Back to Journals » Infection and Drug Resistance » Volume 17
Risk Factors for Occupational Blood Exposure, Compliance with Policies of Infection Prevention and Control, and Costs Associated with Post Exposure Management Among Nursing Staff
Authors Liu Y, Li Y, Yuan S, Ma W, Chen S, Wang LY
Received 24 November 2023
Accepted for publication 8 March 2024
Published 26 March 2024 Volume 2024:17 Pages 1215—1228
DOI https://doi.org/10.2147/IDR.S451615
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Yan Liu, Yang Li, Song Yuan, Wei Ma, Si Chen, Li-Yi Wang
Department of Infection Control, the Second Hospital of Hebei Medical University, Shijiazhuang, People’s Republic of China
Correspondence: Li-Yi Wang, Department of Infection Control, the Second Hospital of Hebei Medical University, No. 215 of Heping West Road; Xinhua District, Shijiazhuang, Hebei, 050000, People’s Republic of China, Tel +86 13673160996, Fax +86 0311 83179721, Email [email protected]
Objective: To examine the risk factors linked with occupational blood exposure (OBE) among nursing staff (NS), we pinpoint deficiencies in the compliance with policies of infection prevention and control, and assess the expenditures associated with infection prevention and control.
Methods: Healthcare workers that completed an “Occupational Blood Exposure Report Form” were divided into NS (observation) group and non-NS (control) group. Univariate and multivariable analyses were conducted to compare both groups in various aspects. We also explored design patents intended to minimize occupational exposure.
Results: The highest incidence of OBE was observed in the department of neurosurgery. Among NS, OBE incidence was found to be influenced by independent risk factors, such as gender, age, occupational title, work location, and incidence of sharps injuries. Protective factors against OBEs included the use of arterial blood gas needles and suture needles. Personal protective equipment (PPE) usage rates were low in both groups prior to OBEs (0.74% vs 0.00%, P > 0.05). Correct emergency management could be improved promptly by both groups following an OBE (P > 0.05). However, the observation group exhibited a higher proportion of blood expression after a sharps injury and a higher re-evaluation rate at 6 months post-exposure compared to the control group (P < 0.05). In 2018, the per capita costs of infection prevention and control for NS were the Chinese Yuan (RMB) 339.43 per individual. In response to these findings, two utility model patents have been authorized.
Conclusion: The risk and protective factors related to the occurrence of OBEs were investigated in this study, suggesting that there is a need for improvement in the rate of PPE usage and the re-evaluation rate of OBEs among NS. Additionally, focused training on emergency blood expression and compliance with policies among non-NS personnel is deemed necessary.
Keywords: compliance, infection prevention and control, nursing staff
Background
Health care workers (HCWs), especially nursing staff (NS), face a significant risk of occupational blood exposure (OBE).1–6 The World Health Organization estimated that each year, of the 35 million HCWs worldwide, 2 million to hepatitis B virus (HBV), 0.9 million to hepatitis C virus (HCV), and 170,000 to human immunodeficiency virus (HIV).1 The career time prevalence of OBE among HCWs was found to be 56.6%.6 A 2016 survey in the United States disclosed that the average economic loss per OBE was US$747, with a direct economic loss of US$425 per case and an indirect economic loss of US$322.7,8 OBEs not only increase administrative costs of hospitals but also elevate the risk of bloodborne infections among HCWs.9 Following exposure, HCWs are susceptible to psychological issues like anxiety, depression, and post-traumatic stress disorder (PTSD). They may also face discrimination and, in extreme cases, lose their employment.10
Despite the World Health Organization’s (WHO) efforts to promote safety devices,11 around 77.22% of Chinese hospitals have issues with underreporting OBEs,12 and only 33.9% of HCWs report OBE incidents.13 This persistent underreporting significantly undermines the effectiveness of post-exposure management measures, underscoring the importance of early preventive measures targeting risk factors. Identifying these risk factors is crucial. Nursing staff are often frontline workers in clinical settings, providing effective nursing services to a large number of patients in such environments. They are also involved in various nursing procedures, such as blood collection and intravenous therapy. These tasks require close contact with patients, exposing nursing staff to numerous occupational hazards, which can impact their physical and mental well-being. Therefore, it is necessary to carefully analyze the occupational exposure risks faced by nursing staff and implement effective measures to strengthen their occupational protection, improve their working environment, and ensure their overall well-being. While cross-sectional studies on NS OBE incidence in China are common, those comparing groups are rare, and research on infection prevention and control compliance’ with policy and costs is even scarcer.
In this study, we categorized NS with OBE incidence as the observation group and non-NS HCWs as the control group. Multivariable logistic regression analysis was employed to identify OBE risk factors among NS compared to non-NS. For the first time, we assigned scores to local emergency management steps, calculated the correctness rate of post-OBE local emergency management, and investigated re-evaluation, diagnostic procedure costs, and prophylactic medication post exposure costs. The aim is to pinpoint weaknesses in current occupational exposure prevention and control measures, offer data support for targeted intervention measures, and effectively mitigate the risk of occupational exposure.
Study Participants and Methods
Study Participants Inclusion Criteria
In this a comparative study between nurse and non-NS HCWs, the following study participants were consecutively included: 1) Those who experienced OBEs between January 1 and December 31, 2018; 2) HCWs who faced these exposures both at our main hospital and north campus; 3) Those who reported the incident to the infection control department; 4) Those who completed the occupational blood exposures report form.
Exclusion Criteria: 1) Those who did not report the incident via phone to the infection control department; 2) Those who did not complete the “Occupational Blood Exposures Report Form”; 3) Those who had missing data.
Research Method
Terminology and Definitions
OBEs:14 A situation in which workers, while carrying out their job duties, encounter blood or other substances that may carry bloodborne pathogens (microorganisms in blood and specific body fluids capable of causing human diseases) via the eyes, mouth, nose, other mucous membranes, damaged skin, or routes other than the gastrointestinal tract.
Patient ward:15 Describes a space dedicated to monitoring, diagnosing, treating, providing rest, sleep, and meals for hospitalized patients. Typically furnished with beds, isolation curtains, chairs, a nurse call system, oxygen supply, negative pressure suction system, hand hygiene stations, restroom, and a container for non-medical waste, among other amenities.
Scoring for Immediate Response Procedures for OBEs is as Follows
To address a sharps injury, it is essential to follow a three-step treatment protocol sequentially, assigning scores to each step.
1 point: Following a sharps injury, the HCW should softly exert pressure from the closer end to the farther end of the wound to release as much blood as they can.
1 point: Following a sharps injury, the HCW should cleanse the injury using a soap solution or running water.
1 point: After cleansing, the wound should be disinfected with 75% ethyl alcohol or 0.5% povidone-iodine.
Scoring for Post-Exposure Emergency Management of Skin and Mucous Membrane Exposures
3 points: Contaminated skin should be washed with soap solution and running water; contaminated mucous membranes should be repeatedly cleansed with normal saline solution.
The preoperative basic blood panel: The preoperative basic panel, quantitative hepatitis B panel, Alanine aminotransferase (ALT), HCV antibody test, Hepatic function panel, Treponema pallidum specific antibody (TP-PA), HIV antibody, complete blood count (CBC) with differential, urinalysis, and renal function panel are to be conducted.
The Prophylactic Medication Post Exposure Regimen Involved in This Study Includes
Hepatitis b immunoglobulin, Tetanus antitoxin, and Benzathine penicillin.
Direct Costs of Prevention and Control
In this study, direct costs, encompassing diagnostic testing, pharmacotherapy, and post-exposure follow-up and review, were considered. The costs of prophylactic medication for exposures involving HIV as the source were assessed by local centers for disease control and prevention (CDC) and, therefore, were not incorporated into the costs of this study.
Survey Methodology
The “Occupational Blood Exposures Report Form” was filled out by healthcare workers who underwent an occupational exposure. The infection control department is where the report was submitted, and it encompassed details such as basic information of the exposed individual, the location of the occupational exposure, the source of exposure, specific operations conducted at the time of exposure, contaminated items, specific post-exposure handling procedures, evaluation of pharmacotherapy, and reimbursement status.
Grouping: HCWs with Incidents of OBEs are Divided into Two Groups
NS as the observation group and non-NS as the control group. The “control” group consists of non-NS individuals, including working doctors, students, residents, visiting doctors, and third-party personnel under contract with the hospital.
Statistical Methods
The occupational exposure survey involved entering data into Excel through a double data entry process, which was then cross-verified by a third party to ensure accuracy. The validated data from Excel was imported into SPSS version 22.0 for analysis. Percentages represented count data, and group comparisons were conducted using the chi-squared test. Statistical significance was determined by a P-value less than 0.05. Variables with significance (P < 0.05) in the univariate analysis were included as independent variables in the multivariable logistic regression analysis. The objective was to identify statistically significant risk factors for NS compared to non-NS in the incidence of OBEs, also requiring a significance level of P < 0.05.
Results
Baseline Comparison
Using 25 years as the dividing line, the proportions of people aged below 25 in the two groups were 37.78% and 22.33%, respectively, with χ2=6.507 and P=0.011, indicating comparability. The composition ratio of individuals under 25 years old in the two groups showed no significant difference, demonstrating comparability. This information has been incorporated into Baseline Comparison.
Departmental Distribution
The prevalence of OBEs is 56.72% (135/238). Among 238 HCWs who faced occupational exposure, 25 (10.50%) belonged to the field of neurosurgery, 23 (9.66%) worked in the emergency department, 17 (7.14%) were associated with cardiology, 14 (5.88%) were from neurology, and 12 (5.04%) represented gastroenterology. Notably, neurosurgery recorded the highest incidence of exposures (Table 1).
 |
Table 1 Departmental Distribution of Occupational Exposure Personnel |
Risk Factor Analysis
Univariate Analysis
Potential Personal Risk Factors
In the observation group, a higher incidence of OBEs was noted in terms of the proportion of females (93.33%), those aged ≤ 25 (37.78%), with a work duration of ≤ 5 years (71.78%), employed workers (88.15%), and junior professional ranks (65.19%) when compared to the control group, where these proportions were at 50.49%, 22.33%, 16.50%, 31.07%, and 6.80%, respectively. The differences were found to be statistically significant (P < 0.05). Furthermore, the proportion of students in the control group (61.17%) was significantly higher than that in the observation group (11.85%) (P < 0.05), as indicated in Table 2.
 |
Table 2 Univariate Analysis of Risk Factors Unique to OBEs Among Nursing Staff |
Exposure Source Classification
A higher risk of experiencing sharps injury was observed in the observation group (96.30%) compared to the control group (77.67%) (P < 0.05). Conversely, a higher incidence of HBV exposure was noted in the control group (38.83%) compared to the observation group (25.19%) (P < 0.05), as indicated in Table 2.
Potential High-Risk Exposure Locations
A higher risk of OBEs was encountered in patient wards (48.89%) and treatment rooms (14.07%) by the observation group compared to the control group (27.18% and 2.91%, respectively, P < 0.05). A higher incidence of OBEs in the operating theater (41.75%) and emergency department (67.96%) was experienced by the control group compared to the observation group (8.15%, P < 0.05), as indicated in Table 2.
Potential Risk Exposure Sites
In the observation group, higher risks of OBEs were noted for the right hand (37.04%), thumb (28.89%), and right thumb (11.11%) in comparison to the control group (20.39%, 16.50%, and 3.88%, respectively, P < 0.05), as depicted in Table 2.
Potential High-Risk Exposure Activities
A higher risk was experienced by the observation group during needle withdrawal (14.07% vs 1.94%) and sharps disposal (17.04% vs 4.85%) in comparison to the control group (P < 0.05), as depicted in Table 2.
Potentially Hazardous Exposure Materials
There was a higher likelihood of needles exposure (85.19% for needles in general, 30.31% for standard injection needles, 11.11% for insulin needles, and 5.93% for scalp acupuncture needles) during an OBE in the observation group compared to the control group (with respective exposure rates of 65.05%, 16.50%, 0.97%, and 0.00%, P<0.05). Additionally, a higher probability of exposure to arterial blood gas (ABG) needles (20.39%) and suture needles (20.39%) was observed in the control group compared to the observation group (with respective exposure rates of 0.74% and 11.11%, P < 0.05), as indicated in Table 2.
Analyzing multiple variables in logistic regression, with the observation group as the independent variable and incorporating significant univariate analysis variables, the findings (refer to Table 3) reveal that the risk factors for OBEs in neurosurgery include being female, age ≤ 25, holding a junior professional position, working in a treatment room, and encountering a sharps injury. Conversely, exposure to ABG needles and suture needles emerged as protective factors against OBE incidence in neurosurgery (P < 0.05).
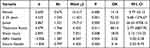 |
Table 3 Logistic Regression Analysis of the Incidence of OBEs Among Nursing Staff |
Compliance with Policies of Protection
Pre-Exposure Protective Equipment Utilization
Prior to exposure, very low rates of glove wearing (0.74% vs 0.00%) and protective gear usage (0.74% vs 0.00%) were observed in both the observation group and the control group, with no significant difference between the groups (P > 0.05), as indicated in Table 2.
Post-Exposure Emergency Local Management
Correct and timely emergency local management after the occurrence of OBEs was successfully executed by 94.81% of the observation group and 90.29% of the control group, with no significant difference between the groups (P > 0.05), as indicated in Table 4.
 |
Table 4 Percentage of HCWs Performing Local Emergency Management Post-Occupational Exposure |
Sharps Exposure
After exposure, blood expression, irrigation, and disinfection were performed by 98.46%, 97.69%, and 94.62% of the observation group, respectively, while the aforementioned emergency management was carried out by 88.75%, 93.75%, and 92.50% of the control group. A higher proportion of emergency blood expression was observed in the observation group compared to the control group (P < 0.05), with correct emergency management rates of 94.62% and 87.50%, respectively, showing no significant difference between the groups (P > 0.05).
Skin and Mucous Membrane Exposure
Both groups were able to carry out cleansing 100% of the time after exposure.
Actual Review Situations
The highest actual follow-up rate for the observation group after OBEs was observed at the third month (59.18%), with a higher rate at the sixth month compared to the control group (44.90% vs 14.81%) (P < 0.05). The highest actual follow-up rate for the control group after OBEs was observed at the second month, at 50.00%, as indicated in Table 5.
 |
Table 5 Actual Review Rates for the Two Groups |
Actual Review Situation for the Main Sources of Exposure
Following exposure to HBV, the re-evaluation rate peaked for both groups in the third month. Similarly, after exposure to HCV, the highest re-evaluation rate for both groups occurred in the third month. In the case of HIV exposure, the observation group exhibited the highest re-evaluation rate in the initial month, as detailed in Table 6.
 |
Table 6 Actual Review Status Following Exposure to HBV, Hepatitis C Virus, Syphilis, and AIDS Viruses |
Costs of Infection
In 2018, the overall expenses for preventing and controlling OBEs amounted to the Chinese Yuan (RMB) 80,783.94, averaging RMB 339.43 per individual. A significant portion (95.55%) of the costs related to infection prevention and control was allocated to post-exposure screening. The primary expenditure focus for testing objectives in both groups was the preoperative basic panel, while hepatitis B immunoglobulin emerged as the main cost for prophylactic medication post exposure. A comparison between the observation and control groups revealed that the observation group incurred higher total testing costs (RMB 47,343), average testing costs per person (RMB 350.69), total prevention and control costs (RMB 48,953.34), and average prevention and control costs per person (RMB 362.62) than the control group (RMB 29,584, RMB 287.22, RMB 31,839.6, and RMB 309.12, respectively), as indicated in Table 7.
 |
Table 7 Overview of Costs of Infection Prevention and Control for Nursing Staff and Non-Nursing Staff |
Two Patented Utility Models for the Reduction of Occupational Exposures
An Adjustable Medical Surgical Support (Publication Number: CN 208710102 U; Patent Number: ZL 2018 2 0289444.5)
The installation of a tray main body in this adjustable medical surgical support facilitates the successful placement or retrieval of medications and tools, streamlining user workflow and expediting the instrument transfer process during surgery. This, in turn, contributes to the effective reduction of HCW occupational exposure incidents during instrument transfer. See Figure 1a–d.
 |
Figure 1 Schematic Diagrams of an Adjustable Medical Surgical Support (a–d) and a High-Fit Facial Protective Mask (e–i). (a) Schematic illustration of the main structure of the novel utility model; (b) Schematic illustration of the hanging buckle main body structure of the utility model; (c) Schematic illustration of the tray main body structure of the utility model; (d) Schematic illustration of the support frame main body structure. The labels for a-d include: 1-telescopic column; 2-hanging buckle main body; 3-tray main body; 4-base stand; 5-caster wheel; 6-waste bin; 7-support frame main body; 8-hook plate; 9-hook column; 10-suspension buckle; 11-tray casing; 12-divider; 13-fixed sleeve column; 14-fixed groove; 15-upper sleeve column; 16-support frame housing; 17-clasp; 18-lower baffle; 19-fixed clamp sleeve. (e) Structural schematic of the high-fit facial protective mask of this utility model. (f) Cross-sectional view along the A-A line in Figure 1. (g) Cross-sectional view along the B-B line in Figure 1. (h) Schematic of the end of the detachable sealing strip. (i) Cross-sectional view of the high-fit facial protective mask in another technical scheme of the utility model. The labels for e-i include: 10-mask shell; 11-metal fixation bar; 12-mask band; 20-detachable sealing strip; 21-side strip; 211-inner side strip; 2111-housing cavity; 2112-skin-contact contour; 212-outer side strip; 2121-raised section; 22-lower strip; 23-cleft; p-zygomatic bone. |
A High-Fit Facial Protective Mask (Publication Number: CN 219613137 U; Patent Number: ZL 2023 2 0571962.7)
The mask shell incorporates a protective mask attached through a detachable sealing strip, establishing a seal at the lower and lateral aspects. Crafted from rubber material, the detachable sealing strip is pliable, adept at conforming to facial contours during movements, thereby demonstrating excellent flexibility. Significantly, the detachable sealing strip is designed for easy removal, facilitating cleaning and disinfection. This configuration effectively shields HCWs from skin and mucosal exposure, consequently reducing the incidence of OBEs affecting HCW facial skin and mucosa. See Figure 1e–i.
Discussion
On an annual basis, OBEs are experienced by approximately 36.4% of HCWs (95% CI: 32.9–40.0).16 OBEs are caused by over 60 known sources, with the three principal pathogens involved being HBV, HCV, and the HIV—the causative agent of AIDS,17 with HBV exposures being the most prevalent.18 The highest incidence of occupational exposures was identified in neurosurgery departments, with a rate of 10.50%. As a result, a risk factor analysis for occupational exposures was conducted in this study in close collaboration with neurosurgeons, with a focus on high-risk groups and critical stages.
A significant share of treatment and operative tasks, often involving direct patient contact, is carried out by the NS, who constitute the largest cohort within HCWs. NS are more likely to incur injuries during their duties compared to their non-nursing HCW counterparts,19 thereby designating them as a primary group for occupational exposures.20 In a study by Gaurus-Pakowska et al, it was found that incidents of OBE were 3.495 times more likely to be underreported by males compared to females.17 This aligns with the findings of Alemayehu et al21 and Gabr HM et al22 who observed higher incidence rates of OBEs among female HCWs than their male counterparts. Junior nurses, typically younger and predominantly engaged in tasks such as needle withdrawal and venipuncture, display less proficiency and psychological resilience, along with a lower compliance with policies of protective measures. This is particularly evident in emergency situations or when dealing with restless and less cooperative patients.23 Therefore, individuals aged ≤ 25 or at a junior professional rank among nursing staff are identified as having a slower response to emergent events, making them risk factors for the incidence of OBEs.
It has been indicated by numerous studies that the incidence of OBEs among HCWs may be influenced by various factors such as having less than five years of work experience,13 working in an operating theater,20 needle withdrawal, the centralized disposal of used sharps,24 needle use,19 or the month of admission for non-employed workers, referring to students, residents in training programs, interns, and visiting scholars.25 Following the control of confounders through logistic regression analysis, it was revealed that a higher risk of OBEs in the treatment room and a higher incidence of sharps injuries were observed in the observation group compared to the control group. Conversely, a lower risk of OBEs than the control group was demonstrated in the observation group when using ABG needles and suture needles. The differing conclusions may be attributed to the selection of study populations. While all previous studies13,19,20,24,25 were cross-sectional and focused on HCWs post-exposure without grouping, only describing the proportional distribution of various factors among HCWs, in our study, we classified HCWs post-exposure into two groups. By comparing the distribution differences of various factors between these groups, we hypothesized risk factors for OBEs among nursing staff compared to non-nursing staff. Future case-control studies are deemed necessary to validate the independent risk factors for OBEs in nursing staff.
Table 2 shows that the proportion of students in the control group (61.17%) is significantly higher than that in the observation group (11.85%) (P < 0.05), indicating that training and exams for graduate students, residents, and visiting doctors should emphasize the inclusion of occupational exposure handling procedures and proper use of personal protective equipment. During departmental early education sessions, the importance of personal protection when students are operating should be emphasized to enhance their awareness and reduce the occurrence of occupational exposure. It can also be observed that the control group has a higher risk of experiencing OBEs in the operating room (41.75%) and the emergency department (67.96%) compared to the observation group (8.15%, P < 0.05). This suggests that the operating room and emergency department are high-risk areas for non-nursing personnel to experience occupational exposure. On the existing basis, occupational exposure handling process diagrams and illustrations of proper personal protective equipment use should be posted on the walls of each room, operating room, corridor, and dressing room in the operating room and emergency department. Regular training and assessment on the use of personal protective equipment should be conducted for surgeons operating in the operating room, increasing the frequency of inspections for the operating room and emergency department to reduce the risk of occupational exposure. Thirdly, the control group has a higher probability of exposure to blood gas needles (20.39%) and suture needles (20.39%) compared to the observation group (0.74% and 11.11%, respectively, P < 0.05). Blood gas needles are commonly used in respiratory departments, while suture needles are common in operating rooms or dressing rooms for wound closure. Therefore, based on these results, specialized personal protective equipment training for doctors in respiratory and surgical departments should be conducted. The frequency and intensity of infection control inspections in the blood gas room, operating room, and dressing room should be increased to standardize the procedures for blood gas needle and wound closure operations, ensuring the correct use of personal protective equipment and reducing the risk of occupational exposure to safeguard the safety and health of healthcare workers.
Following an OBE, local emergency management should be immediately undertaken by the HCW, and subsequent reporting to the infection control department is required. The “Occupational Blood Exposures Report Form” must be completed by the HCW at the infection control department, where the exposure incident shall be evaluated, and an examination conducted by personnel. Based on the results, prophylactic medication post exposure shall be provided to the HCW, and information regarding review times and frequency communicated. A longitudinal study conducted by Sun et al26 on the psychological stress reactions in HCWs following OBEs revealed that peak levels of anxiety, depression, and PTSD were reached one month after exposure. The study by Wang et al27 indicated that psychological stress reactions among HCWs continued to rise within six months after exposure. Due to HBV and HCV being recognized as the primary sources of OBEs,17 it is mandated that HCWs exposed to these viruses undergo their first review in the third month following exposure14–a substantial period after the initial event that may be easily overlooked. This could potentially account for the highest proportions of reviews observed in the second- and third-months post-OBE in our study (P < 0.05).
The capacity of HCWs to respond to emergency management may be affected by the fear and tension experienced at the time of exposure, potentially leading to omissions in the management steps. Correct emergency local treatments were performed by 94.81% in the observation group and 90.29% in the control group post-exposure, but only one instance of pre-exposure glove use was recorded in both groups combined, with monthly re-evaluation rates ranging from 0.00% to 59.18%. The reporting rate for OBEs was noted to be only 22.78% by Sun et al,12 and Hebo et al28 reported a mere 42.6% execution rate for standard precautions among HCWs. These figures point to a common reality: poor compliance with OBE prevention and control among HCWs. Therefore, future priorities in the prevention and control of occupational exposures should involve a shift towards improving compliance of HCWs with OBE prevention and control measures.
Not only is considerable psychological strain and pain brought about by OBEs to HCWs, but also significant economic costs are incurred, which can be classified into direct and indirect economic losses. Direct economic losses encompass diagnostic fees, prophylactic medication, post exposure, and follow-up fees incurred after an HCW experiences OBEs. Indirect economic losses include lost wages, productivity loss, and financial compensation resulting from OBEs. Due to variations in safety legislation and policy implementation related to OBEs across countries,29 the usage of safety devices varies by region, and there is also variation in hospital HCW compliance with policies of protection against OBEs,30 leading to differences in the per capita direct costs of prevention and control between regions. The costs of HIV post-exposure prophylaxis (PEP) as provided by the CDC were not included in this single-center study, thus the per capita OBE costs of infection prevention and control for nursing staff were RMB 362.62, exceeding that for non-nursing staff at RMB 309.12. The per capita direct costs of prevention and control for HCWs were RMB 339.43, lower than the RMB 349.84 reported by Wang et al8 and the US$747 reported by Cook et al10 Effective prevention and control measures suitable for this institution were formulated through the identification of risk factors, high-risk groups, and critical operation phases of occupational exposures, in this study. The objective was to diminish the frequency of occupational exposures and decrease hospital expenditures, encompassing diagnostic fees and lost wages associated with OBEs. This initiative aimed to advance the favorable and sustainable development of the hospital. The visualization, materialization, and embodiment of actual data were supported by the authorization of two practical patents resulting from this study. The transfer of patent rights for the utility model patent, titled “An Adjustable Medical Surgical Support”, has been realized, achieving research-to-practice translation. The application of the two patents in the actual work of this institution and clinical feedback, derived from practical work, can effectively benefit clinical practice, significantly reducing the occurrence of occupational exposures and promoting the clinical application of the patents. This aspect also delineates a prospective avenue for future research. It is imperative to acknowledge the limitation of this study, which lies in its single-center design. Subsequently, it is anticipated that multicenter studies will be conducted in the future to enhance the generalizability of findings.
Conclusion
The risk factors and protective factors linked to the incidence of OBEs, along with the compliance with policies and costs of infection prevention and control among HCWs were explored in this study. A sustained emphasis on the enhancement of occupational exposure prevention and control measures is advocated. Future strategies should encompass the implementation of routine screening and vaccination for medical staff, as well as the proactive promotion of safety devices such as sharps with injury prevention features. It is suggested that a combination of rewards and penalties be adopted to incentivize HCWs for the timely management, reporting, and regular review following an occurrence of OBEs.
Abbreviations
HCW, Health care worker; OBEs, Occupational blood exposures; NS, Nursing staff; WHO, World Health Organization; HBV, Hepatitis B Virus; HCV, Hepatitis C Virus.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
This study was conducted with approval from the Ethics Committee of Second Hospital of Hebei Medical University. This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff who implemented the intervention and evaluation components of the study.
Funding
No external funding received to conduct this study.
Disclosure
The authors declare that they have no competing interests.
References
1. Lee JH, Cho J, Kim YJ, et al. Occupational blood exposures in health care workers: incidence, characteristics, and transmission of bloodborne pathogens in South Korea. BMC Public Health. 2017;17(1):827. doi:10.1186/s12889-017-4844-0
2. Sahiledengle B, Tekalegn Y, Woldeyohannes D, Quisido BJE. Occupational exposures to blood and body fluids among healthcare workers in Ethiopia: a systematic review and meta-analysis. Environ Health Prev Med. 2020;25(1):58. doi:10.1186/s12199-020-00897-y
3. Naylor K, Torres A, Gałązkowski R, Torres K. Self-reported occupational blood exposure among paramedics in Poland: a pilot study. Int J Occup Saf Ergon. 2019;25(4):597–603. PMID: 29521581. doi:10.1080/10803548.2018.1450717
4. Bouya S, Balouchi A, Rafiemanesh H, et al. Global prevalence and device related causes of needle stick injuries among health care workers: a systematic review and meta-analysis. Ann Glob Health. 2020;86(1):35, 1–8. doi:10.5334/aogh.2698
5. Mengistu DA, Tolera ST, Demmu YM. Worldwide prevalence of occupational exposure to needle stick injury among healthcare workers: a systematic review and meta-analysis. Can J Infect Dis Med Microbiol. 2021;2021:9019534. doi:10.1155/2021/9019534
6. Mengistu DA, Dirirsa G, Mati E, et al. Global occupational exposure to blood and body fluids among healthcare workers: systematic review and meta-analysis. Can J Infect Dis Med Microbiol. 2022;2022:5732046. doi:10.1155/2022/5732046
7. Mannocci A, De Carli G, Di bari V, et al. How much do needlestick injuries cost? A systematic review of the economic evaluations of needlestick and sharps injuries among healthcare personnel. Infect Control Hosp Epidemiol. 2016;37(6):635–646. doi:10.1017/ice.2016.48
8. Wang D, Ye Y, Zheng Q. Cost of blood and body fluid occupational exposure management in Beijing, China. Int J Environ Res Public Health. 2020;17(12):4192. doi:10.3390/ijerph17124192
9. Jahic R, Piljic D, Porobic-Jahic H, et al. Epidemiological characteristics of the accidental exposures to blood-borne pathogens among workers in the hospital. Med Arch. 2018;72(3):187–191. doi:10.5455/medarh.2018.72.187-191
10. Cooke CE, Stephens JM. Clinical, economic, and humanistic burden of needlestick injuries in healthcare workers. Med Devices. 2017;10:225–235. doi:10.2147/MDER.S140846
11. World Health Organization. WHO Guideline on the Use of Safety Engineered Syringes for Intramuscular, Intradermal and Subcutaneous Injections in Health-Care Settings. Geneva, Switzerland: World Health Organization; 2015.
12. Sun J, Xu H, Gu AM, et al. 中国医务人员职业暴露与防护工作的调查分析[Investigation and analysis of occupational exposure and protection of medical personnel in China]. Chin J Infect Control. 2016;15(9):681–685. Chinese.
13. Cui Z, Zhu J, Zhang X, Wang B, Li X. Sharp injuries: a cross-sectional study among health care workers in a provincial teaching hospital in China. Environ Health Prev Med. 2018;23(1):2. doi:10.1186/s12199-017-0691-y
14. National Health and Family Planning Commission, People’s Republic of China. Guidelines for protection against occupational exposure to blood-borne pathogen; 2008.
15. National Health and Family Planning Commission of the People’s Republic of China. Hospital infection management standard; 2016.
16. Auta A, Adewuyi EO, Tor-Anyiin A, et al. Global prevalence of percutaneous injuries among healthcare workers: a systematic review and meta-analysis. Int J Epidemiol. 2018;47(6):1972–1980. doi:10.1093/ije/dyy208
17. Garus-Pakowska A, Górajski M. Behaviors and attitudes of polish health care workers with respect to the hazards from blood-borne pathogens: a questionnaire-based study. Int J Environ Res Public Health. 2019;16(5). doi:10.3390/ijerph16050891
18. d’Ettorre G; Gabriele d’ Ettorre. Needlestick and sharp injuries among registered nurses: a case–control study. Ann Work Expo Health. 2017;61(5):596–599. doi:10.1093/annweh/wxx027
19. Garus-Pakowska A, Górajski M, Szatko F. Did legal regulations change the reporting frequency of sharp injuries of medical personnel? Study from 36 hospitals in Łód ´z Province, Poland. Int J Occup Med Environ Health. 2018;31(1):37–46. doi:10.13075/ijomeh.1896.01045
20. Kocur E, Sliwa-Rak B, Grosicki S. Analysis of cases of occupational exposure to blood recorded in the city ´hospital in Zabrze in 2006–2015. Przegl Epidemiol. 2016;70(4):603–615.
21. Alemayehu T, Worku A, Assefa N. Sharp injury and exposure to blood and body fluids among health care workers in health care centers of eastern Ethiopia. Int J Occup Environ Med. 2016;7(3):172–180. doi:10.15171/ijoem.2016.714
22. Gabr HM, El-Badry AS, Younis FE. Risk factors associated with needlestick injuries among health care workers in menoufia governorate, Egypt. Int J Occup Environ Med. 2018;9(2):63–68. doi:10.15171/ijoem.2018.1156
23. Zhou MQ, Yin DP, Bai FQ, Sheng WW. 某三甲医院医务人员血源性职业暴露危险因素分析[Analysis of risk factors of blood-derived occupational exposure among medical staff in a third class hospital]. Chin J Nosocomiol. 2017;27(18):4290–4293. Chinese.
24. Sun XL, Xu GQ, Liu JF, Zhang HM, Wang YM, Hou GY. 医务人员血源性职业暴露调查及其对策[Investigation and countermeasures of blood-derived occupational exposure of medical staff]. Chin J Infect Control. 2018;17(05):440–443. Chinese.
25. Wang BH, Li L, Liu J, et al. 血源性病原体职业暴露特点及防控费用研究[Study on occupational exposure characteristics and prevention and control costs of blood-borne pathogens]. Chin J Infect Control. 2018;17(11):979–982. Chinese.
26. Sun JW, Han Y, Bai HY, Cao FL. 医务人员血源性传染病职业暴露后心理应激反应的纵向研究[Longitudinal study of psychological stress response of medical workers after occupational exposure to blood-borne infectious diseases]. Chin J Ment Health. 2017;31(03):190–194. Chinese.
27. Wang H. 医务人员血源性职业暴露后感知压力、创伤后应激症状及焦虑抑郁情绪[Perceived stress, post-traumatic stress symptoms and anxiety and depression after blood-borne occupational exposure in medical staff]. Chin J Health Psychol. 2018;26(09):1367–1370. Chinese.
28. Hebo HJ, Gemeda DH, Abdusemed KA. Hepatitis B and C viral infection: prevalence, knowledge, attitude, practice, and occupational exposure among healthcare workers of Jimma University medicalCenter, Southwest Ethiopia. ScientificWorldJournal. 2019;2019:9482607. doi:10.1155/2019/9482607
29. Liu SQ, Ren XX, Zhou T, Yang Q, Gao XD. 医务人员相关锐器伤及血源性暴露防护法律法规的国际经验总结[Summary of international experience in laws and regulations on protection against sharp force injuries and blood-borne exposure for medical personnel]. Chin J Nosocomiol. 2018;28(14):2228–2233. Chinese.
30. Reddy VK, Lavoie MC, Verbeek JH, et al. Devices for preventing percutaneous exposure injuries caused by needles in healthcare personnel. Cochrane Database Syst Rev. 2017;11(11):CD009740. doi:10.1002/14651858.CD009740.pub3
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
