Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 15
Prevalence and Outpatient Clinical Diagnostic Approaches for Common Acute Respiratory Tract Infections in Children Under Five Years of Age: A Cross-Sectional Study
Authors Turyasiima M , Kiconco G, Egesa WI , Twesigemukama S, Nduwimana M
Received 21 October 2023
Accepted for publication 9 January 2024
Published 20 January 2024 Volume 2024:15 Pages 49—57
DOI https://doi.org/10.2147/PHMT.S445908
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Roosy Aulakh
Munanura Turyasiima,1,2 Gloria Kiconco,1,3 Walufu Ivan Egesa,4 Sabinah Twesigemukama,1 Martin Nduwimana1
1Department of Pediatrics and Child Health, Kampala International University, Kampala, Uganda; 2Department of Standards Compliance Accreditation and Patient Protection (SCAPP), Ministry of Health, Kampala, Uganda; 3Department of Pediatrics and Child Health, Fort Portal Regional Referral Hospital, Fort Portal, Uganda; 4Department of Pediatrics, Nile International Hospital, Jinja, Uganda
Correspondence: Munanura Turyasiima, Department of Pediatrics and Child Health, Kampala International University, P.O Box 20000, Kampala, Uganda, Email [email protected]
Background: Acute respiratory tract infections are among the leading causes of child morbidity and mortality worldwide. Although the diagnosis of acute respiratory tract infections requires simple outpatient medical techniques and care, it is still misdiagnosed among primary care physicians, leading to delayed treatment and increased mortality. This study described the prevalence of common acute respiratory tract infections and simple techniques that effectively detect and diagnose children presenting with acute respiratory symptoms to primary healthcare physicians in remote settings.
Patients and Methods: This descriptive cross-sectional study was conducted at the pediatric outpatient clinic of a tertiary hospital in western Uganda in April, May and June 2019. A total of 896 children aged 2– 59 months attending the clinic were recruited consecutively into the study and examined for the presence of acute respiratory infection. Participants’ sociodemographic and clinical data were collected through history taking and clinical examination using a validated Uganda Ministry of Health Uganda outpatient clinical checklist (FORM 5). The outcome variable was the presence of an acute upper or lower respiratory condition. Data was analyzed using STATA version 13.0 (StataCorp, College Station, USA) and summarized using descriptive statistics.
Results: The overall period prevalence of acute respiratory tract infections among children aged 2 to 59 months was 36.9% (36,942 per 100,000 population). Upper respiratory tract infections with a prevalence of 24.8% were more common than lower respiratory tract infections. The most frequent upper respiratory tract infection in this setting was common cold (52%), followed by tonsillopharyngitis (10.7%), while pneumonia (26%) was the most frequent lower respiratory tract infection.
Conclusion: Acute respiratory tract infections contribute to the high burden of disease in pediatric outpatient clinics. Simple, affordable, and approved diagnostic clinical techniques that involve physical examination of the upper and lower respiratory systems can precisely diagnose acute respiratory tract infections in resource-limited settings where there is no access to sophisticated diagnostic equipment.
Keywords: acute respiratory tract infections, outpatient diagnosis, children aged 2 to 59 months
Introduction
Acute respiratory tract infections (ARTIs) are responsible for almost 20% of all deaths of children aged less than 5 years worldwide,1 and together with whooping cough, ARTIs contribute more than 16% of the total under-five mortality in sub-Saharan Africa.2 There is an increasing global incidence of upper respiratory infections that now account for 42.8% of cases from all causes and the highest incidence rate observed among those under five years (300,532.1 per 100,000 population), as described in the global burden of disease (GBD) 2019 study.3 In 2019, lower and upper respiratory tract infections were responsible for 7.7% of the total deaths among under-five children in Uganda.2 Acute respiratory infections classified into upper and lower respiratory tract infections (RTIs) can occur in any part of the respiratory system, from the middle ear to the nose to the lungs.4 The common upper ARTIs include acute rhinopharyngitis (common cold), sinusitis, ear infections, acute pharyngitis or tonsillopharyngitis, epiglottitis, and laryngitis, of which ear infections and pharyngitis cause more severe complications (deafness and acute rheumatic fever, respectively), and the common lower RTIs in children are pneumonia and bronchiolitis.1,4,5
The diagnosis of respiratory tract infections is a challenge since no single test can isolate all potential pathogens, and all diagnostic tests are associated with limitations.4,6 During the UNICEF/WHO Meeting on Child Survival Survey-based Indicators, it was recommended to define acute respiratory infection based on mothers’ perceptions of a child who has a cough, is breathing faster than usual with short, quick breaths, or is having difficulty breathing, excluding children who had only a blocked nose.1 This definition is an envelope of many acute respiratory diseases, as the majority of children will always present with acute respiratory symptoms, yet treatment prescription will differ according to the specific disease.
Highly specific and sensitive tests such as culture and sensitivity, direct immunofluorescence test, complement fixation, serology, and antigen detection to isolate the causative organisms6 are very expensive and not available at most primary healthcare centers in developing countries. In such settings where laboratory diagnosis is not possible, history taking and physical examination of the respiratory system, if well conducted, can identify and diagnose children suffering from acute respiratory infections yet guide proper treatment.
The Integrated Management of Childhood Illness guidelines7 is a chart booklet used in the World Health Organization health regions to assist primary health workers in making precise diagnoses for common childhood illnesses, including acute respiratory infections. However, this booklet is not comprehensive enough, and the definitions of some ARIs are not specific; hence, it is a challenge for clinicians to assign specific treatments. This hospital-based study described the outpatient clinical diagnostic approaches and prevalence of commonly missed acute respiratory tract infections among children presenting with acute respiratory symptoms to the primary healthcare physician in a resource-limited setting.
Materials and Methods
Study Design and Setting
This was a descriptive cross-sectional study at Kampala International University Teaching Hospital (KIU-TH), a general hospital located in Western Uganda from April to June 2019. KIU-TH is a private not-for-profit tertiary hospital in the Greater Bushenyi District, western Uganda providing tertiary services in pediatric, maternity, surgery, and general medicine. The study was conducted in the outpatient clinic of the Pediatric Department.
Sample Size Determination and Sampling Procedure
A total of 896 children aged 2–59 months who attended outpatient clinics during the study period were recruited. The children presenting to the physician with at least one of the acute respiratory symptoms, including running nose, cough, fast breathing, and difficulty breathing, were suspected of having a respiratory infection, and a complete physical respiratory examination was conducted.
We excluded children with clinical features of acute aspiration, near drowning, acute foreign body aspiration/inhalation, and asthma as causes of acute respiratory distress in the children (see Figure 1).
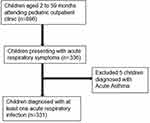 |
Figure 1 Inclusion and exclusion of study participants. |
Study Variables, Tools, and Data Collection Procedure
Screening of the participants for eligibility was performed by a trained licensed nurse, and all screened children were seen and examined by two independent pediatricians who made the diagnosis of acute respiratory tract infections (ARTIs).
The outcome variable was a child diagnosed with ARTI whose respiratory tract symptoms had not lasted more than 14 days expressed as prevalence. These were classified into upper and lower respiratory tract infections based on the anatomic classification of respiratory diseases.6,7 Independent variables included child demographics, such as age, sex, residence status, nutritional status, and religion of the mother.
The Ministry of Health Uganda validated outpatient clinical checklist (FORM 5) was used to capture parental/child’s demographic information, presenting complaints (focusing on respiratory symptoms) and physical examination findings for every child. History of presenting complaints was validated through physical respiratory examination by the attending pediatrician, and chest radiographs (X-rays) were performed for children who were found to have abnormal breath sounds, including crackles, wheezing, and bronchial breathings on auscultation, to confirm lower respiratory infections.
We examined the throat for features of tonsillitis and/or pharyngitis, performed an ear exam through otoscopy to diagnose and confirm otitis media, counted the number of chest movements to approximate the respiratory rate, and performed chest auscultation (with Litman® stethoscope) for any added sounds to examine for the possibility of pneumonia and bronchiolitis. Chest X-rays were performed for all children suspected to have pneumonia or bronchiolitis ruling out asthma (see Table 1).
 |
Table 1 Outpatient Diagnostic Criteria for Common Acute Respiratory Infections |
Data Analysis
Data were arranged, coded, and entered into the computer using EXCEL 2016 and then imported to STATA version 13.0 (StataCorp, College Station, USA) for analysis. Descriptive statistical analysis was performed to determine the frequencies and proportions of different respiratory infections. Period prevalence was calculated by dividing the number of children diagnosed with a respiratory infection by the total number of children seen in the outpatient clinic in the study period (3 months).
Outpatient Diagnostic Approaches and Definitions of Acute Respiratory Infections
The diagnosis of Acute Respiratory Infections was based on clinical history and physical chest examination of the children presenting with acute respiratory symptoms.7,14 In addition, chest radiography, visual inspection of the throat, and otoscopic examination of the ears in children are suspected to have pneumonia and/or bronchiolitis, tonsillopharyngitis, and acute otitis media, respectively.4–7,11,15 This is described in Table 1.
Results
Social Demographic Data
A total of 896 children aged 2 to 59 months attending the pediatric outpatient clinic were recruited into the study with an average age of 22.7 months. Three hundred thirty-six (336) children presented with acute respiratory tract symptoms such as cough, nasal discharge, and noisy or fast breathing, the majority of whom were males (53.3%) aged 24 to 59 months (51.8%) of rural residences (54.2%), whose parents/caretakers had attained primary level of education (42%). This is shown in Table 2.
 |
Table 2 Socio-Demographic Characteristics of the Study Participants |
Prevalence of Acute Respiratory Infections Among Children Attending the Outpatient Pediatric Clinic
The majority of children presenting with acute respiratory symptoms, 98.5% (331/336), were diagnosed with at least one acute respiratory infection (ARTI) by the physician. Five children presenting with acute respiratory symptoms were diagnosed with asthma and excluded from the study.
Upper respiratory tract infections (URTIs) found in these children included the common cold, tonsillopharyngitis, acute otitis media, and pertussis-like syndrome, while lower respiratory tract infections (LRTIs) were pneumonia and bronchiolitis in order of decreasing frequency (see Table 3).
 |
Table 3 Prevalence Rates and Proportions of Acute Respiratory Tract Infections by Child Age Group |
The overall prevalence of acute respiratory infections in this study among children aged 2 to 59 months was 36.9% (36,942 per 100,000 population). The prevalence of URTIs was twice that of LRTIs at 24.8% (24,776.8 per 100,000 population) and 12.2% (12,165.2 per 100,000 population) respectively. The most frequent URTI was common cold (52%), while pneumonia (26%) was the most frequent LRTI. This is shown in Table 3.
Common cold was the most frequent condition across all age categories. Acute tonsillopharyngitis (15.9%) and otitis media (5.3%) were found mostly among children aged 24 to 59 months. Pneumonia was mostly diagnosed among children aged below 6 months (37%), while bronchiolitis occurred most often among children aged 6 to 11 months (16.2%). This is shown in Table 3.
Discussion
Acute respiratory tract infections are the most common infectious diseases and one of the leading causes of mortality in children under five.3,4,6 In limited resource settings where invasive procedures are not possible, proper history and clinical chest examination are paramount due to diagnostic challenges. This study described the prevalence and simple outpatient diagnosis approaches of the most common acute respiratory tract infections (ARTIs).
Overall, 36.9% of children under five years attending the outpatient clinic at this hospital suffered an acute respiratory tract infection. This is comparable to the findings from the systematic review that acute respiratory tract infections (ARTIs) account for 20–40% of outpatient and 12–35% of inpatient attendance in general hospitals.16
In this study, upper RTIs in children aged 2 to 59 months accounted for 24.8% (24,776.8 per 100,000 population) of the total pediatric outpatient burden and constituted 67% of the total respiratory tract infections. Although we were not able to control for the incidence-prevalence bias in this study, these findings of high prevalence in this population reflect the increasing global incidence of upper respiratory infections that now account for 42.8% of cases from all causes and the highest incidence rate observed among those under five years (300,532.1 per 100,000 population), as described in the global burden of disease (GBD) 2019 study.3
Common cold accounted for 19.2% (172/896) of the total outpatient attendance and was the most frequent (52%) acute RTI in this study. This finding is comparable to the national common cold 24.8% contribution of the total under-five outpatient attendance only second to malaria infection according to Ministry of Health data.17 This is also consistent with studies performed in Uganda and Cameroon, in which the common cold accounted for 49% and 54.7% of the total children presenting with acute respiratory symptoms in outpatient clinics.18,19 The common cold is the most common respiratory infection in children living in developing countries, as most of its population is not vaccinated against the influenza virus, the leading cause of the common cold in children.16,20
Twenty-six percent of the children presenting with acute respiratory symptoms had pneumonia, and pneumonia was the second most frequent ARTI, with a prevalence of 9598.2 per 100,000 population. World Health Organization data captures all children presenting with acute respiratory symptoms as acute RTI, and this is described as “presumed pneumonia” to reflect probable cause better and the recommended interventions.1 According to this indicator, 9–10.6% of children aged five years and younger present to health workers with acute respiratory symptoms in Uganda and hence are considered to suffer from pneumonia.17,21 In a study conducted in Uganda at Mulago National Referral Hospital, 61.9% of children aged under five years presenting with acute respiratory symptoms had pneumonia.15 The discrepancy between the national prevalence and hospital studies shows how significantly indicators change with the use of the right diagnostic criteria since the presence of respiratory symptoms in a child captures a syndrome of many other diseases and not only pneumonia. In this study, we used history-taking and chest auscultation and added chest radiographs to distinguish pneumonia from other lower respiratory infections, such as bronchiolitis.7,9,11
Pneumonia is the single largest infectious cause of death in children worldwide, affecting children and families everywhere, but deaths are highest in southern Asia and sub-Saharan Africa.22 Although its diagnosis is quick and simple through history and physical examination, it is often missed by primary healthcare physicians, and treatment is delayed.
Bronchiolitis is often misdiagnosed by primary healthcare physicians as pneumonia, as both conditions often present with cough, fevers, and difficulty breathing,9 yet a slight line of differences exists in outpatient diagnosis and treatment. In this study, 6.8% of the children presenting with acute respiratory symptoms had bronchiolitis, with an prevalence rate of 2567 per 100,000 population. The Integrated Management of Childhood Illnesses guidelines7 do not clearly distinguish bronchiolitis from pneumonia, the two life-threatening lower respiratory tract diseases in children aged under five years. In the outpatient setting, bronchiolitis presents in a child as a first wheeze plus respiratory distress with a prodrome of fever, cough, congestion, and rhinorrhea.5,10 It is a viral lower respiratory infection mostly caused by respiratory syncytial virus in young infants younger than two years of age and is associated with high mortality in infants younger than six months. Similar to pneumonia, chest examination sometimes will reveal crackles, but the presence of a first episodic wheezing before 12 months of age is pathognomonic,9,10 and a chest radiograph (X-ray) will show signs of hyperinflation, which is not common in pneumonic chest X-ray unless it is complicated with pneumothorax.
Tonsillopharyngitis was present in 10.7% of the children presenting with acute respiratory symptoms to the outpatient clinic, with a prevalence of 4017.9 per 100,000 population (Table 3). This is approximately 6 times lower than the prevalence of streptococcal pharyngitis in the data from a pooled meta-analysis of the prevalence of streptococcal pharyngitis and streptococcal carriage presenting with a sore throat in children.12 This study recruited only children presenting with symptoms of acute respiratory disease and probably missed asymptomatic forms of tonsillopharyngitis. Tonsillopharyngitis is an infection of the tonsils and pharynx that often follows a common cold. In the outpatient setting, children with bacterial tonsillopharyngitis present with a history of sore throat (school-going children), drooling of saliva (infants) with the presence of petechiae, vesicles, or discharge compared to the viral form where the tonsils and the pharynx merely appear red or inflamed on visual inspection.23,24
Acute otitis media had a prevalence of 1450.9 per 100,000 population and was the 5th most common acute respiratory infection in this population. This is similar to the prevalence in other African countries and higher than the prevalence rates in developed countries such as Norway, England, and the United States, probably due to better pneumococcal conjugate vaccination rates in the developed world.25–29 Although mostly ignored and under-looked by most physicians, acute otitis media, which is the inflammation of the structures of the middle ear, is common and associated with long-term complications such as hearing loss when diagnosis and treatment are delayed.26,30 Outpatient diagnosis is possible through visualization of inflammation or whitish discharge in an outpatient visual inspection using an otoscope.7,30
Conclusion
This study found a high prevalence of both upper and lower acute respiratory tract infections in children under five years of age. Diagnosis of acute respiratory tract infections using simple and affordable procedures in an outpatient clinical setting by primary healthcare physicians is feasible through history taking and physical chest examination which involves visual inspection, palpation, percussion and auscultation with a stethoscope, and visual inspection of the tonsils, pharynx, and ears for all children who present with acute respiratory symptoms in the outpatient clinics. In resource-limited settings where laboratory isolation of specific causative agents for respiratory tract infections is almost impossible, these procedures give almost 100% certainty that the infection is present or not7 and can guide the physician to proper effective treatment.
Abbreviations
ARIs, Acute Respiratory Infections; WHO, World Health Organization; IMCI, Integrated Management of Childhood Illnesses; GINA, Global Initiative for Asthma; REC, Research Ethics Committee.
Data Sharing Statement
The dataset will be shared by the corresponding author upon request.
Ethical Considerations
Ethical approval was obtained from the research ethics committee (REC) of Kampala International University (No: UG-REC-023/201902). Informed consent was sought from each child’s parent/caretaker, and the purpose of the study was well explained to the parents/caregivers before administering the questionnaire. The study was conducted in accordance with the ethical principles and regulations set in the Declaration of Helsinki regarding biomedical research involving human subjects.
Acknowledgment
We thank the radiologists and nursing staff of Kampala International University Teaching Hospital who helped with patient clerkship, chest radiography and interpretation. This research article is part of the Thesis for the Award of Masters of Medicine in Pediatrics and Child Health; therefore, we thank all other pediatricians at Kampala International University Teaching Hospital for their guidance throughout the study.
This research article is the second of the article series of the Pneumonia Study conducted at Kampala International University Teaching Hospital.31
Author Contributions
All authors made substantial contributions to the conception and design of the study, acquisition of data, or data analysis and interpretation, took part in drafting the article or revising it critically for important intellectual content, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
There was no funding for this research; it was part of the thesis for the award of Masters of Medicine in Pediatrics and Child Health of Kampala International University.
Disclosure
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
1. World Health Organization. Children aged <5 years with acute respiratory infection (ARI) symptoms taken to facility (%). The Global Health Observatory. Explore a world of health data; 2023 [cited August 29, 2023]. Available from: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3147.
2. GBD Compare Data Visualization. Seattle WIU of W. Institute for Health Metrics and Evaluation (IHME); 2020 [cited August 29, 2023]; Available from: http://vizhub.healthdata.org/gbd-compare.
3. Jin X, Ren J, Li R, et al. Global burden of upper respiratory infections in 204 countries and territories, from 1990 to 2019. EClinicalMedicine. 2021;37:100986. doi:10.1016/j.eclinm.2021.100986
4. Calderaro A, Buttrini M, Farina B, Montecchini S, De Conto F, Chezzi C. Respiratory tract infections and laboratory diagnostic methods: a review with a focus on syndromic panel-based assays. Microorganisms. 2022;10(9):1856. doi:10.3390/microorganisms10091856
5. Ralston SL, Lieberthal AS, Meissner HC, et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014;134(5):e1474–e502. doi:10.1542/peds.2014-2742
6. Mauch H. Diagnosis of acute respiratory tract infections: serology and new method. Clin Microbiol Infect. 1996;1:2S16–9. doi:10.1111/j.1469-0691.1996.tb00186.x
7. World Health Organization. Integrated Management of Childhood Illness (IMCI) Chart Booklet [Internet]. Switzerland; 2014 [cited August 21, 2023]. Available from: https://resourcecentre.savethechildren.net/document/imci-chart-booklet/.
8. Global Initiative for Asthma. Global strategy for asthma management and prevention; 2019 [cited August 30, 2023]; Available from: www.ginasthma.org.
9. Friedman JN, Rieder MJ, Walton JM; Canadian Paediatric Society ACCDT and HSC. Bronchiolitis: recommendations for diagnosis, monitoring and management of children one to 24 months of age. Paediatr Child Health. 2014;19(9):485–498. doi:10.1093/pch/19.9.485
10. Cahill AA, Cohen J. Improving evidence based bronchiolitis care. Clin Pediatr Emerg Med. 2018;19(1):33–39. doi:10.1016/j.cpem.2018.02.003
11. O’Grady KAF, Torzillo PJ, Frawley K, Chang AB. The radiological diagnosis of pneumonia in children. Pneumonia. 2014;5(Suppl 1):38–51. doi:10.15172/pneu.2014.5/482
12. Shaikh N, Leonard E, Martin JM. Prevalence of streptococcal pharyngitis and streptococcal carriage in children: a meta-analysis. Pediatrics. 2010;126(3):e557–e564. doi:10.1542/peds.2009-2648
13. Gu W, Wang K, Zhang X, et al. Pathogen analysis of pertussis-like syndrome in children. BMC Infect Dis. 2020;20(1):353. doi:10.1186/s12879-020-05074-8
14. Saffar M, Hashemi A, Ghorbani G, Rezai M, Shahmohammadi S, Shojaei J. Clinical and laboratory features of pertussis in hospitalized infants with confirmed versus probable pertussis cases. Ann Med Health Sci Res. 2014;4(6):910. doi:10.4103/2141-9248.144911
15. Nantanda R, Tumwine JK, Ndeezi G, Ostergaard MS, Schildgen O. Asthma and pneumonia among children less than five years with acute respiratory symptoms in Mulago Hospital, Uganda: evidence of under-diagnosis of asthma. PLoS One. 2013;8(11):e81562. doi:10.1371/journal.pone.0081562
16. Jain N, Lodha R, Kabra SK. Upper respiratory tract infections. Indian J Pediatr. 2001;68(12):1135–1138. doi:10.1007/BF02722930
17. Ministry of Health. Annual Health Sector Performance Report - FY 2021/22 [Internet]; 2022. Available from: http://health.go.ug/.
18. Kibuule D, Kagoya HR. Household management of acute respiratory infections in children under five years in Kampala Uganda. Afr J Pharm Pharmacol. 2015;9(30):730–737. doi:10.5897/AJPP2015.4378
19. Tazinya AA, Halle-Ekane GE, Mbuagbaw LT, Abanda M, Atashili J, Obama MT. Risk factors for acute respiratory infections in children under five years attending the Bamenda Regional Hospital in Cameroon. BMC Pulm Med. 2018;18(1):7. doi:10.1186/s12890-018-0579-7
20. Denny FW. The clinical impact of human respiratory virus infections. Am J Respir Crit Care Med. 1995;152(4_pt_2):S4–S12. doi:10.1164/ajrccm/152.4_Pt_2.S4
21. Uganda Bureau of Statistcs (UBOS) and ICF. Uganda Demographic and Health Survey 2016: Key Indicators Report. Kampala, Uganda: UBOS, and Rockville, Maryland, USA: UBOS and ICF; 2017:4. Available from: https://dhsprogram.com/pubs/pdf/PR80/PR80.pdf%0Awww.ubos.org.
22. World Health Organization. Pneumonia in Children [Internet]; 2022 [cited August 19, 2023]. Available from: https://www.who.int/news-room/fact-sheets/detail/pneumonia.
23. Anderson J, Paterek E. Tonsillitis. StatPearls Publishing; 2023 [cited October 12, 2023]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544342/.
24. Gerber MA. Diagnosis and Treatment of Pharyngitis in Children. Pediatr Clin North Am. 2005;52(3):729–747. doi:10.1016/j.pcl.2005.02.004
25. Kvaerner KJ, Austeng ME, Abdelnoor M. Hospitalization for Acute Otitis Media as a Useful Marker for Disease Severity. Pediatr Infect Dis J. 2013;32(9):946–949. doi:10.1097/INF.0b013e318297c436
26. Hu T, Done N, Petigara T, et al. Incidence of acute otitis media in children in the United States before and after the introduction of 7- and 13-valent pneumococcal conjugate vaccines during 1998–2018. BMC Infect Dis. 2022;22(1):294. doi:10.1186/s12879-022-07275-9
27. Mohanty S, Podmore B, Cuñado Moral A, et al. Incidence of acute otitis media from 2003 to 2019 in children ≤ 17 years in England. BMC Public Health. 2023;23(1):201. doi:10.1186/s12889-023-14982-8
28. Amusa Y, Ijadunola I, Onayade O. Epidemiology of Otitis media in a local tropical African population. West Afr J Med. 2006;24(3). doi:10.4314/wajm.v24i3.28202
29. Choffor‐Nchinda E, Bola Siafa A, Nansseu JR. Otitis media with effusion in Africa‐prevalence and associated factors: a systematic review and meta‐analysis. Laryngoscope Investig Otolaryngol. 2020;5(6):1205–1216. doi:10.1002/lio2.502
30. Danishyar A, Ashurst JV. Acute Otitis Media. Treasure Island (FL): StatPearls Publishing; 2023.
31. Kiconco G, Turyasiima M, Ndamira A, et al. Prevalence and associated factors of pneumonia among under-fives with acute respiratory symptoms: a cross sectional study at a Teaching Hospital in Bushenyi District, Western Uganda. Afr Health Sci. 2021;21(4):1701–1710. doi:10.4314/ahs.v21i4.25
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
