Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 15
Predictors of Failure in Ultrasound-Guided Hydrostatic Reduction of Intussusception in Children: Retrospective Analysis in a Specialized Center in Ethiopia
Authors Wondemagegnehu BD , Kerego EN, Mammo TN, Robele AT, Gebru FT, Aklilu WK
Received 26 November 2023
Accepted for publication 8 February 2024
Published 19 February 2024 Volume 2024:15 Pages 87—94
DOI https://doi.org/10.2147/PHMT.S451832
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Belachew Dejene Wondemagegnehu,1 Ephrem Nidaw Kerego,2 Tihtina Negussie Mammo,1 Amezene Tadesse Robele,1 Fisseha Temesgen Gebru,1 Woubedel Kiflu Aklilu1
1Department of Surgery, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 2Department of Surgery, St. Paul’s Millennium Medical College, Addis Ababa, Ethiopia
Correspondence: Belachew Dejene Wondemagegnehu, Lideta Sub City Churchill Road, Zambia St, Addis Ababa, 26038, Ethiopia, Email [email protected]
Purpose: To identify factors predicting the failure of ultrasound-guided hydrostatic reduction of intussusception in children.
Patients and Methods: The medical records of 174 children who underwent ultrasound-guided hydrostatic reduction of intussusception over four years were reviewed at Tikur Anbessa Specialized Hospital. Patient’s demography, clinical data, and sonography findings (type of intussusception, length of intussusception, presence of lead point, trapped fluid, lymph node, and free peritoneal fluid) were entered into SPSS 25 (IBM) and analyzed using logistic regression.
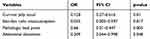
Results: The overall success rate of ultrasound-guided hydrostatic reduction was 81.6%. The sex, presence of abdominal cramps, vomiting, diarrhea, trapped lymph nodes on ultrasound, or history of upper respiratory tract infection had no association with hydrostatic reducibility. Currant jelly stool (OR 0.128; 95% CI, 0.27– 0.616; P=0.01), Ileo-ileo colic intussusception (OR 0.055; 95% CI, 0.005– 0.597; P=0.017), pathologic lead point (OR 0.66; 95% CI, 0.01– 0.447; P=0.005) and abdominal distention (OR 0.209; 95% CI, 0.044– 0.998; P=0.048) showed significant association with failed hydrostatic reduction.
Conclusion: The presence of currant jelly stool, ileo-ileo colic type intussusception, pathologic lead point, and abdominal distention are the most important predictors for failed ultrasound ultrasound-guided reduction intussusception in children.
Plain Language Summary: Intussusception occurs when an upper part of the bowel invaginate into the lower adjacent segment. Usually, the small intestine slides into the wider large intestine. It is the common cause of gut obstruction in children below 3 years of age. It occurs in 2 out of 1000 children, and the cause is not known in 95% of the cases.
Most of the children are treated without surgery. If left untreated may complicate life-threatening conditions. The non-surgical management is feasible in a child who is not critical. It is achieved by putting air or suitable fluids under pressure through a tube to the rectum. The fluid in the rectum flows to the intestine creating a pressure that pushes back the invaginated intestine to its normal position. The reduction is followed by an ultrasound of the belly. Currently, this technique is widely practiced with reasonable success rates.
In some children, the reduction with this technique may fail due to different conditions. So, our study was aimed at identifying the possible factors that are responsible for the failure of reduction. The success rate of reduction during our study period was 81.6% (144/176). This study has identified that in children with blood-mixed mucous in stool during illness, the Presence of belly distention, and the presence of known causes of intussusception detected by ultrasound during the examination of the child significantly contributed to failure of non-surgical reduction.
Keywords: pediatric intestinal obstruction, idiopathic intussusception, pediatric ultrasound, saline enema
Introduction
Intussusception is one of the most frequent causes of bowel obstruction in infants and toddlers. Intussusception occurs when a proximal bowel telescopes into the distal bowel. This condition happens at a rate of 1 to 4 in 2000 infants and children. In most series, there are reports of higher male proportion with seasonal variation and 90% of the cases are children within 3 years of age.1 The most common type of intussusception is idiopathic which accounts for 95% of the cases and about 4% of cases are secondary to pathologic lead points. A rare variant of postoperative intussusception most often occurs in the small bowel after prolonged laparotomy with excessive bowel manipulation.1
Children with idiopathic intussusception are usually healthy and well-nourished. The classic presenting signs and symptoms are crampy abdominal pain, abdominal mass, and passage of “currant Jelly” stool. The main investigative modality is abdominal ultrasound which requires patience, skill, and accurate interpretation of findings. Given these conditions, sonography is a reliable aid to the clinical diagnosis of intussusception. The diagnostic accuracy can reach up to 100% with experienced hands.2 There are also added advantages of being radiation-free and the capacity to be used in the management of intussusception.
The two most used methods of management of intussusception are operative and non-operative management. Non-operative management is only feasible in a child who is hemodynamically stable without signs of peritonitis or bowel perforation. Techniques of non-operative reduction of intussusception in children are barium enema or pressurized air enema done under fluoroscopy, and UltraSound-Guided Hydrostatic Reduction (USGHR). The reported success rate of non-operative reduction in different literature ranges from 46% to 94%. There has been a general shift toward the non-operative management of intussusception in the past few decades, currently, most pediatric intussusceptions are being managed with non-operative techniques with higher efficacy. In a meta-analysis done by Amuddhu et al there was no statistical difference in the overall recurrence rate between successfully reduced intussusceptions in children managed at inpatients and Emergency Department (ED) patients (8.8% Vs 10.1%). They concluded management of intussusception in the ED after uncomplicated reduction appears acceptable.3 Though can be done in an awake child without any form of sedation in setups with limitations of resources, there is evidence showing the use of sedation while performing enema reduction of intussusception is safe and can even increase the success rate.4,5
According to Kelley Quon et al, in hemodynamically stable children without critical illness, pre-reduction antibiotics are unnecessary, and repeated attempts can be done when clinically appropriate.6 A 96.77% success rate of a randomized controlled trial conducted by Xiaolong Xie et al and 20 years of experience from France by Flaum indicated the safety of the procedure in children with uncomplicated intussusception with a low complication rate.7,8 Ogundoyin et al from southwest Nigeria reported a 58% success rate and Y. Mensah, Glover Addy et al from Ghana showed a success rate of 75% with a hydrostatic reduction.9,10 In an Ethiopian single-center study by Wakjira et al, the success rate for hydrostatic reduction was 87.2%, but the mainstay of management in most centers in Ethiopia was operative reduction.11,12
Though there is a higher rate of failure of hydrostatic reduction in sub-Saharan Africa, literature describing the risk factors for failure is lacking, also there are few papers available internationally. Kim et al conducted a systemic review and meta-analysis reviewing 38 studies and found that fever, vomiting, and Sonography findings of left-sided intussusception, rectal bleeding, trapped fluid, and ascites were associated with a failed reduction.13 Nianam et al from China had similar findings.14
There is a paucity of research done locally and internationally that specifically tries to assess the predictors for failure of hydrostatic reduction. There is no uniform guideline followed in performing USGHR and the number of attempts is also not well described in the literature. There is no known regional literature describing factors associated with failed USGHR of intussusception in children. This research will try to address this knowledge gap and try to determine the factors associated with failed USGHR which can be used as input for the development of guidelines and further recommendations based on the results of the study.
Materials and Methods
Study Setting and Design
It is a retrospective cross-sectional institution-based study conducted on all cases of pediatric acute intussusception managed by ultrasound-guided hydrostatic reduction from May 2018 to July 2022. At Tikur Anbesa Specialized Teaching Hospital where full-time pediatric surgical services are given to children by Pediatric Surgery residents, Fellows, and Consultants and is a high pediatric surgery load center with more than 1500 procedures performed yearly.
Source Population
All pediatric intussusception cases seen at Tikur Anbessa Specialized Hospital during the study period were included.
Study Population
All pediatrics intussusception cases for which ultrasound-guided hydrostatic reduction was done during the study period and who met inclusion criteria.
Inclusion Criteria
All pediatric patients who were diagnosed to have acute intussusception and managed by ultrasound-guided hydrostatic reduction during the study period.
Exclusion Criteria
Lost patient charts, incomplete patient data, those patients with intussusception who were directly managed surgically without an attempt of ultrasound-guided hydrostatic reduction because of anticipated or proven clinical and radiologic contraindications.
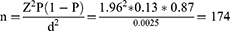
Sample Size Determination
In a study conducted previously at Tikur Anbessa Specialized Hospital, the success rate following hydrostatic reduction was 87.2%. Using this research, a failure rate of 13% was used as the proportion for the calculation of sample size in our study. Based on the calculation indicated below, we set out to collect 174 data (cards) and we collected all available cards of pediatrics patients for whom hydrostatic reduction was attempted and met inclusion criteria in the study period.
CI = 95% confidence interval, P value = 0.13, Z score = 1.96, 5% margin of error
Measurement/Variables
Dependent Variable
The outcome of ultrasound-guided hydrostatic reduction of intussusception in children.
Independent Variable
Age, sex, duration of symptom, presence of vomiting, bloody diarrhea, abdominal cramps, finding of abdominal mass, palpable mass in the rectum, record of fever, number of hydrostatic reduction attempts, and ultrasound findings: the type of intussusception, presence of pathologic lead point, length of intussusception, trapped fluid in the intussusception, presence of free peritoneal fluid also trapped lymph nodes in the intussusception.
Data Management
Epidemiologic, clinical, and sonographic data were collected from each patient’s card. The tool was used to collect information on the patient’s demographic, clinical, and radiologic findings as well as the success of ultrasound-guided hydrostatic Reduction intussusception. The data were entered into MS Excel curated and then transcribed to IBM SPSS Statistics 25 software for detailed analysis. The failed reduction was defined as those cases who failed to have a complete reduction on guiding ultrasound after three or more attempts that lasted 5–10 minutes and were treated surgically.
Data Analysis
Data were analyzed using IBM SPSS Statistics 25. Descriptive statistics of the independent variables were done, and correlation was identified. Binary logistic regression analysis was done to identify the risk factors associated with failed hydrostatic reduction. The relationship between the clinical data and abdominal ultrasound findings with the outcome of ultrasound-guided hydrostatic reduction was analyzed. The P values were determined using paired comparisons of the chi-square test. A value of p < 0.05 was considered statistically significant, and the results were presented using text, tables, and a figure.
Results
Demographic Data
The study included a total of 174 cases of Ultra Sound Guided Hydrostatic Reduction performed at the emergency department. None of the successful cases were admitted to the pediatric ward. Operative reduction was performed on those cases where the hydrostatic reduction was not successful after repeated attempts of reduction or the vascularity of the bowel became questionable on the Doppler probe. The minimum age at USGHR was three months and the oldest child was eight years old with a median age of 21 months. Eighty-two percent of the USGHR was performed in children less than 3 years of age. Boys accounted for 98 (56.3%) cases and girls 76 cases (43.7%). Most of the cases (77%) were from Addis Ababa city indicating that most intussusceptions in children are not referrals from far away corners of the country.
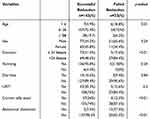
Clinical Parameters
The mean duration of symptoms is 2.41 days ranging from 1 to 14 days with the most common symptom being abdominal cramps in 172(98.8%) and the second most common symptom was vomiting accounting for 96.6% of cases. Currant jelly type of stool was reported in 65 children (37.4%). At the time of arrival, only 16% of children had a fever, and 22.4% of them were found to have a recent history of URTI. On physical examination, a sausage-shaped abdominal mass was detected in 34 children (19.5%), and abdominal distention was found in 9.8% of children. On rectal digital examination, only 7.5% of them had palpable mass felt on the examining finger. The classic finding of abdominal cramps, currant jelly stool, and palpable abdominal mass was found in only 16 (9.2%) of cases (Table 1).
Pre-Hydrostatic Reduction Ultrasound Findings
Abdominal sonography was performed for each patient before any attempt at hydrostatic reduction. The most common type was ileocolic intussusception (87.4%) followed by Colo-colic intussusception (5.75%). There were six cases of ileo-Colo-colic and ileo-ileo-colic intussusception each accounting for 3.45% of cases. Pathologic lead point was detected in nine children (5.2%). The transverse colon was the closest location for the intussusceptum reached, accounting for almost half of the locations (47.47%). Trapped lymph node was detected in more than half of the cases (54.6%) and trapped fluid was found in 21.8%. Free peritoneal fluid was seen in 21.8% of the cases. The mean length of intussusception on sonography was 5.23 cm on the longitudinal axis. The success rate of hydrostatic reduction during the study period was 81.6% (144) and the rest 18.4% underwent operative management after failed attempts at hydrostatic reduction. The success rate of USGHR of intussusception was noticed to drop with an increased number of attempts at reduction (Figure 1).
 |
Figure 1 The success rate of each attempt in Ultrasound-guided hydrostatic reduction of intussusception in children. |
Association of Clinical Data and Ultrasound Findings with the Outcome of USGHR
The relationship between the clinical data and abdominal ultrasound findings with the outcome of USGHR was analyzed. The p-values were determined using paired comparisons using the chi-square test. ρ <0.05 was used to determine a significant association. The sex of the patient, abdominal cramp, vomiting, diarrhea, trapped lymph node on ultrasound, and history of URTI did not show a significant association ρ >0.05. Presence of Abdominal distension and the type of intussusception showed a statistically significant association with P <0.01 (Table 2).
Risk Factors Associated with Failed USGHR
Binary logistic regression was used to identify the independent risk factors associated with failed hydrostatic reduction of intussusception. Our analysis showed the presence of clinical findings of currant jelly stool and abdominal distension showed a significant association (ρ <0.05). Sonographic findings of pathologic lead point and ileocolic intussusception were independent risk factors (ρ<0.05) associated with failed USGHR as shown in (Table 3).
Discussion
Since the introduction of the reduction of intussusception by warm saline using real-time sonography guidance in 1982 by Kim et al USGHR has enjoyed major popularity.15 The lack of radiation exposure has made this method of reduction a favorable management option for children with intussusception. Since 2013 USGHR has been used as the first line of management of intussusception in children at Tikur Anbessa Specialized Hospital. All children with intussusception who presented without any sign of peritonitis or bowel perforation are managed non-operatively. The introduction of USGHR has resulted in rewarding results. Our study used a total of 174 samples and used logistic regression to find clinical and sonographic factors associated with the failure of USGHR.
The success rate of USGHR in our study spanning over 4 years is 81.6%. This result is comparable with previously done research on our setup which showed a success rate of 87.2%.11 In this study, symptoms lasting for four days or more were directly operated on and were not managed by hydrostatic reduction. This may be partly the reason for the modest decrement in the success rate despite more experience gained in the past few years. A systemic review and meta-analysis done by Kim et al over 20 years comprising 40,133 cases showed a similar rate of 82% and results are consistently higher than other sub-Saharan Africa reports which showed a success rate of 58% in Nigeria and 75% in Ghana.9,10,13
The median age of presentation is 24 months with 82% under 3 years of age and male predominance implicating more than half of USGHR performed were boys. All these findings are consistent with most reports on pediatric intussusception.1 The classic triads of abdominal cramp, abdominal mass, and currant jelly stool are reported in up to 30% of cases in most literature.1 In our research, this finding was found only in 9.2% which was much lower than others but higher than a report by Li, Y.16 The incidence of intussusception secondary to a pathologic lead point was 5.2% matching with other literature reporting ranges from 1.5% to 12%.1 Like in similar studies by Xiaolong et al,17 age at presentation and duration of symptoms were associated with decreased success rate on chi-square paired-wise comparison but were not statistically significant (P > 0.05) on binary logistic regression analysis. Prolonged duration >12 hours in the Katz et al study and >24 hours in Fike et al studies were associated with decreased reducibility.18,19 On the contrary, some papers did not find the duration of symptoms as a relevant factor in the failure of reduction.14,20 Our research identified currant jelly stool as a risk factor for failed USGHR (P<0.05) in logistic regression analysis. Other researchers also found bloody stool as a significantly poor prognostic factor.14,19 The site of intussusception was a statistically significant factor in reducing the success of hydrostatic reduction in some literature. Nianan et al found intussusception on the left side of the abdomen had a lower rate of success (P<0.05).14 Fike et al also identified the colonic extent of intussusception as having a statistically significant (P<0.01) association.19 We were able to identify a correlation on the chi-square test but no significant association was drawn with logistic regression analysis.
Abdominal distention showed a statistically significant reduction in the success rate of intussusception (P<0.05). Gross abdominal distention signifies significant bowel obstruction and is possibly caused by the late presentation. Having abdominal distention at presentation, therefore, was a significant factor that resulted in a decreased rate of reduction with USGHR. Trapped fluid and free peritoneal fluid on sonographic examination were not significant independent risk factors in our study (P>0.05). In research conducted by Nianan et al, these two factors were significant in lowering the success rate (P<0.05).14 Crystal et al found the presence of trapped fluid (P<0.02) to significantly lower the success rate while free peritoneal fluid was found to be not the predictor of outcome (P>0.1).21 The presence of a pathologic lead point suspected on ultrasound significantly reduced the success rate (P<0.05). Ileo-ileo colic type of intussusception was found to be a statistically significant risk factor in logistic regression analysis (P<0.05). To our knowledge, there are no papers that specifically try to correlate such different types of compound intussusceptions and their implication in reducibility on USGHR. The overall findings of the risk factors for failure of USGHR of intussusception in children in this study were comparable to similar studies or failures in other non-operative management options.22,23
The retrospective nature of the research can be considered as one limitation. The procedure at our setup is performed by a senior pediatric surgery resident or fellow accompanied by a radiology resident and with or without any sedation. In some difficult cases experienced pediatric radiologists were involved. However, the research design did not take the level of experience and whether done under sedation or not into consideration which might be a reason for the reduced success rate. This can be considered another limitation of this study.
Conclusion
The research has identified the presentation of a child with currant jelly stool, abdominal distention, the presence of an ileo-ileo-colic type of intussusception, and pathologic lead point are statistically significant predictors of failure of hydrostatic reduction. Though Ultrasound-guided hydrostatic reduction is an efficient and safe way of non-operative means of reducing intussusception in children, the presence of any one or more of the identified risk factors should raise the possibility of failed hydrostatic reduction. The significant drop in success rate after repeated attempts of hydrostatic reduction implies that repeated attempts should be exercised with caution.
Data Sharing Statement
The data used during the study are available from the corresponding.
Ethics Approval and Informed Consent
All methods were carried out per the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments for which reason. The study approval was obtained from the institutional review board of Addis Ababa University College of Health Sciences School of Medicine. Because of the retrospective nature of the study, the need for consent to participate was waived by the same committee and patient data confidentiality was maintained throughout the study.
Acknowledgments
We would like to thank the administrators of the College and the hospital staff for allowing us to access the patients’ charts. We would like to extend our thanks to Pediatric Surgery and Radiology residents for helping us to collect a list of patients from the operation registry books and more importantly to Patient Record Office workers for their genuine effort during patient chart searching.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published on the Pediatric Health, Medicine and Therapeutics; and agree to be accountable for all aspects of the work.
Funding
The authors receive no financial support for any gain.
Disclosure
The authors declare that the research was conducted in the absence of any conflicts of interest.
References
1. Columbari PM. Intussusception. In: Coran AG, editor. Pediatric Surgery.
2. Wright JE, Slater S. Suspected intussusception: is ultrasound a reliable diagnostic aid? The Australian and. New Zealand J Surg. 1996;66(10):686–687. doi:10.1111/j.1445-2197.1996.tb00718.x
3. Amuddhu SK, Chen Y, Nah SA. Inpatient admission versus emergency department management of intussusception in children: a systemic review and meta-analysis of outcomes. Eur J Pediatr Surg. 2019;29(1):7–13. doi:10.1055/s-0038-1668145
4. Eisapour A, Mehrayin R, Esmaeili-Dooki M. The effect of midazolam on decreasing the duration of intussusception hydrostatic reduction in children. Med Arch. 2015;69(5):289–292. doi:10.5455/medarh.2015.69.289-292
5. Gal M, Gamsu S, Jacob R, Cohen D, Shavit M. Reduction of ileocolic intussusception under sedation or anesthesia: a systematic review of complications. Arch Dischildhood. 2022;107(4):335–340. doi:10.1136/archdischild-2021-322706
6. Kelley-Quon LI, Arthur LG, Williams RF, et al. Management of intussusception in children: a systematic review. J Pediatr Surg. 2021;56(3):587–596. doi:10.1016/j.jpedsurg.2020.09.055
7. Xie X, Wu Y, Wang Q, Zhao Y, Chen G, Xiang B. A randomized trial of pneumatic reduction versus hydrostatic reduction for intussusception in pediatric patients. J Pediat Surg. 2015;53(8):1464–1468. doi:10.1016/j.jpedsurg.2017.08.005
8. Flaum V, Schneider A, Gomes Ferreira C, et al. Twenty years’ experience for reduction of ileocolic intussusceptions by saline enema under sonography control. J Pediat Surg. 2016;51(1):179–182. doi:10.1016/j.jpedsurg.2015.09.022
9. Ogundoyin O, Lawal T, Olulana D, Atalabi O. Experience with sonogram-guided hydrostatic reduction of intussusception in children in South-West Nigeria. J West Afr Coll Surg. 2013;3(2):76–88.
10. Mensah Y, Glover-Addy H, Etwire V, Appeadu-Mensah W, Twum M. Ultrasound-guided hydrostatic reduction of intussusception in children at Korle Bu Teaching Hospital: an initial experience. Ghana Med J. 2011;45(3):128–131.
11. Wakjira E, Sisay S, Zember J, et al. Implementing ultrasound-guided hydrostatic reduction of intussusception in a low-resource country in Sub-Saharan Africa: our initial experience in Ethiopia. Emerg Radiol. 2018;25(1):1–6. doi:10.1007/s10140-017-1546-y
12. Tadesse A, Teshager F, Weldegebriel G, et al. Epidemiology of intussusception among infants in Ethiopia. Pan Afr Med J. 2021;39(Suppl 1):2. doi:10.11604/pamj.supp.2021.39.1.21299
13. Kim PH, Hwang J, Yoon HM, et al. Predictors of failed enema reduction in children with intussusception: a systematic review and meta-analysis. Eur Radiol. 2021;31(11):8081–8097. doi:10.1007/s00330-021-07935-5
14. He N, Zhang S, Ye X, Zhu X, Zhao Z, Sui X. Risk factors associated with failed sonographically guided saline hydrostatic intussusception reduction in children. J Ultrasound Med. 2014;33(9):1669–1675. doi:10.7863/ultra.33.9.1669
15. Kim YG, Choi BI, Yeon KM, et al. Diagnosis and treatment of childhood intussusception using real-time ultra-sonography and saline enema: a preliminary report. J Korean Soc Med Ultras. 1982;1:66–70.
16. Li Y, Zhou Q, Liu C, et al. Epidemiology, clinical characteristics, and treatment of children with acute intussusception: a case series. BMC Pediatr. 2023;23:143. doi:10.1186/s12887-023-03961-y
17. Xiaolong X, Yang W, Qi W, Yi Yang Z, Bo X. Risk factors for failure of hydrostatic reduction of intussusception in pediatric patients: a retrospective study. Medicine. 2019;98(1):e13826. PMID: 30608396; PMCID: PMC6344150. doi:10.1097/MD.0000000000013826
18. Katz M, Phelan E, Carlin JB, Beasley SW. Gas enema for the reduction of intussusception: the relationship between clinical signs and symptoms and outcome. AJR Am J Roentgenol. 1993;160:363–366. doi:10.2214/ajr.160.2.8424351
19. Fike FB, Mortellaro VE, Holcomb GR, St Peter SD. Predictors of failed enema reduction in childhood intussusception. J Pediatr Surg. 2012;47:925–927. doi:10.1016/j.jpedsurg.2012.01.047
20. Tareen F, Ryan S, Avanzini S, Pena V, McLaughlin D, Puri P. Does the length of the history influence the outcome of pneumatic reduction of intussusception in children? Pediatr Surg Int. 2011;27:587–589. doi:10.1007/s00383-010-2836-6
21. Crystal P, Hertzanu Y, Farber B, Shabshin N, Barki Y. Sonographically guided hydrostatic reduction of intussusception in children. J Clin Ultras. 2002;30(6):343–348. doi:10.1002/jcu.10085
22. Issa K, Ali W, AL-Abbas B. Factors associated with success of sonographically guided hydrostatic reduction of ileocolic intussusception in children. SN Compr Clin Med. 2021;3:242–246. doi:10.1007/s42399-021-00731-8
23. Khorana J, Singhavejsakul J, Ukarapol N, Laohapensang M, Siriwongmongkol J, Patumanond J. Prognostic indicators for failed nonsurgical reduction of intussusception. Therapeut Clin Risk Manag. 2016;12:1231–1237. doi:10.2147/TCRM.S109785
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.