Back to Journals » Journal of Asthma and Allergy » Volume 17
Real-World Safety and Effectiveness of Benralizumab in Japanese Patients with Severe Asthma: A Multicenter Prospective Observational Study
Authors Yamaguchi M , Nishimura Y, Takumi Y, Hayashi N , Sakamoto K, Tohda Y
Received 27 July 2023
Accepted for publication 19 December 2023
Published 20 January 2024 Volume 2024:17 Pages 45—60
DOI https://doi.org/10.2147/JAA.S432695
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Luis Garcia-Marcos
Masao Yamaguchi,1 Yoshihiro Nishimura,2 Yuko Takumi,3 Nobuya Hayashi,4 Kei Sakamoto,3 Yuji Tohda5
1Division of Respiratory Medicine, Third Department of Medicine, Teikyo University Chiba Medical Center, Ichihara, Chiba, Japan; 2Kita-Harima Medical Center, Ono, Hyogo, Japan; 3Patient Safety Division, Research and Development, AstraZeneca K.K., Osaka, Japan; 4Data Science and Innovation Division, Research and Development, AstraZeneca K.K., Osaka, Japan; 5Department of Respiratory Medicine and Allergology, Kindai University School of Medicine, Osaka-Sayama, Osaka, Japan
Correspondence: Masao Yamaguchi, Division of Respiratory Medicine, Third Department of Medicine, Teikyo University Chiba Medical Center, Ichihara, Chiba, Japan, Tel +81-436-62-1211, Fax +81-436-62-7340, Email [email protected]
Introduction: This study aimed to demonstrate whether benralizumab maintained the safety and effectiveness profiles established in randomized controlled trials among all patients with severe uncontrolled asthma initially prescribed benralizumab in the real-world setting in Japan.
Methods: This was a prospective, observational, multicenter post-marketing study (ClinicalTrial.gov, NCT03588546). The safety and tolerability of benralizumab over 1 year were assessed by the incidence of adverse events (AEs), serious AEs, adverse drug reactions (ADRs), and serious ADRs. Patient background characteristics indicating a more frequent onset of ADRs with benralizumab were explored. The main effectiveness assessment was the change in Asthma Control Questionnaire-5 (ACQ-5) score from baseline. Patients with baseline ACQ-5 scores ≥ 1.5 were defined as having severe uncontrolled asthma.
Results: In total, 632 patients were evaluated for safety and 274 for effectiveness; 139 patients were included in the severe uncontrolled asthma subgroup. ADRs were reported in 12.7% and serious AEs in 13.0% of patients. Serious infections occurred in 3.8%, serious hypersensitivity in 0.3%, and malignancy in 0.3% of patients. No helminthic infections occurred. In the effectiveness population, benralizumab improved the mean (standard deviation [95% confidence interval]) ACQ-5 score by − 1.16 (1.40 [− 1.36, − 0.96]) from baseline; forced expiratory volume in 1 second by 0.151 (0.440 [0.09, 0.21]) L; and Mini-Asthma Quality of Life questionnaire score by 1.16 (1.29 [0.94, 1.38]) at the last observation. The annual asthma exacerbation rate was 0.42. A greater ACQ-5 score improvement was observed among patients with eosinophilic asthma characteristics.
Conclusion: No new safety concerns were raised, and patients experienced benefits consistent with previous studies of benralizumab, thus supporting the use of benralizumab for the add-on maintenance treatment of patients with eosinophilic severe uncontrolled asthma.
Keywords: benralizumab, severe uncontrolled asthma, anti-interleukin-5 receptor α monoclonal antibody, eosinophils, exacerbation, asthma control, quality of life
Introduction
In 2019, it was estimated that over 260 million people globally were affected by asthma.1 Of the total population with asthma, approximately 3%–10% of patients have severe disease and have symptoms and exacerbations despite treatment with maximal standard-of-care controller therapy.2 The recent KEIFU study, a non-interventional insurance claims database analysis in Japan, reported that 7.8% of continuously treated asthma patients had severe asthma, of whom 2.5% had severe uncontrolled asthma.3 Patients with severe asthma have a disproportionately high disease burden, reflected by the marked impairment in quality of life and the increased healthcare and societal costs.4,5 This is also the case in Japan, as reported in a recent analysis of asthma-associated healthcare resource utilization using data from the Japan Medical Data Center database.6 The analysis showed that healthcare resource utilization was heavily concentrated among severe asthma patients, with significantly more all-cause hospitalizations, outpatient visits, prescriptions, and total medical costs than those with non-severe asthma.6 Eosinophilic asthma is the most common subtype of severe asthma, accounting for over 80% of cases.7 An increased number of airway and circulating eosinophils is associated with an increased frequency of asthma exacerbations, a high symptom burden, and impaired lung function.8–10
Benralizumab (Fasenra®) is a humanized, afucosylated, anti-interleukin (IL) 5 receptor α monoclonal antibody that induces direct, rapid, and nearly complete depletion of eosinophils11 via enhanced antibody-dependent cell-mediated cytotoxicity, the process by which natural killer cells cause eosinophil apoptosis.12 In 2018, benralizumab was approved in Japan as add-on maintenance therapy for adults with severe asthma whose asthma cannot be controlled with high-dose inhaled corticosteroids (ICS) plus additional controllers. Three Phase 3 randomized controlled trials (RCTs) have assessed the clinical efficacy of benralizumab in patients with severe uncontrolled eosinophilic asthma: CALIMA11 and SIROCCO13 both demonstrated significant reductions in exacerbations as well as improvements in lung function, asthma control, and quality-of-life measures, whereas ZONDA demonstrated a considerable reduction in maintenance oral corticosteroid (mOCS) dose.14
Individuals with specific vulnerabilities tend to be excluded from RCTs because of stringent eligibility criteria; however, such individuals may be prescribed the tested and approved drugs in daily clinical practice despite such vulnerabilities and without adequate evidence or appropriate treatment decision information.15 This post-marketing study aimed to demonstrate whether benralizumab maintained the safety and effectiveness profiles established in RCTs among all patients with severe uncontrolled asthma initially prescribed benralizumab per the approved indication in the real-world setting in Japan. Furthermore, the patient background characteristics that may indicate a more frequent onset of adverse drug reactions (ADRs), as well as those that can act as indicators of a good response to benralizumab, were explored.
Materials and Methods
Study Design, Ethics, and Population
This prospective, observational, multicenter post-marketing study (ClinicalTrial.gov, NCT03588546) was conducted between May 2018 and Nov 2021 at 195 sites across Japan. The study included a 1-year observational period and a 2-year follow-up period. This study was planned under the benralizumab Risk Management Plan (RMP) and was conducted under local regulations according to the Japanese Good Post-Marketing Study Practice (GPSP) ordinance in Japan and in compliance with the Declaration of Helsinki. In Japan, the assignment of medical intervention was at the discretion of the investigator. That is, benralizumab was prescribed to patients at the investigator’s discretion. Although the Japan Ministry of Health, Labour and Welfare stipulates that ethical review and informed consent are required for interventional clinical trials, research carried out pursuant to the provisions of laws and ordinances, including post-marketing surveillance under the jurisdiction of the Pharmaceuticals and Medical Devices Agency (PMDA), is exempt from these requirements, as described in the Ethical Guidelines for Medical and Health Research Involving Human Subjects. Therefore, the requirement of approval from the ethics committee and written informed consent from patients are waived for this purely observational study.
Eligible patients were those diagnosed with severe asthma who had been prescribed benralizumab for severe asthma for the first time in Japan (ie, limited to refractory patients whose asthmatic symptoms cannot be controlled by currently available treatment consisting of high-dose ICS plus additional controllers). Patients with baseline Asthma Control Questionnaire-5 (ACQ-5) scores ≥1.5 were defined as having severe uncontrolled asthma. Patients were enrolled from contracted hospitals by a central registration method until a number of patients up to or beyond the target number had been met. The approved benralizumab dose is 30 mg every 4 weeks via subcutaneous injection for the first three doses and then 30 mg every 8 weeks subcutaneously thereafter.16
Safety and Effectiveness Assessments
The safety and tolerability of benralizumab over 1 year was assessed based on the following endpoints: incidence of adverse events (AEs), serious AEs, ADRs, and serious ADRs. Investigators assessed AEs and ADRs. An AE was defined as any undesirable or unintended signs, symptoms, and disease regardless of the causality with the administration of benralizumab. ADRs were defined as any AE causally related to benralizumab or for which a causal relationship with benralizumab was unknown due to insufficient or contradictory information. Safety specifications in the Japanese RMP were AEs of serious hypersensitivities, serious infections, helminth infections, and malignancies in this study. Furthermore, the frequency of ADRs was classified by baseline characteristics.
The main effectiveness assessment was the change in ACQ-5 score from baseline. Other effectiveness assessments were change in spirometry parameters from baseline (forced expiratory volume in 1 second [FEV1]); Mini-Asthma Quality of Life questionnaire (MiniAQLQ) score; asthma exacerbation frequency; change in mOCS dose; and change in biomarkers, peripheral blood eosinophil counts, fractional exhaled nitric oxide (FeNO), and total serum immunoglobulin E (IgE). Most lung function tests were performed in daily clinical practice, while patients were undergoing treatment with continuous asthma controller medications that had bronchodilation effects (eg, ICS/long-acting β2-agonist [LABA], ICS, long-acting muscarinic antagonist [LAMA], or theophylline).
An asthma exacerbation was defined as a worsening of asthma that led to one of the following: use of systemic corticosteroids for 3 days or more or a temporary increase in a stable, background dosage of oral corticosteroids; an emergency department or urgent care visit (<24 h) due to asthma that required treatment with systemic corticosteroids; or an inpatient admission to hospital (≥24 h) due to asthma.
Data Collection
Data were collected in case report forms, and investigation items consisted of patient demographic and clinical data at baseline, information about exacerbations, hospitalization due to asthma, use of asthma treatments, current and past medical history, laboratory tests, concomitant drugs and/or therapies, information on benralizumab administration, clinical course, and AEs, including serious infections as a key item.
Statistical Analysis
This study aimed to enroll 600 patients to provide a sufficiently accurate estimate to detect serious infection frequency above a threshold of 2.2%, which is the combined frequency reported in the Phase 3 RCTs SIROCCO and CALIMA (2.2% [18/822] in the benralizumab 30 mg Q8W group),11,13 with 80% power if the true serious infection frequency was 4.4% (twice the frequency observed in Phase 3 RCTs). Safety was evaluated using the safety population, which included patients who received benralizumab at least once, but excluded those patients with an invalid registration, or lacking observation following enrollment. The effectiveness population was defined as patients with baseline efficacy data and one or more effectiveness measures but excluded patients who violated the approved usage of benralizumab in Japan.
Safety and effectiveness outcomes were descriptive. Data are presented using appropriate descriptive statistics such as mean, standard deviation (SD), median, minimum and maximum for continuous variables, and frequency and percentage for categorical variables. For a focused evaluation, possible background factors that could serve as effectiveness indicators were evaluated based on data from patients with severe uncontrolled asthma who had baseline ACQ-5 scores ≥1.5 and more than one ACQ-5 score measurement during the observation period. Additionally, subgroup analysis was conducted to compare ADR and ACQ-5 changes from baseline based on patient background characteristics. Fisher’s exact test was used to compare the proportion of patients with ADRs among groups defined by baseline characteristics. The tests were two-sided, and the significance level was 5%. The software used for statistical analysis was SAS version 9.4 (SAS Institute Inc., NC, USA).
Results
Patient Disposition and Baseline Characteristics
During the case registration period, 640 patients were enrolled (Figure 1). Eight patients were excluded for protocol deviations (n=4), lack of observation after enrollment (n=3), and lack of safety evaluation (n=1). Thus, a total of 632 patients were included in the safety population. Of these, 358 were excluded for not using a high-dose ICS plus additional controller at baseline (n=135), deviation of the approved dose (n=18), and lacking efficacy data for evaluations at baseline or at other time points (n=205). The resulting effectiveness population included 274 patients. After excluding 135 patients who lacked data or had a baseline ACQ-5 score <1.5, 139 patients were included in the severe uncontrolled asthma subgroup.
 |
Figure 1 Patient disposition. aACQ-5 improvement was evaluated. Abbreviations: ACQ-5, Asthma Control Questionnaire-5; ICS, inhaled corticosteroids. |
Table 1 summarizes the baseline characteristics of patients included in the safety population. Patients had a mean (SD) age of 63.9 (15.5) years; 45.9% of patients were ≥70 years of age. Of the total, 61.6% of patients were female, and the mean (SD) body mass index (BMI) was 24.0 (4.7) kg/m2. Patients had a median (min, max) disease duration of 14.0 (0.3, 85.0) years. The percentage of patients who experienced asthma exacerbation in the previous year was 77.8%. Concomitant drugs included a combination of ICS and LABA in 581 (92.1%); leukotriene receptor antagonist (LTRA) in 429 (68.0%); LAMA in 246 (39.0%); and theophylline in 186 (29.5%) patients. At baseline, 27.3% of patients were taking mOCS at a mean daily dose of 7.6 (6.0) mg/day prednisolone equivalent. Regarding previous treatments, 114 (18.2%) patients had received an anti-IL5 antibody, 48 (7.7%) had received an anti-IgE antibody, and five (0.8%) had received an anti-IL4 receptor α antibody. The mean blood eosinophil count was 557 (649) cells/μL at baseline. Benralizumab was used to treat 16 patients with “mild intermittent” asthma or “mild persistent” asthma (13 patients during the first year and an additional 3 patients in the subsequent year). Of these, 11 had a history of eosinophil-related complications (9 patients with chronic sinusitis, 3 patients with eosinophilic otitis media, 1 patient with eosinophilic esophagitis, and 1 patient with Churg–Strauss syndrome).
 |
Table 1 Patient Background Characteristics (Safety Population) |
Overall, the mean follow-up period was 302.3 (121.0) days. A total of 202 (32.0%) patients discontinued or withdrew from the study. The major reasons for discontinuation were insufficient effectiveness of the drug in 67 (10.6%), AEs in 46 (7.3%), improvement of symptoms in 24 (3.8%), cessation of hospital visits during treatment (ie, transfer to another hospital, move, or other) in 25 (4.0%), and other reasons in 40 (6.3%) patients.
Continuation rates and reasons for discontinuation were analyzed every 3 months (Table 2). Between 0 to <3 months, 46/632 (7.3%) patients discontinued; in ≥3 to <6 months, 59/586 (10.1%); in ≥6 to <9 months, 39/503 (7.8%); in ≥9 to <12 months, 41/464 (8.8%); and in ≥12 months, 17/218 (7.8%) discontinued. The most common reason for discontinuation was AEs (n=19) in 0 to <3 months, insufficient effectiveness in ≥3 to <9 months, and improved symptoms in ≥9 to <12 months.
 |
Table 2 Reasons for Discontinuation by Observation Period (Safety Population) |
Safety Assessments
Incidence of ADRs, Serious AEs, and Death
ADRs were reported for 12.7% (80 of 632) of patients (Table 3). ADRs that occurred in three or more patients were headache, 17 (2.7%); pyrexia, 15 (2.4%); asthma, 10 (1.6%); malaise, five (0.8%); pneumonia, five (0.8%); rash, four (0.6%); and eosinophil count increased, three (0.5%) (Supplementary Table 1).
 |
Table 3 Summary of Adverse Drug Reactions and Serious Adverse Events (Safety Population) |
Of the 13.0% (82 of 632) of patients who reported serious AEs, serious AEs that occurred in three or more patients were as follows: asthma, 44 (7.0%); pneumonia, nine (1.4%); pneumonia aspiration, four (0.6%); and bronchitis, four (0.6%) (Table 3, Supplementary Table 2).
One male patient died during the study. He had several comorbidities, including diabetes, hypertension, and chronic renal disease. The patient appeared to have inadequate adherence to the treatment regimen as he discontinued hospital visits 10 days after the initiation of benralizumab. The death of the patient was reported by approximately 3 months after treatment initiation, but no detailed information regarding the patient’s death was provided.
Concerning laboratory parameters, three patients presented with eosinophil count alterations after blood eosinophil count decreased to zero with benralizumab administration. One patient was treated with prednisolone 60 mg daily after developing edema as an AE 11 months post-benralizumab initiation. Over the course of approximately 1 month, the prednisolone dose was tapered to 22.5 mg daily, during which an eosinophil increase (AE) was observed and benralizumab was stopped. The eosinophil increase event was considered resolved (240 cells/µL) approximately 1 month after the maximum count (3322 cells/µL) was reached, and the eosinophil count returned to zero approximately 4 months later. Another patient presented with a transient increase in blood eosinophil count up to 8.7% (the absolute cell count was unavailable) 9 months after starting benralizumab. However, the eosinophil count decreased to zero after 1 month without additional treatment. The third patient’s eosinophil rate increased to 14.3% (915.2 cells/μL) after 10 months and then declined to 2.8% (204.4 cells/μL) after 3 more months. These events were not considered serious AEs. For all three patients who presented with an unexpected increase in eosinophil counts after treatment, the levels eventually decreased, and physicians judged their state as recovered.
Analysis of background factors associated with a higher frequency of ADRs showed that patients who had aspirin-exacerbated respiratory disease (AERD; 28.6%; p=0.0011), who initiated benralizumab at hospitalization (27.5%; p=0.0109), had a duration of asthma ≥30 years (19.5%; p=0.0257), and who had serum total IgE ≥150 IU/mL (17.2%; p=0.0227) presented with ADRs more frequently than patients with other background characteristics (Supplementary Table 3).
Safety Specifications Listed in the Risk Management Plan
Serious infection occurred in 24 (3.8%) patients. Serious infections occurring in three or more patients were nine (1.4%) patients with pneumonia, four (0.6%) patients with bronchitis, and four (0.6%) patients with aspiration pneumonia. All four patients (three with pneumonia and one with gastroenteritis) whose events were thought to be causally related to benralizumab treatment either recovered or improved. No helminthic infections were reported. No cases of COVID-19 were reported in this study.
Serious hypersensitivity, diagnosed as an anaphylactic reaction, occurred in two (0.3%) patients. One patient presented with wheezing and dyspnea 20 to 30 minutes after initiating benralizumab administration. The patient recovered within a day after receiving an adrenaline injection. Benralizumab administration was suspended due to this event. The other patient presented with skin itching and nausea 11 days after the first administration of benralizumab. However, the symptoms were recovering with levocetirizine treatment and the patient continued benralizumab without the recurrence of events, and thus, the investigator considered the causality of this anaphylactic reaction due to the patient’s concomitant disease, not to benralizumab.
Two (0.3%) patients developed a malignancy. One had an advanced colorectal adenocarcinoma with liver metastasis incidentally detected during examination for anorexia a week after initiation of benralizumab. The other was that of a patient with pancreatic cancer, which was discovered 4 months after benralizumab initiation; the outcome was reported as unrecovered. Neither was considered causally related to benralizumab by the reporting physician.
Effectiveness Assessments
The effectiveness population included 274 patients treated with benralizumab according to the approved usage in Japan. For these patients, the overall disease control improved after 1 year of treatment (Table 4). At the last observation, benralizumab improved the mean (SD) ACQ-5 score by −1.16 (1.40) (95% confidence interval [CI]: −1.36, −0.96) from baseline; mean (SD) FEV1, 0.151 (0.440) L (95% CI: 0.09, 0.21) from baseline; and mean (SD) MiniAQLQ score, 1.16 (1.29) (95% CI: 0.94, 1.38) from baseline.
 |
Table 4 Summary of Asthma Control Parameters (Effectiveness Population) |
Regarding biomarkers, peripheral blood eosinophil counts were suppressed after 4 weeks of treatment, and the suppression was maintained throughout the observation period (Supplementary Table 4).
Among the severe uncontrolled asthma patients whose baseline ACQ-5 score was ≥1.5 (n=139), the proportion of patients who had a decrease in ACQ-5 score of 0.5 (minimal clinically important difference) or more was 74.8% (104 of 139) at the last observation, the proportion of patients with well-controlled asthma (ACQ-5 <0.75) was 30.2% (42 of 139), and that of patients with partly controlled asthma (ACQ-5 0.75–1.5) was 18.0% (25 of 139) (Supplementary Table 5). The change in ACQ-5 score from baseline was >0.5 (minimal clinically important difference) for ACQ-5 scores in all patient subgroups of severe uncontrolled asthma (Figure 2). However, ACQ-5 score improvements were greater among male patients, those aged <70 years, those with severe persistent disease before treatment, disease duration of 10 to <20 years, BMI <25 kg/m2, those without history of AERD, with chronic sinusitis, with administration of systemic corticosteroids ≥3 times in the previous year, with eosinophil count ≥300/µL, higher FeNO (≥37 ppb), and serum total IgE ≥150 IU/mL. Patients who switched from an anti-IL5 antibody as previous treatments for asthma, such as mepolizumab, showed additional ACQ-5 score improvement (−1.37 [95% CI: −2.23, −0.51]).
The annual asthma exacerbation rate was 0.42/person-year. During the observation period, the proportion of patients who did not present with any asthma exacerbation with systemic corticosteroid use was 78.8%. The proportion of patients who did not suffer exacerbations requiring emergency room visits was 85.8%, and that of patients who did not suffer exacerbations requiring hospitalization was 93.1% (Table 5).
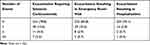 |
Table 5 Summary of Asthma Exacerbations During the Observation Period (Effectiveness Population; n=274) |
Among the patients requiring mOCS therapy at baseline in the effectiveness population, 33.3% (19 of 57) of patients withdrew from mOCS therapy at the last observation (Supplementary Figure 1).
Discussion
The present study showed that the profiles of safety, tolerability, and efficacy of benralizumab shown in RCTs were maintained in a sample of over 630 patients who started treatment in the real-world setting after benralizumab approval in Japan.
In the present sample of patients, the mean age was 63.9 years, which was higher than the mean age of patients in the CALIMA study (49.0 years of age, benralizumab 30 mg Q8W group), a Phase 3 trial including Japanese patients.11 Furthermore, the patients in the present study were treated more intensively compared with patients from the CALIMA study. For instance, in this study and CALIMA, respectively, 68.0% and 28.0% of patients had used LTRA; 39.0% and 9.0% had used LAMA, and 29.5% and 12.0% had used theophylline. Another relevant difference was that in the present study, 26.4% of patients were prescribed other biologics prior to benralizumab. However, such patients were excluded from CALIMA,11 as well as other Phase 3 trials.13,14
The overall discontinuation rate in our study was 32.0%. Reports on clinical practice in Japan showed that the 1-year discontinuation rates of omalizumab and mepolizumab were 41.4% and 43.1%, respectively,18,19 which are higher than reports from other countries.20 It is possible that the high medical expense burden for patients in Japan may have influenced the discontinuation rates of these drugs. The discontinuation rate due to AEs in our study was 7.3%, which is consistent with the reported rates in similar real-world studies (2%–10% after 1 year of biologics treatment).18,19,21,22 Similar to the proportion of patients who presented ADRs in this study (12.7%), the proportion reported in CALIMA was 13%.11 Additionally, no new safety signals were observed. Although the mean age in the present study was 14.9 years higher than that of patients from CALIMA, there were no significant differences in the proportions of ADRs regardless of the age group (ie, <70 years, 14.3%; ≥70 years, 10.7%; Supplementary Table 3).
Initiation of benralizumab as an inpatient (27.5%; p=0.0109), long asthma duration (≥30 years), presence of AERD, and baseline total IgE ≥150 IU/mL were identified as factors associated with a higher frequency of ADRs during benralizumab treatment in the present study. Of note, the frequency of asthma exacerbations was higher among patients with the initiation of benralizumab as an inpatient and long asthma duration (≥30 years) than other background characteristics. A recent study with a 2-year follow-up that included patients with severe asthma treated with anti-IL5 biologics found that shorter durations of asthma and higher FEV1 were associated with a greater response to treatment.23 The result of the present study in terms of long asthma duration (≥30 years) is consistent with the abovementioned study on anti-IL5 biologics for severe asthma.23 Furthermore, the frequency of hypersensitivity reactions (eg, rash pruritic) was higher in patients with AERD than those without AERD, as well as in patients with serum total IgE ≥150 IU/mL than those with IgE <150 IU/mL.
Serious infection was listed as an important potential risk in the Japanese RMP. The rate of serious infections in the present study was 3.8%, numerically higher than in the Phase 3 CALIMA and SIROCCO studies (1.9%–2.5%),11,13 and all cases were reported as recovered or improved. Long-term OCS therapy and chronic obstructive pulmonary disease (COPD) are associated with increased risk of infection.24,25 The proportions of the patients who had maintenance OCS therapy at baseline or had COPD in this study (mOCS 27.3%, COPD 22.9%) were higher than the Phase 3 studies (mOCS 10.0%–18.3%, COPD was excluded). This finding is thought to be almost consistent with previous reports indicating that patients with low blood eosinophil counts due to disease or treatments do not have an increased risk of infections.26,27 After the 1st of January 2020, 59 patients were registered in this study, during which time no cases of COVID-19 infection were reported. This result was consistent with an existing report on biologics for asthma.28
Serious hypersensitivity was listed as an important identified risk in the Japanese RMP because few serious hypersensitivity reactions have been reported in the completed studies of benralizumab for asthma. In the present study, anaphylaxis was reported in two patients. One patient who developed an anaphylactic reaction recovered quickly after an adrenaline injection, and the other patient who developed skin itching and nausea recovered with antihistamine. Hypersensitivity event rates were consistent with those reported in previously described RCTs (approximately 3%).11,13
Overall, the incidence of malignant neoplasm AEs in benralizumab-treated patients during the Phase 3 CALIMA and SIROCCO studies and the BORA extension study were low (<1%), with no apparent trends in organs or affected tissues.11,13,29 Although eosinophil infiltration of tumors is common, the cause and consequences (ie, protumorigenic versus antitumorigenic) of this recruitment and accumulation are unclear.30,31 Malignancy was listed as an important potential risk in the RMP. However, in the present study, malignancy was reported in only two patients, and neither of the cases was considered by the investigators to be related to benralizumab.
Recent evidence shows that eosinophils have multiple relevant biological functions.32 The safety of eosinophil depletion as a possible effect of the blockade of eosinophil-mediated immune regulation with eosinophil-targeted therapy, such as mepolizumab and benralizumab,32 is gaining attention. Furthermore, the frequency of ADRs in the patients who switched from mepolizumab (14.0%) was similar to that of the overall population (12.7%).
The ACQ-5 score change from baseline in the effectiveness population of the present study (−1.16 at the last observation) was lower than in previous reports. The ACQ-5 score change from baseline in severe uncontrolled asthma patients whose baseline ACQ-5 score was ≥1.5 was similar to that in the CALIMA study (the present study: −1.53, CALIMA study: −1.00 to −1.44).11 Senna et al reported an improvement in asthma control in a patient population with a baseline blood eosinophil count of 300 to 450 cells/μL treated with benralizumab.33 Additionally, in this study, improvement in ACQ-5 score beyond the minimal clinically important difference was observed in a patient population with a blood eosinophil count of <150 cells/μL (−0.92) and a patient population with a blood eosinophil count of 150 to <300 cells/μL (−1.33). A greater ACQ-5 score improvement was also observed among patients who had eosinophilic asthma characteristics, such as chronic sinusitis, eosinophil count ≥300/µL, higher FeNO (≥37 ppb), and serum total IgE ≥150 IU/mL. Patients who switched from mepolizumab showed additional ACQ-5 score improvement (−1.37). These observations were consistent with the mechanism of action of benralizumab that results in eosinophil depletion. Furthermore, these observations were consistent with predicting factors of benralizumab efficacy in the Phase 3 RCTs.11,13,14
The FEV1 change from baseline after 1 year of benralizumab administration in this study was 0.062 L, which was lower than the FEV1 at other evaluation time points. However, the FEV1 change from baseline at the last observation was 0.151 L, which was similar to that reported in previous studies, including patients who switched from other biologics.34,35
At present, the Global Initiative for Asthma guidelines recommend multiple biologics for eosinophilic severe asthma, but prioritization of biologics is yet to become available.2 It is expected that the findings from the present study will be helpful for patients with severe eosinophilic asthma who lack treatment.
This study has several limitations. There was no blinding in this open-label study, and no comparator was assessed. As a result, there was an imbalance between subgroups, which may have led to bias, and thus, the results of the subgroup analysis should be interpreted with caution. Additionally, the first patient with COVID-19 was confirmed in Japan in January 2020. With the adoption of social distancing, wearing of masks, and other public health interventions during the COVID-19 outbreak, there was a decrease in the frequency of asthma exacerbations, with fewer emergency department visits, as well as other asthma-related outcomes.36,37 Therefore, the interpretation of the differences in the frequency of asthma exacerbations before and after the study period should be done with caution. Despite these limitations, we consider that this study provides additional information regarding the safety and effectiveness of benralizumab in a large population of Japanese patients in a real-world setting.
Conclusion
In conclusion, no new safety concerns were raised during this post-marketing study conducted in a large population under real-world settings. Patients with severe uncontrolled asthma (ACQ-5 score ≥1.5) in this real-world study experienced similar benefits of the improvement in ACQ-5 score consistent with previous studies of benralizumab. The results support the use of benralizumab for the add-on maintenance treatment of patients with eosinophilic severe uncontrolled asthma.
Abbreviations
ABPA, allergic bronchopulmonary aspergillosis; ACQ-5, Asthma Control Questionnaire-5; ADR, adverse drug reaction; AE, adverse event; AERD, aspirin-exacerbated respiratory disease; BMI, body mass index; CI, confidence interval; EOM, eosinophilic otitis media; FeNO, fractional exhaled nitric oxide; FEV1, forced expiratory volume in 1 second; ICS, inhaled corticosteroids; IgE, immunoglobulin E; IL, interleukin; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; LTRA, leukotriene receptor antagonist; MiniAQLQ, Mini-Asthma Quality of Life questionnaire; mOCS, maintenance oral corticosteroid; OCS, oral corticosteroid; RCT, randomized controlled trial; RMP, risk management plan; SABA, short-acting β2-agonist; SD, standard deviation.
Data Sharing Statement
The data underlying the findings described in this manuscript may be obtained in accordance with AstraZeneca’s data sharing policy described at https://astrazenecagrouptrials.pharmacm.com/st/submission/disclosure.
Data for studies directly listed on Vivli can be requested through Vivli at www.vivli.org.
Data for studies not listed on Vivli could be requested through Vivli at https://vivli.org/members/enquiries-about-studies-not-listed-on-The-vivli-platform/.
The AstraZeneca Vivli member page is also available outlining further details: https://vivli.org/ourmember/astrazeneca/.
Acknowledgments
The authors wish to thank the investigators, research staff, health-care providers, and—in particular—the patients who participated in this study. The authors also wish to thank Toshimitsu Tokimoto, former employee of AstraZeneca K.K., for his contributions to the study and critically reviewing the manuscript, Tadataka Yabuta of Medical Department, AstraZeneca K.K. for critically reviewing the manuscript, and Keyra Martinez Dunn, MD, of Edanz, Japan for providing medical writing support, which was funded by AstraZeneca K.K., Japan, through EMC K.K., Japan, in accordance with Good Publication Practice 2022 guidelines (https://www.ismpp.org/gpp-2022).
Data from the manuscript were presented at the Japanese Society of Allergology meeting, Tokyo, Japan, 20–23 October 2023.
Author Contributions
All authors made a significant contribution to the work reported, whether that was in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study was funded by AstraZeneca K.K., Japan. The study sponsor provided funding for the study, publication, and medical writing and was involved in all stages of the study, such as the study design, data collection, analysis, and interpretation, as well as the review of the manuscript.
Disclosure
Yamaguchi M: AstraZeneca K.K.: support for this study, consulting fees, and lecture fees.
Nishimura Y: AstraZeneca K.K.: support for this study and consulting fees.
Takumi Y, Hayashi N, and Sakamoto K: employees of AstraZeneca K.K. and stock ownership in the company.
Tohda Y: AstraZeneca K.K.: support for this study and consulting fees; Boehringer-Ingelheim Co., Ltd., Kyorin Pharmaceutical Co., Ltd., Otsuka Pharmaceutical Factory, Taiho, Teijin Pharma Co., Ltd., Astellas, GSK, Daiichi Sankyo Co., Ltd., Ono Pharmaceutical: grants or contracts; AstraZeneca K.K., Kyorin Pharmaceutical Co., Ltd., Teijin Pharma Co., Ltd., Boehringer Ingelheim Co., Ltd., Daiichi Sankyo Co., Ltd., Astellas, Pearl Therapeutics, Inc.: payment or honoraria.
References
1. The Global Asthma Report 2022. Available from: http://globalasthmareport.org/burden/burden.php.
2. GINA Main Report 2022. Available from: https://ginasthma.org/wp-content/uploads/2022/07/GINA-Main-Report-2022-FINAL-22-07-01-WMS.pdf.
3. Nagase H, Adachi M, Matsunaga K, et al. Prevalence, disease burden, and treatment reality of patients with severe, uncontrolled asthma in Japan. Allergol Int. 2020;69(1):53–60. doi:10.1016/j.alit.2019.06.003
4. Wang E, Wechsler ME, Tran TN, et al. Characterization of severe asthma worldwide: data from the International Severe Asthma Registry. Chest. 2020;157(4):790–804. doi:10.1016/j.chest.2019.10.053
5. Scichilone N, Barnes PJ, Battaglia S, et al. The hidden burden of severe asthma: from patient perspective to new opportunities for clinicians. J Clin Med. 2020;9(8):2397. doi:10.3390/jcm9082397
6. Inoue H, Kozawa M, Milligan KL, Funakubo M, Igarashi A, Loefroth E. A retrospective cohort study evaluating healthcare resource utilization in patients with asthma in Japan. NPJ Prim Care Respir Med. 2019;29(1):13. doi:10.1038/s41533-019-0128-8
7. Heaney LG, Perez de Llano L, Al-Ahmad M, et al. Eosinophilic and noneosinophilic asthma: an expert consensus framework to characterize phenotypes in a global real-life severe asthma cohort. Chest. 2021;160(3):814–830. doi:10.1016/j.chest.2021.04.013
8. Louis R, Lau LC, Bron AO, Roldaan AC, Radermecker M, Djukanović R. The relationship between airways inflammation and asthma severity. Am J Respir Crit Care Med. 2000;161(1):9–16. doi:10.1164/ajrccm.161.1.9802048
9. Talini D, Novelli F, Bacci E, et al. Sputum eosinophilia is a determinant of FEV1 decline in occupational asthma: results of an observational study. BMJ Open. 2015;5(1):e005748. doi:10.1136/bmjopen-2014-005748
10. Belda J, Parameswaran K, Lemiere C, Kamada D, O’Byrne PM, Hargreave FE. Predictors of loss of asthma control induced by corticosteroid withdrawal. Can Resp J. 2006;13:129–133.
11. FitzGerald JM, Bleecker ER, Nair P, et al. Benralizumab, an anti-interleukin-5 receptor α monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2016;388(10056):2128–2141. doi:10.1016/S0140-6736(16)31322-8
12. Kolbeck R, Kozhich A, Koike M, et al. MEDI-563, a humanized anti-IL-5 receptor alpha mAb with enhanced antibody-dependent cell-mediated cytotoxicity function. J Allergy Clin Immunol. 2010;125(6):1344–1353.e2. doi:10.1016/j.jaci.2010.04.004
13. Bleecker ER, FitzGerald JM, Chanez P, et al. Efficacy and safety of benralizumab for patients with severe asthma uncontrolled with high-dosage inhaled corticosteroids and long-acting β2-agonists (SIROCCO): a randomised, multicentre, placebo-controlled phase 3 trial. Lancet. 2016;388(10056):2115–2127. doi:10.1016/S0140-6736(16)31324-1
14. Nair P, Wenzel S, Rabe KF, et al. Oral glucocorticoid-sparing effect of benralizumab in severe asthma. N Engl J Med. 2017;376(25):2448–2458. doi:10.1056/NEJMoa1703501
15. Tan YY, Papez V, Chang WH, Mueller SH, Denaxas S, Lai AG. Comparing clinical trial population representativeness to real-world populations: an external validity analysis encompassing 43 895 trials and 5 685 738 individuals across 989 unique drugs and 286 conditions in England. Lancet Healthy Longev. 2022;3(10):e674–e689. doi:10.1016/S2666-7568(22)00186-6
16. AstraZeneca PLC. Fasenra (Benralizumab) Package Insert. AstraZeneca PLC; 2018.
17. Nakamura Y, Tamaoki J, Nagase H, et al. Japanese guidelines for adult asthma 2020. Allergol Int. 2020;69(4):519–548. doi:10.1016/j.alit.2020.08.001
18. Adachi M, Kozawa M, Yoshisue H, et al. Real-world safety and efficacy of omalizumab in patients with severe allergic asthma: a long-term post-marketing study in Japan. Respir Med. 2018;141:56–63. doi:10.1016/j.rmed.2018.06.021
19. Tsuboi E. [Evaluation of long-term safety and efficacy of recombinant mepolizumab in bronchial asthma patients under actual use: interim report of a specific use-results survey]. Therapeutic Research. 2023;44(6):405–421. In Japanese.
20. Menzies-Gow AN, McBrien C, Unni B, et al. Real world biologic use and switch patterns in severe asthma: data from the International Severe Asthma Registry and the US CHRONICLE Study. J Asthma Allergy. 2022;15:63–78. doi:10.2147/JAA.S328653
21. Pilette C, Canonica GW, Chaudhuri R, et al. REALITI-A Study: real-world oral corticosteroid-sparing effect of mepolizumab in severe asthma. J Allergy Clin Immunol Pract. 2022;10(10):2646–2656. doi:10.1016/j.jaip.2022.05.042
22. Thelen JC, van Zelst CM, van Brummelen SE, et al. Efficacy and safety of dupilumab as add-on therapy for patients with severe asthma: a real-world Dutch cohort study. Respir Med. 2023;206:107058. doi:10.1016/j.rmed.2022.107058
23. Eger K, Kroes JA, Ten Brinke A, Bel EH. Long-term therapy response to anti-IL-5 biologics in severe asthma—a real-life evaluation. J Allergy Clin Immunol Pract. 2021;9(3):1194–1200. doi:10.1016/j.jaip.2020.10.010
24. Price DB, Trudo F, Voorham J, et al. Adverse outcomes from initiation of systemic corticosteroids for asthma: long-term observational study. J Asthma Allergy. 2018;11:193–204. doi:10.2147/JAA.S176026
25. Inghammar M, Engström G, Kahlmeter G, Ljungberg B, Löfdahl CG, Egesten A. Invasive pneumococcal disease in patients with an underlying pulmonary disorder. Clin Microbiol Infect. 2013;19(12):1148–1154. doi:10.1111/1469-0691.12182
26. Gleich GJ, Klion AD, Lee JJ, Weller PF. The consequences of not having eosinophils. Allergy. 2013;68(7):829–835. doi:10.1111/all.12169
27. Legrand F, Klion AD. Biologic therapies targeting eosinophils: current status and future prospects. J Allergy Clin Immunol Pract. 2015;3(2):167–174. doi:10.1016/j.jaip.2015.01.013
28. Poddighe D, Kovzel E. Impact of anti-type 2 inflammation biologic therapy on COVID-19 clinical course and outcome. J Inflamm Res. 2021;14:6845–6853. doi:10.2147/JIR.S345665
29. Busse WW, Bleecker ER, FitzGerald JM, et al. Long-term safety and efficacy of benralizumab in patients with severe, uncontrolled asthma: 1-year results from the BORA phase 3 extension trial. Lancet Respir Med. 2019;7(1):46–59. doi:10.1016/S2213-2600(18)30406-5
30. Jackson DJ, Korn S, Mathur SK, et al. Safety of eosinophil-depleting therapy for severe, eosinophilic asthma: focus on benralizumab. Drug Saf. 2020;43(5):409–425. doi:10.1007/s40264-020-00926-3
31. Jacobsen EA, Helmers RA, Lee JJ, Lee NA. The expanding role(s) of eosinophils in health and disease. Blood. 2012;120(19):3882–3890. doi:10.1182/blood-2012-06-330845
32. Lombardi C, Berti A, Cottini M. The emerging roles of eosinophils: implications for the targeted treatment of eosinophilic-associated inflammatory conditions. Curr Res Immunol. 2022;3:42–53. doi:10.1016/j.crimmu.2022.03.002
33. Senna G, Aliani M, Altieri E, et al. Clinical features and efficacy of benralizumab in patients with blood eosinophil count between 300 and 450 cells/mm3: a post hoc analysis from the ANANKE study. J Asthma Allergy. 2022;15:1593–1604. doi:10.2147/JAA.S383012
34. Kavanagh JE, Hearn AP, Dhariwal J, et al. Real-world effectiveness of benralizumab in severe eosinophilic asthma. Chest. 2021;159(2):496–506. doi:10.1016/j.chest.2020.08.2083
35. Numata T, Araya J, Okuda K, et al. Long-term efficacy and clinical remission after benralizumab treatment in patients with severe eosinophilic asthma: a retrospective study. J Asthma Allergy. 2022;15:1731–1741. doi:10.2147/JAA.S391807
36. Al-Hazaymeh A, Patrie J, Adams JC, Borish L, McGowan EC. Asthma-related outcomes during the SARS-CoV2 pandemic: a single-center observational study. J Allergy Clin Immunol Pract. 2021;9(9):3483–3486.e2. doi:10.1016/j.jaip.2021.05.034
37. Abe K, Miyawaki A, Nakamura M, Ninomiya H, Kobayashi Y. Trends in hospitalizations for asthma during the COVID-19 outbreak in Japan. J Allergy Clin Immunol Pract. 2021;9(1):494–496.e1. doi:10.1016/j.jaip.2020.09.060
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

