Back to Journals » Patient Preference and Adherence » Volume 18
Resourcefulness Among Initial Ischemic Stroke Patients: A Longitudinal Study of 12 Months
Authors Guo L , Zauszniewski JA , Zhang G, Lei X, Zhang M, Wei M, Ma K , Yang C, Liu Y, Guo Y
Received 7 November 2023
Accepted for publication 26 February 2024
Published 5 March 2024 Volume 2024:18 Pages 565—577
DOI https://doi.org/10.2147/PPA.S448647
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Lina Guo,1 Jaclene A Zauszniewski,2 Gege Zhang,1 Xiaoyu Lei,1 Mengyu Zhang,1 Miao Wei,1 Keke Ma,1 Caixia Yang,1 Yanjin Liu,3 Yuanli Guo1
1Department of Neurology, National Advanced Stroke Center, the First Affiliated Hospital of Zhengzhou University, Zhengzhou, Henan, People’s Republic of China; 2Frances Payne Bolton School of Nursing, Case Western Reserve University, Cleveland, OH, USA; 3Department of Nursing, the First Affiliated Hospital of Zhengzhou University, Zhengzhou, Henan, 450052, People’s Republic of China
Correspondence: Yuanli Guo, Email [email protected]
Objective: To explore distinct longitudinal trajectories of resourcefulness among initial ischemic stroke patients from diagnosis to 12 months, and to identify whether sociodemographic factors, disease-related factors, self-efficacy, family function, and social support can predict patterns in the trajectories of resourcefulness.
Methods: A prospective longitudinal study was conducted. Initial ischemic stroke patients who met inclusion and exclusion criteria were followed up when still in hospital (Preparing for discharge, Baseline, T1), at 1 month (T2), at 3 months (T3), at 6 months (T4), at 9 months (T5) and 12 months (T6) (± 1 week) after discharge. General information, National Institute of Health Stroke Scale (NIHSS), Modified Rankin Scale (mRS), General Self-Efficacy Scale (GSES), General Family Functioning Subscale (FAD-GF), and Social Support Rate Scale (SSRS) were used in T1. The Resourcefulness Scale© was evaluated at 6 time points. Growth mixture modeling was used to identify trajectory patterns of resourcefulness. Logistic regression was used to identify predictors of resourcefulness trajectories.
Results: Three longitudinal trajectories of resourcefulness were identified and named as the high-stable class (38.9%, n=71), fluctuation class (41.2%, n=75), and low-stable class (19.9%, n=36), respectively. Dwelling areas (x2= 6.805, P= 0.009), education (x2= 44.865, P= 0.000), monthly income (x2= 13.063, P= 0.001), NIHSS scores (x2= 44.730, P= 0.000), mRS scores (x2= 51.788, P= 0.000), Hcy (x2= 9.345, P= 0.002), GSES (x2= 56.933, P= 0.000), FAD-GF (x2= 41.305, P= 0.000) and SSRS (x2=52.373, P= 0.000) were found to be statistically significant for distinguishing between different resourcefulness trajectory patterns. Lower education (OR=0.404), higher NIHSS(OR=6.672) scores, and higher mRS(OR=21.418) scores were found to be risk factors for lower resourcefulness, whereas higher education(OR=0.404), GSES(OR=0.276), FAD-GF(OR=0.344), and SSRS(OR=0.358) scores were identified as protective factors enhancing resourcefulness.
Conclusion: This study obtained three patterns of trajectories and identified their predictive factors in initial ischemic stroke. The findings will assist health care professionals in identifying subgroups of patients and when they may be at risk of low resourcefulness and provide timely targeted intervention to promote resourcefulness.
Keywords: initial ischemic stroke, resourcefulness, longitudinal study, social ecology theory, predictive factors, nursing care
Introduction
Stroke, a major chronic non-communicable disease, poses a serious threat to global public health due to its high incidence, mortality, recurrence, and disability rates, as well as its overall burden on society.1,2 Among its types, ischemic stroke is the most common, accounting for approximately 85% of all cases,3 further underscoring the significance of addressing this condition. As the second leading cause of death and the main cause of adult disability worldwide,4 stroke’s impact is expected to grow, with estimates indicating a substantial increase in cases in Europe (1.5 million added annually by 2025) and an even sharper rise in China (a 50% increase in the next two decades).5,6 In the United States, about 0.80 million people experience a stroke every year, resulting in significant long-term disability, and the fifth most common cause of death.7 Around 75% of stroke survivors will have different degrees of disability, including physical, communicative, cognitive, emotional disorders, and swallowing disorders.8 Surprisingly, approximately one-third of stroke survivors develop PSD within 5 years,9 impacting rehabilitation and quality of life, while increasing mortality and suicide risk.10 Therefore, early recognition and intervention for patients with PSD is of great clinical relevance.11
Excitingly, resourcefulness has been confirmed as a mediating variable between stress and depression, and it can prevent the occurrence and development of PSD.12 Resourcefulness refers to an individual’s cognitive behavior ability to complete daily activities independently (personal resourcefulness) and the ability to ask for help from others when they cannot complete them alone (social resourcefulness).13 Personal resourcefulness refers to the ability to remain independent in doing daily work, although in difficult circumstances, it also includes the use of self-help strategies to deal with adversity or challenges.14 Social resourcefulness refers to the ability to seek help from others, including professionals, family members, and friends, when one is unable to handle a problem by oneself.14 People with high levels of resourcefulness showed lower stress, less anxiety, and fewer depressive cognitions, and resourcefulness intervention is effective in individuals’ psychological and physical health.14,15
However, most of the published studies on resourcefulness have been cross-sectional surveys, lacking longitudinal follow-up studies, and these studies mostly analyzed the total score of resourcefulness, ignoring the differences in specific scores between individuals.12,16 Moreover, little is known about the trajectory patterns of resourcefulness among people after a first ischemic stroke. Trajectory refers to the stable and continuous psychological or behavioral state that individuals change over time in the process of disease, which represents the individual’s health status and intervention needs to a certain extent.17 Therefore, describing the trajectory patterns of resourcefulness can provide new ideas for targeted interventions and improve the allocation efficiency of medical resources in clinical practice. Growth mixed model (GMM) is a person-centered approach that can identify latent longitudinal classes of people with similar characteristics.18 Latent class growth model (LCGM) is a special form of GMM, GMM and LCGM can determine individual patterns of resourcefulness by identifying subgroups that follow similar trajectories over time.19 Identifying the predicting factors of the trajectory patterns of resourcefulness is of great significance in formulating further interventions.
The social-ecology model encompasses individual, family, and social levels across three tiers, stressing complex environmental influences.20,21 At the individual level, self-efficacy plays a crucial role in the social-ecology model, epitomizing the degree of confidence that individuals possess in regulating their behavior, motivation, and the dynamics of their social environment. So higher self-efficacy bolsters resourcefulness, thereby improving the use and mobilization of resources to achieve goals.22 At the family level, dynamics such as emotional support, communication, and affective responsiveness could be included. Studies indicate that supportive family environments can bolster an individual’s resourcefulness by providing emotional resources and practical assistance that facilitate adaptive responses to challenges.12 Social level variables may encompass community support, medical system, and societal attitudes towards disability or recovery.23 Research highlights that a strong social network and a robust medical system can create environments that foster resourcefulness by offering necessary aid and resources.24 Exploring the influencing factors of the trajectory patterns of resourcefulness from the perspective of the social-ecology model has important guiding significance for future intervention research. Additionally, resourcefulness was shown to be a significant factor in promoting positive health outcomes and reducing depressive symptoms among elderly individuals following a stroke.25 This study suggests that individuals who employ both personal and social resourcefulness skills tend to exhibit better adjustment and recovery post-stroke.
Therefore, this study puts forward the following hypotheses: (1) there are different trajectories patterns of resourcefulness among people after a first ischemic stroke over 12 months; and (2) under the guidance of the social-ecology model, the baseline factors can predict the trajectories patterns of resourcefulness. To test the hypotheses stated above, the purpose of this study was to identify the trajectory patterns of resourcefulness and explore the predictive factors among people after a first ischemic stroke over 12 months. The findings can provide a theoretical basis for the development of longitudinal resourcefulness training programs for stroke survivors and provide further strategies for improving their quality of life. This study aimed to identify patterns of resourcefulness trajectories over a 12-month period in individuals post-first ischemic stroke and to ascertain baseline factors predictive of these trajectory patterns.
Methods
Design and Setting
This was a prospective longitudinal study of first-time ischemic stroke patients followed up 12 months. All the data was from the First Affiliated Hospital of Zhengzhou University, one of the National Advanced Stroke Center of China, which treated around 9600 ischemic stroke patients annually, and about 2800 were first-time ischemic stroke patients (within 7 days after onset). Moreover, this National Advanced Stroke Center was a data collection subcenter of the China National Stroke Screening and Prevention Project (CNSSPP). It was responsible for following up at least 2000 stroke patients (follow-up 1, 3, 6, 9, and 12 months after discharge) every year and reporting the data through the information platform. To control for confounding factors, this study used GPower to calculate the necessary sample size and randomly selected it from the pool. This study followed the STROBE statement checklist.26
Participants
The inclusion criteria were: (1) over 18 years old, (2) clinically diagnosed first-time ischemic stroke by a qualified neurology physician, (3) stroke event within 14 days, (4) ability to communicate, (5) remained in hospital for at least 3 days due to their stroke. People were excluded if they: (1) score below 20 on the Mini-Mental State Examination (MMSE) which indicated the existence of cognitive impairment; (2) Score ≥4 on the Modified Rankin Scale (mRS), which demonstrated severe disability; (3) stroke recurrence or other existing major diseases that seriously affect physical function during the follow-up period; and (4) participation in other studies.
Sample size was calculated by GPower 3.1. Test family was “F-test” and Statistical test was “ANOVA: Repeated measures, within factors”. Type of power analysis was “A priori: Computer required sample size”. Other relevant indicators were Effect size f=0.25, α err prob=0.05, Power (1-β err prob)=0.95, Number of group=1, Number of measurements=6, Corr among rep measures=0 and Nonsphericity correction ε=0.2. Accordingly, the total number of sample size was 176. Considering the 10% loss of samples, the target 196 stroke patients were followed up in this study. Finally, 12 people were lost during follow-up. Therefore, 182 individuals completed three or more follow-ups and were included in the final analysis, providing a response rate of 93.81%.
Variables and Measurements
Individual Level Variables
Social-demographic information, such as age, gender, education, spouse, monthly income, dwelling areas, BMI, and history of smoking and alcohol were obtained using a self-administered questionnaire.
Disease-related characteristics, such as TOAST (Trial of ORG 10172 in Acute Stroke Treatment) type, thrombolysis/ectomy, homocysteine, and complications were obtained from the medical records. Stroke severity was also obtained from the medical records based on the National Institute of Health Stroke Scale (NIHSS)27 and Modified Rankin Scale (mRS),28 which are used widely in China to evaluate stroke severity.
General Self-Efficacy Scale (GSES) was used to assess an individual’s ability to control and dominate one’s actions with a confident attitude. GESE was originally developed by German health psychologists Jerusalem and Schwarzer and has been widely used in many countries.29 The scale had 10 items and a single dimension. Likert 4-level scoring method is adopted, from “not true at all” to “exactly true”, with a score of 1 to 4 points. The total score is obtained by adding the scores of each item, ranging from 1 to 40. The higher the score, the higher the self-efficacy. The Chinese version of GSES was first applied and verified by Zhang and Schwarzer30 in Hong Kong cultural background and proved to have good reliability and validity.
Family Level Variable
General Family Functioning Subscale (FAD-GF) is a 12-item General Functioning (GF) subscale of the McMaster Family Assessment Device (FAD).31 It was used to evaluate family function, including problem-solving, communication, familial roles division, affective responsiveness, and emotional involvement, reflecting the role of family interactions in patient recovery and well-being to recognize the dynamic interplay between survivors and their families. Using Likert 4-level scoring method, the scores from “strongly disagree” to “strongly agree” are 1 to 4, respectively. The higher the score, the better the family function. The scale has been translated into Chinese and applied to Chinese population with good reliability and validity.32
Social Level Variable
Social Support Rate Scale (SSRS) was used to assess social support level, and it was developed by Chinese scholars Xiao.33 It was a 10-item and three dimensions, including objective support, subjective support, and utilization of social support. Items 1–4 and 8–10 use a Likert 4-level scoring method that ranges from “cannot get support” to “get sufficient support” and are scored from 1 to 4. Item 5 counts the total score of five questions: A, B, C, D, and E, with a total score of 1–4 points for each question from “None” to “full support”. If items 6 and 7 were answered with “no source”, scored 0, if answered with “those from the following sources”, scored the number of the listed sources. The higher the total score, the better the social support. It has been proven to have good reliability and validity and has been widely used in many studies.34
Resourcefulness
Resourcefulness Scale (RS)© was used to assess the skills constituting resourcefulness and it was developed by Zauszniewski and translated into Chinese by Lai.13 It included 28 items and two subscales, namely personal resourcefulness and social resourcefulness. The RS uses a 6-point Likert scale from “extremely non-descriptive of one’s behavior” to “extremely descriptive;” scores range from 0 to 5 on each item. Total RS scores range from 0 to 140, with higher scores indicating better resourcefulness. This scale has shown good reliability and validity and has been used widely in the Chinese context.12
Ethics
This study was approved by the Ethical Committee of Zhengzhou University (No.2020-KY-459) and was conducted according to the principles outlined in the Declaration of Helsinki.35 All participants were informed about the study at the beginning of the survey and written informed consent was obtained from all of them. The principles of benefit, confidentiality, fairness, and no harm were followed throughout the study. Permission for use of all study measures not in the public domain was obtained.
Data Collection
This study was conducted from January 2020 to December 2021. The participants were followed up for 12 months and questionnaire surveys were conducted while they were still in the hospital (Preparing for discharge, Baseline, T1), at 1 month (T2), at 3 months (T3), at 6 months (T4), at 9 months (T5) and 12 months (T6) (±1 week) after discharge. When the participants had stable vital signs, baseline data (Individual level, family level, social level, and outcome variables) were collected after the introduction by nursing staff and informed consent was gained. The participant’s contact information and home address after discharge were also collected at T1 so that the investigators could contact the participants to conduct the follow-up surveys. The researcher used the special follow-up telephone of the stroke center or via WeChat to investigate T2-T6 time points of patients’ resourcefulness level (outcome variable) after discharge. Those who could not be contacted ≥ 3 times at a follow-up time point were regarded as lost to follow-up. Attrition was recorded for those who have lost to follow-up ≥ 3 times.
Data Analysis
SPSS version 21.0 (IBM Corporation, Armonk, NY, USA) and Mplus version 8.0 were used for data analysis. A descriptive analysis was conducted for each independent variable. The frequency and percentage of descriptive variables are presented in tables and figures. Averages and standard deviations are employed to characterize the central tendency and variability of the data. Logistic regression was undertaken to examine the predictive capacity of one or more independent variables of the dependent variable, elucidating the interrelations among the variables. GMM and LCGM were carried out by using Mplus. P<0.05 was defined as a statistically significant difference.
Trajectory patterns of resourcefulness are judged through unconditional LCGM and GMM. LCGM does not allow individual variation in the development track within the group, so the variance of growth factor is set to 0. The single-category model is set as the baseline model, the number of categories of the model is gradually increased, the fitting indicators of each model are compared, and then the best model is determined according to the actual clinical situation. Fitting indicators include the Akaike information criterion (AIC), Bayesian information criterion (BIC), Sample- size adjusted BIC (aBIC), Entropy, Lo-Mendell-Rubin adjusted likelihood ratio test (LMRT), and Bootstrapped likelihood ratio test (BLRT). AIC, BIC, and aBIC are mainly indicators used to evaluate the quality between different models, and the lower values indicate better model fit. Entropy is a measure of classification accuracy with higher values indicating better classification quality. The LMRT and BLRT are tests of significance between two models with k classes against k-1 classes; a significant p-value indicates that the k class is better.
Finally, univariable analysis (x2 test) and multivariable analysis (Logistic regression) were used to explore the predictive effect of baseline data on trajectory patterns of resourcefulness from the three levels of society, family, and individual.
Results
Characteristics of the Samples
Among the 182 participants, ages ranged from 23 to 87, and the mean value was 58.02 years (SD=11.65). The mean scores of GSES, FAD-GF, SSRS were 2.236 (SD=0.91), 28.29 (SD=8.37), and 28.38 (SD= 10.66), respectively. Total scores on RS ranged from 53 to 96, with a mean value of 76.31 years (SD=13.63). Scores on the NIHSS were from 0 to 20, with a median value of 3. The detailed socio-demographic and clinical characteristics of the sample are presented in Table 1.
 |
Table 1 Characteristics of the Sample (n=182) |
Trajectory Patterns of Resourcefulness
Taking the resourcefulness scores of the stroke survivors at 6-time points as observation variables, data from 182 subjects who met the inclusion criteria were included in the model. As shown in Table 2, when the extracted categories are increased from 1 to 3, AIC BIC and aBIC decreased and the entropy value gradually increased. LMRT and BLRT were statistically significant. When the four categories were increased to five categories, AIC and aBIC increased slightly, the BIC continued to decline, and the entropy value also decreased. The model showed no further improvement and the LMRT and BLRT values were not statistically significant. To determine the optimal model, the GMM was tested. When the extracted categories were increased from 1 to 3, the AIC, BIC, and ABIC decreased, and the entropy value gradually increased. The LMRT was not statistically significant, but the BLRT was statistically significant. When the four categories were increased to five categories, the AIC continued to decline, the BIC and aBIC increased slightly, and the entropy value also increased. The LMRT and BLRT were not statistically significant. The three categories of LCGM were finally determined based on the comprehensive statistical indicators and clinical practice.
 |
Table 2 Fit Indices of LCGM and GMM for Resourcefulness (n=182) |
Trajectory patterns of resourcefulness were classified into three latent classes, and the probabilities of three classes were class 1 (38.9%, n=71), class 2 (41.2%, n=75), and class 3 (19.9%, n=36). Three latent longitudinal classes were further labeled based on trajectory characteristics of resourcefulness and clinical symptom characteristics. As revealed in Figure 1, class 1 had a high level of resourcefulness,36,37 with the lowest score of resourcefulness in 3 months after discharge (T3) and the highest score in 12 months after discharge (T6). The average scores in this group ranged between 88.63 and 108.23 and were therefore labeled “ high-stable class”. The average scores of Class 2 were at a moderate level from 70.33 to 89.26,36,37 which gradually increased from hospitalization (T1) to 1 month after discharge (T2), gradually decreased from 1 month after discharge (T2) to 6 months after discharge (T4) and fluctuated increased from 6 months after discharge (T4) to 12 months after discharge (T6). Therefore, it was named “fluctuation class”. Class 3 reported a fair level of resourcefulness and the average scores were from 60.49 to 69.68 in 12 months,36,37 and it was therefore labeled the “low-stable class”.
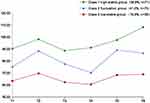 |
Figure 1 Trajectories patterns of resourcefulness of 12 months. |
Univariable Analysis of the Trajectories of Resourcefulness
According to different classes determined by LCGM, univariable analysis was used to identify possible predictors. Class 3 and class 2 were combined for the subsequent analyses because class 3 had a relatively small sample size, and the average scores of both classes reflected similar levels of resourcefulness defined by Zauszniewski et al.36 Additionally, combining these two classes might emphasize the resourcefulness patterns exhibited by the majority of patients at specific points in their disease progression or rehabilitation process, thereby allowing for a more focused interpretation of how resourcefulness fluctuates throughout different stages of patient care. The name of combined class 2 and class 3 was “Group 2-lower resourcefulness group”, and class 1 was considered as “Group 1-higher resourcefulness group”. Subsequent data are further analyzed based on this classification. Baseline data, including personal, family, and social three-dimensional variables, were included in the x2 test. The results showed that differences in dwelling areas (x2=6.805, p=0.009), education (x2=44.865, p=0.000), monthly income (x2=13.063, p=0.001), NIHSS scores (x2=44.730, p=0.000), mRS scores (x2=51.788, p=0.000), Hcy (x2=9.345, p=0.002), GSES (x2=56.933, p=0.000), FAD-GF (x2=41.305, p=0.000) and SSRS (x2=52.373, p=0.000) were statistically significant, and the other variables were not statistically significant as shown in Table 3.
 |
Table 3 Univariable Analysis of the Trajectories of Resourcefulness |
Multivariate Analysis of the Trajectories of Resourcefulness
As presented in Table 4, the logistic analysis indicated that education, NIHSS, mRS, GSES, FAD-GF, and SSRS were significant predictors, but dwelling areas, monthly income, and Hcy were not significant. Higher education (OR=0.404), higher scores on the GSES (OR=0.276), FAD-GF (OR=0.344), and SSRS (OR=0.358) were predictive factors of higher resourcefulness. Higher scores on the NIHSS (OR=6.672) and mRS (OR=21.418) were predictive factors of lower resourcefulness. Individuals who had higher NIHSS scores and mRS scores were 6.672 and 21.418 times more likely to report lower levels of resourcefulness compared with group 1 (higher resourcefulness) than those who did not, respectively.
 |
Table 4 Predicting Three Trajectory Patterns of Resourcefulness |
Discussion
This is the first reported longitudinal study to use LCGM with people who had first-time ischemic stroke and to identify different trajectory patterns of resourcefulness and their predictive factors. The findings have shown the applicability of this approach for current and future nursing research. LCGM /GMM has been extensively applied in statistical analysis for several decades, proving to be powerful tools in exploring latent longitudinal classes using individuals’ self-reports of resourcefulness and automatically identifying and marking different patterns of trajectories. It has the potential to assist health care professionals in identifying who and when a person may be at high risk for demonstrating fewer resourcefulness skills. The approach is also highly valuable for clinical nursing practice, as it provides a clear focus for healthcare providers to begin to develop targeted interventions designed to promote and sustain high levels of resourcefulness for specific subgroups at different time points, which can ultimately reduce their risk of depression.
Three trajectory patterns of resourcefulness were found, namely Class 1(high-stable class), Class 2 (fluctuation class), and Class 3 (low-stable class), and they were consistent with previous studies,36,37 where the range of RS cut scores indicated very low to very high need to learn resourcefulness skills. The total scores of resourcefulness within the three trajectory patterns were relatively low during hospitalization and then gradually increased until one month after discharge. This shows that through systematic treatment and health education during hospitalization, all patients may gradually reach the state of adaptation. This is consistent with Selye’s stress and adaptation theory, that is, after the stressor acts on the individual, the individual will produce a series of physical and mental reactions to adapt to the stressor to maintain the individual’s homeostasis.38 The total score of resourcefulness in the three longitudinal classes began to decrease from 1 month after discharge, class 1 fell to the lowest at 3 months after discharge, and then gradually increased, class 2 and class 3 fell to the lowest at 6 months, and then fluctuated increased. The possible reason was that with disease progression, financial burden, fear of recurrence, and caregivers’ exhaustion, the patient’s stress level began to rise again.39 The study showed that the cumulative recurrence rates of stroke patients were 7.7% in 3 months, 9.5% in 6 months and 22.9% in 1 year.40 This suggests that health practitioners should provide relevant interventions at least 1 month after discharge to promote the increase in resourcefulness and continue to do interventions at 3, 6, 9, and 12 months after discharge to promote the improvement and stability of resourcefulness.
The logistic regression analysis of the predictors of the trajectory patterns of resourcefulness demonstrated that people with higher education were more likely to be more resourceful. This finding is similar to one previous study that showed people who had higher education were usually more skilled and self-disciplined in maintaining and promoting health behaviors and finally reaching a good adaptive state.41 People who had higher scores on the NIHSS and mRS were more likely to have lower resourcefulness. Simultaneously, Zhao et al42 pointed out that reducing the degree of disability of patients with acute ischemic stroke and carrying out active functional recovery training play a positive role in promoting resilience and activity of daily living. Most importantly, the findings also explained that people with high scores of self-efficacy, family function, and social support had greater resourcefulness. Hohl and his team43 reported that individuals with high self-efficacy have personal resources to cultivate their ability to choose and build an environment that promotes successful adaptation and therefore may have a stronger motivation for self-help and help-seeking. A relevant study also showed that better family function could enhance people’s self-confidence and ability to deal with difficulties and conflicts.44 One study found that social support may be the most useful therapy and it enables individuals to actively seek external help and use available resources to promote the adoption of positive coping strategies.45 In addition, it can also provide emotional incentives for individuals and increase or maintain their self-worth.46
This study explores the factors influencing the ability to acquire resources across three levels of the socio-ecological model: individual, family, and society. The findings indicate that individuals with higher education levels have a greater capacity to acquire resources, whereas higher NIHSS and mRS scores are associated with a lower capacity. At the family level, strong family functioning supports individuals in dealing with challenges. In society, robust social support provides individuals with additional resources and encourages the adoption of coping strategies. In particular, although homocysteine was not shown to be a meaningful predictor in regression analysis, a prospective study47 found that elevated homocysteine levels were independently positively associated with depression or vascular dementia in women with mild acute ischemic stroke or TIA. Thus, future research should examine homocysteine levels as biochemical biomarkers for indicating a risk for low resourcefulness.
There are some limitations in this study: first, considering that the physical dysfunction of participants may affect their activities of daily living, and thus limit their capacity for self-help and help-seeking, patients with mRS ≥ 4 were not included in this study. However, such patients suffer from great physical and mental stress due to limited activities of daily living and therefore need special consideration in future research. Second, due to the limitations of objective conditions (research time and investigator resources), the total sample size included in this study is small, resulting even smaller sample size for each longitudinal trajectory class. In the x2 test and regression analysis, class 2 and class 3 were combined, which may have reduced the statistical power and had an impact on the results. Large-sample multicenter research should be pursued in future research. Third, the follow-up time of this study is 12 months. However, stroke is a chronic disease, which needs continuous follow-up and dynamic intervention.
Conclusion
This study employed LCGM and GMM to identify and explore trajectory patterns of resourcefulness over a 12-month period following a first-time ischemic stroke, classifying the participants into three significant trajectory patterns, and identifying their predictive factors in initial ischemic stroke. The high-stable group maintained a consistent level of resourcefulness; the fluctuation class demonstrated variable resourcefulness across time points; and the low-stable class persistently reported lower levels of resourcefulness throughout the study. Findings suggest that systematic treatment and health education provided during hospitalization positively impact resourcefulness initially, in line with Selye’s stress and adaptation theory. However, this study also identified critical time points post-discharge—specifically, one month, three months, and six months—where resourcefulness tends to decline and interventions may be most beneficial. This study highlights the need for targeted interventions to support stroke survivors, particularly after discharge when they are vulnerable to decreases in resourcefulness. Interventions should be tailored to improve self-efficacy, strengthen family function, and enhance social support which are critical factors for resourcefulness.
In conclusion, this study sheds light on the dynamic nature of resourcefulness post-stroke and underscores the importance of personal, familial, and social factors as predictors of these trajectories. These insights can inform healthcare professionals in delivering continuous and customized care to stroke survivors, fostering their adaptive capacity, and potentially mitigating the risk of subsequent adverse psychological outcomes such as depression, has great clinical significance for the health promotion of health and well-being in individuals with ischemic stroke patients. Future research should aim to expand the sample size, including participants with a broader range of disabilities, investigate additional predictors like biochemical markers, and extend the follow-up period to characterize the long-term trajectories of resourcefulness post-stroke more fully.
Data Sharing Statement
The data used to support the findings of this study are available from the first author (Lina Guo, [email protected]) and the corresponding author (Yuanli Guo, email address: [email protected]).
Acknowledgments
We express our gratitude to all the respondents.
Author Contributions
All authors made a significant contribution to the work conception, study design, acquisition, analysis and interpretation of data, taking part in drafting, revising or critically reviewing the article. All authors also gave final approval of the version to be published and have agreed on the journal to which the article has been submitted and to be accountable for all aspects of the work.
Funding
This study was funded by the National Natural Science Foundation of China (72204225, 72274179); China Postdoctoral Science Foundation (2023M733234); Medical Science and Technology Project of Henan Province (SBGJ202102076, 222102310246, LHGJ20220429); Nursing Science Foundation of the First Affiliated Hospital of Zhengzhou University (HLKY2023001).
Disclosure
The authors stated that they have no conflicts of interest in this work.
References
1. Liu F, Huang K, Lu X. Lifetime risk of stroke in the global burden of disease study. N Engl J Med. 2019;380:1377. doi:10.1056/NEJMc1900607
2. Chao BH, Yan F, Hua Y, et al. Stroke prevention and control system in China: csppc-stroke program. Int J Stroke. 2021;16:265–272. doi:10.1177/1747493020922513
3. Ding Q, Liu S, Yao Y, Liu H, Cai T, Han L. Global, regional, and national burden of ischemic stroke, 1990–2019. Neurology. 2022;98:e279–e290. doi:10.1212/WNL.0000000000013115
4. Feigin VL, Stark BA, Johnson CO, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. 2021;20:795–820. doi:10.1016/S1474-4422(21)00252-0
5. Wafa HA, Wolfe C, Emmett E, Roth GA, Johnson CO, Wang Y. Burden of stroke in Europe: thirty-year projections of incidence, prevalence, deaths, and disability-adjusted life years. Stroke. 2020;51:2418–2427. doi:10.1161/STROKEAHA.120.029606
6. Kim AS, Johnston SC. Temporal and geographic trends in the global stroke epidemic. Stroke. 2013;44:S123–S125. doi:10.1161/STROKEAHA.111.000067
7. Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics-2022 update: a report from the American heart association. Circulation. 2022;145:e153–e639. doi:10.1161/CIR.0000000000001052
8. Chen Z, Jiang B, Ru X, et al. Mortality of stroke and its subtypes in China: results from a nationwide population-based survey. Neuroepidemiology. 2017;48:95–102. doi:10.1159/000477494
9. Robinson RG, Jorge RE. Post-stroke depression: a review. Am J Psychiatry. 2016;173:221–231. doi:10.1176/appi.ajp.2015.15030363
10. Medeiros GC, Roy D, Kontos N, Beach SR. Post-stroke depression: a 2020 updated review. Gen Hosp Psychiatry. 2020;66:70–80. doi:10.1016/j.genhosppsych
11. Liu F, Song M, Huang X, Yi H, Chen H, Tian F. Symptomatic plaque enhancement is associated with early-onset post-stroke depression. J Affect Disord. 2022;306:281–287. doi:10.1016/j.jad.2022.03.026
12. Guo L, Zauszniewski JA, Liu Y, Yv S, Zhu Y. Is resourcefulness as a mediator between perceived stress and depression among old Chinese stroke patients? J Affect Disord. 2019;253:44–50. doi:10.1016/j.jad.2019.04.083
13. Zauszniewski JA, Lai CY, Tithiphontumrong S. Development and testing of the resourcefulness scale for older adults. J Nurs Meas. 2006;14:57–68. doi:10.1891/jnum.14.1.57
14. Zauszniewski JA. Resourcefulness. West J Nurs Res. 2016;38:1551–1553. doi:10.1177/0193945916665079
15. Toly VB, Zauszniewski JA, Yu J, Sattar A, Rusincovitch B, Musil CM. Resourcefulness intervention efficacy for parent caregivers of technology-dependent children: a randomized trial. West J Nurs Res. 2022;44:296–306. doi:10.1177/01939459211062950
16. Zauszniewski JA, Burant CJ. Resourcefulness as a mediator of the effects of dementia symptoms and caregiver reactions on caregiver mental health. Issues Ment Health Nurs. 2020;41:486–493. doi:10.1080/01612840.2019.1693670
17. Burton CR. Re-thinking stroke rehabilitation: the Corbin and Strauss chronic illness trajectory framework. J Adv Nurs. 2000;32:595–602. doi:10.1046/j.1365-2648.2000.01517.x
18. Saloner R, Lobo JD, Paolillo EW, et al. Identification of youthful neurocognitive trajectories in adults aging with HIV: a latent growth mixture model. AIDS Behav. 2022;26:1966–1979. doi:10.1007/s10461-021-03546-9
19. Kinouchi K, Ohashi K. Assessing engagement with patient-generated health data recording and its impact on health behavior changes in multicomponent interventions: supplementary analysis. JMIR Form Res. 2022;6:e35471. doi:10.2196/35471
20. Cho D, Nguyen NT, Strong LL, et al. Multiple health behaviors engagement in an African American cohort: clustering patterns and correlates. Health Educ Behav. 2019;46:506–516. doi:10.1177/1090198119826207
21. Harris WG, Gonzalez-Guarda R, Yang Q, Shah S, Prvu BJ. Socio-ecological perspective on factors influencing acute recovery of younger stroke survivors: a mixed methods study. J Adv Nurs. 2021;77:2860–2874. doi:10.1111/jan.14778
22. Jeddi H, Aghebati N, Ghavami V, Rezaeitalab F. The effect of self-care nurturance using the theory of modeling and role-modeling on self-efficacy in stroke patients: a randomized controlled trial. Holist Nurs Pract. 2023;37:E24–E35. doi:10.1097/HNP.0000000000000567
23. Ioannou E, Humphreys H, Homer C, Purvis A. Beyond the individual: socio-ecological factors impacting activity after gestational diabetes mellitus. Diabet Med. 2024;e15286. doi:10.1111/dme.15286
24. Bekhet AK, Zauszniewski JA. Resourcefulness, positive cognitions, relocation controllability and relocation adjustment among older people: a cross-sectional study of cultural differences. Int J Older People Nurs. 2013;8:244–252. doi:10.1111/j.1748-3743.2012.00341.x
25. Zhu Y, Xu H, Ding D, et al. Resourcefulness as a mediator in the relationship between self-perceived burden and depression among the young and middle-aged stroke patients: a cross-sectional study. Heliyon. 2023;9:e18908. doi:10.1016/j.heliyon.2023.e18908
26. von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (strobe) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–808. doi:10.1136/bmj.39335.541782.AD
27. Cheung RT, Lyden PD, Tsoi TH, et al. Production and validation of putonghua- and Cantonese-Chinese language national institutes of health stroke scale training and certification videos. Int J Stroke. 2010;5:74–79. doi:10.1111/j.1747-4949.2010.00411.x
28. Liu X, Zhou M, Zhao J, et al. Functional Independence and disability evaluation in stroke patients: optimal cutoff scores for a pictorial-based longshi scale, Barthel index, and modified rankin scale. Front Neurol. 2022;13:710852. doi:10.3389/fneur.2022.710852
29. Schwarzer R. Self-Efficacy: Thought Control of Action. Washington: Hemisphere Pub. Corp.; 1992.
30. Zhang JX, Schwarzer R. Measuring optimistic self-beliefs: a Chinese adaptation of the general self-efficacy scale. Psychologia. 1995;38:174–181.
31. Byles J, Byrne C, Boyle MH, Offord DR. Ontario child health study: reliability and validity of the general functioning subscale of the McMaster family assessment device. Fam Process. 1988;27:97–104. doi:10.1111/j.1545-5300.1988.00097.x
32. Yuan H, Zhang R, University S. Applicability of the general functioning scale of the family in China. China J Health Psychol. 2019;2019:1.
33. Dou W, Yu X, Fang H, et al. Family and psychosocial functioning in bipolar disorder: the mediating effects of social support, resilience and suicidal ideation. Front Psychol. 2021;12:807546. doi:10.3389/fpsyg.2021.807546
34. Wang L, Luo J, Li Y, Zhou Y, Wang W. Social support, anxiety, and depression in patients with prostate cancer: complete mediation of self-efficacy. Support Care Cancer. 2022;30:6851–6856. doi:10.1007/s00520-022-07065-8
35. World Medical Association. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–2194. doi:10.1001/jama.2013.281053
36. Zauszniewski JA, Lekhak N, Yolpant W, Morris DL. Need for resourcefulness training for women caregivers of elders with dementia. Issues Ment Health Nurs. 2015;36:1007–1012. doi:10.3109/01612840.2015.1075236
37. Zauszniewski JA, Au TY, Musil CM. Resourcefulness training for grandmothers raising grandchildren: is there a need? Issues Ment Health Nurs. 2012;33:680–686. doi:10.3109/01612840.2012.684424
38. Selye H. Stress and the general adaptation syndrome. Br Med J. 1950;1:1383–1392. doi:10.1136/bmj.1.4667.1383
39. Guo LN, Liu YJ, McCallum J, et al. Perceived stress and depression amongst older stroke patients: sense of coherence as a mediator? Arch Gerontol Geriatr. 2018;79:164–170. doi:10.1016/j.archger.2018.08.010
40. Lin B, Zhang Z, Mei Y, et al. Cumulative risk of stroke recurrence over the last 10 years: a systematic review and meta-analysis. Neurol Sci. 2021;42:61–71. doi:10.1007/s10072-020-04797-5
41. Guo L, Liu Y, Zhu Y, Wei M. Identification of health behaviour clusters among people at high risk of stroke: a latent class profile analysis. J Adv Nurs. 2020;76:3039–3047. doi:10.1111/jan.14523
42. Zhao L, Sun Q, Guo Y, Yan R, Lv Y. Mediation effect of perceived social support and resilience between physical disability and depression in acute stroke patients in China: a cross-sectional survey. J Affect Disord. 2022;308:155–159. doi:10.1016/j.jad.2022.04.034
43. Hohl DH, Schultze M, Keller J, Heuse S, Luszczynska A, Knoll N. Inter-relations between partner-provided support and self-efficacy: a dyadic longitudinal analysis. Appl Psychol Health Well Being. 2019;11:522–542. doi:10.1111/aphw.12166
44. Mei YX, Xiang DD, Zhang ZX, Twumwaah BJ, Lin BL, Chen SY. Family function, self-efficacy, care hours per day, closeness and benefit finding among stroke caregivers in China: a moderated mediation model. J Clin Nurs. 2022;32:506–516. doi:10.1111/jocn.16290
45. Liu Q, Jin Y, Wang Y, et al. Association between self-efficacy and self-management behaviours among individuals at high risk for stroke: social support acting as a mediator. J Clin Nurs. 2022;32:71–82. doi:10.1111/jocn.16191
46. Lin S, Wang C, Wang Q, et al. The experience of stroke survivors and caregivers during hospital-to-home transitional care: a qualitative longitudinal study. Int J Nurs Stud. 2022;130:104213. doi:10.1016/j.ijnurstu.2022.104213
47. Li R, Weng H, Pan Y, et al. Relationship between homocysteine levels and post-stroke cognitive impairment in female and male population: from a prospective multicenter study. J Transl Int Med. 2021;9:264–272. doi:10.2478/jtim-2021-0035
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
