Back to Journals » Risk Management and Healthcare Policy » Volume 17
Retrospective Investigation and Research on Fall Events Among Hospitalized Patients in the Rehabilitation Department
Authors Lin FF, Yang WY, Zhou JX, Cao LY, Huang LL
Received 20 October 2023
Accepted for publication 1 April 2024
Published 24 April 2024 Volume 2024:17 Pages 1069—1078
DOI https://doi.org/10.2147/RMHP.S445808
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Kyriakos Souliotis
Fang-Fang Lin,1 Wei-Yuan Yang,1 Jun-Xiang Zhou,1 Luo-Yuan Cao,2 Ling-Ling Huang1
1Department of Rehabilitation, Ningde Municipal Hospital Affiliated to Ningde Normal University, Ningde, 352000, People’s Republic of China; 2Department of Central Laboratory, Ningde Municipal Hospital Affiliated to Ningde Normal University, Ningde, 352000, People’s Republic of China
Correspondence: Jun-Xiang Zhou; Wei-Yuan Yang, Department of Rehabilitation, Ningde Municipal Hospital Affiliated to Ningde Normal University, No. 7 of Jiaocheng North Road, Jiaocheng District, Ningde, 352000, People’s Republic of China, Tel +86-15159370026 ; +86-13004929861, Email [email protected]; [email protected]
Objective: We investigated the clinical characteristics, fall outcomes, and related factors of falls in patients who were hospitalized in the rehabilitation department, and explored strategies to reduce the incidence of falls and prevent falls in patients.
Methods: Data from 60 patients who fell in the rehabilitation department between 2016 and 2021 were analyzed for clinical characteristics, associated factors, incidence of falls, injuries, and patient demographics. Under the random stratified sampling method, 60 patients who did not fall during the same period were selected as the control group, and relevant data was collected. Measurement data were compared using an independent sample t-test. Enumeration data were compared using chi-squared (χ2) test was employed to compare these data between the two groups. Non-parametric data were analyzed using the Mann–Whitney U-test. Factors potentially influencing falls were scrutinized through both univariate and binary logistic regression analyses.
Results: The median annual incidence of falls among patients who were hospitalized in the rehabilitation department was 0.04%, while the overall fall injury rate was 60%. Falls were most prevalent within 30 days of hospitalization (71.67%). The most common fall-related condition was craniocerebral disease (83.33%). The incidents of falls location of fall were mainly reported in nearby areas of rehabilitation ward (70%). Most accidents occurred between 7:00 a.m.– 12:00 p.m. and 3:01 p.m.– 6:00 p.m. (63.33%), and dyskinesia was the most common cause of falls (71.67%). There were 39 patients (65.00%) with Barthel Index (BI) scores ranging between 40– 60.
Conclusion: Patients in the rehabilitation department had a greater incidence of falls and fall injuries. Within 30 days of admission, patients with moderately dependent craniocerebral disorders and dyskinesia frequently experienced falls during typical daytime shifts in areas characterized by endemic conditions.
Keywords: daily living activities, dyskinesia, fall, hospitalized patients, rehabilitation department, retrospective analysis
Introduction
Fall events of hospitalized patients may not only result in physical injury, an increase medical expenses and prolong hospitalization days, but they can also easily lead to medical disputes, thereby negatively impacting the relationship between doctors and patients, which is not conducive to further treatment of patients.1 Management of fall prevention has become an important aspect of hospital management.2 Scholars have attempted to prevent falls through various strategies, such as the use of risk assessment tools to predict the risk of falling, multi-factor nursing intervention, and evaluating the activity ability of patients, but falls are still common among hospitalized patients.3–6 Based on a survey conducted by Wu et al, which covered 490 tertiary hospitals across China, there was an annual increase in the incidence of falls among hospitalized patients from 2014 to 2017. By 2017, the median incidence rate of falls had reached 0.054‰, with the median injury rate from falls at 73.68%.7
Most hospitalized patients in the rehabilitation department have difficulty in moving and have a high frequency of falling. Reducing the incidence of falls and injuries among hospitalized patients has become a crucial medical and nursing task in the rehabilitation department. The purpose of this study is to retrospectively analyze the clinical features, causes, and outcomes of falls among 60 hospitalized patients in the rehabilitation department over the past 6 years, and put forward management countermeasures to prevent falls among hospitalized patients in the rehabilitation department, so as to provide reference for enhancing the safety management level of hospitalized patients. The report is as follows:
Materials and Methods
General Material
In this study, falls refer to a sudden, involuntary, and unintentional changes in position, resulting in falling to the ground or a lower plane. The data of adverse falls of hospitalized patients in the Department of Rehabilitation in our hospital from January 1, 2016 to December 31, 2021 were obtained retrospectively. Inclusion criteria: (1) Hospitalized patients in the rehabilitation department; (2) Adverse events of falling, including falling off the bed based on the Management Measures for Nursing Adverse Events; (3) Complete incident records. Exclusion criteria: More than 20% of the reported information is missing and cannot be supplemented by other means.
This study was a retrospective review of medical records, and the acquired data did not include any identifying information of the research participants. A total of 60 cases of falls were collected using the hospital nursing adverse event reporting system, and were designated as the fall group, which included 41 males and 19 females, with an average age of 59.45±16.38 years old. Simultaneously, using the stratified sampling method, 60 patients who did not fall in the same timeframe were randomly selected as the control group, and the relevant data were collected. There were 30 males and 30 females, with an average age of 46.13 ± 22.57 years in the control group.
Methods
The study of patients within the fall group comprised of two parts: a structured questionnaire and a standardized evaluation scale. These assessments were implemented within 48 hours subsequent to the fall incident. For the structured questionnaire, the following parameters were captured: Demographics: name, age, gender, and educational level, medical history: significant ailments and associated medications. Fall incidents during hospital stay: number of days since admission, timing, locale, causative factors, and any adverse outcomes following the fall. Presence or absence of caregivers during the fall. Furthermore, evaluations were conducted concerning daily living capabilities, motor functionality, sensory ability, and cognitive capacities at the time of the fall. The Barthel Index (BI) was employed to assess the Activities of Daily Living (ADL) of the patients.8 The scoring criteria were as follows: 0–40 points: signifies high dependency; 41–60 points: indicates moderate dependency; 61–99 points: denotes mild dependency; 100 points: represents complete independence. Motor function assessment encompassed aspects such as muscular strength, tone, and equilibrium, as well as coordination capabilities. Any deviations from the norm were flagged as positive. Similarly, evaluations for sensory abilities, speech functionality, and cognitive capabilities were conducted through primary complaints and physical examinations. Any identified abnormalities in these areas were also deemed positive. For the control group, analogous data was sourced through a thorough review of their medical records.
Fall injuries were classified based on the severity of the injury sustained post-fall, potentially ranging from minor physical injury to fatalities. The specific categorizations are outlined as follows:7 (1) None: The patient experienced no injury. (2) Level 1 severity (Mild): Minimal injury requiring little to no medical intervention, encompassing injuries like abrasions, contusions, or minor lacerations that do not necessitate suturing. (3) Level 2 severity (Moderate): More substantial injury demanding medical or nursing interventions such as ice applications, bandaging, suturing, or splinting. This includes injuries like sprains, significant or deep lacerations, skin tears, or minor contusions. (4) Level 3 severity (Severe): Serious injury that mandates medical treatments and potentially specialist consultations. Injuries in this category include fractures, loss of consciousness, or any significant change in cognitive or physical states. (5) Death. The proportion of fall injuries of a particular severity grade within a year = the number of fall injuries at that specific severity grade / by the total number of fall injury incidents in that year x 100%.7
Statistical Methods
The dataset was subjected to statistical analysis using IBM SPSS version 26.0. Measurement data are presented as mean ± standard deviation (X±S). A normality check was performed on the data, and the comparison between the two groups was executed using an independent sample t-test. Enumeration data are expressed in terms of frequency, composition ratio (%), and incidence rate (%). The chi-squared (χ2) test was employed to compare these data between the two groups. Non-parametric data are expressed as the median and interquartile range [M (P25, P75)], and their comparison was carried out using the Mann–Whitney U-test. Factors potentially influencing falls were scrutinized through both univariate and binary logistic regression analyses. The significance threshold was set at α = 0.05, and any results with P < 0.05 were considered statistically significant.
Results
Comparative Analysis of Demographic and Clinical Characteristics in Fall and Control Groups
The age, gender, major diseases, medication history, education level, accompanying conditions and dysfunction (motor, sensory, speech, cognitive and ADL) were compared between the two groups (Table 1). Patients in the fall group was significantly older than that in the control group (P < 0.01). In the fall group, there were more male patients, patients with brain diseases, patients with medication history and accompanying patients than those in the control group (P< 0.05). The patients with motor, sensory and speech disorders in the fall group were more than those in the control group (P < 0.01). The median BI score in the fall group was significantly lower than that in the control group. The aforementioned differences were statistically significant. There was no significant difference between the two groups in terms of education level, hospitalization days and cognitive impairment (P ≥ 0.05).
 |
Table 1 Comparison of Related Factors Between Fall and Control Groups |
Binary Logistic Regression Analysis of the Influencing Factors of Falls
The factors with statistically significant differences in univariate analysis were taken as independent variables, their corresponding values were assigned, and a series of binary logistic regression analyses were conducted one by one with whether the fall occurred as the dependent variable. Age, diagnosis, medication history, dyskinesia (determined by a doctor’s physical examination, and motor functions include muscle strength, muscle tension, range of motion, balance ability, coordination ability. Any item that cannot reach a normal state is defined as dyskinesia), sensory disorder, language disorder, and BI score (activity of daily life) were the influencing factors of falls among hospitalized patients based on the logistic regression analysis (P < 0.05) (Table 2).
 |
Table 2 Analysis of the Factors Causing Falls Using a Single Factor Binary logistic Regression |
Falling Process
- Significantly more falls occurred during the first 30 days of hospitalization than during later hospitalization periods (Table 3).
- During the daytime hours of 7:00 a.m. to 12:00 p.m. and 3:01 p.m. to 6:00 p.m., there were 38 cases (63.33%) of normal work-related falls, higher than any other period (Table 4).
- The majority of fall incidents predominantly took place in wards, encompassing both the ward rooms and their adjacent corridors. Out of the total cases, 42 or 70%, of the falls were recorded in these areas, indicating a higher incidence rate in these locales compared to other locations (Table 5).
- Analyzing the underlying causes for the 60 fall incidents, dyskinesia emerged as the most prevalent reason. Specifically, 43 out of the 60 cases or 71.67%, were attributed to dyskinesia, which included manifestations such as unstable standing and incorrect transfer methods. This cause was notably higher than other reasons identified. For instance, unfavorable daily activities (eg, inflexibility, incoordination, and imprecision of movement, excluding unstable standing and improper transfer. For example, when a fall is about to occur, the body cannot respond in time or react incorrectly due to limited activity, and cannot make protective actions to further prevent falls. Such as falling off the bed, getting things) were responsible for 7 cases (11.67%), environmental factors like wet floors or inconvenient restroom facilities were the cause for 4 cases (11.67%), and other disease-related factors, including episodes like seizures, accounted for 2 cases (3.33%) (Table 6).
- The BI scores for patients within the fall group predominantly ranged between 40 and 60. Specifically, out of the total, 39 cases or 65% of the patients had BI scores within this 40–60 range (Table 7, Figure 1).
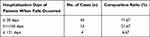 |
Table 3 Hospitalization Days of Patients Who Suffered Falls (n = 60) |
 |
Table 4 Time Distribution of Falls (n = 60) |
 |
Table 5 Distribution of the Area Where the Fall Occurred (n = 60) |
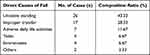 |
Table 6 Direct Causes of Fall (n,%) |
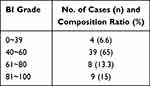 |
Table 7 BI Scores of the Two Patient Groups [n (%)] |
 |
Figure 1 BI score distribution of falls among 60 patients. |
Fall Rate and Fall Injury in the Rehabilitation Department from 2016 to 2021
The median fall rate stood at 0.04%, and the median fall injury rate was observed at 54%. Out of 60 patients who fell, 36 sustained injuries, translating to a fall injury rate of 60.00%. This includes 19 cases of Level 1 soft tissue injuries (52.78%), 10 cases categorized under Level 2 injuries (27.78%), and 7 cases falling under Level 3 injuries, of which 2 involved cerebral hemorrhages and 5 pertained to fractures, representing 9.44% of the total. Additionally, one major medical dispute arose as a result of these incidents (Table 8).
 |
Table 8 Fall Rate and Fall Injury Rate (n, %) of 60 Patients Between 2016 and 2021 |
Discussion
In our study, focusing on the rehabilitation department from 2016 to 2021, also observed a rising trend in fall incidents. However, the fall rate in this department was markedly higher than the national average reported by Wu et al. Specifically, the median annual fall rate in the rehabilitation department stood at 0.04%, which is a staggering 7.4 times the national median for hospitalized patients in 2017. This indicates that patients in the rehabilitation department face a significantly higher risk of falling compared to patients in other departments within general hospitals. Moreover, the injury rate resulting from these falls in the rehabilitation department was also notably higher, registering at 59.61%. This disparity in fall rates and injury outcomes between the rehabilitation department and other hospital departments may be attributed to the unique characteristics of diseases treated in rehabilitation, as well as the specific treatment and nursing modalities employed within the department. Further analyses, as presented in this paper, delve into these distinctions and their implications.
Disease Characteristics of Hospitalized Patients in the Rehabilitation Department
The majority of hospitalized patients in the rehabilitation department are diagnosed with cerebrovascular diseases. Alongside this primary diagnosis, many also suffer from chronic underlying conditions such as hypertension, diabetes, and coronary heart disease, which necessitate continuous medication. Furthermore, many experience psychological and neurological challenges like anxiety, depression, insomnia, and pain, leading to the administration of sedatives and analgesics. In this study of 60 patients who experienced falls, the predominant diagnosis was brain-related diseases, with 50 cases (or 83.33%) fitting this profile. A significant 90% of these patients had a medication history that included prolonged use of anti-hypertensives drugs, hypoglycemic drugs, antiepileptics drugs, muscle relaxants, sedatives, analgesics, and antidepressants. The utilization of these drugs, whether in isolation or in combination, can trigger adverse reactions such as hypoglycemia, postural hypotension, morning fatigue, dizziness, and more. Such side effects can result in delayed reactions or diminished cognitive functions, subsequently elevating the risk of falls.9,10 Worryingly, the majority of these patients remain uninformed about the potential fall risks associated with these medications.11 The findings of this study underscore that both the diagnosis of brain diseases and the medication history of the patient are significant factors influencing the likelihood of falls (P < 0.01, as demonstrated in Tables 1 and 2). Therefore, for patients in the rehabilitation department diagnosed with craniocerebral diseases and with a concurrent medication history, it is imperative to regularly monitor their blood pressure and glucose levels and assess their mental states. Efforts should also be made to streamline their medication regimens to reduce potential drug interactions and side effects.12 Equally crucial is the need to bolster educational initiatives to enhance the comprehension of related drugs among patients, ensuring they are better informed, thereby aiding in fall prevention.
Patients admitted to the rehabilitation department typically present with a multitude of functional impairments, including muscle atrophy, weakness, abnormal muscle tension, restricted joint mobility, and balance disturbances. These conditions inevitably diminish their motor control capabilities. There is a significant body of evidence suggesting that decreased motor abilities are closely tied to the risk of falls.13,14 Our analysis, which used binary logistic regression, revealed that motor dysfunction, sensory impairment, and speech disorders were significant influencing factors linked to falls (P < 0.01, as noted in Tables 1 and 2). Within our cohort of 60 patients who experienced falls, a striking 95% (or 57 patients) had motor dysfunctions. Moreover, 43 of these patients (or 71.6%) experienced falls directly attributable to these motor dysfunctions, manifesting as unstable standing, walking instabilities, and inappropriate transfer techniques (as outlined in Tables 1 and 6). Additionally, we identified sensory disturbances in 41 of the 60 patients, translating to 68.33% (Table 1). Most of these sensory disturbances pertained to tactile sensations like touch, pain, and temperature, particularly deeper sensations such as proprioception and vibratory sensations. Such deficits inevitably compromise motion perception, anticipatory judgment, and movement accuracy, leading to falls.15,16 Of the study cohort, 30 patients (or 50%) exhibited speech disorders (Table 1). Patients with communication difficulties tend to be reticent to request assistance, often taking independent actions without consultation, leading to falls. Furthermore, our study highlighted cases of patients with cognitive impairments, notably those with decreased attention spans.17 Especially concerning were patients with unilateral neglect who, despite the weakness in their limbs, erroneously believed they could execute movements like sitting and standing without assistance, culminating in falls. Unilateral neglect, also known as unilateral spatial neglect (unilateral spatial neglect) or unilateral neglect (unilateral neglect), is a kind of cognitive impairment caused by brain damage. It is characterized by the absence of sensory perception of the affected limb or body, resulting in the inability to notice stimuli from the affected side, including visual, hearing, touch sensation, and recognition of body parts. This disorder is often related to the patient’s ability to spatially localize, as manifested by a greater tendency to ignore objects or regions that are more distant from the central axis of the body. Unilateral neglect is common in clinical practice, especially after stroke, and it is more common in right stroke. Patients with unilateral neglect are more likely to fall. Given these findings, it becomes paramount for the rehabilitation department to amplify the precision and comprehensiveness of their assessments. This includes conducting detailed evaluations of mobility, balance, sensory, and cognitive functions. By tailoring rehabilitation interventions and implementing prolonged and vigilant fall prevention strategies, patient outcomes can be improved.
Age is indeed a recognized factor influencing the probability of falls.18,19 As age progresses, there is a natural decline in organ functions, sensory acuity diminishes, and reflexes and response times deteriorate. Consequently, older patients are more susceptible to falls, and the injuries sustained from such falls tend to be more severe.20 In the rehabilitation department, a significant proportion of the patient population consists of middle-aged and elderly patients. An analysis of the 60 patients who experienced falls in this study revealed a trend: the average age for male patients was 59.44 ± 16.32 years, while for female patients it was 59.40 ± 16.40 years. These averages are significantly higher than those observed in the control group (P < 0.01, as shown in Tables 1 and 2). When compared to other departments in general hospitals, the rehabilitation department tends to cater to an older demographic, who are inherently at a higher risk of falls. Thus, given the inherent vulnerabilities of this age group, it becomes imperative for the rehabilitation department to prioritize and intensify their fall prevention and management strategies, especially for elderly patients.
Treatment Mode of Hospitalized Patients in Rehabilitation Department
The treatment approach in the rehabilitation department is notably distinct, emphasizing a team-based collaborative approach that stands in contrast to traditional medical or surgical treatments.21 This team comprises of rehabilitation physicians, nurses, therapists, among other professionals. Predominantly, treatment sessions are conducted within wards and designated rehabilitation treatment rooms, with patients frequently needing to transition to these treatment rooms.
In our study of 60 fall incidents, a significant 70% (or 42 cases, as outlined in Table 5) took place within the ward area, inclusive of the ward corridors. These incidents predominantly occurred during regular daytime shifts, specifically between 7:00 a.m.–12:00 p.m. and 3:01 p.m.–6:00 p.m., with 38 cases (or 63.33%, as seen in Table 4) happening in these periods. Most falls during these times were associated with patients transitioning: either preparing to move from the ward to the treatment room, en route between the ward and treatment room, or actively undergoing rehabilitation treatments that necessitated bodily position changes and movements such as transfers from bed to chair, sitting-to-standing practices, and walking exercises. Given these findings, it is clear that enhanced vigilance is required during these high-risk periods. Nurses, especially, should amplify their oversight in wards during regular daytime shifts, providing guidance and oversight for the daily activities of patients to mitigate fall risks. Another noteworthy observation was that 16.67% (or 10 cases, referenced in Table 5) of falls occurred within the rehabilitation treatment room. Some of these were under the supervision of rehabilitation therapists or occurred post-treatment when patients practiced exercises independently. The primary role of rehabilitation therapists revolves around facilitating the rehabilitation training of the patients, leaving them less engaged in proactive fall prevention management and potentially leading to a less developed fall prevention awareness. To bridge this gap, it is imperative to foster active involvement of rehabilitation therapists in fall prevention management, enhancing their awareness and commitment to reducing fall risks, particularly within treatment spaces.22
Nursing Mode of Hospitalized Patients in the Rehabilitation Department
Beyond the conventional nursing tasks like daily monitoring of the vital signs of the patients, administrating infusion therapy, and preventing bedsores, rehabilitation nurses have a unique set of responsibilities tailored to the specific needs of their department and its patients. Integral to their role is orienting patients to the ward environment, elucidating the rehabilitation treatment process, and guiding patients on effectively collaborating with rehabilitation physicians to undergo relevant evaluations and consultations. Moreover, rehabilitation nurses play a pivotal role in addressing and ameliorating dysfunctions among patients.23 A significant aspect of their job is to supervise and guide the training related to the Activities of Daily Living (ADL) among the patients within the ward.
This study highlighted that the majority of fall incidents happened within the initial 30 days of hospitalization, accounting for 43 cases or 71.67% (as detailed in Table 3). This pattern can likely be attributed to the unfamiliarity of the patients with the ward environment and the nuances of the rehabilitation treatment process shortly after admission. Moreover, a significant portion of these falls, 33 cases or 55%, took place within the ward, particularly around the bedside and toilet areas. Factors like wet floors, insufficient lighting, unfamiliarity with the operation of fixtures such as sinks and toilets, and a general lack of acclimatization to the ward environment can be the potential reasons behind these incidents. Prior research has indicated that as many as 67.39% of falls among hospitalized patients can be traced back to environmental factors. Implementing a comprehensive ward environment assessment is shown to proactively identify and address such environment-related fall risk factors, thus significantly reducing the chances of fall occurrences.24 Consequently, hospitalized patients in the rehabilitation department should optimize the hospitalization process, strengthen the environmental assessment of the ward and treatment room, improve the hospitalization environment, enhance the familiarity of the patient with the environment, guide the patient to operate the bed, chair, lamp, call bell, ward armrest, and toilet utensils in the ward, and evaluate and supervise the daily life activities of the patient in order to further reduce the incidence of falls.
The ability to perform activities of daily living is intricately linked to the risk of falling.25 Furthermore, the significance of recognizing and evaluating ADL capabilities has increasingly become a focal point of attention in medical and rehabilitation communities.26 In our study, the BI scores, a measure of ADL, were notably lower in the fall group compared to the control group, clearly highlighting the ADL capabilities as one of the determinants affecting the likelihood of falls (as corroborated by the statistical significance of P < 0.01 in Tables 1 and 2). Delving deeper into the fall group, 65% of these patients, or 39 out of the 60, had BI scores that ranged between 40 and 60 (as presented in Table 7 and visually depicted in Figure 1).
This data suggests that patients who exhibit moderate dependence in their self-care activities have some mobility. However, this mobility is marred by limited range and poor motor control. Despite these limitations, these patients often exhibit a strong inclination to move. Their eagerness to be mobile, combined with their suboptimal motor skills, makes them particularly challenging to manage from a care perspective, elevating their risk of falls. Given this, there is a pressing need to amplify the evaluation and screening processes related to ADL. Special emphasis should be placed on patients categorized with moderate dependence. Comprehensive management strategies should be implemented to preclude falls in this specific demographic, ensuring their safety while respecting their autonomy and desire for mobility.
The rehabilitation department, catering primarily to hospitalized patients with various dysfunctions, often necessitates round-The-clock assistance for these patients. In this context, caregivers, be they family members or professional aides, play a pivotal role in mitigating the risks associated with falls. Their involvement and understanding of fall prevention measures are critical to ensuring patient safety. In the study of 60 patients who experienced falls in this study, some were unaccompanied at the time of the fall, totaling 9 cases.
In certain instances, even though caregivers were present, they had momentarily stepped away without implementing adequate protective measures for the patient.
Furthermore, there were situations where, despite the presence of caregivers during the fall, they were positioned too distantly from the patient to intervene effectively and prevent the fall. A common thread running through many of these incidents is a potential lack of awareness or underestimation of the fall risk on the part of the caregivers. Many might operate under the misconception that patients are not prone to falling, or they may not fully comprehend the severity of consequences associated with falls. To address this gap, it is imperative to intensify educational efforts targeting both patients and their caregivers.27 This would entail comprehensive briefings on the risks associated with falls, the importance of constant vigilance, and effective preventative strategies tailored to individual needs and dysfunctions of the patients. Furthermore, both caregivers and patients should be encouraged to actively participate in fall prevention management.28
Conclusions
Patients in the rehabilitation department had a greater incidence of falls and fall injuries. Within 30 days of admission, patients with moderately dependent craniocerebral disorders and dyskinesia frequently experienced falls during typical daytime shifts in areas characterized by endemic conditions. The management of fall prevention in these patients should be improved by enhancing assessment and screening, patient education, environmental optimization, focused rehabilitation training, and increasing patient and rehabilitation therapist participation. This approach aims to optimize the hospitalization process and environment, refine fall prevention education methods, enhance patients’ physical capabilities, and encourage active participation of patients, caregivers, and rehabilitators in fall prevention activities.29,30
Abbreviations
BI, Barthel Index; ADLL, Activities of daily living.
Data Sharing Statement
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Ningde Municipal Hospital Affiliated to Ningde Normal University (NSYKYLL-2023-058). A written informed consent was obtained from all participants.
Consent for Publication
Consent for publication was obtained from every individual whose data are included in this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Dykes PC, Duckworth M, Cunningham S, et al. Pilot Testing Fall TIPS (Tailoring Interventions for Patient Safety): a patient-centered fall prevention toolkit. Jt Comm J Qual Patient Saf. 2017;43(8):403–413. PMID: 28738986. doi:10.1016/j.jcjq.2017.05.002
2. China Hospital Association. China Hospital Association Patient Safety Objectives (2019 Edition). China Health. 2019;25(12):57–58.
3. Kim YJ, Choi KO, Cho SH, Kim SJ. Validity of the morse fall scale and the Johns Hopkins fall risk assessment tool for fall risk assessment in an acute care setting. J Clin Nurs. 2022;31(23–24):3584–3594. PMID: 34964175. doi:10.1111/jocn.16185
4. Welch SA, Ward RE, Beauchamp MK, Leveille SG, Travison T, Bean JF. The Short Physical Performance Battery (SPPB): a quick and useful tool for fall risk stratification among older primary care patients. J Am Med Dir Assoc. 2021;22(8):1646–1651. PMID: 33191134; PMCID: PMC8113335. doi:10.1016/j.jamda.2020.09.038
5. Barker AL, Morello RT, Wolfe R, et al. 6-PACK programme to decrease fall injuries in acute hospitals: cluster randomised controlled trial. BMJ. 2016;352:h6781. PMID: 26813674; PMCID: PMC4727091. doi:10.1136/bmj.h6781
6. Moreira NB, Rodacki ALF, Pereira G, Bento PCB. Does functional capacity, fall risk awareness and physical activity level predict falls in older adults in different age groups? Arch Gerontol Geriatr. 2018;77:57–63. PMID: 29673964. doi:10.1016/j.archger.2018.04.002
7. Wu ZJ, Shang WH, Jian WY, Yao L, Zhang HY. Analysis of the current situation of falls in hospitalized patients in China: based on a Survey of 490 Third Class A Hospitals. Health Qual Manage China. 2019;26(3):14–17.
8. Min Y, Wu YY, Yan TB. A study on the validity and reliability of the Modified Barthel Index (Simplified Chinese Version) Scale in Evaluating Activities of Daily Living in Stroke Patients. Chin J Phys Med Rehabil. 2008;3:185–188.
9. Zhou CX, Sun LL, Wang ZD, et al. Study on the effect of cluster education model on improving the cognition of falls related drugs in elderly people. Chin J Crit Care Med. 2021;14(3):261–264.
10. Shaver AL, Clark CM, Hejna M, Feuerstein S, Wahler RG, Jacobs DM. Trends in fall-related mortality and fall risk increasing drugs among older individuals in the United States, 1999–2017. Pharmacoepidemiol Drug Saf. 2021;30(8):1049–1056. PMID: 33534172; PMCID: PMC8254780. doi:10.1002/pds.5201
11. Haddad YK, Karani MV, Bergen G, Marcum ZA. Willingness to change medications linked to increased fall risk: a comparison between age groups. J Am Geriatr Soc. 2019;67(3):527–533. PMID: 30548593; PMCID: PMC6647846. doi:10.1111/jgs.15696
12. Bartlett D, Pang N, Massey C, Evans P. Pharmacist consultations: simplifying daily drug regimens and providing education on fall risk for older adults. Consult Pharm. 2015;30(3):141–152. PMID: 25760664. doi:10.4140/TCP.n.2015.141
13. Zhang DD, Xi H, Qi HM, et al. A study on the correlation between decreased intrinsic ability and falls in elderly people. Chin J Geriatrics. 2020;39(10):1182–1185.
14. Paillard T. Methods and strategies for reconditioning motor output and postural balance in frail older subjects prone to falls. Front Physiol. 2021;12:700723. doi:10.3389/fphys.2021.700723
15. Liu D, Guo ZQ, Tian E, Zhu YT, Xu WC, Zhang SL. Clinical effects of multi-sensory training and rehabilitation therapy on patients with balance disorders. Chin J Med. 2021;101(26):2050–2054.
16. Iwasaki S, Yamasoba T. Dizziness and imbalance in the elderly: age-related decline in the vestibular system. Aging Dis. 2014;6(1):38–47. PMID: 25657851; PMCID: PMC4306472. doi:10.14336/AD.2014.0128
17. Westlake KP, Johnson BP, Creath RA, Neff RM, Rogers MW. Influence of non-spatial working memory demands on reach-grasp responses to loss of balance: effects of age and fall risk. Gait Posture. 2016;45:51–55. PMID: 26979883; PMCID: PMC4794637. doi:10.1016/j.gaitpost.2016.01.007
18. Jeon YK, Jeong J, Shin SD, et al. The effect of age on in-hospital mortality among elderly people who sustained fall-related traumatic brain injuries at home: a retrospective study of a multicenter emergency department-based injury surveillance database. Injury. 2022;53(10):3276–3281. PMID: 35907679. doi:10.1016/j.injury.2022.07.036
19. Wang Z, Hu Y, Peng F. Long-term trends in unintentional fall mortality in china: a population-based age-period-cohort study. Front Public Health. 2021;9:749295. PMID: 35024364; PMCID: PMC8744467. doi:10.3389/fpubh.2021.749295
20. Bhattacharya B, Maung A, Schuster K, Davis KA. The older they are the harder they fall: injury patterns and outcomes by age after ground level falls. Injury. 2016;47(9):1955–1959. PMID: 27346422. doi:10.1016/j.injury.2016.06.019
21. Huang XL, Yan TB. Rehabilitation Medicine.
22. Su XX, Zhao M, Li SG. A survey on the application status of fall prevention evidence in elderly inpatients in 81 tertiary and first-class comprehensive hospitals. Chin J Pract Nurs. 2021;37(22):1716–1722.
23. Giovannini S, Brau F, Forino R, et al. Sarcopenia: diagnosis and management, state of the art and contribution of ultrasound. J Clin Med. 2021;10(23):5552. PMID: 34884255; PMCID: PMC8658070. doi:10.3390/jcm10235552
24. Giovannini S, Onder G, van der Roest HG, et al.; SHELTER Study Investigators. Use of antidepressant medications among older adults in European long-term care facilities: a cross-sectional analysis from the SHELTER study. BMC Geriatr. 2020;20(1):310. PMID: 32854659; PMCID: PMC7457305. doi:10.1186/s12877-020-01730-5
25. Yokoya T, Demura S, Sato S. Relationships between physical activity, ADL capability and fall risk in community-dwelling Japanese elderly population. Environ Health Prev Med. 2007;12(1):25–32. PMID: 21432078; PMCID: PMC2723624. doi:10.1007/BF02898189
26. Martins LM, Ribeiro NF, Soares F, Santos CP. Inertial data-based ai approaches for ADL and fall recognition. Sensors. 2022;22(11):4028. PMID: 35684649; PMCID: PMC9185447. doi:10.3390/s22114028
27. Naseri C, McPhail SM, Morris ME, et al. Tailored education increased capability and motivation for fall prevention in older people after hospitalization. Front Public Health. 2021;9:683723. PMID: 34414157; PMCID: PMC8369365. doi:10.3389/fpubh.2021.683723
28. Dykes PC, Burns Z, Adelman J, et al. Evaluation of a patient-centered fall-prevention tool kit to reduce falls and injuries: a nonrandomized controlled trial. JAMA Network Open. 2020;3(11):e2025889. PMID: 33201236; PMCID: PMC7672520. doi:10.1001/jamanetworkopen.2020.25889
29. Suh M, Cho I. Effectiveness of nursing care provided for fall prevention: survival analysis of nursing records in a tertiary hospital. Jpn J Nurs Sci. 2021;18(2):e12403. PMID: 33448157. doi:10.1111/jjns.12403
30. Keuseman R, Miller D. A hospitalist’s role in preventing patient falls. Hosp Pract. 2020;48(Sup1):63–67. PMID: 32053043. doi:10.1080/21548331.2020.1724473
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
