Back to Journals » Infection and Drug Resistance » Volume 17
Retrospective Analysis of the Efficacy and Safety of Endoscopic Spinal Tuberculosis Focus Removal versus Posterior Pedicle Lesion Removal, Bone Grafting, and Internal Fixation Combined with Drug Chemotherapy for Thoracolumbar Tuberculosis
Authors Abudurexiti T, Haibier A , Yusufu A, Shoukeer K, Lin H
Received 13 November 2023
Accepted for publication 7 February 2024
Published 26 February 2024 Volume 2024:17 Pages 733—748
DOI https://doi.org/10.2147/IDR.S449684
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Tuerhongjian Abudurexiti,1,2,* Abuduwupuer Haibier,1,2,* Alimujiang Yusufu,1,2,* Kutiluke Shoukeer,1,2,* Hang Lin1,2
1Department of Spine surgery, The Sixth Affiliated Hospital of Xinjiang Medical University, Orthopaedic Hospital of Xinjiang Uygur Autonomous Region, Urumqi, People’s Republic of China; 2Xinjiang Medical University, Urumqi, Xinjiang Uygur Autonomous Region, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Tuerhongjian Abudurexiti, Email [email protected]
Objective: This study aims to investigate the clinical efficacy of endoscopic spinal tuberculosis focus removal, posterior pedicle lesion removal, bone grafting, and internal fixation combined with drug chemotherapy in treating thoracolumbar tuberculosis. It also seeks to summarize strategies for preventing complications and provide a reference for clinical treatment.
Methods: We retrospectively analyzed 105 patients with spinal tuberculosis treated in our hospital from January 2018 to December 2022. Patients were divided into two groups: Group A (n=38), who underwent endoscopic spinal tuberculosis focus removal, and Group B (n=67), who underwent posterior pedicle lesion removal, bone grafting, and internal fixation. All patients received preoperative quadruple anti-tuberculosis drug chemotherapy (Isoniazid, Rifampicin, Pyrazinamide, Ethambutol) for 2– 4 weeks. We recorded and compared parameters such as operation time, intraoperative blood loss, postoperative drainage, recovery time, hospital stay, blood transfusion, and complications. We also compared pre- and postoperative lumbar VAS, ODI, erythrocyte sedimentation rate, C-reactive protein, Procalcitonin, D-Dimer, Neutrophil to Lymphocyte ratio, hemoglobin, total protein, and Cobb angle to evaluate kyphotic deformity and correction.
Results: Preoperative data including age, sex, body mass index, segment involvement, past medical history, smoking history, preoperative erythrocyte sedimentation rate, C-reactive protein, Procalcitonin, D-Dimer, Neutrophil to Lymphocyte ratio, hemoglobin, total protein, lumbar VAS score, lumbar ODI score, and spinal Cobb’s angle showed no significant difference between the groups (P> 0.05). Main postoperative indicators revealed that Group A had significantly lower lumbar VAS scores, higher hemoglobin and total protein levels, and a lower recurrence rate than Group B at the last follow-up (P< 0.05). Secondary postoperative indicators showed that Group A required significantly less blood transfusion, had shorter operative time, less intraoperative blood loss, shorter postoperative hospitalization time, and lower Cobb Angle than Group B (P< 0.05).
Conclusion: Endoscopic spinal tuberculosis focus removal can achieve comparable safety to posterior pedicle lesion removal, bone grafting, and internal fixation, with shorter operation time, less intraoperative bleeding, lower postoperative recurrence rate, and less postoperative drainage. This method can effectively improve blood sedimentation, lumbar function, restore Cobb angle, and reduce pain, making it worthy of promotion and application.
Keywords: spinal tuberculosis, focus clearance, infectious diseases of spine, drug chemotherapy
Introduction
Tuberculosis (TB) is a chronic, non-specific infectious disease caused by Mycobacterium tuberculosis.1 Each year, over 8 million new TB cases and 1.3 million deaths are reported. Despite a declining incidence due to increased emphasis and standardization of treatment, China remains one of the countries with the highest tuberculosis burden worldwide.2 According to World Health Organization (WHO) data, the annual number of tuberculosis cases reported in China accounts for approximately 10% of the global total.3,4
Spinal tuberculosis is the most common type of extrapulmonary TB, with thoracolumbar tuberculosis being the most prevalent form, accounting for 50% of osteotuberculosis cases. Thoracolumbar tuberculosis can significantly impact health and quality of life, causing pain and neurological dysfunction. It is more common in the elderly due to factors such as decreased immune function, weakened resistance, and the presence of chronic diseases. However, treating older patients is challenging, and the long postoperative rehabilitation period poses significant challenges to clinical treatment.5
Surgical strategies for treating spinal TB include thorough removal of infected TB foci, performing standardized and effective anti-TB therapy, facilitating functional recovery, and rebuilding the stability of the spine. Traditional thoracolumbar tuberculosis surgery involves open surgery to expose the patient’s spine through a large incision and remove the infected vertebra and intervertebral disc tissue to achieve a thorough treatment effect.6 Although traditional posterior pedicle lesion removal, bone grafting, and internal fixation are suitable for a variety of different types and severity of thoracolumbar tuberculosis cases, allowing for flexible surgical design according to individual conditions and lesion characteristics, they result in large trauma and severe postoperative pain, leading to a long rehabilitation cycle.7,8
In contrast, endoscopic spinal tuberculosis focus removal combined with medical chemotherapy is an emerging minimally invasive surgical approach.9 This technique, based on medical therapy, involves entering the patient’s thoracic or lumbar region through small skin incisions using a percutaneous endoscopic technique. Through endoscopy, doctors can directly visualize the infected vertebrae and intervertebral discs, and use special tools to remove, lavage, and drain the lesions.10 Compared with posterior pedicle lesion removal, bone grafting, and internal fixation, this method has the advantages of being minimally invasive, causing less trauma, having a short rehabilitation period, and reducing the risk of postoperative pain and complications.
In this study, we treated 105 patients with endoscopic spinal tuberculosis focus removal and posterior pedicle lesion removal to investigate the differences in the efficacy and safety of these two treatments in thoracolumbar patients.
Objects and Methods
Design
Retrospective cohort study
Time and Location
This study was conducted in the Spine Surgery Department at the Sixth Affiliated Hospital of Xinjiang Medical University from January 2018 to December 2022.
Object
The Spine Surgery Department of the Sixth Affiliated Hospital of Xinjiang Medical University treated 105 patients with thoracolumbar tuberculosis using endoscopic spinal tuberculosis focus removal and posterior pedicle lesion removal, bone grafting, and internal fixation from January 2018 to December 2022. Patients were divided into two groups according to the different surgical methods: posterior pedicle lesion removal, bone grafting, and internal fixation (n=67) and endoscopic spinal tuberculosis focus removal (n=38). The study was reviewed and approved by the Ethics Committee of the Sixth Affiliated Hospital of Xinjiang Medical University.
Inclusion Criteria
①Patients with a history of tuberculosis, clinical manifestations, laboratory and imaging examinations suggestive of thoracolumbar tuberculosis; ②intractable low back pain, no relief after antituberculous drug treatment; ③severe or progressive spinal nerve damage;④ imaging suggesting obvious epidural abscess, single segment lesion; ⑤severe bone destruction, spinal instability; ⑥patients with a follow-up time of at least 6 months and those with complete follow-up data.
Exclusion Criteria
①Patients with active tuberculosis (such as pulmonary tuberculosis, enteric tuberculosis, etc.); ②spinal diseases other than spinal tuberculosis, such as spinal intervertebral disc herniation, tumor, infection, fracture, etc.; ③lesions involving 2 or more segments; ④patients unable to tolerate the surgery.
Diagnostic Criteria for Spinal Tuberculosis
The patient had previous or existing tuberculosis of other sites, with clinical manifestations including low-grade fever, night sweats, weight loss, pain at the site of spinal lesion, and percussion pain. Preoperative imaging showed disc destruction, the presence of bone sequestrum, abscess, and compressive myelopathy. The laboratory inspection shows that CRP, ESR, tuberculin test, and other indicators are abnormal. Tuberculous granulation tissue or caseous necrosis were found in postoperative pathology.
Surgical Method
Preoperative Preparation
In both groups, a detailed medical history was taken and a physical examination was performed. Relevant X-rays (including thoracic or lumbar side, dynamic level, etc.), CT, MRI, and other auxiliary examinations were conducted to evaluate the patient’s systemic condition and limb function status. For hypertensive patients, blood pressure was controlled below 160/100mmHg. For diabetic patients, fasting blood glucose was controlled within 8 mmol/L, postprandial blood glucose within 10 mmol/L, and urinary glucose was controlled at + ~ + +. Drugs that may affect the study (eg, anticoagulant drugs) were suspended. Patients were instructed to rest to reduce the damage caused by spinal instability and ensure good nutrition before surgery. Chemotherapy regimen: After initial preoperative diagnosis of spinal tuberculosis, oral Isoniazid 0.3g/d, Rifampicin 0.45g/d, Ethambutol 0.75g/d, Pyrazinamide 0.75g/d were administered for at least 2–4 weeks. When the patient’s appetite improved, without low-grade fever or night sweats, protein levels improved, chest radiograph and sputum culture results were negative, and laboratory tests of CRP <20mm/h, ESR <50mm/h or both were significantly decreased, elective surgical treatment was considered. The condition and all risks were explained before surgery, and the consent form was signed.
Surgery Method
Posterior Pedicle Lesion Removal, Bone Grafting and Internal Fixation
After patient anesthesia, the prone position was taken. The patient’s abdomen was placed on a horseshoe pad, the surgical area was disinfected, and a sterile drape was applied. Cefuroxime sodium 2g was administered intravenously. A posterior median incision was made to separate the tissue layer by layer, expose the lesion, and completely remove it. The residual disc, nucleus pulposus, and endplate cartilage were scraped for full decompression. Screws were implanted, attachment rods were mounted, and intervertebral bone grafting was performed. The wound cavity was washed with a washing gun + 3L bag. Anti-tuberculosis drugs (streptomycin 1g + Isoniazid 300mg) and 2 drainage tubes were placed at the lesion, and the incision was closed layer by layer. Specific implant materials are shown in Table 1.
 |
Table 1 Material Characteristics of the Implant |
Endoscopic Spinal Tuberculosis Focus Removal
All patients in Group A underwent intervertebral graft removal. As an example, for patients with tuberculosis at the L3 and L4 levels, general anesthesia was administered through airway intubation, and they were positioned prone. The C-arm X-ray machine was utilized to determine the body surface projection of the lesion space. The right intervertebral foramen at the L3,4 disc level, located 9 cm from the spine’s midline, was selected as the needle injection point. The puncture needle was angled at 20–35 degrees relative to the trunk towards L4, facilitating the expansion of the soft tissue channel along the needle to the spinal canal. This process enabled the visualization and treatment of the lumbar tuberculosis focus, including spinal canal decompression, nerve root adhesion release, intervertebral disc radiofrequency ablation, and intervertebral space catheterization.Under microscopic guidance, turbid purulent secretions and caseous necrotic scar tissue were cleared. Dead bone was removed, and the lesions were thoroughly cleaned. Complete relief was provided to the front edge of the nerve and dural sac. After the lesion removal, a suitable autologous bone graft, typically harvested from the posterior end of the anterior superior iliac spine, was embedded between the vertebrae. Alternatively, the graft bed was treated with mixed rifampicin. The effectiveness of the bone graft fixation was verified by X-ray, ensuring satisfactory positioning. During the operation, the surgical field was continuously irrigated with an isoniazid diluent. Tissue samples from the lesion were collected for bacterial culture, drug sensitivity testing, and pathological examination. A 12 double-lumen tube was placed at the lesion’s center. After confirming the position through fluoroscopy, a subcutaneous tunnel was established, the tube secured with stitches, and the area bandaged. Specific implant materials are detailed in Table 2.
 |
Table 2 Complete Set of Surgical Instruments for Vertebroplasty |
Postoperative Management
① An intravenous infusion of antibiotics was administered for 24 hours postoperatively to prevent infection, along with nonsteroidal anti-inflammatory drugs to alleviate postoperative pain.② Drainage from the operative area was monitored and considered adequate if less than 30mL/24 hours.③ Patients were allowed to engage in ground activities wearing a waist brace 1–2 days after the surgery.④ Patients continued to take a regular oral chemotherapy regimen of Isoniazid 0.3g/d, Rifampicin 0.45g/d, Pyrazinamide 30mg/(kg·d), and Ethambutol 15 mg/(kg·d) for 9–12 months. Liver and kidney function were regularly monitored during this period.⑤ Before discharge, patients underwent X-ray and CT scans to evaluate the bone grafting and the position of the fixation device.⑥ MRI was performed before discharge to evaluate the decompression and lesion removal.⑦ Waist brace protection was continued for 3 months postoperatively.⑧ Liver and kidney function were regularly reviewed after discharge.
Postoperative Index Evaluation
Visual Analogue Scale (VAS)
The VAS was scored on the day of admission, on the fifth day after surgery, and at the last follow-up visit (within 1 year), and the results were compared. The patient’s analgesic regimen during the hospitalization was oral Paracetamol and Dihydrocodeine Tartrate Tablets. Scoring criteria: total score: 10; specific scoring details are shown in Figure 1. During the recording process, the patient indicated the pain on a graduated ruler, which was evaluated by the physician.
 |
Figure 1 The VAS scoring criteria for low-back pain. |
Oswestry Disability Index (ODI)
Composed of 10 questions, including the intensity of the pain, life care, content, walking, sitting, standing, sleep, sex, social life, tourism, 10 aspects, each six options, each question of the highest score of 5 points, choose the first option score 0 points, choose the last option score 5 points, if there are 10 questions do a question and answer. The scoring method is the actual score / 50 (highest possible score) 100%, if there is a question not answered, the scoring method is: the actual score / 45 (highest possible score) 100%, if the higher the dysfunction, the more serious.
Intraoperative Blood Loss
This was calculated by adding the weight of the postoperative gauze to the blood volume in the aspirator, then subtracting the volume of irrigation fluid. Intraoperative bleeding was considered significant if 30mL could completely wet the gauze (180mL), or if the content of the aspirator minus the amount of normal saline used for washing was significant.
Blood Transfusion Requirements
Blood transfusion was administered if the postoperative hemoglobin level was less than 70g/L, or if it was 70g/L with uncomfortable symptoms such as dizziness, pallor, and weakness. The hemoglobin level was reassessed 6 hours after transfusion, and further blood transfusion was considered using the same criteria.
Cobb Angle
The Cobb angle is the angle between the vertical line of the upper edge of the superior vertebra and the vertical line of the lower edge of the inferior vertebra. If the upper and lower edges of the vertebra are not clear, the connection between the upper and lower edge of the pedicle should be selected, and then the angle of the vertical line is the Cobb angle. The Cobb angle is one of the reference standards for the size of the scoliosis angle and the severity of scoliosis, as shown in Figure 2.Pre-operative and postoperative Cobb angle were included in this study.
 |
Figure 2 Cobb angle method for waist measurement. Notes: Apply the method of measuring Cobb angle on the X tablet. |
General Information
- Clinical data from 105 patients with thoracic and lumbar tuberculosis who underwent endoscopic spinal tuberculosis focus removal and posterior pedicle lesion removal, bone grafting, and internal fixation from January 2018 to December 2022 were collected for a retrospective study. Patients were divided into two groups based on the two different procedures: 1) posterior pedicle lesion removal, bone grafting, and internal fixation group (n=67), and 2) minimally invasive surgery group (n=38).
- The efficacy of posterior pedicle lesion removal, bone grafting, and internal fixation, and endoscopic spinal tuberculosis focus removal was statistically analyzed. General data of the two groups included patient gender, age, body mass index, affected segments, smoking history, and past history.
Observed Indicators
Primary Outcome Measures
Preoperative, 1 day postoperative, and final postoperative follow-up erythrocyte sedimentation rate, C-reactive protein, Procalcitonin, D-Dimer, Neutrophil to Lymphocyte ratio, preoperative hemoglobin and preoperative protein, preoperative, 1 day postoperative, 3 months postoperative, and final postoperative follow-up lumbar lumbago VAS score, ODI score, and spinal Cobb angle.
Secondary Outcome Measures
Operation time, intraoperative blood loss, postoperative drainage, postoperative time, postoperative complications (dural tear, lower limb intermuscular vein thrombosis, lower limb deep vein thrombosis, incision infection, cerebrospinal fluid leakage, internal loosening, skin margin necrosis, sinus formation, and total complication rate), blood transfusion rate, and blood transfusion volume, etc.
Statistical Methods
Data analysis was performed using the SPSS 26.0 statistical software. Quantitative data are described by the mean ± standard deviation (X ± S), and qualitative data are represented by the number of cases. Comparison of the quantitative data was performed using the independent samples t-test. For cases not eligible for t-test, rank sum test was used. Comparison of the qualitative data was performed using the χ 2 test. A P <of 0.05 was considered as statistically significant.
Data analysis was performed using the SPSS 26.0 statistical software. Quantitative data are described by the mean ± standard deviation (X ± S), and qualitative data are represented by the number of cases. Comparison of the quantitative data was performed using the independent samples t-test. For cases not eligible for t-test, rank sum test was used. Comparison of the qualitative data was performed using the χ 2 test. A P < 0.05 was considered statistically significant.
Results
Analysis of the Number of Participants
Included in the study were 105 patients with thoracolumbar tuberculosis who received both endoscopic spinal tuberculosis focus removal and posterior pedicle lesion removal, bone grafting, and internal fixation. Patients were divided into 2 groups according to the surgical method: 1) posterior pedicle lesion removal, bone grafting, and internal fixation group (n=67), and 2) minimally invasive surgery group (n=38). Data from 2 cases in Group A and 3 in Group B.
Experimental flow chart The flow chart of the two groupings is shown in Figure 3.
 |
Figure 3 Flow chart of test grouping. |
Comparison of Preoperative Data Between the Two Groups
In both groups, there were no statistically significant differences (P > 0.05) in age, gender, body mass index, segment involvement, past history (cardiovascular and cerebrovascular, respiratory system, endocrine system, metabolic diseases, and history of tuberculosis), smoking history, preoperative erythrocyte sedimentation rate, C-reactive protein, Procalcitonin, D-Dimer, Neutrophil to Lymphocyte ratio, hemoglobin, total protein, lumbar VAS score, lumbar ODI score, and spinal Cobb angle. Specific data are shown in Table 3.
 |
Table 3 Basic Preoperative Data of the Two Groups |
Postoperative VAS and ODI Scores in Both Groups
There was no significant difference in low back VAS scores and ODI scores between the two groups at 1 month and 3 months postoperatively (P>0.05). However, at the last follow-up, the low back VAS score in the minimally invasive surgery group was significantly lower than that in the posterior pedicle lesion removal, bone grafting, and internal fixation group (t=5.124, P<0.05). This suggests that the minimally invasive surgery group may have a better long-term prognosis.Specific data are shown in Table 4.
 |
Table 4 Postlumbar VAS and ODI Scores in Both Groups |
Comparison of Indexes at 1 Day and Last Follow-Up Test in the Two Groups
There was no significant difference in all the test indices included in this study between the two groups on the first day after surgery (P > 0.05). However, at the last postoperative follow-up, the minimally invasive surgery group had significantly higher hemoglobin and total protein levels than the posterior pedicle lesion removal, bone grafting, and internal fixation group (t=6.081/0.565, P < 0.05), as shown in Table 5. This indicates that the minimally invasive surgery group recovered hemoglobin and total protein levels more quickly.
 |
Table 5 Test Tested at 1 Day and Last Follow-Up in the Two Groups |
Analysis of the Postoperative Complications in the Two Groups
The postoperative incidence of dural laceration, calf muscle vein thrombosis, deep vein thrombosis, infections, cerebrospinal fluid leakage, internal fixation loosening, skin necrosis, and sinus formation were not significantly different (P > 0.05) in both groups. The rates of internal fixation loosening, skin necrosis, and sinus formation were also not significantly different (P > 0.05). However, the postoperative recurrence rate in the posterior pedicle lesion removal, bone grafting, and internal fixation group (10 cases) was significantly higher than that in the minimally invasive surgery group (1 case), with a significant difference (t=3.908, P=0.048) (see Table 6). These data suggest that endoscopic removal of spinal tuberculosis foci has superior therapeutic efficacy, while both groups demonstrated significant clinical outcomes.
 |
Table 6 Comparison of Postoperative Complications Between the Two Groups |
Comparison of Transfusion Rate and Volume of the Two Groups
In the posterior pedicle lesion removal, bone grafting, and internal fixation group, 23 patients received transfusions during the perioperative period, with a transfusion rate of 34.3% and a volume of 1.97±2.38 U. In the endoscopic spinal tuberculosis focus removal group, 11 patients were transfused, with a rate of 28.9% and a volume of 1.02±1.96 U. The transfusion volume in the endoscopic group was significantly lower than in the posterior pedicle lesion removal, bone grafting, and internal fixation group, with a statistically significant difference (X²=1.149, P<0.05) (see Table 7). However, the difference in transfusion rates between the two groups was not statistically significant (X²=2.007, P>0.05) (see Table 7).
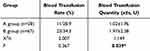 |
Table 7 Comparison of Transfusion Rates and Transfusion Volume Between Two Groups |
Operation Time, Intraoperative Blood Loss, Postoperative Drainage Rate, Postoperative Drainage Time and Cobb Angle Were Compared in Both Group
There was no significant difference between the two groups (P> 0.05). The operation time in Group B was 244.44 ± 48.92, compared to 216.18 ± 45.10 in Group A, with Group A having significantly less operation time (t=0.207, P<0.05). The intraoperative blood loss in Group B was 273.58 ± 149.49, compared to 214.47 ± 99.77 in Group A, with Group A having significantly less blood loss (t=8.950, P<0.05). The postoperative drainage time in Group B was 5.70 ± 2.41, compared to 3.47 ± 1.57 in Group A, with Group A having significantly less drainage time (t=2.996, P<0.05). The Cobb angle in Group B was 9.81 ± 1.66, compared to 8.88 ± 2.39 in Group A, with Group A having a significantly smaller Cobb angle (t=8.218, P<0.05) (see Table 8 and Figure 4). These data suggest that Group A has a better safety profile.
 |
Table 8 Comparison of Secondary Indicators Between the Two Patient Groups |
 |
Figure 4 Box plots of comparative secondary indicators in the two patient groups. Notes: (A); Operative time; (B) Intraoperative bleeding; (C) Post-operative downtime; (D); Cobb angle. |
Typical cases, see Figures 5–8.
Discussion
Summary of Evidence
Endoscopic removal of spinal tuberculosis foci is an emerging technique in the field of minimally invasive spinal surgery. Numerous studies have demonstrated its clinical efficacy in treating lumbar degenerative diseases.11–14 In recent years, the broad application of this technique in clinical practice has led to an expansion of its surgical indications, extending beyond lumbar degenerative diseases. Currently, some researchers have begun to employ this technique in treating spinal infectious diseases such as epidural abscess,15 purulent spondylitis,16 and spinal tuberculosis.17 Anti-tuberculosis drug chemotherapy remains the primary treatment method for thoracolumbar tuberculosis, often yielding positive results. The minimally invasive treatment methods for thoracolumbar tuberculosis mainly include CT-guided percutaneous catheter drainage, foraminal endoscopic lesion removal, percutaneous screw internal fixation technology, and channel-assisted small incision surgery.18,19 The foraminal endoscopic technique, characterized by minimal trauma, reduced intraoperative bleeding, and a clear surgical field, was initially applied in the removal of the nucleus pulposus of lumbar disc herniation. With its continued development, it has been utilized in the treatment of spinal tuberculosis.18,20–23
In 2017, Korean scholar Eun et al24 proposed using arthroscopy to provide vision in the observation channel, inserting minimally invasive discectomy instruments in the operating channel, and successfully applying it in the treatment of lumbar diseases. In recent years, endoscopic spinal tuberculosis focus removal has garnered the attention of spine physicians and has been widely used in spine-related diseases. This is because patients prefer minimally invasive surgery due to its reduced trauma, pain, and postoperative complications. According to data from Fu Shuanyu et al,20 the foraminal endoscopic technique was used to remove lesions in 12 cases of lumbar spinal tuberculosis. A large volume of streptomycin normal saline solution was used for washing, and calcium sulfate artificial bone was implanted into the intervertebral space. The stability of the spine was then reconstructed with percutaneous pedicle screw technology. This procedure can achieve the same curative effect as traditional open surgery, but it is more minimally invasive. The channel-assisted small incision technique uses the channel system to complete spinal canal decompression, discectomy, interbody graft fusion, and internal fixation under a limited surgical incision. Currently, this technique has been widely used in the treatment of lumbar degenerative diseases. Xue Haibin et al25 applied the channel small incision technique to treat 56 patients with lumbar tuberculosis. At the final follow-up, all lesions were cured, bone grafts were fused, lumbar curvature was improved, and there were no patients with internal fixation failure, essentially restoring the patients to their pre-disease life and work conditions. In addition, our results also showed that patients undergoing minimally invasive surgery experienced less trauma, shorter operation time, less intraoperative blood loss, lower postoperative recurrence rate, and lower postoperative drainage rate. Minimally invasive puncture and drainage combined with local chemotherapy can effectively improve blood sedimentation and lumbar function, restore the Cobb angle, and provide a better long-term prognosis. In 2021, Kim et al’s team26 successfully treated spinal tuberculosis with UBE debridement lesions and percutaneous screw instrumentation. Their study results confirmed that this technique is beneficial in diagnosing and treating spinal tuberculosis. A 2023 study by Wang Xiangbin’s team27 treated 9 patients with debridement, decompression, interbody fusion, and percutaneous screw fixation under UBE. All patients had no complications such as recurrence, incision infection, dural tear, and cerebrospinal fluid leakage during the follow-up period. Wang Xiangbin’s team28 used debridement, decompression, interbody fusion, and percutaneous screw fixation under UBE to treat 13 patients with Brucellosis spondylitis. The study data showed that all patients had no clinical symptoms, no local tenderness, and no percussion pain. Thirteen patients had a lordosis angle of 47.18 ± 6.88, and the lordosis angle was 42.26 ± 6.92, with a significant difference (P <0.05). Twelve patients reached grade I and one case reached grade II, with a fusion rate of 12/13. HSU et al29 used UBE inferior discectomy and debridement for Salmonella spondylitis with an epidural abscess, and the patient had good postoperative results. The above research results prove that percutaneous endoscopic spinal tuberculosis focus removal as an adjuvant treatment for thoracolumbar tuberculosis has a definite initial clinical efficacy. It is a safe, feasible, and effective method, providing a new direction for minimally invasive surgery in the treatment of spinal tuberculosis.
Implications for Future Research
This study is retrospective in nature. According to our analysis, there was no significant difference in safety between the two groups undergoing thoracolumbar tuberculosis surgery. However, significant differences were observed in operation time, surgical blood loss, postoperative time, spinal Cobb angle, blood transfusion, last follow-up lumbar VAS score, hemoglobin, and total protein. The case data of the patients included in the study is comprehensive, but the number of included studies is limited. Variations in surgical experience among different surgeons may influence the analysis results. Furthermore, the exploration of different surgical procedures for different segments of the spine could be a direction for future research. In recent years, with the continuous development of minimally invasive concepts, minimally invasive technology, which offers advantages such as less trauma, reduced intraoperative bleeding, quicker recovery, fewer complications, and shorter hospital stays, has been widely used in thoracolumbar surgery and has also been enriched and developed in the treatment of thoracolumbar tuberculosis. The disadvantages of minimally invasive surgery, including small correction angle, ease of losing angle, and surgical operation restrictions, have prevented its full popularization. Due to the shortage of blood inventory in the regional central blood stations, the development of some surgical procedures is limited, and many hospitals have not implemented related minimally invasive surgery. For the surgical treatment of thoracolumbar tuberculosis, standardized anti-tuberculosis drug treatment remains an important prerequisite. Anti-tuberculosis treatment 2–4 weeks before surgery is necessary, but the treatment duration should be adjusted according to the specific condition of the patient. Surgical treatment is an important auxiliary means, but the choice of surgical approach and method should be fully evaluated in the comprehensive situation of patients, and the surgeon should be adept at combining various methods to develop the optimal treatment plan.
Analysis of Article Results
A total of 1105 patients were included in this study to compare the parameters of the endoscopic spinal tuberculosis focus removal and the posterior pedicle lesion removal, bone grafting, and instrumentation. Endoscopic spinal tuberculosis focus removal Group 38 Case (Age 74.02 ± 6.31), posterior pedicle lesion removal, bone grafting, and and internal fixation Group 67 (age 70.02 ± 17.11).Main postoperative indicators revealed that Group A had significantly lower lumbar VAS scores, higher hemoglobin and total protein levels, and a lower recurrence rate than Group B at the last follow-up (P<0.05). Secondary postoperative indicators showed that Group A required significantly less blood transfusion, had shorter operative time, less intraoperative blood loss, shorter postoperative hospitalization time, and lower Cobb Angle than Group B (P<0.05).
Limitations of the Article
① As this study is retrospective, there may be data loss or unrecorded data, which could bias the results. However, the research team has meticulously recorded the postoperative outcome indicators to maintain the integrity of the experimental data to the greatest extent; ② The sample size included was relatively small, leading to insufficient statistical efficacy and potential reporting bias; ③ The evaluation indices are limited as they do not include treatment cost and postoperative hospital stay. The results of this study require further clarification through multicenter, prospective studies to elucidate the relationship between spinal tuberculosis surgery and clinical efficacy.
Conclusion
The results of this study demonstrate that minimally invasive puncture drainage combined with local chemotherapy treatment for spinal tuberculosis can achieve the same safety level as traditional posterior surgery. However, minimally invasive puncture drainage combined with local chemotherapy treatment for thoracolumbar tuberculosis results in less trauma, shorter operation time, less intraoperative bleeding, lower postoperative recurrence rate, and less postoperative drainage. Furthermore, this approach can effectively improve blood sedimentation, lumbar function, restore the Cobb angle, and reduce pain, making it worthy of promotion and application.
Abbreviations
ESR, Erythrocyte sedimentation Rate; CRP, C-reactive protein; PCT, Procalcitonin; ODI, Oswestry disability index; VAS, Visual analogue scale; DVT, deep venous thrombosis; CSF, Cerebrospinal fluid; TB, Tuberculosis.
Data Sharing Statement
Follow-up To explore and analyze the clinical efficacy of endoscopic spinal tuberculosis focus removal, posterior pedicle lesion removal, bone grafting and internal fixation combined with drug chemotherapy in the treatment of thoracolumbar tuberculosis, and to summarize the strategies for preventing complications and provide reference for clinical treatment. Because part of the data is incomplete, so the dataset analyzed in this study is not publicly available but is available to the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
We confirm that all experiments were performed in accordance with the Declaration of Helsinki. The study was approved by the Ethical Committee of the Sixth Affiliated Hospital of Xinjiang Medical University. Each patient provided written informed consent before participating in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yang Z, Liu C, Niu N, et al. Selection of the fusion and fixation range in the intervertebral surgery to correct thoracolumbar and lumbar tuberculosis: a retrospective clinical study. BMC Musculoskelet Disord. 2021;22(1):466. doi:10.1186/s12891-021-04335-0
2. Shi T, Zhang Z, Dai F, et al. Retrospective study of 967 patients with spinal tuberculosis. Orthopedics. 2016;39(5):e838–843. doi:10.3928/01477447-20160509-03
3. Chakaya J, Khan M, Ntoumi F, et al. Global tuberculosis report 2020 - reflections on the global tb burden, treatment and prevention efforts. Int J Infect Dis. 2021;113(Suppl 1):S7–s12. doi:10.1016/j.ijid.2021.02.107
4. Dong Z, Wang QQ, Yu SC, et al. Age-period-cohort analysis of pulmonary tuberculosis reported incidence, China, 2006–2020. Infect Dis Poverty. 2022;11(1):85. doi:10.1186/s40249-022-01009-4
5. Wang F, Wu HB, Yu ZJ, et al. The effect of percutaneous puncture and local chemotherapy combined with tuberculosis tuberculosis and its effect on immune function. Chin J Gerontol. 2022;42(10):2417–2421.
6. Chen L, Zhang J. Retrospective evaluation of short-course versus traditional preoperative chemotherapy in thoracolumbar spinal tuberculosis patients. Med Sci Monit. 2023;29:e941003. doi:10.12659/MSM.941003
7. Dunn RN, Ben Husien M. Spinal tuberculosis: review of current management. Bone Joint J. 2018;100-b(4):425–431. doi:10.1302/0301-620X.100B4.BJJ-2017-1040.R1
8. Ma S, Zhou Z, Wan Z, et al. Osteotomized debridement versus curetted debridement in posterior approach in treating thoracolumbar tuberculosis: a comparative study. Eur Spine J. 2022;31(2):473–481. doi:10.1007/s00586-021-07075-w
9. Zhang X, Wang KR, Gao X, et al. Endoscopic vertebral debridement and lavage drainage in the treatment of lumbar tuberculosis. Chin J Bone Joint. 2020;9(7):516–521.
10. Guan XL, Xue W, Wang D, et al. [Clinical application of percutaneous spinal endoscopy debridement and lavage in sacroiliac joint tuberculosis]. Zhongguo Gu Shang. 2021;34(11):1006–1010. Chinese. doi:10.12200/j.issn.1003-0034.2021.11.004
11. Wu H, Cui Y, Gong L, et al. Comparison between single anterior and single posterior approaches of debridement interbody fusion and fixation for the treatment of mono-segment lumbar spine tuberculosis. Arch Orthop Trauma Surg. 2022;142(12):3643–3649. doi:10.1007/s00402-021-03955-4
12. Zhang HQ, Li L, Xu JZ, et al. Chinese guidelines for surgical management of spinal tuberculosis (2022 edition). Orthop J China. 2022;30(17):1537–1548.
13. Kang T, Park SY, Lee SH, et al. Spinal epidural abscess successfully treated with biportal endoscopic spinal surgery. Medicine. 2019;98(50):e18231. doi:10.1097/MD.0000000000018231
14. Wang X, Long Y, Li Y, et al. Biportal endoscopic decompression, debridement, and interbody fusion, combined with percutaneous screw fixation for lumbar brucellosis spondylitis. Front Surg. 2023;9:1024510. doi:10.3389/fsurg.2022.1024510
15. Xing WQ, Wu JJ, Chang ZQ, et al. Endoscopic treatment of lumbar tuberculosis: a case report and literature review. Orthop J China. 2022;30(15):1391–1394.
16. Zhang X, Wang KR, Gao X, et al. A Clinical Study of the Treatment of Lumbar Tuberculosis with Vertebral Debridement and Lavage Drainage by Spinal endoscopy.Medical. University Of Chongqing; 2020.
17. Kalanjiyam GP, Dilip Chand Raja S, Rajasekaran S, et al. A prospective study comparing three different all-posterior surgical techniques in the management of thoracolumbar spinal tuberculosis. J Clin Orthop Trauma. 2022;34:102026. doi:10.1016/j.jcot.2022.102026
18. Lou YM, Zhu ZA, Huang QX, et al. Clinical observation of lumbar tuberculosis treated by lesion lavage and drainage at the upper edge of the pedicle. J Minim Invas Med. 2018;13(03):393–395.
19. Wang ZY, Zhang ZY, Sun RF, et al. Clinical value of CT guided percutaneous catheter drainage for lumbar spinal tuberculosis with major lumbar abscess. J Clin Med. 2016;3(33):6513–6514.
20. Fu SH, Qin K, Lu DH, et al. Lumbar spinal tuberculosis implanted with artificial bone with streptomycin sulfate and percutaneous pedicle screw under transforaminal endoscopy. Zhongguo Zuzhi Gongcheng Yanjiu. 2021;25(04):493–498.
21. Gao Y, Ou Y, Quan Z, et al. [Research progress of surgical treatment of thoracolumbar spinal tuberculosis]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2018;32(1):112–117. Chinese. doi:10.7507/1002-1892.201705124
22. Tang Y, Wu WJ, Yang S, et al. Surgical treatment of thoracolumbar spinal tuberculosis-a multicentre, retrospective, case-control study. J Orthop Surg Res. 2019;14(1):233. doi:10.1186/s13018-019-1252-4
23. Pang X, Shen X, Wu P, et al. Thoracolumbar spinal tuberculosis with psoas abscesses treated by one-stage posterior transforaminal lumbar debridement, interbody fusion, posterior instrumentation, and postural drainage. Arch Orthop Trauma Surg. 2013;133(6):765–772. doi:10.1007/s00402-013-1722-9
24. Eun SS, Eum JH, Lee SH, et al. Biportal endoscopic lumbar decompression for lumbar disk herniation and spinal canal stenosis: a technical note. J Neurol Surg a Cent Eur Neurosurg. 2017;78(4):390–396. doi:10.1055/s-0036-1592157
25. Xue HB, Luo XB, Sun F, et al. Analysis of clinical efficacy of posterior transforaminal debridement and interbody fusion with instrumentation via tubular retractor system for lumbar tuberculosis. Chin J Antituberculosis. 2021;43(05):457–462.
26. Kim SK, Alarj M, Yang H, et al. Biportal endoscopic debridement and percutaneous screw fixation technique for spinal tuberculosis: how I do it. Acta Neurochir. 2021;163(11):3021–3025. doi:10.1007/s00701-021-04820-4
27. Wang XB, Wang C. Preliminary application effect of unilateral biportal endoscopy technique combined with drug chemotherapy in thoracic and lumbar tuberculosis. Zhonghua Yi Xue Za Zhi. 2023;103(15):1148–1153. doi:10.3760/cma.j.cn112137-20221019-02180
28. Wang XB, Long YB, Wang C, et al. Application of unilateral biportal endoscopy technique in the treatment of lumbar brucellosis spondylitis. Chin Gen Pract. 2023;26(08):963–971.
29. Hsu TL, Yang CJ, Pao JL. Salmonella spondylodiscitis and epidural abscess successfully treated with unilateral biportal endoscopic discectomy and debridement: a rare case report. J Int Med Res. 2022;50(3):3000605221085405. doi:10.1177/03000605221085405
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




