Back to Journals » ClinicoEconomics and Outcomes Research » Volume 15
The Cost-Effectiveness of Anti-IL17 Biologic Therapies for Moderate-to-Severe Plaque Psoriasis Treatment in Italy and Germany: A Sequential Treatment Analysis
Authors Nyholm N , Danø A , Schnack H , Colombo GL
Received 20 April 2023
Accepted for publication 15 June 2023
Published 28 July 2023 Volume 2023:15 Pages 607—619
DOI https://doi.org/10.2147/CEOR.S417922
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Dean Smith
Nanna Nyholm,1 Anne Danø,2 Henrik Schnack,2 Giorgio Lorenzo Colombo3
1LEO Pharma AS, Ballerup, Denmark; 2EY, Frederiksberg, Denmark; 3CEFAT Center of Pharmaceuticals Economics and Medical Technologies Evaluation, Department of Drug Sciences, University of Pavia, Pavia, Italy
Correspondence: Nanna Nyholm, LEO pharma A/S, Industriparken 55, Ballerup, 2750, Denmark, Tel +45 6178 2096, Email [email protected]
Objective: The objective of this study was to optimise the cost-effectiveness of different anti-IL17 treatment sequences used in the treatment of moderate-to-severe plaque psoriasis in Italy and Germany over a five-year time horizon.
Methods: We adjusted a previously published treatment sequence model for biologic drugs used in psoriasis treatment to an Italian and German setting, respectively. The model included all anti-IL17 biologics currently available in the treatment of moderate-to-severe plaque psoriasis in the markets of scope (secukinumab, ixekizumab, brodalumab and bimekizumab). Real-world discontinuation rates were used to model switches between the four anti-IL17 biologics included in the study. The treatment costs were based on label dosing recommendations for each drug, including induction and maintenance therapy, and the manufacturer prices of each drug in Italy and Germany, respectively. We used long-term Psoriasis Area and Severity Index 100 (PASI100) measures to inform the model on the efficacy for each treatment. The cost-effectiveness in the analysis was evaluated based on the cost per PASI100-responder.
Results: We found that the most cost-effective treatment sequence was achieved by using brodalumab as first-line treatment, bimekizumab as second-line treatment, ixekizumab as third-line treatment and secukinumab as fourth-line treatment in both Italy and Germany, which resulted in a total cost per responder of € 128,200 and € 138,212, respectively, over a five-year period. Several scenario analyses were also conducted and ensured that the results were robust to changes in key input parameters.
Conclusion: Our study showed that using brodalumab as a first-line therapy to treat moderate-to-severe psoriasis in both Italy and Germany leads to the most cost-effective treatment sequence, when compared to all possible combinations of anti-IL17s over a five-year time horizon. In addition, we found that treatment discontinuation and switching are important factors when assessing the cost-effectiveness of biologic therapies.
Keywords: cost-per-responder, psoriasis vulgaris, treatment sequences, interleukin-17
Introduction
Plaque psoriasis is a chronic, autoimmune skin condition that affects approximately 2% of the population in Italy and Germany.1,2 It is characterised by the rapid turnover of skin cells, leading to the formation of red, scaly plaques on the skin. These plaques can be itchy, painful, and often have a negative impact on the patient’s quality of life.3 While there is currently no cure for plaque psoriasis, a variety of treatment options are available to manage the symptoms and improve quality of life for those living with the condition.3–6
The pathogenesis of plaque psoriasis is characterised by sustained inflammation that promotes uncontrolled proliferation of keratinocytes in the epidermis. This process is mediated by a dysregulated secretion of cytokines, including interleukin 17 (IL-17), interleukin 23 (IL-23), and tumour necrosis factor (TNF), which play pivotal role in the inflammatory cascade, ultimately leading to the sustained inflammation observed in plaque psoriasis.3
One class of treatments that has gained increasing attention in recent years is biologic drugs.7–9 These are genetically engineered proteins that target specific immune pathways involved in the development of psoriasis.10 Biologics have been shown to be highly effective in reducing the severity of psoriasis symptoms and are often used in the treatment of patients with moderate-to-severe psoriasis.7,11 Often, the Psoriasis Area Severity Index (PASI) is used to assess disease severity and treatment response rates (eg, PASI100 response is defined by a 100% improvement from the baseline PASI score). Especially, the biologics targeting IL-17 and IL-23 have been proven highly effective in suppressing the psoriatic symptoms and seem to be superior in achieving a PASI response compared to biologics targeting interleukin 12/23 (IL-12/23) and TNF.12–15
However, the use of biologic drugs is not without its challenges. The typical treatment pattern for patients treated with biologics involves loss of treatment response over time or potential unwanted side effects experienced by some patients.4,9,16 Thus, switching to different treatment options is usually necessary to continue managing the condition effectively. This can be particularly challenging for patients with moderate-to-severe plaque psoriasis, who may require a biologic treatment in order to achieve good disease control.4,6,17,18 Treatment with biologics is associated with a significant economic burden, especially during the first year due to the higher dosage and treatment frequency required during the induction phase compared to maintenance therapy.4,19
In recent years, a number of new biologic drugs have been introduced, including bimekizumab targeting IL-17.5,20 Patients with plaque psoriasis can switch between different drug classes, however, patients also sequence within classes (eg, within anti-IL17s). With the recent addition of bimekizumab, there is currently a lack of evidence on the optimal treatment sequence within the anti-IL17 class in the management of moderate-to-severe plaque psoriasis. Given the cost of biologic drugs, it is important to consider the cost-effectiveness of different treatment options.11,12,17 This is an important consideration, as the choice of treatment sequence can have a significant impact on the overall cost of treatment, as well as the likelihood of achieving good disease control.17
The objective of this study was to assess the cost-effectiveness of different anti-IL17 treatment sequences (secukinumab, ixekizumab, brodalumab and bimekizumab) used in the treatment of moderate-to-severe plaque psoriasis in Italy and Germany over a five-year time horizon. We aimed to provide guidance on the most cost-effective approach to managing moderate-to-severe plaque psoriasis in an Italian and German setting by focusing on the current landscape of anti-IL17s that was recently expanded by a new treatment option, bimekizumab.
Methods
Treatment Sequence Model
To evaluate the cost-effectiveness of different anti-IL17 treatment sequences of biologics used in psoriasis, we adapted a treatment sequence model which had previously been developed and published by Egeberg et al17 to an Italian and German payer perspective.
The model simulated the progression of treatment for patients with moderate-to-severe plaque psoriasis. Patients would enter the model in a state of first-line biologic treatment. After each model cycle, covering four weeks of treatment, patients could either discontinue their treatment and switch to the next treatment in the sequence or they could stay on their initial treatment. The probability of a patient transitioning to a different treatment was determined by the rate of discontinuation for each of the biologic drugs included in the analysis. In addition, patients were only allowed to make one treatment switch in each cycle. Figure 1 illustrates the patient flow in the model.
The model simulated the treatment of moderate-to-severe plaque psoriasis using up to four different biological therapies over a five-year period. As a result, patients who had reached the fourth-line treatment were assumed to remain on this treatment for the remainder of the time horizon.
While simulating the use of different biologic therapies, the model also accumulated the costs associated with each treatment. This allowed for the comparison of different treatment sequences in terms of costs. When considering the cost-effectiveness of a treatment, it is important to consider not only the cost, but also the efficacy of the drugs, as this varies between different treatment options. Thus, each biologic treatment was associated with a response rate for patients who achieve a certain level of improvement in their psoriasis symptoms after treatment. In the model, we accounted for treatment efficacy by dividing the accumulated cost for each treatment in the sequence by the corresponding treatment efficacy (defined by improvement in PASI score from baseline) for each drug. Thus, the cost-effectiveness in the analysis was evaluated based on the cost per patient achieving response in the treatment sequence. In this analysis, the following four anti-IL17 biologics were included: secukinumab, ixekizumab, brodalumab and bimekizumab. We calculated the cost-effectiveness of all possible treatment sequence combinations of anti-IL17s and ranked them according to cost-effectiveness; from most cost-effective to least cost-effective sequence.
Model Inputs
Treatment Efficacy
We used long-term efficacy measure (48–56 weeks of treatment), defined by PASI100 (complete clearance of psoriasis), to evaluate cost-effectiveness in the primary analysis. The PASI100 response rate of the included anti-IL17s was based on a network meta-analysis (NMA) published by Armstrong et al,21 which was identified through a systematic literature review (SLR) focusing on treatment efficacy of anti-IL17s and other biologic treatments.22
To assess the robustness of the analysis, we performed a scenario analysis where we changed the responder definition to PASI90 (48–56 weeks of treatment) instead of PASI100. The efficacy measures for PASI90 were also based on the NMA published by Armstrong et al21 and are presented in Table 1.
 |
Table 1 Efficacy of Biologics |
Discontinuation and Treatment Switching
Drug survival is a key indicator of therapeutic effectiveness, as it reflects both clinical outcomes and patient adherence to treatment, tolerability and the occurrence of adverse events that may lead to treatment discontinuation.16 In this treatment sequence model, it was assumed that patients would gradually discontinue their current biologic therapy and switch to the next treatment in the sequence to reflect the real-world treatment pattern of patients treated with biologics.
In the analysis, the risk of discontinuation was based on 12-month real-world discontinuation rates for secukinumab, ixekizumab and brodalumab from Torres et al.16 The primary cause of discontinuation in Torres et al was ineffectiveness of the treatment while safety issues, patients’ decision to discontinue and other non-specified causes also contributed to treatment discontinuation.16 As the discontinuation rates from Torres et al was based on real-world data, development of psoriasis arthritis or other psoriasis related secondary illnesses that may affect treatment adherence or discontinuation rates were indirectly accounted for as patients with poor treatment response would discontinue treatment.
The average discontinuation rate for these drugs (secukinumab, ixekizumab, and brodalumab) was applied to bimekizumab, as real-world evidence on drug survival for this drug is currently very limited due to its recent launch. The per-cycle discontinuation rate for each therapy is presented in Table 2.
 |
Table 2 Discontinuation Rates and Evaluation Periods |
In the base case analysis, the discontinuation rate for bimekizumab was assumed to be the same as the average discontinuation rate for secukinumab, ixekizumab, and brodalumab. To assess the significance of this assumption, we conducted two scenario analyses on the discontinuation rate of bimekizumab using ±20% of the base case value.
The effects of biological treatments may not be immediately apparent and are typically evaluated after the initial 12–16 weeks of therapy. This initial period is referred to as the induction phase. In the analysis, the length of the induction phase for each treatment was determined based on recommendations in the Summaries of Product Characteristics (SmPC) for the different therapies.23–26 It was assumed that during the induction phase, patients would remain on their treatment regardless of clinical response, as the effects of the treatment may not yet be fully achieved. The share of patients discontinuing treatment after the induction phase was estimated based on the accumulated risk of discontinuation in the period between treatment initiation and the induction treatment evaluation. This meant that discontinuation was higher in the cycle following the induction treatment evaluation than in the subsequent cycles. The time of treatment evaluation is presented in Table 2.
Treatment Dosing
The dosing for each drug included in the analysis was based on recommendations in the SmPCs.23–26 To accurately model the course of treatment, both the induction phase and the maintenance phase of the treatments were included in the model (Table 3). In the analysis, we assumed that all patients underwent a new induction treatment phase, every time they switched to a new treatment. In addition to this, we assumed that patients who switched treatment did not have a wash-out period, meaning that patient commenced the subsequent treatment immediately after discontinuation of their previous treatment.
 |
Table 3 Dosing and Drug Costs |
In clinical practice, dose adjustment is frequent and sometimes occurs due to suboptimal treatment.27,28 We performed a scenario analysis to assess the significance of including real-world evidence on dose adjustment from Egeberg et al27 and Torres et al.18 In Egeberg et al, the average weighted dosage for secukinumab was reported to be 8% above the recommended SmPC level.24,27 As Egeberg et al did not investigate dose adjustment for the remaining three anti-IL-17s, we used the finding from Torres et al18 to estimate a dose adjustment factor for these drugs. Torres et al18 found that the proportion of patients being dose adjusted was 7.4% for secukinumab, 6.4% for ixekizumab and 2.4% for brodalumab. The dose adjustment factor for secukinumab (8%) and the relative proportion of patients being dose adjusted between secukinumab and the remaining anti-IL17s was then multiplied to estimate a dose adjustment factor for each drug.
Bimekizumab was not included in either Egeberg et al27 or Torres et al,18 and thus, we used the average value from secukinumab, ixekizumab and brodalumab to estimate a dose adjustment factor. The dose adjustment factors applied in the scenario analysis were 8% for secukinumab, 6.9% for ixekizumab, 2.2% for brodalumab, and 5.7% for bimekizumab.
Treatment Pricing
The cost of each treatment was based on the pharmaceutical manufacturer prices in Italy and Germany extracted on 5 October 2022 and 15 March 2023, respectively.29,30 The drug costs were based on the pack with the lowest cost per milligram to minimise the cost of each treatment. We did not include costs related to administration, monitoring or adverse events, as these costs previously have been deemed miniscule compared to the drug costs.31
In Italy, a cashback agreement on ixekizumab and brodalumab is put in place, meaning that the Italian healthcare system receives a 5% discount on these drugs.32 In the base case analysis, we accounted for this by adjusting the price of these two drugs by −5%. To assess the significance of including a 5% discount in the price level of ixekizumab and brodalumab in Italy, we performed a scenario analysis where the costs were based solely on the pharmaceutical manufacturer prices without the mandatory cashback. As the cashback agreement only applies in Italy, this scenario analysis was not conducted for Germany.
Results
Primary Analysis
In this analysis, we calculated the cost-effectiveness of all possible treatment sequence combinations of anti-IL17s and ranked them according to cost-effectiveness; from most cost-effective to least cost-effective sequence in Italy and Germany (Table 4 and 5). Given the four treatments included in the analysis, a total of 24 (4 factorial) different treatment sequences were evaluated in each country. The most cost-effective treatment sequence for patients with moderate-to-severe plaque psoriasis among the four anti-IL17s was brodalumab, bimekizumab, ixekizumab, and secukinumab (BRO-BIM-IXE-SEC) in both Italy and Germany, resulting in a cost per responder of €128,200 and €138,212, respectively, over a five-year period.
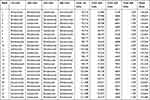 |
Table 4 Cost per Responder of All Treatment Sequence Combinations with Anti-IL17 in the Base Case Analysis (Italy) (€) |
 |
Table 5 Cost per Responder of All Treatment Sequence Combinations with Anti-IL17 in the Base Case Analysis (Germany) (€) |
The analysis showed that all six sequence combinations in Italy where brodalumab was the first-line treatment were more cost-effective compared to all remaining sequences where brodalumab was not the first-line treatment. The first sequence where brodalumab was not the first-line treatment was BIM-BRO-IXE-SEC (ranked as no. 7) and had a cost per responder of €133,681, 4% higher compared to the most cost-effective sequence.
The results for Germany also indicated that using brodalumab as the first-line treatment would result in the lowest cost per responder, as the four most cost-effective treatment sequences had brodalumab as first-line treatment. The fifth most cost-effective sequence was BIM-BRO-IXE-SEC, had a cost per responder of €148,141, 7% higher compared to the most cost-effective sequence, and was the first sequence where brodalumab was not the first-line treatment.
The analysis also suggested that drug survival plays an important role in the cost-effectiveness of each sequence. Drug survival was particularly relevant in terms of the increased costs associated with a treatment switching due to patients receiving induction therapy when starting a new treatment. This is indicated by Table 3, where the cost in the first year of treatment is compared to the subsequent years of therapy. The table shows that there are higher costs associated with first year of treatment compared to the subsequent years. As such, a high drug survival rate means that a higher percentage of patients will continue treatment with the same drug, which leads to fewer patients needing to switch to a different therapy. This reduces the cost of treatment by reducing the number of patients who need induction therapy, which is more costly compared to maintenance therapy. This was shown by the simulation of BRO-BIM-IXE-SEC (ranked as no.1 in both Italy and Germany), where the aggregated treatment distribution after five years of treatment was brodalumab 56%, bimekizumab 31%, ixekizumab 10%, and secukinumab 3% (Figure 2). In comparison, the simulation of BIM-BRO-IXE-SEC (ranked as no. 7 in Italy and 4 in Germany) showed that the aggregated treatment distribution after five years of treatment was bimekizumab 51%, brodalumab 37%, ixekizumab 10%, and secukinumab 3% (Figure 3). Fewer patients discontinuing from brodalumab compared to bimekizumab contributed to reducing the costs of BRO-BIM-IXE-SEC compared to BIM-BRO-IXE-SEC.
In Italy, we found that the first year of treatment with brodalumab was associated with an added cost of €525, corresponding to a 4% increase compared to the subsequent years (Table 3). In contrast, the added cost for the first year of treatment with bimekizumab was €6498, corresponding to a 50% increase compared to future years. Bimekizumab had a slightly higher response rate compared to brodalumab (57.3% vs 56.1%) and a 5% lower annual cost for maintenance treatment (€12,996 vs €13,650). Despite this, sequences with bimekizumab as a first-line treatment remained less cost-effective compared to sequences with brodalumab as a first-line treatment due to the induction costs of bimekizumab being 36% higher compared to brodalumab (€19,494 vs €14,175).
In Germany, the added cost of the first year of treatment with brodalumab was €557, corresponding to a 4% increase compared to the subsequent years, while the added cost for bimekizumab was €7270, corresponding to a 50% increase compared to future years. As in Italy, this contributed to sequences with bimekizumab as a first-line treatment being less cost-effective compared to sequences with brodalumab as a first-line treatment. In addition, the treatment costs of bimekizumab were 45% higher compared to brodalumab in the first year of treatment (€21,810 vs €15,039), while it was 0.4% higher in the subsequent years (€14,540 vs €14,482).
Scenario Analyses
To assess the robustness of the analysis, we performed a series of scenario analyses where alternative inputs were used for key parameters in the model. The parameters included in the scenario analyses included altering the definition of a responder, adjusting the dosage of each drug according to real-world evidence estimates, altering the discontinuation rate of bimekizumab and applying a different price level to the treatments. The scenario analyses performed in this study are presented in Table 6.
 |
Table 6 Scenario Analyses |
Changing the responder definition in the analysis to patients achieving PASI90 by weeks 48–56 instead of PASI100 implied that the cost of treatments became more significant, as a larger proportion of patients were responders. The most cost-effective treatment sequences when applying PASI90 as response definition were BRO-BIM-SEC-IXE in Italy and BRO-IXE-BIM-SEC in Germany. Thus, no changes were observed when considering the optimal first-line treatment, while minor changes were observed when considering the second-, third- and fourth-line treatments. In Italy, ixekizumab and secukinumab had switched places, while bimekizumab and ixekizumab had switched places in Germany. As indicated by row 1 in Table 6, the total cost per responder was significantly lower when using PASI90 compared to PASI100 in both Italy and Germany, as more patients were considered responders in this analysis.
In the scenario analysis where dose adjustment was included, a slight increase in the total cost per responder was observed due to increased drug usage. No changes to the optimal sequence order were observed in either Italy or Germany when compared to the base case. Thus, the inclusion of dose adjustment had a marginal effect of the results of the analysis (Table 6).
As the discontinuation rate for bimekizumab was estimated based on the average drug survival of brodalumab, ixekizumab and secukinumab, we undertook two sensitivity analyses on the discontinuation rate of bimekizumab. We changed the per-cycle discontinuation rate of bimekizumab by ±20% to 1.27% and 0.85% per cycle (base case was 1.06%). This was performed to assess whether the results were driven by the estimated drug survival rate of bimekizumab. As indicated by row 3 and 4 in Table 6, these analyses did not change the results significantly and did not change the overall conclusion.
We also performed a scenario analysis on the Italian drug price for ixekizumab and brodalumab where the 5% discount was not included. As expected, this increased the total cost per responder for all treatment sequences; however, no changes to the optimal sequence order were observed in Italy when compared to the base case (Table 6).
Discussion
This study was the first to compare the cost-effectiveness of all possible sequences of all available anti-IL17s (secukinumab, ixekizumab, brodalumab and bimekizumab) for the treatment of moderate-to-severe plaque psoriasis in Italy and Germany. We found that a treatment sequence with brodalumab as first-line treatment and bimekizumab as second-line treatment was the most cost-effective in both countries. Several scenario analyses were also conducted and ensured that the results were robust to changes in key input parameters.
Relatively few studies have assessed the cost-effectiveness of different biologic treatment sequences for patients with moderate-to-severe plaque psoriasis. Egeberg et al17 investigated the sequential cost-effectiveness of seven different biologic treatments in Spain (certolizumab, ustekinumab, brodalumab, secukinumab, ixekizumab, guselkumab, and risankizumab) and found that treatment sequences starting with brodalumab as first-line therapy were the most cost-effective. Among the anti-IL17s, Egeberg et al also found that, while sequences starting with brodalumab were most cost-effective, sequences starting with ixekizumab and secukinumab, respectively, gradually became less cost-effective.17 Thus, these findings are in line with the results of the present study. Another study by Di Matteo et al33 investigated the sequential cost-effectiveness of brodalumab, risankizumab and secukinumab as second-line therapy after treatment with adalimumab in Italy. The study found that brodalumab was a more cost-effective treatment compared to both risankizumab and secukinumab as second-line treatment, thus also suggesting that brodalumab should be used prior to secukinumab in the treatment sequence order.33
An advantage of using a treatment sequence model when evaluating cost-effectiveness is that drug survival can be incorporated in the analysis; traditional pair-wise cost-effectiveness models do not allow this. Thus, we were able to mimic the nature of psoriasis treatment progression over time and to include the added costs associated with a switch. We found that both parameters were important for the cost-effectiveness and that these should not be disregarded when evaluating cost-effectiveness of biologics used in moderate-to-severe plaque psoriasis.
A limitation of the model was that patients could not switch beyond a fourth-line treatment and thus, remained on this treatment for the remainder of the time horizon. It was observed that only few patients (2.6–3.4% depending on the sequence) would transition to the fourth-line treatment during a five-year time horizon, thus, suggesting that this assumption has a minimal impact on the results of the model when using a five-year time horizon. Egeberg et al also found that only a small number of patients reached the fourth treatment over a five-year period, suggesting that four lines of treatment were sufficient in this time frame.17 In addition, the drug survival reported by Torres et al16 also indicate that a time horizon shorter than five years would result in insufficient time to model the transition of patients from a first-line to a fourth-line treatment. Therefore, this cost-effectiveness analysis required a longer time horizon compared to traditional cost per responder analyses, which does not include treatment switching.
We used real-world evidence from Torres et al16 to estimate the drug survival of secukinumab, ixekizumab and brodalumab. In the absence of real-world drug survival of bimekizumab, due to its recent launch in Europe, we made an assumption that drug survival was an average of the drugs in the anti-IL17 class. This was an inherent limitation of the study; however, the sensitivity analyses performed on the discontinuation rate of bimekizumab showed that the base case result were robust to changes in this parameter.
Dose adjustment of biologics is relatively common and often results in patients receiving higher or more frequent treatment dosages.28 It may be an expression of suboptimal treatment and have implications for the cost of treatment. As a result, the treatment costs in the present study may have been underestimated across all four treatments. In a multi-centric, multi-country cohort study in the EU, Torres et al18 reported that dose adjustment was performed for 7.4% of patients treated with secukinumab, 6.4% of patients treated with ixekizumab, and 2.4% for brodalumab. These findings may suggest that the costs of brodalumab might, however, have been underestimated to a minor degree compared to secukinumab and ixekizumab. This could have disfavoured brodalumab in the present analysis, despite it being the optimal first-line treatment.
To investigate the impact of including dose adjustment to the analysis, we performed a scenario analysis where the SmPC treatment dosages were adjusted according to Egeberg et al27 and Torres et al.18 We found that this parameter had a minor impact on the cost-effectiveness of the included drugs. Nonetheless, it is essential to acknowledge that adjusting the dosages could potentially affect the overall expenses for payers, as the overall drug costs increase. In addition, it must be noted that this scenario analysis was affected by several limitations in data availability and that more data is warranted to confirm the effects of dose adjustment in real life. As such, this scenario analysis must be interpreted with caution with the main limitation being that the dose adjustment factor for bimekizumab was estimated based on the average value of the remaining anti-IL17s. In addition to this, there may also be safety implications, as well as potential effects on efficacy which are important aspects in relation to dose adjustment. Ideally, these factors should be considered when modelling the cost-effectiveness of biologics used in the treatment of plaque psoriasis; however, more studies are required to inform of these parameters.28
We used the 48–56-week PASI100 response rate from Armstrong et al21 to define a responder. As such, we indirectly assumed that this response rate applied throughout the five-year time horizon, regardless of the duration patients had been on a given treatment. As the response rate of biologics tend to increase during the first year of treatment, this may have overestimated the response rate for patients staying on a treatment for less than a year.21 On the contrary, patients may lose response after being on the same treatment for several years.16 This was observed by Torres et al, who found that 11% of patients on secukinumab, 6% of patients on ixekizumab and 3% of patients on brodalumab had discontinued treatment due to loss of treatment response between month 12 and month 24 of treatment.16 However, as the model took into account discontinuation, this issue mainly applied to patients discontinuing treatment before completing one year of therapy.
Another potential limitation of modelling long-term cost-effectiveness was that treatment costs were kept constant throughout time horizon. In reality, changes in drug prices are likely to occur over a five-year period due to new entries in the market and biosimilar competition. Thus, the results of our study may change if the competitive landscape of biologics are altered.
Conclusion
To optimise cost-effectiveness of anti-IL17s used in the treatment of moderate-to-severe plaque psoriasis in Italy and Germany, our results show that of all possible treatment sequences combinations with all anti-IL17s, brodalumab should be used as first-line treatment and bimekizumab should be used as second-line treatment. Over a five-year period, the most cost-effective treatment sequence was (1) brodalumab, (2) bimekizumab, (3) ixekizumab and (4) secukinumab in both Italy and Germany, resulting in the lowest cost per responder out of 24 possible sequence combinations.
Using a sequential treatment model, we optimised the cost-effectiveness of anti-IL17 biologic treatments used in moderate-to-severe plaque psoriasis. Besides efficacy and treatment costs, we found that accounting for drug survival and the added costs associated with treatment switching is important when evaluating cost-effectiveness. This research will be of particular relevance to patients, healthcare providers, and payers, as it will provide valuable insights to guide the selection of treatment options for managing moderate-to-severe plaque psoriasis in an Italian and German setting.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by LEO Pharma.
Disclosure
Giorgio Lorenzo Colombo has received speaker fees, research and educational grants from Abbott, Boehringer Ingelheim, LEO Pharma, Eli Lilly, Novo Nordisk, Dompè, Sanofi, and Pfizer. Nanna Nyholm is an employee at LEO Pharma. Henrik Schnack is an employee at EY, a vendor of LEO Pharma. Anne Danø was also an employee at EY during the study's development and submission but had left EY at the time of publication.
References
1. Papp KA, Gniadecki R, Beecker J, et al. Psoriasis prevalence and severity by expert elicitation. Dermatol Ther. 2021;11(3):1053–1064. doi:10.1007/s13555-021-00518-8
2. Parisi R, Iskandar IYK, Kontopantelis E, Augustin M, Griffiths CEM, Ashcroft DM. National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ. 2020;m1590. doi:10.1136/bmj.m1590
3. Rendon A, Schäkel K. Psoriasis pathogenesis and treatment. IJMS. 2019;20(6):1475. doi:10.3390/ijms20061475
4. Gisondi P, Altomare G, Ayala F, et al. Italian guidelines on the systemic treatments of moderate-to-severe plaque psoriasis. J Eur Acad Dermatol Venereol. 2017;31(5):774–790. doi:10.1111/jdv.14114
5. Rønholt K, Iversen L. Old and new biological therapies for psoriasis. IJMS. 2017;18(11):2297. doi:10.3390/ijms18112297
6. Nast A, Altenburg A, Augustin M, et al. German S3‐guideline on the treatment of psoriasis vulgaris, adapted from EuroGuiDerm – part 1: treatment goals and treatment recommendations. JDDG. 2021;19(6):934.
7. Thatiparthi A, Martin A, Liu J, Egeberg A, Wu JJ. Biologic treatment algorithms for moderate-to-severe psoriasis with comorbid conditions and special populations: a review. Am J Clin Dermatol. 2021;22(4):425–442. doi:10.1007/s40257-021-00603-w
8. de Ruiter CC, Rustemeyer T. Biologics can significantly improve Dermatology Life Quality Index (DLQI) in psoriatic patients: a systematic review. PTT. 2022;12:99–112. doi:10.2147/PTT.S356568
9. Egeberg A, Ottosen MB, Gniadecki R, et al. Safety, efficacy and drug survival of biologics and biosimilars for moderate-to-severe plaque psoriasis. Br J Dermatol. 2018;178(2):509–519. doi:10.1111/bjd.16102
10. Tobin P, Richards D, Callender R, Wilson C. Protein engineering: a new frontier for biological therapeutics. CDM. 2015;15(7):743–756. doi:10.2174/1389200216666141208151524
11. Yasmeen N, Sawyer LM, Malottki K, Levin LÅ, Didriksen Apol E, Jemec GB. Targeted therapies for patients with moderate-to-severe psoriasis: a systematic review and network meta-analysis of PASI response at 1 year. J Dermatolog Treat. 2020;33(1):204–218. doi:10.1080/09546634.2020.1743811
12. ten Bergen LL, Petrovic A, Krogh Aarebrot A, Appel S. The TNF/IL‐23/IL‐17 axis—head‐to‐head trials comparing different biologics in psoriasis treatment. Scand J Immunol. 2020;92. doi:10.1111/sji.12946
13. Furue K, Ito T, Furue M. Differential efficacy of biologic treatments targeting the TNF-α/IL-23/IL-17 axis in psoriasis and psoriatic arthritis. Cytokine. 2018;111:182–188. doi:10.1016/j.cyto.2018.08.025
14. Pina Vegas L, Penso L, Claudepierre P, Sbidian E. Long-term persistence of first-line biologics for patients with psoriasis and psoriatic arthritis in the French health insurance database. JAMA Dermatol. 2022;158(5):513. doi:10.1001/jamadermatol.2022.0364
15. Ratner M. IL-17–targeting biologics AIM to become standard of care in psoriasis. Nat Biotechnol. 2015;33(1):3–4. doi:10.1038/nbt0115-3
16. Torres T, Puig L, Vender R, et al. Drug survival of IL-12/23, IL-17 and IL-23 inhibitors for psoriasis treatment: a retrospective multi-country, multicentric cohort study. Am J Clin Dermatol. 2021;22(4):567–579. doi:10.1007/s40257-021-00598-4
17. Egeberg A, Danø A, Pedersen MH, Sohrt A, Borg E, Notario J. Modeling the optimal sequence of biologic therapies in plaque psoriasis in Spain. J Med Econ. 2021;24(1):1134–1142. doi:10.1080/13696998.2021.1970953
18. Torres T, Puig L, Vender R, et al. Drug survival of interleukin (IL)‑17 and IL‑23 inhibitors for the treatment of psoriasis: a retrospective multi‑country, multicentric cohort study. Am J Clin Dermatol. 2022;23(6):891–904. doi:10.1007/s40257-022-00722-y
19. Burgos-Pol R, Martínez-Sesmero JM, Ventura-Cerdá JM, Elías I, Caloto MT, Casado MÁ. The cost of psoriasis and psoriatic arthritis in 5 European countries: a systematic review. Actas Dermo Sifiliogr. 2016;107(7):577–590. doi:10.1016/j.ad.2016.04.018
20. Ruggiero A, Potestio L, Camela Snr E, Fabbrocini G, Megna M. Bimekizumab for the treatment of psoriasis: a review of the current knowledge. PTT. 2022;12:127–137. doi:10.2147/PTT.S367744
21. Armstrong AW, Soliman AM, Betts KA, et al. Long-term benefit–risk profiles of treatments for moderate-to-severe plaque psoriasis: a network meta-analysis. Dermatol Ther. 2022;12(1):167–184. doi:10.1007/s13555-021-00647-0
22. Nyholm N, Schnack H, Danø A, Skowron F. Cost per responder of biologic drugs used in the treatment of moderate-to-severe plaque psoriasis in France and Germany. Curr Med Res Opin. 2023;39(6):833–842. doi: 10.1080/03007995.2023.2214046
23. European Medicines Agency. Bimzelx®: summary of product characteristics; 2022. Available from: https://www.ema.europa.eu/en/documents/product-information/bimzelx-epar-product-information_en.pdf.
24. European Medicines Agency. Cosentyx®: summary of product characteristics; 2022. Available from: https://www.ema.europa.eu/en/documents/product-information/cosentyx-epar-product-information_en.pdf.
25. European Medicines Agency. Kyntheum®: summary of product characteristics; 2022. Available from: https://www.ema.europa.eu/en/documents/product-information/kyntheum-epar-product-information_en.pdf.
26. European Medicines Agency. Taltz: summary of product characteristics; 2020. Available from: https://www.ema.europa.eu/en/documents/product-information/taltz-epar-product-information_en.pdf.
27. Egeberg A, Freilich J, Stelmaszuk MN, et al. Real-world dose adjustments of biologic treatments in psoriasis and their economic impact - a Swedish national population study. Clin Exp Dermatol. 2022;47:1968–1975. doi:10.1111/ced.15288
28. Gambardella A, Licata G, Sohrt A. Dose adjustment of biologic treatments for moderate-to-severe plaque psoriasis in the real world: a systematic review. Dermatol Ther. 2021;11(4):1141–1156. doi:10.1007/s13555-021-00559-z
29. Codifa. Codifa - L’Informatore Farmaceutico [Codifa - Pharmaceutical Informer]; 2022. Available from: https://www.codifa.it/.
30. ABDATA Pharma-Daten-Service. Pharmaceutical manufacturer prices in Germany; 2023.
31. Augustin M, Wirth D, Mahlich J, Pepper AN, Druchok C. Cost per responder analysis of guselkumab versus targeted therapies in the treatment of moderate to severe plaque psoriasis in Germany. J Dermatolog Treat. 2020;33(2):976–982. doi:10.1080/09546634.2020.1793891
32. Agenzia Italiana del Farmaco. Modifica dell’allegato n. 2 della determina n. 285/2022 del 27 giugno 2022, concernente procedura pay-back 5% [Amendment of attachment no. 2 of decision n. 285/2022 of 27 June 2022, concerning the 5% pay-back procedure]; 2022. Available from: https://www.aifa.gov.it/.
33. Di Matteo S, Cavaliere A, Danesi R. Terapie biologiche e sequenze di trattamento per i pazienti con psoriasi a placche moderata-grave: un’analisi farmacoeconomica per il Sistema Sanitario Nazionale italiano. Clinico Economics; 2022. Available from: http://www.clinicoeconomics.eu/articles/flipbook/17_2022_137-154/.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



