units of inpatient days. The cost of care per patient per admission is ultimately calculated by multiplying the unit cost by the length of stay for each individual patient. The burden was estimated using the step-down approach’s unit cost for COVID-19 management. Every expense was translated into US dollars. The conversion’s exchange rate is 1 KD = 3.3142 USD (Year 2021).26
The following formula was used to determine the overall provider cost per patient:
Total Provider costs = mean costs for administration + maintenance cost + store and consumable costs + central sterile services department (CSSD) costs + dietetic and food costs + laundry and linen costs + drug costs + radiology costs + laboratory costs + physiotherapy costs + ICU costs + mean costs for physician and nursing services.
Total Provider costs = 147 (KD) + 21 (KD) + 42 (KD) + 23 (KD) + 35 (KD) + 20 (KD) + 121 (KD) + 83 (KD) + 225 (KD) + 109 (KD) + 457 (KD) + 932 (KD) (Table 1)
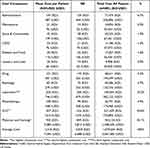 |
Table 1 Components of COVID-19 Patient Treatment Cost |
Total Provider costs per patient per admission = 2,216 (KD) equal to 3,089 (USD) (Table 1)
Computing Provider Cost (Hospitalization Cost)
The average unit cost per patient per admission in the in medical ward of General Hospital was computed using step-down costing approach, amounting KD 2216 (USD 7344). Then, multiplying this average cost by the number of COVID-19 inpatients with PCR positive in the year 2021 (14,518 cases) calculates the total provider costs on hospitalization. The total provider costs on hospitalization are calculated as follows:
PCHC = NIC x UC
PCHC = Provider cost (hospitalization cost)
NIC = Number of inpatient cases with PCR positive
UC = unit cost per admission
Provider cost (hospitalization cost)
= 14,518 × KD 2216 (USD 7344) = KD 32,171,888.00 (USD 106,620,192.00) (Table 2)
 |
Table 2 Economic Burden of COVID-19 Epidemic with Positive PCR in the State of Kuwait 2021 |
Computing Provider Cost (Institutional Quarantine Cost)
Due to the lack of information related to the unit cost per day in the institutional quarantine especially in the field hospital, The decision was made to use the lowest unit cost per day of stay in one of the government hospitals in Kuwait as a reference. The cheapest unit cost per day in the medical wards of Mubarak Al-kabeer hospital was found to be KD 183 per day (USD 606.50).27 It was assumed that the unit cost per day of stay in the field hospital is 50% of this cost. So, the daily cost of institutional quarantine in Kuwait was estimated at KD 91.50 (USD 303.25). A total of 3928 cases of institutional quarantine were found to have tested positive for PCR, with an average stay of 14 days.
The Provider cost for institutional quarantine (PCIQC) was calculated as follows:
PCIQC = NIQC × UC × ALOS
PCIQC = Provider cost (Institutional quarantine cost)
NIQC = Number of institutional quarantine cases with PCR positive
UC = unit cost per day in institutional quarantine
ALOS = Average Length of Stay (ALOS) in Institutional quarantine
Institutional quarantine cost = 3928 × KD 91.50 (USD 303.25) × 14 days = KD 5,031,768.00 (USD 16,676,324.00) (Table 2)
Patient Cost (Indirect Cost)
When estimating the loss of productivity due to inpatient hospitalization, institutional quarantine, and home quarantine, the human capital approach was employed. The average income per capita per day for Kuwait in 2021 was calculated by dividing the country’s total income by 365 days.28 The following formula was used to determine the productivity loss resulting from institutional, home, and inpatient quarantines.
Average income per capita per day = Average income per capita in year 2021
Total number of days in year 2021
Income per capita per year (2021) = USD 24,812 (Current USD)
Total number of days per year = 365 days
Average income per capita per day = 24,812 = USD 67.98 (KD 20.51)
365
Total Number of COVID-19 cases with PCR positive admitted in hospitals (in year 2021) was 14,518
Total number of COVID-19 cases with PCR positive in Institutional quarantine (in year 2021) was 3928
Total number of COVID-19 cases with PCR positive in-home quarantine (in year 2021) was 365,285
Average length of stay was 14 days as proposed by WHO.
Computing Loss of Productivity Due to Inpatient Hospitalization
The Loss of Productivity Cost due to inpatient hospitalization (LPC) was calculated as follows:
LPC_IH = NIH × AICD × ALOS
LPC_IH = Loss of productivity cost due to inpatient hospitalization
NIH = Number of inpatient hospitalizations with PCR positive
AICD = Average income per capita per day
ALOS = Average Length of Stay (ALOS) in hospital
Loss of productivity cost due to inpatient hospitalization = 14,518 × KD 20.51 (USD 67.98) × 14 days = KD 4,168,699.00 (USD 13,817,071.00) (Table 2)
Computing Loss of Productivity Cost Due to Institutional Quarantine
The Loss of Productivity Cost due to institutional quarantine (LPC_IQ) was calculated as follows.
LPC_IQ = NIQC × AICD × ALOS
LPC_IQ = Loss of productivity cost due to institutional quarantine
NIQC = Number of institutional quarantine cases with PCR positive
AICD = Average income per capita per day
ALOS = Average Length of Stay (ALOS) in institutional quarantine
Loss of productivity cost due to institutional quarantine = 3928 × KD 20.51 (USD 67.98) × 14 days = KD 1,127,886.00 (USD 3,738,356.00) (Table 2)
Computing Loss of Productivity Cost Due to Home Quarantine
The Loss of Productivity Cost due to home quarantine (LPC_HQ) was calculated as follows:
LPC_HQ = NHQC × AICD × ALOS
LPC_HQ = Loss of productivity cost due to home quarantine
NHQC = Number of home quarantine cases with PCR positive
AICD = Average income per capita per day
ALOS = Average Length of Stay (ALOS) in home quarantine
Loss of productivity cost due to home quarantine = 365,285 × KD 20.51 (USD 67.98) × 14 days = KD 104,887,935.00 (USD 347,649,040.00) (Table 2)
Computing the Economic Burden
The Shlonik data base, which is used to track COVID-19 cases managed by the Preventive Unit of MOH Kuwait, provided estimates for the prevalence of COVID-19 cases with PCR positive, whether treated or isolated in hospital, institutional, and home quarantine, which were used to estimate the national economic burden. The entire economic burden was estimated using the unit cost for managing COVID-19 in hospitals, which was determined using a step-down approach, the unit cost per day for institutional quarantine, and the average daily income per capita.
Total economic burden = Provider cost (the hospitalization cost + institutional quarantine cost) + Patient cost (loss of productivity cost due to hospitalization + loss of productivity cost due to institutional quarantine + loss of productivity cost due to home quarantine).
Sensitivity Analysis
Sensitivity analysis was performed to determine the worst-case and best-case scenarios by adjusting the prevalence and economic burden value. The total economic burden for COVID-19 cases was calculated for the base case, best case, and worst-case cost scenarios as part of the costing scenarios. The entire budget of Kuwait’s Ministry of Health, the cost per GDP of Kuwait, the provider and patient perspectives, and the total economic burden of COVID-19 cases are all calculated in each scenario. Based on the mean economic burden and the total number of COVID-19 cases in the current study, the base case scenario for the overall economic burden was computed. The worst-case cost scenario for COVID-19 was calculated by increasing the disease prevalence 50% of the base case scenario figures. For calculation of the best-case scenario, COVID-19 economic burden was calculated by decreasing the disease prevalence 50% of the base case scenario figures.
Results
Patient Characteristics and Demographics
This study included 485 hospitalized COVID-19 in-patients in total. Eighty-two percent of the patients were older than 40 years. A majority of the patients, comprising 87.0% Kuwaitis, were female (54.6%), mild/moderate (82.1%), severe (17.9%), and either discharged home or recovered (73.4%) (Table 3).
 |
Table 3 COVID-19 Patients’ Demographics and Clinical Outcomes |
Provider Cost (Hospitalization)
As can be seen in Table 4 and Table 1, COVID-19 cases in severe condition cost an average of KD 4,626 (SD = 3,035), or USD 15,332 (SD = 10,060), while COVID-19 inpatients admitted to the ICU cost an average of KD 4,342 (SD = 2,992), or USD 14,392 (SD = 9,914). Compared to mild/moderate and non-ICU cases, the average cost of severe COVID-19 admissions was higher. KD 2,216 (SD = 2,018), or USD 7,344 (SD = 6,688), was the total treatment cost per patient per admission. The average length of stay (ALOS) was 9.4 days (SD = 8.5). The total treatment cost of 485 patients with confirmed COVID-19 (PCR positive) in a General Hospital was KD 1,074,644 equal to USD 3,561,585. There were 12 component cost included in this costing analysis. Physician and nursing care costs (42.1%) accounted for the largest component cost, with KD 452,154, or USD 1,498,529, being the highest. Next came the costs of laboratory investigation (10.2%) at KD 109,264, or USD 362,123, and intensive care (20.6%) at KD 221,439, or USD 733,893.
 |
Table 4 COVID-19 in-Patient Mean Cost by Severity and ICU Category |
Hospital Provider Cost and Indirect Cost
The total annual cost of hospital provider and Institutional quarantine were estimated at KD 32,171,888 (USD 106,620,192) and KD 5,031,768 (USD 16,676,324) respectively. Whereas the total annual indirect cost for loss of productivity due to inpatient hospitalization, institutional quarantine and home quarantine were estimated KD 4,168,699 (USD13,817,071), KD 1,127,886 (USD 3,738,356) and KD 104,887,935 (USD 347,649,040) respectively (Table 2).
Economic Burden
The total number of COVID-19 patient in Kuwait with positive PCR in year 2021 was 383,731. The total annual provider cost was 37,203,656 (KD) equal to 123,296,516 (USD) and the total annual patient or indirect cost was 110,184,520 (KD) equal to 365,204,467 (USD). Furthermore, the estimated total economic cost of COVID-19 was KD 147.4 (USD 488.5) million, or roughly 5.9% of the KD 2.5 (USD 8.3) billion annual budget allocation for the Ministry of Health in 2021. A base-case, a best-case, and a worst-case scenario were created based on the number of COVID-19 cases requiring hospital admission, institutional quarantine, and home quarantine for the purpose of conducting sensitivity analysis. In the worst-case scenario, calculation involved adding 50% of the number of COVID-19 cases with PCR positives that required hospital admission (21,777 patients), institutional quarantine (5,892 patients), and home quarantine (547,928 patients). Based on actual costs or current data, the base-case scenario accounts for hospital admissions (14,518 patients), institutional admissions (3928 patients), and home quarantines (365,285 patients). A 50% reduction in the current prevalence (7,259 patients), institutional quarantine (1964 patients), and home quarantine (182,643 patients) was assumed in the best-case scenario. A range of KD 73.6 (USD 244.2) million to KD 221.0 (USD 732.7) million can be used to estimate the national economic burden in the best-case scenario and the worst-case scenario. Furthermore, in the base case, best case, and worst-case cost scenarios, the impact of COVID-19 on the Kuwait Ministry of Health’s overall budget was approximately 5.88%, 2.94%, and 8.82%, respectively. In addition, the base, best, and worst-case cost scenarios of COVID-19 each accounted for roughly 0.46%, 0.23%, and 0.69% of Kuwait’s current GDP (Table 2).
Discussion
This study includes 485 COVID-19 in-patients who tested positive for the virus on PCR. The average cost of a COVID-19 patient admitted to the intensive care unit (ICU) was KD 4,342 (SD = 2,992), or USD 14,392 (SD = 9,914), while the average cost of a COVID-19 patient with a severe condition was KD 4,626 (SD = 3,035), or USD 15,332 (SD = 10,060). According to this study, patients with more severe COVID-19 had higher healthcare costs than patients with less severe COVID-19 (mild/moderate). This result is consistent with research by Li et al.29 Athanasakis et al.30 Gedik et al31 and Khan et al.32 An ICU admission for a COVID-19 patient also came with a higher average cost than a non-ICU or general ward admission. This study result is consistent with findings from another study conducted in Saudi Arabia, where the ICU and general medical ward costs were 21,173 USD and 11,385 USD, respectively.33 This result is also less than that of a recent study by Shrestha et al (2021) that was carried out in the US and found that the average hospitalization costs per patient were 13,090 USD without an ICU and 21,222 USD with an ICU admission.34
The total treatment cost per patient per admission was KD 2,216 (SD = 2,018), or USD 7,344 (SD=6,688). This is less than the cost reported in Saudi Arabia (12, 547 USD), but it is comparable to the cost in China of 6,827 USD from 70 empirically observed cases. It is also less than that reported in a recent study carried out in the United States by Shrestha et al (2021). According to their report, the estimated cost of hospitalization for each patient was 13,090 USD on average. This result is greater than those of a number of studies by Bartsch et al in the USA, where COVID-19 costs ranged from 2,837 to 3,205 USD; Gedik et al in Turkey, where COVID-19 patients’ mean costs were 882 USD (SD = 667); and Ghaffari Darab et al in Iran,35 where COVID-19 patients’ mean costs were 3,755 USD. Physician and nursing care costs (42.1%) accounted for the largest component cost, with KD 452,154, or USD 1,498,529, being the highest. Next came the costs of laboratory investigation (10.2%) at KD 109,264, or USD 362,123, and critical care (20.6%) at KD 221,439, or USD 733,893. Unlike the Ghaffari Darab study, this highest component cost is comprised primarily of nursing services and intensive care, accounting for 43% of total costs. Nonetheless, Li X-Z’s study found that pharmaceuticals accounted for the majority of costs. Variations in sample size, study duration, cost methodology, and sample member composition could be the cause of the cost discrepancies. When it comes to non-coronavirus situations, there have been notable variations in healthcare delivery unit costs across the globe. On the other hand, these kinds of comparisons can help comprehend the extent of the financial impact on other nations’ health systems as well as the breakdown cost component.
The current study reveals that the average treatment cost per patient per admission for COVID-19 in Kuwait is higher than reported in studies from the USA, Turkey, and Iran. The prominence of physician and nursing care costs underscores the significant contribution of healthcare professionals to the overall cost. These findings emphasize the need for targeted cost-management strategies, potentially involving workforce optimization and further exploration of the factors driving the higher costs in Kuwait. Policymakers and healthcare administrators should consider these insights to enhance the efficiency and sustainability of COVID-19 management in the country if facing the same epidemic in the future.
The estimated annual cost of care or economic burden for COVID-19 patients in Kuwait was KD 147.4 (USD 488.5) million, or roughly 5.8% of the KD 2.5 (USD 8.3) billion annual budget allocation for the Ministry of Health in 2021. Additionally, about 0.46% of Kuwait’s current GDP was attributed to the economic burden of COVID-19.36 Despite a higher percentage of MOH expenditure (5.5%), this finding is less than the total annual cost of COVID-19 in Iran (Darab et al). For inpatient cases, the average direct and indirect costs were undoubtedly 43.1 trillion Rials (USD 2.7 billion), or 1.5% of the average yearly health expenditures in 2018.37 The current financial burden is also less than that of a study conducted in the United States (Bartsch, 2020), which estimated that a 20% infection rate would result in roughly 53.8 million COVID-19 cases with symptoms and a total direct medical cost of USD 163.4 billion.
Assuming a clinical attack rate of 48% and a case fatality ratio of 1.5%, COVID-19 alone would impose a direct health-related economic burden of £39.6 billion (USD 49.1 billion) (1.73% of GDP) on the UK economy. This finding is also lower than that of a study conducted in the UK (Keogh-Brown 2020). The mitigation strategy, which included a 14-day quarantine, social distancing, and a 12-week closure of schools and universities, resulted in a 3.3% increase in the direct health-related economic burden, amounting to £53.1 billion (USD 65.8 billion). The entire macroeconomic cost of the suppression scenario, which included a 14-day quarantine, social distancing, and the permanent closure of schools and universities, was £668.4 billion (USD 628.9 billion), or nearly one-third (29.2%) of the UK GDP in 2020. The current estimate is also less than that of a Russian study that estimated the socioeconomic cost of COVID-19 in the Russian Federation to be 4.6 trillion rubles. (4%) of GDP, or D71.1 billion.38 The range of the national economic burden was found to be KD 73.6 (USD 244.2) million or 2.9 of Kuwait MOH budget or 0.2% of Kuwait National GDP to KD 221.0 (USD 732.7) million or 8.8 of Kuwait MOH budget or 0.7% of Kuwait National GDP. These results were obtained from a sensitivity analysis using the national economic burden estimates based on the best-case scenario (prevalence 4.5%) and the worst-case scenario (prevalence 13.5%). The economic burden of COVID-19 in this study is estimated to be between KD 73.6 million and KD 221.0 million, with corresponding percentages of the Ministry of Health (MOH) budget and the national GDP. The lower end of the range represents a more conservative estimate, while the higher end indicates a potentially larger economic impact. These figures provide insights into the scale of financial resources that may be required to manage and mitigate the effects of the pandemic on the healthcare system and the national economy.
Research Limitations
First, the long-term economic effects of COVID-19 were not captured in the analysis, as only the first three months of the epidemic in 2021 were covered. Second, because of a dearth of information, we were unable to incorporate direct medical expenses (societal costs) from the viewpoint of the patient, such as the price of lost productivity for caregivers of confirmed cases, hospital out-of-pocket expenses for transportation and meals, and over-The-counter medications. The costs of lost productivity as a result of COVID-19 premature mortality and absenteeism from work were not included in our calculations. Third, not all patients suspected of having COVID-19 were tested due to a shortage of PCR tests from January to April 2021. As a result, it’s likely that the number of confirmed cases reported is underestimated. Fourth, it’s possible that the number of working days lost for those who worked from home was overestimated, as the estimate was based on the WHO standard institutional/home quarantine period of 14 days. Fifth, some information about the suspected cases and close contacts was left out and only verified COVID-19 cases were considered. Lastly, we excluded the cost of PPE and vaccinations as well as the mitigation strategy, which included a 14-day quarantine, social distancing, and a 12-week closure of schools and universities. To assess the long-term financial effects of COVID-19 on the healthcare system and comprehensive cost calculations; including mitigation strategy costs, vaccination expenses, personal protective equipment (PPE) costs, COVID-19 treatment expenses in hospitals and primary care centers, societal cost, loss of productivity due to hospitalization, institutional quarantine, and home quarantine) etc., necessitate more advanced research in the future.
Conclusion
This study underscores the substantial impact of ICU admissions on resource usage for severe COVID-19 patients. Higher costs were observed for patients aged 40–79 and those with greater severity. COVID-19 may impose a significant financial burden on Kuwait’s healthcare system, estimated at 5.9–8.8% of the MOH’s yearly budget and 0.2–0.7% of the GDP in 2021. Prioritizing prevention and health education is crucial. The notable contribution of physician and nursing care costs emphasizes the role of healthcare professionals. Addressing these highest costs requires targeted strategies, including potential workforce optimization. Strategic financial planning is vital for managing the pandemic’s impact on the healthcare system and the national economy. Policymakers and healthcare administrators should use these insights to enhance the efficiency and sustainability of COVID-19 management amid future epidemics.
Data Sharing Statement
The General Hospital provides the data that back up the study’s conclusions, but there are limitations on their availability, and they are not made public. However, upon reasonable request and with permission from a Kuwaiti general hospital, data are available from the corresponding author.
Ethical Approval
The study was approved by the Research and Ethics Committee of Kuwait Ministry of Health (The Standing Committee for Coordination of Health and Medical Research) (Approval Code:1502/2020). The study did not require informed consent because the data was extracted from a General Hospital information system database and did not involve interviews of patients, hence the need of informed consent was waived by the Research and Ethics Committee of Kuwait Ministry of Health (The Standing Committee for Coordination of Health and Medical Research). All methods were performed in accordance with the relevant guidelines and regulations or in accordance with the Declaration of Helsinki.
Acknowledgments
We would like to thank Kuwait University Research Sector for providing us with the complete support we needed to carry out this study. Additionally, we would like to express our gratitude to the Standing Committee for Coordination of Health and Medical Research in the Ministry of Health for granting ethical approval for this research. We also extend our appreciation to the MOH financial sector, Dr. Nader Alawadhi (Hospital Manager), Mrs Huda Behrami (Head of IT Department), Mrs. Shaimaa Sanaseri (Head of Medical Records Department), and the MOH Information Technology department personnel namely, Mrs. Haifaa Al-Mayyan, Mr. Khaled Al-Azmi, and Eng. Mr. Abdullah Al-Ghadyan for their invaluable contributions to this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Non-funded project.
Disclosure
The authors disclose no conflicts of interest in this work.
References
1. Cheng VCHO: Timeline: WHO’s COVID-19 Response. Geneva: World Health Organization; 2020.
2. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;2024:(20):30120.
3. Kuwait confirms 3 coronavirus patients’ coming from Iran. Available from: https://www.kuna.net.kw/ArticleDetails.aspx?id=2864385&language=en.
4. Ayed M, Abdulwahab A, Borahmah B, et al. Assessment of clinical characteristics and mortality-associated factors in COVID-19 critical cases in Kuwait. Med Princ Pract. 2021;30(2):185–192. doi:10.1159/000513047
5. Available from: https://covid19.who.int/?mapFilter=cases.
6. Available from: https://covid19.who.int/region/emro/country/kw.
7. Gupta AG, Moyer CA, Stern DT. The economic impact of quarantine: SARS in Toronto as a case study. J Infect. 2005;50(5):386–393. doi:10.1016/j.jinf.2004.08.006
8. Warren DK, Shukla SJ, Olsen MA, et al. Outcome and attributable cost of ventilator-associated pneumonia among intensive care unit patients in a suburban medical center. Crit Care Med. 2003;31(5):1312–1317. doi:10.1097/01.CCM.0000063087.93157.06
9. Cheung AM, Tansey CM, Tomlinson G, et al. Two-year outcomes, health care use, and costs of survivors of acute respiratory distress syndrome. J Respir Crit Care Med. 2006;174(5):538–544. doi:10.1164/rccm.200505-693OC
10. Bartsch SM, Ferguson MC, McKinnell JA, et al. The potential health care costs and resource use associated with COVID-19 In the United States. Health Aff. 2020;39(6):927–935. doi:10.1377/hlthaff.2020.00426
11. Rapoport J, Teres D, Zhao Y, Lemeshow S. Length of stay data as a guide to hospital economic performance for ICU patients. MedCare. 2003;41(3):386–397. doi:10.1097/01.MLR.0000053021.93198.96
12. Dasta JF, McLaughlin TP, Mody SH, Piech CT. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit. Care Med. 2005;33(6):1266–1271. doi:10.1097/01.CCM.0000164543.14619.00
13. Norris C, Jacobs P, Rapoport J, Hamilton S. ICU and non-ICU cost per day. Can J Anaesth. 2024;42(3):192–196. doi:10.1007/BF03010674
14. Worldometer, 2020. Available from: www.worldometers.info/coronavirus.
15. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan China. JAMA. 2020;323(11):1061–1069. doi:10.1001/jama.2020.1585.
16. Grasselli G, Zangrillo A, Zanella A, et al. COVID-19 Lombardy ICU network. baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to icus of the Lombardy region, Italy. JAMA. 2020;323(16):1574–1581. doi:10.1001/jama.2020.5394
17. Oostenbrink JB, Buijs-Van der Woude T, van Agthoven M, Koopmanschap MA, Rutten FF. Unit costs of inpatient hospital days. Pharmacoeconomics. 2003;21(4):263–271. doi:10.2165/00019053-200321040-00004
18. Lee J-W, McKibbin WJ. Estimating the global economic costs of SARS.
19. Rice DP, Hodgson TA, Kopstein AN. The economic costs of illness: a replication and update. Health Care Financing Rev. 1985;7(1):61.
20. Brahmbhatt M, Dutta A. On SARS type economic effects during infectious disease outbreaks: the World Bank. 2008.
21. Keogh-Brown MR, Smith RD, Edmunds JW, Beutels P. The macroeconomic impact of pandemic influenza: estimates from models of the United Kingdom, France Belgium and the Netherlands. Eur J Health Econ. 2010;11(6):543–554. doi:10.1007/s10198-009-0210-1
22. McKibbin W, Fernando R. The economic impact of COVID-19. Economic Time of COVID-19. 2020;2020:45.
23. Fernandes N. Economic effects of coronavirus outbreak (COVID-19) on the world economy. SSRN 2020 3557504.
24. Kabir M, Afzal MS, Khan A, Ahmed H. COVID-19 pandemic and economic cost; impact on forcibly displaced people. Travel Med Infect Dis. 2020;35:101661. doi:10.1016/j.tmaid.2020.101661
25. Shepard DS, Hodgkin D, Anthony YE. Analysis of Hospital Cost: A Manual for Managers. Geneva: World Health Organization; 2000.
26. Available from: https://www.exchangerates.org.uk/KWD-USD-spot-exchange-rates-history-2021.html.
27. Ministry of Health Kuwait, Financial Affairs, Budget and Control Department, Cost Accounting Section. Cost analysis and performance evaluation for government health services, 2017, p.52.
28. Available from: https://data.worldbank.org/country/KWtotalpopulacedanGDP.
29. Li XZ, Jin F, Zhang J-G, et al. Treatment of coronavirus disease 2019 in Shandong, China: a cost and affordability analysis. Infect Dis Poverty. 2020;9(1):78. doi:10.1186/s40249-020-00689-0
30. Athanasakis K, Nomikos N, Souliotis K, et al. PNS21 from disease burden to healthcare cost: highlighting the health economics aspects of the COVID-19 pandemic. Value Health. 2020;23:S647. doi:10.1016/j.jval.2020.08.1465
31. Gedik H. The cost analysis of inpatients with COVID-19. Acta Medica Med. 2020;36(1):3289–3292.
32. Khan AA, AlRuthia Y, Balkhi B, et al. Survival and estimation of direct medical costs of hospitalized COVID-19 patients in the Kingdom of Saudi Arabia. Int J Environ Res Public Health. 2020;17(20):7458. doi:10.3390/ijerph17207458
33. AlRuthia Y, Somily AM, Alkhamali AS, et al. Estimation of direct medical costs of middle east respiratory syndrome coronavirus infection: a single-center retrospective chart review study. Infect Drug Resist. 2019;12:3463–3473. doi:10.2147/IDR.S231087
34. Shrestha SS, Kompaniyets L, Grosse SD, et al. Estimation of coronavirus disease 2019 hospitalization costs from a large electronic administrative discharge database. Open Forum Infect Dis. 2020;2021:1–7.
35. Ghaffari Darab M, Keshavarz K, Sadeghi E, et al. The economic burden of coronavirus disease 2019 (COVID-19): evidence from Iran. BMC Health Serv Res. 2021;21(1):132. doi:10.1186/s12913-021-06126-8
36. Available from: https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS?locations=KW.
37. Darab MG, Keshavarz K, Sadeghi E, Shahmohamadi J, Kavosi Z. The economic burden of coronavirus disease 2019 (COVID-19): evidence from Iran. BMC Health Serv Res. 2021;21(1):132. doi:10.1186/s12913-021-06126-8
38. “Deputies approved the budget for the next three years”. [“Deputaty utverdili byudzhet na blizhajshie tri goda”. 2024Available from: http://duma.gov.ru/news/47030/.Thelinkisactiveasof05/05/2020.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
