Back to Journals » Transplant Research and Risk Management » Volume 14
Predictive Value of Abnormal Hemodynamic Response to Dobutamine Stress Echocardiography in Liver Transplant Recipients
Authors Peotter AM, Hammel LL, Groose MK
Received 8 September 2021
Accepted for publication 8 December 2021
Published 6 January 2022 Volume 2022:14 Pages 1—6
DOI https://doi.org/10.2147/TRRM.S337542
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Qing Yi
Ashley M Peotter,1 Laura L Hammel,2 Molly K Groose2
1University of Wisconsin School of Medicine and Public Health, Madison, WI, USA; 2Department of Anesthesiology, University of Wisconsin Hospital, Madison, WI, USA
Correspondence: Molly K Groose Email [email protected]
Background: Dobutamine stress echocardiography (DSE) is an effective tool for perioperative cardiac risk stratification in patients without end-stage liver disease (ESLD). However, DSE is frequently used in cardiac risk stratification in patients with ESLD despite its documented lower sensitivity. We investigated whether abnormal hemodynamic response to DSE could improve the sensitivity of the test in this patient population.
Methods: A retrospective chart review of all patients who underwent DSE prior to orthotopic liver transplantation (OLT) at the University of Wisconsin Hospital from 2009 to 2018 was performed to determine if hypotension, hypertension, and/or inability to achieve 85% maximum predicted heart rate (MPHR) during the test were associated with major adverse cardiac events (MACE). Data were analyzed with conventional bivariate tests and logistic regression.
Results: A total of 412 patients were included in analysis with 68.5% male and 31.5% female with a median age at transplant of 57.4 (51.3– 61.9). Etiologies for liver disease included 43% alcoholic, 18% non-alcoholic fatty liver disease, 14% autoimmune, 10% hepatitis C, and 7.5% for both malignancy and other causes. The incidence of MACE was 27.3%. There was no correlation between a hypotensive response (p = 0.52) or an inability to obtain 85% MPHR (p = 0.28) and MACE. There was a trend toward significance with hypertensive response (p = 0.06) including a significant correlation between increasing systolic blood pressure and the incidence of MACE (p = 0.01).
Conclusion: Hypotensive response or inability to achieve 85% MPHR on DSE does not appear to predict MACE in this patient population, though hypertensive response may. Future prospective studies will be needed to further investigate these findings.
Keywords: post-operative, cardiac, hemodynamic, morbidity, allocation
Introduction
While associated with high morbidity and mortality, end-stage liver disease (ESLD) can be completely cured with orthotopic liver transplantation (OLT). OLT improves survival and reduces the burden of symptoms, but there is a significant risk of adverse cardiovascular events associated with the operation. Nationally, the incidence of ESLD is steadily increasing and the number of patients on the liver transplant waiting list well exceeds the number of organs available.1 Given the scarcity of this resource, improving recipient outcomes and graft survival is crucial.
It was historically believed that coronary artery disease (CAD) incidence was lower in patients with ESLD than the general population. However, recent studies have estimated a prevalence of 27% compared to 2.5% in the healthy population which may be in part due to the increasing frequency of non-alcoholic steatohepatitis as an indication for OLT.2,3 Also, patients with documented CAD who undergo OLT have worse outcomes than patients without CAD. One study estimated a 1-year mortality at 50% in patients with CAD.4 Another study found 22% of patients with preoperative CAD experienced death from cardiovascular causes within 5 years of transplantation.5 Thus, screening and detection of CAD before determining OLT candidacy is of utmost importance.
However, the physiological changes associated with ESLD lead to challenges when screening for CAD. The chronic vasodilatory state associated with ESLD dramatically decreases the sensitivity of myocardial perfusion scintigraphy.6 Additionally, many patients are deconditioned and frail – with muscle wasting and large volumes of ascites or symptoms of hepatic encephalopathy – preventing exercise stress testing as an option for patients who may be physically unable to walk on a treadmill. Thus, dobutamine stress echocardiography (DSE) is often used as an initial screening test.7
Despite the frequent use of DSE, it is known to have a reduced predictive value and accuracy in the ESLD population. A meta-analysis found that DSE had a sensitivity of 0.20 and positive predictive value of 0.33 for predicting perioperative major adverse cardiac events (MACE) in ESLD patients.8 In an attempt to increase the sensitivity and specificity of DSE, others have investigated the predictive value of abnormal hemodynamic response to DSE. One study in non-ESLD patients found that hypotension during DSE was predictive of perioperative cardiac mortality, myocardial infarction, and ischemia.9 Conversely, another study in non-ESLD patients found that a hypotensive response during DSE was not associated with increased risk but that a hypertensive response increased the likelihood of a positive DSE and CAD.10 Lastly, it is unknown if patients who do not obtain 85% maximum predicted heart rate (MPHR) on DSE, potentially indicating chronotropic incompetence, are at increased risk of MACE.
With this in mind, we aimed to determine if abnormal hemodynamic response, specifically hypertension, hypotension, or the inability to achieve MPHR during DSE was associated with perioperative or postoperative MACE in patients undergoing OLT to aid in decision-making and risk stratification when determining OLT candidacy.
Materials and Methods
Patient Population
All adult patients who underwent preoperative DSE prior to OLT at the University of Wisconsin Hospital from January 2009 to May 2018 were eligible for inclusion in this study. Patients younger than 18 years of age were excluded. The patient population information was identified from the University of Wisconsin Transplant Surgery Department’s Solid Organ Transplant Database.
Identification of Patients with Pre-Operative DSE
Per our institution’s pre-transplant screening protocol, patients deemed to be of intermediate risk for coronary artery disease undergo non-invasive stress testing, usually DSE, whereas low risk patients do not undergo ischemic evaluation and high-risk patients proceed directly with coronary angiography. The electronic medical record for each patient undergoing OLT during the specified time frame was reviewed in HealthLink, the Epic Systems electronic medical record used at our institution (Epic Systems Corporation, Verona, WI). Presence of a legible DSE report in HealthLink with a date of service prior to the patient’s OLT date of service was necessary for study inclusion. The DSE reports from outside institutions that were scanned into the medical record were included if they fit the above criteria.
Data Collection
Data were obtained from electronic medical records and the University of Wisconsin Transplant Surgery Department’s Solid Organ Transplant Database. Along with identifying patients with preoperative DSE, additional patient data were extracted including: institution that completed the DSE, etiology of ESLD, patient age, baseline heart rate, baseline blood pressure, and baseline ECG, peak heart rate, MPHR, calculated 85% MPHR, percent MPHR achieved, blood pressure at peak stress, presence of arrhythmias during stress, presence of ST-T wave changes during stress, and ischemic response to stress.
Presence of MACE was determined from diagnosis codes from the patient’s hospital discharge summary that had been previously uploaded into the University of Wisconsin Transplant Surgery Department’s Solid Organ Transplant Database. MACE diagnosis codes were grouped into four categories: cardiac arrest, myocardial infarction, heart failure and arrhythmia.
Data Analysis
The data were analyzed based on the three categories of a hypertensive response, hypotensive response, and an inability to obtain 85% MPHR. The MPHR was determined based on the patient’s age at the time of the DSE and calculated using the predefined equation  . Previously published definitions of hypotensive and hypertensive responses to DSE were utilized. A hypotensive response was defined as a decrease in systolic blood pressure of ≥20 mmHg from the peak pressure during the infusion protocol or an absolute systolic blood pressure ≤80 mmHg.9 A hypertensive response was defined as a systolic blood pressure of ≥180 mmHg.10 All statistical analyses were completed in R (version 3.6.3). The number and percentage of patients with each DSE response were reported. An odd ratio (MACE/No MACE) was calculated for each DSE response category. A two-tailed Fisher Exact test was utilized to compare the groups of heart rate responses. Fisher Exact testing was also used to compare blood pressure changes during DSE as well, with the normotensive response serving as the reference to hypo/hypertensive response. Results were reported as p-values. Lastly, a two-tailed logistic regression was used to model the incidence of any MACE event. Regression inputs included those that failed to reach 85% of MPHR, hypotensive response, and hypertensive response following DSE. An additional logistic regression model was completed with MACE as a function of maximum systolic blood pressure (for all systolic blood pressures above 120 mmHg). Results reported as odds ratio (MACE/No MACE), 95% confidence interval, and p-value. A priori significance level was set to p < 0.05.
. Previously published definitions of hypotensive and hypertensive responses to DSE were utilized. A hypotensive response was defined as a decrease in systolic blood pressure of ≥20 mmHg from the peak pressure during the infusion protocol or an absolute systolic blood pressure ≤80 mmHg.9 A hypertensive response was defined as a systolic blood pressure of ≥180 mmHg.10 All statistical analyses were completed in R (version 3.6.3). The number and percentage of patients with each DSE response were reported. An odd ratio (MACE/No MACE) was calculated for each DSE response category. A two-tailed Fisher Exact test was utilized to compare the groups of heart rate responses. Fisher Exact testing was also used to compare blood pressure changes during DSE as well, with the normotensive response serving as the reference to hypo/hypertensive response. Results were reported as p-values. Lastly, a two-tailed logistic regression was used to model the incidence of any MACE event. Regression inputs included those that failed to reach 85% of MPHR, hypotensive response, and hypertensive response following DSE. An additional logistic regression model was completed with MACE as a function of maximum systolic blood pressure (for all systolic blood pressures above 120 mmHg). Results reported as odds ratio (MACE/No MACE), 95% confidence interval, and p-value. A priori significance level was set to p < 0.05.
Ethical Considerations and IRB Approval
This study was approved by the University of Wisconsin institutional review board and the University of Wisconsin Hospital Transplant Surgery Department’s Publication and Clinical Research Services Committee (study number 2014-1070). Patient consent was not required for record review in accordance with the University of Wisconsin institutional review board policy. After collection, all data was deidentified and stored in a password-protected, secure database in accordance with the Declaration of Helsinki. All organs were donated voluntarily with documented informed consent in accordance with the Declaration of Istanbul.
Results
There were 412 patients included in this study with baseline characteristics described in Table 1. The etiology of liver disease in this population included 43% from alcoholic liver disease, 18% from non-alcoholic fatty liver disease, 14% from autoimmune liver disease, 10% from hepatitis C, 7.5% from malignancy, and 7.5% from other causes not previously mentioned (Table 1). Of the 412 total patients, 108 experienced at least one MACE during their post-transplant hospital admission with 29.6% experiencing a myocardial infarction, 59.3% arrhythmia, 18.5% cardiac arrest, and 19.4% heart failure. Of the 59.3% who experienced arrhythmia, 77.6% experienced atrial fibrillation alone, 7.5% experienced atrial fibrillation plus another arrhythmia, and 14.9% experienced an arrhythmia other than atrial fibrillation. The number of MACE experienced by each patient varied, with 75.9% experiencing one event, 22.3% experiencing two events and 1.8% experiencing three events (Table 1).
 |
Table 1 Demographic Data |
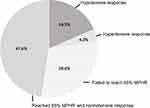
Within this study, the responses to preoperative DSE in ESLD patients included 18.5% (n = 73) with a hypotensive response, 4.3% (n = 17) with a hypertensive response, and 29.6% (n = 117) who failed to reach 85% MPHR (Figure 1). The odds ratio (MACE/No MACE) was <1 for all three response categories. Additionally, Fisher Exact testing demonstrated non-significance for all three responses (<85% MPHR: p = 0.39; hypotensive: p = 0.46; hypertensive: p = 0.09; Table 2). A multivariable analysis predicting MACE from the three risk categories of hypotension, hypertension, and 85% MPHR demonstrated insufficient evidence for direct correlation (p = 0.52, p = 0.06, p = 0.28, respectively). On additional logistic modeling, when MACE was considered as a function of maximum systolic blood pressure, there was a statistically significant association between increasing blood pressure and the incidence of MACE (p = 0.01). With this model, the odds ratio for a 10 mmHg increase in systolic blood pressure was 1.19, 95% CI [1.04 to 1.37]. This relationship is equivalent to a doubled odds of MACE at 160mmHg systolic blood pressure relative to normal (4 × 10 mmHg above 120 mmHg, 1.194 = 2.0; Table 3).
 |
Table 2 Univariate Analysis |
 |
Table 3 Multivariable Analysis |
Discussion
Major adverse cardiac events occurred frequently in our study population with approximately 1 in 4 patients experiencing MACE during their hospital stay for OLT. This rate is in line with previously published rates11–13 despite the patients in our study having what was interpreted to be a normal or low-risk DSE preoperatively. This is in part explained by the highly morbid nature of the surgical procedure itself with its associated hemodynamic instability and often large volume blood loss and thus, inherent cardiac risk. Additionally, this can be explained by previously published data indicating DSE has lower sensitivity in the ESLD population compared to the non-ESLD population.8
In one such study, 633 patients underwent coronary angiography within six months of DSE. The authors concluded the sensitivity of a positive DSE for determining CAD was 24% and specificity was 90%.14 A second study found the positive predictive value of a positive DSE for predicting MACE post-operatively in ESLD patients undergoing OLT was 6.7% and with a negative predictive value of 83.5%. When considering the later study, only 13% of patients had a positive DSE which is not an isolated occurrence.15 Additionally, this information highlights the high-risk nature of liver transplantation which can sometimes be overlooked by practitioners not intimately involved in liver transplantation. Despite patients undergoing cardiac evaluation preoperatively, there is an inherent cardiac risk with the procedure itself. While preoperative cardiac testing can improve identification of those at risk, it will not completely eliminate the risk.
Interestingly, in our study, there was no correlation between hypotension or the inability to achieve 85% MPHR on DSE and MACE rates in our patient population. While it has been shown in non-ESLD populations that a DSE indicating chronotropic incompetence or, more broadly, the inability of the heart to respond and augment appropriately in the face of major stress, increased MACE rates.9 It is unclear why there was no such association found in our study. It is plausible that the low systemic vascular resistance and high cardiac output state associated with ESLD increases the rates of hypotension and inability to achieve MPHR on DSE but does not, in fact, increase the rate of MACE. Additionally, this may also be explained by beta-blocker therapy. As evidence mounts showing improved outcomes in patients with ESLD with initiation of beta-blocker therapy16,17 more patients are likely taking oral beta-blockers prior to undergoing their pre-listing cardiac testing. It would seem plausible that a patient taking a beta-blocker would be more likely to have a hypotensive response or inability to achieve 85% MPHR. However, given the retrospective nature of our study, it is not possible to determine if patients that were on beta-blockers had them held prior to DSE, posing a significant limitation to this study. Beta-blocker therapy may explain hypotension or inability to achieve MPHR on DSE but no increased risk of MACE compared to patients who were not hypotensive and who achieved 85% MPHR.
While hypotension or inability to achieve 85% MPHR were not associated with increased risk of MACE, there was a trend toward significance in patients with a truly hypertensive response on DSE (SBP > 180 mmHg) being more likely to experience MACE. More specifically, for systolic blood pressures starting at 120mmHg, there is a two-fold increase in incidence of MACE for every additional 40mmHg increase during stress. This finding mirrors previously published findings in non-ESLD patients.10 Average MELD score was lower in the hypertensive group compared to the average MELD score of patients who did not have a hypertensive response (25.1, 26.2, respectively) though not statistically significant due to small sample size. This group’s lower MELD scores may explain why this patient population behaves more similarly to non-ESLD patients. These results should be interpreted with caution due to the small sample size, and therefore, the clinical significance of a hypertensive response to DSE can be further explored.
This study certainly has limitations with one such being the retrospective study design. Additionally, diagnosis codes from discharge summaries may be missing or incomplete, particularly in patients with post-operative complications leading to long hospitalizations. To ensure this was not a significant bias, 20 charts with no MACE-related diagnosis codes were randomly selected and thoroughly evaluated. In these 20 charts, there was no evidence of myocardial infarction, heart failure, arrhythmia, or cardiac arrest during surgery or at any point during their post-operative stay. Additionally, our calculated MACE rates were similar to previously published studies adding to validity of our data. Of these MACE incidents, all arrhythmia events occurred during the hospitalization. Unfortunately, it is unknown how many of these events required hospital discharge follow-up or persisted in the long-term, post-transplant course. It should also be noted that atrial fibrillation was the most common arrhythmia reported and made up 77.6% of arrhythmia diagnosis codes. As atrial fibrillation is not classically a marker for ischemia this may have limited our findings. Lastly, the DSEs included in the study came from multiple institutions with variable reliability in data reporting. For example, not all reports included whether or not atropine was administered during the test or if beta-blockers were held prior to examination. However, this does add generalizability to our study since in our regular evaluation of liver transplant candidates, we are frequently asked to utilize and interpret DSEs from institutions outside of our own.
Conclusion
Candidacy for liver transplantation is determined by evaluation of the entirety of the patient which includes cardiovascular risk stratification—oftentimes determined by the results of a pre-listing DSE. Despite the well-published lower sensitivity of DSE in this patient population, it is oftentimes the solitary testing modality used to evaluate the patient for perioperative risk of ischemia. Our study emphasizes that what is read as a normal or low-risk DSE does not insulate the patient from perioperative cardiac complications. Patients with a hypertensive response may benefit from additional, more invasive, risk stratification as they may be more likely to experience MACE peri- or post-operatively. Further investigation including prospective studies with larger cohorts would be needed confirm or refute these findings.
Abbreviations
BMI, body mass index; CAD, coronary artery disease; DSE, dobutamine stress echocardiogram/echocardiography; ESLD, end-stage liver disease; MACE, major adverse cardiac event; MELD, model for end-stage liver disease; MET, measure of exercise tolerance; MPHR, maximum predicted heart rate; OLT, orthotopic liver transplant.
Acknowledgments
Bryan Krause, PhD, assistant scientist and biostatistician at the Department of Anesthesiology, UW—Madison.
Funding
There is no funding to report.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. UNOS. Transplant trends. Available from: https://unos.org/data/transplant-trends.
2. Carey WD, Dumot JA, Pimentel RR, et al. The prevalence of coronary artery disease in liver transplant candidates over age 50. Transplantation. 1995;59:859–864. doi:10.1097/00007890-199503270-00010
3. Froelicher VF, Thompson AJ, Wolthuis R, et al. Angiographic findings in asymptomatic aircrewmen with electrocardiographic abnormalities. Am J Cardiol. 1977;39:32–38. doi:10.1016/S0002-9149(77)80007-6
4. Plotkin JS, Scott VL, Pinna A, Dobsch BP, De Wolf AM, Kang Y. Morbidity and mortality in patients with coronary artery disease undergoing orthotopic liver transplantation. Liver Transplant Surg. 1996;2(6):426–430. doi:10.1002/lt.500020604
5. Neuberger J. Liver Transplantation. J Hepatol. 2000;32:198–207. doi:10.1016/S0168-8278(00)80426-2
6. Bhutani S, Tobis J, Gevorgyan R, et al. Accuracy of stress myocardial perfusion imaging to diagnose coronary artery disease in end stage liver disease patients. Am J Cardiol. 2013;111:1057–1061. doi:10.1016/j.amjcard.2012.12.023
7. Martin P, DiMartini A, Feng S, Brown R, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guidelines by the AASLD and the American Society of Transplantation. Am Assoc Study Liver Dis. 2013;59:1144–1165.
8. Nguygen P, Plotkin J, Fishbein TM, et al. Dobutamine stress echocardiography in patients undergoing orthotopic liver transplantations: a pooled analysis of accuracy, perioperative and long term cardiovascular prognosis. Int J Cardiovasc Imaging. 2013;29:1741–1748. doi:10.1007/s10554-013-0275-x
9. Day SM, Younger JG, Karavite D, Bach DS, Armstrong WF, Eagle KA. Usefulness of hypotension during dobutamine echocardiography in predicting perioperative cardiac events. Am J Cardiol. 2000;85:478–483. doi:10.1016/S0002-9149(99)00775-4
10. Abram S, Arruda-Olson AM, Scott CG, et al. Frequency, predictors, and implications of abnormal blood pressure responses during dobutamine stress echocardiography. Circ Cardiovasc Imaging. 2017;10(4):e005444. doi:10.1161/CIRCIMAGING.116.005444
11. Koshy A, Farouque O, Cailes B, et al. Prediction of perioperative cardiovascular events in liver transplantation. Transplantation. 2021;105:593–601. doi:10.1097/TP.0000000000003306
12. Piazza N, Singal A. Frequency of cardiovascular events and effect on survival in liver transplant recipients for cirrhosis due to alcoholic or nonalcoholic steatohepatitis. Exp Clin Transplant. 2016;14:79–85. doi:10.6002/ect.2015.0089
13. VanWagner L, Serper M, Kang R, et al. Factors associated with major adverse cardiovascular events after liver transplantation among a national sample. Am J Transplant. 2016;16:2684–2694. doi:10.1111/ajt.13779
14. Doytchinova A, Feigenbaum T, Pondicherry-Harish R, et al. Diagnostic performance of dobutamine stress echocardiography in end stage liver disease. JACC Cardiovasc Imaging. 2019;12:2115–2122. doi:10.1016/j.jcmg.2018.10.031
15. Agrawal A, Jain D, Dias A, Jorge V, Figueredo V. Real world utility of dobutamine stress echocardiography in predicting perioperative cardiovascular morbidity and mortality after orthotopic liver transplantation. Korean Circ J. 2018;48(9):828–835. doi:10.4070/kcj.2017.0350
16. Kuo S, Lizaola B, Hayssen H, Lai J. Beta-blockers and physical frailty in patients with end-stage liver disease. World J Gastroenterol. 2018;24:3770–3775. doi:10.3748/wjg.v24.i33.3770
17. Rodrigues S, Mendoza Y, Bosch J. Beta-blockers in cirrhosis: evidence-based indications and limitations. J Hepatol. 2020;2:100063.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.