Back to Journals » Breast Cancer: Targets and Therapy » Volume 15
Popularity of Traditional Chinese Medicine Use Among Breast Cancer Patients in North China: A Cross-Sectional Study
Authors Zhao R , Zhang J, Gou Q, Gao J
Received 14 April 2023
Accepted for publication 3 August 2023
Published 10 August 2023 Volume 2023:15 Pages 577—589
DOI https://doi.org/10.2147/BCTT.S416998
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Pooja Advani
Rong Zhao,1,* Jianyong Zhang,2,* Qingxiang Gou,3 Jinnan Gao1,2
1General Surgery Department, Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences, Tongji Shanxi Hospital, Third Hospital of Shanxi Medical University, Taiyuan, People’s Republic of China; 2Third Hospital of Shanxi Medical University, Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences, Tongji Shanxi Hospital, Taiyuan, People’s Republic of China; 3School of Public Health, Shanxi Medical University, Taiyuan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jinnan Gao, General Surgery Department, Shanxi Bethune Hospital, Longcheng Street 99, Taiyuan, Shanxi, 030032, People’s Republic of China, Tel +86 15135086600, Email [email protected]
Background: The role of traditional Chinese medicine (TCM) in breast cancer treatment is controversial. The aim of this study is to explore the popularity of TCM among the breast cancer patients who have been treated with Western medicine (WM) in north China.
Methods: An observational, cross-sectional study was conducted. We consecutively recruited 691 breast cancer patients who were diagnosed in Shanxi Bethune Hospital between 1 January 2017 and 31 December 2020 and completed follow-up between June and August 2022. A self-designed questionnaire was used for data collection. Participants were asked about TCM use by phone. Univariate and multivariate analyses were performed as appropriate.
Results: At median follow-up of 41 months (range, 17– 61 months), 326 (47.2%) participants used TCM. The results of multivariate logistic regression showed that residential area, education, annual income per capita, experienced TCM treatment before, stage of diagnosis, and trust in TCM were independent predictors of TCM use. The detail of TCM use and the reason for non-TCM use were presented comprehensively.
Conclusion: The use of TCM was prevalent among breast cancer patients treated with WM in north China. If WM physician encourage the patients with higher intention to use TCM and provide them with appropriate advices, the quality of life of patients will be further improved through integrating TCM into standard adjuvant therapy.
Keywords: traditional Chinese medicine, breast cancer, cross-sectional study, China
Background
Traditional Chinese medicine dates back thousands of years. It is based on the yin–yang theory and the five elements theory, with a holistic, traditional system, and has developed from practical life of the Chinese nation.1 TCM has its special cultural style and enriched experience.2 With thousands of years of development, TCM is recognized for various diagnostic and treatment advantages for various diseases. Until the end of the nineteenth century, TCM was the only healthcare security choice for the Chinese.1 Interestingly, most Chinese doctors have only undergraduate training in Western medicine.3 This has led to Western medicine currently dominating the treatment of carcinoma in China, especially in general hospitals based on Western medicine.
Breast cancer has become the most prevalent malignant tumor globally, including in China, with the highest incidence rate.4 Progress has been achieved in treating breast cancer in the Western medicine system, with significant effects and good prognoses.5,6 Research on the occurrence and development of breast cancer has been performed at the genetic and signaling levels. The major means of breast cancer treatment include surgery, radiation, chemotherapy, targeted therapies, endocrine treatment, and immunotherapy.7 From the TCM point of view, Qi stagnation and blood stasis are the two main causes of breast cancer. Blood stasis syndrome affects most tumor patients to varying degrees. A person with breast cancer has poor emotions and stagnating liver Qi, resulting in poor blood circulation and an illness affecting the collaterals, thereby leading to blood stasis symptoms.8 Traditional Chinese medicine (TCM) treatment of breast cancer emphasizes a holistic approach and individualized care. Western medicine, on the other hand, possesses more advanced technology and evidence-based support in the treatment of breast cancer. In recent years, scholars have conducted research on the pathophysiological mechanisms of TCM in cancer treatment and have made some progress.9 Although traditional Chinese medicine and Western medicine hold different therapeutic concepts, each has its own characteristic advantages.
According to a national survey conducted in China, there were 1,030,935 health institutions in 2021, of which 77,336 were TCM-specialized health institutions, including 5715 TCM hospitals, 71,583 outpatient departments/clinics, and 38 research institutes. TCM health practitioners reached 884,000, and the total number of visits for a TCM diagnosis and treatment reached 1.2 billion.3 In other words, it is easy for the Chinese to access TCM services in China.
For breast cancer survivors treated with Western medicine treatment, what is their attitude toward TCM? Have they ever sought help from TCM treatment? Did TCM address their matter? Therefore, we carried out this study to address these questions.
Method
Study Population
With Institutional Review Board approval, we identified all breast cancer patients who were diagnosed pathologically for the first time at Shanxi Bethune Hospital between 1 January 2017 and 31 December 2020 (all patients are of Han nationality). Shanxi Bethune Hospital is a university teaching hospital with a TCM department; WM is the main type of service available. No cooperation has been established between our treating team and TCM since our department was established, nor have we incorporated TCM into the breast cancer diagnosis and treatment plan.
The patients described above constituted the subjects of our investigation based on the following two reasons. First, our team members were trained uniformly at the end of 2016, and the use of TCM is neither encouraged nor discouraged during and after the end of treatment. That is to say, our team had a neutral attitude toward TCM. Second, a Chinese patent medicine, ie, Huaier Granules, was recommended for breast cancer patients with triple-negative subtype from the time of six months within the end of treatment since April 2022. The patients whom we investigated received neutral recommendations about TCM.
Patients who had passed away or been lost to follow-up at the time of the survey were excluded.
Data Collection
An internal database and an electronic medical record system were used to collect the disease-related information. Other patient information was obtained by telephone follow-up using a self-designed questionnaire.
Once oral consent had been provided by the patients, an electronic informed consent form was sent to them via WeChat, and the participants provided an electronic signature. After that, the data were collected immediately via telephone.
We implemented a three-stage design in this study. First (stage I), four investigators (ie, GJN, ZR, ZJY and GQX) independently reviewed the literature and jointly created the survey questionnaire.
In the second stage (stage II), three investigators (ie, ZR, ZJY and GQX) followed up with five patients and explained the study to them via telephone, respectively. The requirement was that at least four participants would answer all the questions in the questionnaire. The investigation was followed by a new round of discussion, adjusting the questionnaire content and structure. The data on the questionnaire were entered into EpiData Manager (version 4.0.2.101), and a double-entry system was employed in the data entry process.
In the third stage (stage III), three investigators (ie, ZR, ZJY and GQX) followed up with all other patients who met the aforementioned criteria. All investigators maintained a neutral demeanor throughout the investigation.
Demographic data, socioeconomic data, and TCM usage were requested, and the patients had the right to refuse to answer any questions that were uncomfortable The questionnaire was considered valid if the question “has ever used TCM or not” was answered. The patients were further contacted for disease-related information verification to guarantee the accuracy of the data entry.
The Questionnaire
The questionnaire consisted of five parts. The first part was for sociodemographic information, such as age, education, place of residence, occupation, and income. The second part contained disease-related information: the date of initial diagnosis, the time to the end of treatment, pathological types, tumor stage (stage of the disease at the diagnosis), as well as treatment information. The third part contained three questions: the attitude to TCM (the Likert 5-level scoring method was used, with 1 point for “very unconvinced” and 5 point for “very convinced”), experience of TCM treatment before, and the intention to seek subsequent TCM treatment. The fourth part asked non-TCM users about the reasons for non-TCM use.
The fifth section contained details of TCM use, including treatment means, the timing, and the purpose. There are several definitions in this section:
Internal therapy: treating diseases using oral administration.10 The present study included Chinese herbal medicine, therapeutic food, and health products.
External therapy: external application of herbal medicine or exposure of the bodily surface to appliances.11 Moxibustion, acupoint application, lotions/fumigants, and TCM enemas/suppositories were included in this study.
Non-drug therapy: lifestyle management, dietary adjustment, psychological adjustment, exercise, and external conditioning constitute five cornerstones of TCM health management.12 Non-drug therapy in our study included acupuncture, Chinese massage, cupping, and traditional Chinese exercises.
Length of TCM use: the final length was the sum of each treatment used.
Statistical Analysis
All data were analyzed using Statistical Package for Social Sciences (SPSS) version 26. Missing values of annual income per capita were handled using multiple imputations. We did not use statistical methods to impute other missing values, and they were included in the statistical calculation. Categorical variables were reported as a proportion (%), and numerical data were reported as a median and range. Univariate analyses were performed using a t-test or chi-squared test as appropriate. A multivariate logistic regression analysis was performed for the multivariate analyses. All p-values were considered to be statistically significant at a two-tailed p < 0.05. An online tool (https://dycharts.com/) was used for the graphs.
Results
We consecutively recruited 809 patients. Excluding patient deaths (4) and those lost to follow-up (70), a total of 735 (90.9%) individuals were contacted. Twenty-two invalid questionnaires and 22 patients who refused follow-up were excluded. The final analyzed questionnaires amounted to 691 (Figure 1).
 |
Figure 1 Flow chart. |
Factors Associated with Seeking TCM
Demographic and Socioeconomic Characteristics
In this study, 326 (47.2%) participants had used at least one type of TCM, and the median age of the patients was 55 years (range: 29–88 years). Three hundred and twenty-five (47.0%) of the surviving patients were unemployed, 188 (27.2%) were retired, and 178 (25.8%) were in employment at the time of the surveys. A total of 56.4% (390) lived in an urban area; what is more, 65.7% (454) had achieved education at the level of middle school or below. Most patients’ (423, 61.2%) annual income per capita was higher than 30,000 RMB yuan (Table 1).
 |
Table 1 Description of Sample Characteristics |
With increased age, preferences toward TCM use were lower (P = 0.034). The participants were unemployed, lived in rural areas, had a middle school education or below, or had an annual income per capita of less than 30,000 RMB yuan, had a lower prevalence of TCM use (all P < 0.001) (Table 1).
Disease-Related Information
The median time to the end of the treatment was 41 months (17–67 months). The most common type of pathology was luminal B (HER-2 -negative) (385, 55.7%), and 500 (72.4%) patients were at stages I–II. Five hundred and fifty-eight (80.8%) patients accepted chemotherapy, 452 (65.4%) accepted radiotherapy, 502 (72.6%) accepted endocrine therapy, and 146 (21.1%) accepted targeted therapy (Table 1).
Patients accepted chemotherapy (275, 84.4%, P = 0.023), or accepted radiotherapy (230, 33.3%, P = 0.007) were more likely to use TCM. Stages were different between users and non-users (P = 0.005) (Table 1).
Belief in TCM and TCM Usage Before
Most participants held a positive attitude toward TCM (171 (24.7%) with a score of 5 and 273 (39.5%) with a score of 4) (Figure 2). Patients who believed in TCM (a score of 4 or 5, 260, 37.6%) were more inclined to use TCM (P < 0.001). 50.4% (348) patients were TCM users before. Non-TCM users before had a lower prevalence of TCM use (P < 0.001) (Table 1).
 |
Figure 2 Attitude to TCM in total participant. |
Multivariate Analyses
Logistic regression analyses revealed that residential area (rural vs urban, OR = 1.68, 95% CI: 1.17–2.41), education (high middle school or above vs middle school or below, OR = 2.08, 95% CI: 1.41–3.05), annual income per capita (OR = 0.86, 95% CI: 0.58–1.26), TCM users before (yes vs no, OR = 1.75, 95% CI: 1.25–2.44), stage of diagnosis (P = 0.006, stages I–II vs stage 0, OR = 3.12, 95% CI: 1.56–6.23; stages III–IV vs stage 0, OR = 1.42, 95% CI: 0.91–2.21) and trust in TCM (P <0.001, neutralized vs disbelieved, OR = 4.69, 95% CI: 2.20–10.01; believed vs disbelieved, OR = 3.54, 95% CI: 2.41–5.19) were independent predictors of TCM use (Table 2).
 |
Table 2 Logistic Regression |
Sought Subsequent Treatment
The patients who had the intention to seek subsequent help in the form of TCM treatment out of the total population amounted to 357 (51.7%) (Figure 3a), including 240 (73.6%) users of TCM (Figure 3b) and 117 (32.1%) non-TCM users (Figure 3c).
 |
Figure 3 Sought subsequent treatment (The total population: (a), Users of TCM: (b), and Non-TCM users: (c)). |
Details of TCM Use
Most respondents (193, 59.2%) did not inform their physician (Figure 4a), and about half (166, 50.9%) of users of TCM relied on a network query for information, with other means, including relatives (73, 22.4%), breast cancer patients (30, 9.2%), physicians (21, 6.4%), and others (33, 10.1%) (Figure 4b). Regular hospitals (165, 50.6%) and clinics (81, 24.8%) constituted the main treatment pathway (Figure 4c); concerning patients’ attitude toward TCM, most of the respondents (221, 67.8%) demonstrated a positive attitude toward TCM (42.0% were satisfied and 25.8% were very satisfied) (Figure 4d). About 6.1% (20) demonstrated a negative attitude, the main reasons for which were failing to achieve the expected results (15) and spending too much money (6) (Figure 4e). Less than half (134, 41.1%) have recommended TCM to other patients (Figure 4f). The length of TCM use is presented in Figure 4g. For most patients, TCM use was short-term only (153, less than three months).
Treatment Means
Treatment means included internal therapy (296, 90.8%), external therapy (86, 26.4%) and non-drug therapy (76, 23.3%). In internal therapy, Chinese herbal medicine demonstrated the highest frequency (251, 84.8%); this was represented by moxibustion (56, 65.1%) in external therapy and Chinese massage (61, 80.3%) in non-drug therapy (Table 3).
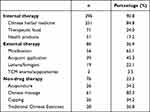 |
Table 3 TCM Treatment Means |
The Timing and Purpose of TCM Use
Most users use TCM during endocrine therapy (215, 66.0%) and after comprehensive Western medicine treatment (92, 28.2%). Only 2.1% (7) of users use TCM during surgery (Table 4).
 |
Table 4 The Timing of TCM Use |
The primary aim of TCM use in our study was overall conditioning (279, 85.6%), followed by alleviating the side effects of Western medicine (126, 38.7%). The top-three side effects that they wanted to address were diarrhea/constipation (58, 46.0%), sleep disturbance (35, 27.8%) and joint pain (30, 23.8%) (Table 5).
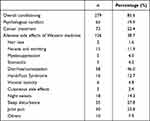 |
Table 5 The Purpose of TCM Use |
The Reason for Non-TCM Use
Over a quarter of non-TCM users did not use TCM due to “not being recommended by a physician” (198, 54.2%). The second reason was “did not know which TCM doctor to seek for” (139, 38.1%), followed by “reject China herbal medicine” (117, 32.1%). Only 24.1% (88) of patients did not use it due to “higher costs”, and a very small number stated that it was due to “not believing in TCM treatment” (33, 9%) (Figure 5).
 |
Figure 5 The reason for non-TCM use. |
Discussion
Our results revealed that approximately half of the breast cancer patients had already sought TCM help and that nearly one-third of non-TCM users intended to seek TCM help. Most TCM users evaluated TCM favorably. Most participants, be they TCM users or not, maintained an attitude of trust toward TCM. Overall, our participants had a high demand and great endorsement for TCM. This finding was somewhat unexpected and intriguing. They may seek TCM for help after finding a breast mass. However, the proportion was not high among our patients; in fact, it was somewhat low (5.8%). This finding has significant implications. Our study revealed a high need for TCM among breast cancer patients. To our knowledge, this is the first study to evaluate TCM needs amongst this group of patients.
The phenomenon of most Chinese believing in TCM and a small proportion preferring TCM treatment to Western medicine treatment when they are sick is common.12 This seeming contradiction may be explained by the “overall conditioning purpose” — most patients used TCM based on the overall conditioning aim. That is to say, in their traditional conception, TCM played the role of adjunct therapy rather than the main role, and WM was more convenient.13–15 People with acute symptoms were inclined to seek Western medicine, while those with chronic symptoms flocked to Eastern medicine.16
Similar previous studies investigated the situation of TCM use in a certain population.17 Even though those studies had a large sample size or a long duration of follow-up, a lack of sufficient information18,19 and large heterogeneity20,21 were found between these studies. Our population consisted of only breast cancer cases, whereby providing an excellent degree of consistency. Beyond this, we probed some issues in more depth, eg, TCM pattern types, purposes related to TCM interventions, influencing factors, people’s understanding and attitude, the efficacy of interventions, and so on. Thus, we could better understand the needs of patients.
High education, high income, and urban background were associated with TCM use in our research. This conclusion followed the results of “the majority relied on network query for information” and “regular hospital was the main treatment pathway.” To some extent, participants with a high level of cognition demonstrated more demand for TCM services. This conclusion is consistent with Xin’s study21 but inconsistent with Tina L’s study.22 This might be because of the difference in study subjects (the participants in Tina L’s study were Hong Kong-born Chinese individuals).
Among TCM treatments, TCM drugs constitute an important means. Chinese herbs and their combinations as prescriptions have been tested by people for thousands of years, and a wide variety of diseases can be treated by iteratively finding natural products that have improved clinical effectiveness.15,23–25 In a proportion of these respondents’ impressions, TCM drugs mean TCM; therefore, “reject China herbal medicine” was the second reason for no TCM use. Indeed, TCM is an extremely broad discipline, as we have mentioned. It is noteworthy that short-term use was most common amongst TCM users.
In addition to the purpose of overall conditioning, the other main purpose was that of alleviating the side effects of Western medicine and the most common side effect to alleviate is diarrhea/constipation. TCM has a long history and unique advantages in alleviating this side effect.26,27 Therefore, this result is within our expectations. Reviewing our study, amongst the population with this purpose, six patients indicated that they were dissatisfied (two for sleep disturbance, one each for joint pain, night sweats, stomatitis, and fatigue, respectively). In total, alleviating the side effects of Western medicine through TCM therapy was recognized by our patients. It has been proven that TCM may be capable of protecting cancer patients from suffering from complications, reducing the side effects of conventional treatment, and improving the quality of life and survival.15,28,29
An interesting phenomenon happened between the team members and survey respondents. Over half of TCM users did not inform their physician, and more than half of non-TCM users selected the reason of “not being recommended by a physician.” Our neutral attitude toward TCM affected patients’ selection to some extent. In the context of breast cancer patients’ TCM needs, professional guidance and personalized advice are particularly important.
Limitation
This study has some notable limitations. First, cost is a topic of great interest to patients. However, there were missing data in our study, and we cannot provide further analysis. Second, the TCM use length was the sum of each treatment — thus, we cannot provide further details on each treatment. Third, the follow-up time was short compared to breast cancer patients’ long treatment durations and better prognoses.
Conclusion
There is a great TCM need amongst breast cancer survivors who have been receiving WM treatment. The lead physician plays an important role in patients’ TCM healthcare-seeking behavior. Most patients reported that TCM treatment was effective. Enhanced communication concerning TCM was called for WM doctors.
Abbreviations
TCM, traditional Chinese medicine; WM, Western medicine.
Data Sharing Statement
The raw data supporting the conclusions of this article will be made available by the corresponding author, without undue reservation.
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Shanxi Bethune Hospital Ethics Committee (No. YXLL-2023-153).
Consent to Participate
The patients/participants provided their written informed consent to participate in this study. The manuscript has been read and approved by all the authors.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by Four “Batches” Innovation Project of Invigorating Medical through Science and Technology of Shanxi Province (2022XM01) and Shanxi Province “136 Revitalization Medical Project Construction Funds”.
Disclosure
The authors have no relevant financial or non-financial interests to disclose for this work.
References
1. Xu J, Yang Y. Traditional Chinese medicine in the Chinese health care system. Health Policy. 2009;90:133–139. doi:10.1016/j.healthpol.2008.09.003
2. A-p L, Jia H-W, Xiao C, Q-p L. Theory of traditional Chinese medicine and therapeutic method of diseases. World J Gastroenterol WJG. 2004;10:1854–1856. doi:10.3748/wjg.v10.i13.1854
3. The statistical bulletin on the development of health and health services in China in 2021; 2022. Available from: http://www.nhc.gov.cn/guihuaxxs/s3586s/202207/51b55216c2154332a660157abf28b09d.shtml.
4. Cancer today. Available from: http://gco.iarc.fr/today/home.
5. Liang Y, Zhang H, Song X, Yang Q. Metastatic heterogeneity of breast cancer: molecular mechanism and potential therapeutic targets. Semin Cancer Biol. 2020;60:14–27. doi:10.1016/j.semcancer.2019.08.012
6. Burstein HJ, Curigliano G, Thürlimann B, et al. Customizing local and systemic therapies for women with early breast cancer: the St. Gallen international consensus guidelines for treatment of early breast cancer 2021. Ann Oncol off J Eur Soc Med Oncol. 2021;32:1216–1235. doi:10.1016/j.annonc.2021.06.023
7. Trayes KP, Cokenakes SEH. Breast Cancer Treatment. Am Fam Physician. 2021;104:171–178.
8. Jiang H, Li M, Du K, et al. Traditional Chinese Medicine for adjuvant treatment of breast cancer: Taohong Siwu Decoction. Chin Med. 2021;16:129. doi:10.1186/s13020-021-00539-7
9. Khan MI, Bouyahya A, Hachlafi NEL, et al. Anticancer properties of medicinal plants and their bioactive compounds against breast cancer: a review on recent investigations. Environ Sci Pollut Res Int. 2022;29:24411–24444. doi:10.1007/s11356-021-17795-7
10. li ZB, Wu M. Traditional Chinese Internal Medicine.
11. Kang ZY, Rong CX. External Treatment of Traditional Chinese Medicine.
12. Li-li T, Ma X. Importance of non-drug therapy on ‘preventive treatment of disease’ of TCM from the guideline of hypertension. China J Tradit Chin Med Pharm. 2018;33:4859–4862.
13. Tan KY, Liu CB, Chen AH, et al. The role of traditional Chinese medicine in colorectal cancer treatment. Tech Coloproctol. 2008;6. doi:10.1007/s10151-008-0392-z
14. Zhang X, Qiu H, Li C, et al. The positive role of traditional Chinese medicine as an adjunctive therapy for cancer. Biosci Trends. 2021;15:283–298. doi:10.5582/bst.2021.01318
15. Qi F, Zhao L, Zhou A, et al. The advantages of using traditional Chinese medicine as an adjunctive therapy in the whole course of cancer treatment instead of only terminal stage of cancer. Biosci Trends. 2015;9:16–34. doi:10.5582/bst.2015.01019
16. Zhang Q, Feng S, Wong IOL, et al. A population-based study on healthcare-seeking behaviour of persons with symptoms of respiratory and gastrointestinal-related infections in Hong Kong. BMC Public Health. 2020;20:402. doi:10.1186/s12889-020-08555-2
17. Duan Y, Xu Z, Lin Y, et al. A scoping review of cross-sectional studies on traditional Chinese medicine. Am J Chin Med. 2021;49:1275–1296. doi:10.1142/S0192415X21500610
18. Liao Y-H, Lin -C-C, Li T-C, Lin J-G. Utilization pattern of traditional Chinese medicine for liver cancer patients in Taiwan. BMC Complement Altern Med. 2012;12:146. doi:10.1186/1472-6882-12-146
19. Lin Y-H, Chiu J-H. Use of Chinese medicine by women with breast cancer: a nationwide cross-sectional study in Taiwan. Complement Ther Med. 2011;19:137–143. doi:10.1016/j.ctim.2011.04.001
20. Sun K, Szymonifka J, Tian H, et al. Association of traditional Chinese medicine use with adherence to prescribed western rheumatic medications among Chinese American patients: a cross-sectional survey. Arthritis Care Res. 2020;72:1474–1480. doi:10.1002/acr.24031
21. Xin B, Mu S, Tan T, et al. Belief in and use of traditional Chinese medicine in Shanghai older adults: a cross-sectional study. BMC Complement Med Ther. 2020;20:128. doi:10.1186/s12906-020-02910-x
22. Rochelle TL, Yim KH. Factors associated with utilisation of traditional Chinese medicine among Hong Kong Chinese. Psychol Health Med. 2014;19:453–462. doi:10.1080/13548506.2013.819439
23. Fang S, Dong L, Liu L, et al. HERB: a high-throughput experiment- and reference-guided database of traditional Chinese medicine. Nucleic Acids Res. 2021;49:D1197–D1206. doi:10.1093/nar/gkaa1063
24. Parekh HS, Liu G, Wei MQ. A new dawn for the use of traditional Chinese medicine in cancer therapy. Mol Cancer. 2009;8:21. doi:10.1186/1476-4598-8-21
25. Chien T-J, Liu C-Y, R-h L, et al. Therapeutic efficacy of Traditional Chinese medicine, “Kuan-Sin-Yin”, in patients undergoing chemotherapy for advanced colon cancer - A controlled trial. Complement Ther Med. 2016;29:204–212. doi:10.1016/j.ctim.2016.10.001
26. Zhong LLD, Zheng G, Da Ge L, et al. Chinese herbal medicine for constipation: zheng-based associations among herbs, formulae, proprietary medicines, and herb-drug interactions. Chin Med. 2016;11:28. doi:10.1186/s13020-016-0099-4
27. Zhou Q, Zhang D, Zhang H, et al. Effects of Xiao Chengqi formula on slow transit constipation by assessing gut microbiota and metabolomics analysis in vitro and in vivo. Front Pharmacol. 2022;13:864598. doi:10.3389/fphar.2022.864598
28. Chen D, Guo Y, Yang Y. Liujunanwei decoction attenuates cisplatin-induced nausea and vomiting in a Rat-Pica model partially mediated by modulating the gut microbiome. Front Cell Infect Microbiol. 2022;12:876781. doi:10.3389/fcimb.2022.876781
29. Ashraf-Uz-Zaman M, Bhalerao A, Mikelis CM, et al. Assessing the current state of lung cancer chemoprevention: a comprehensive overview. Cancers. 2020;12:1265. doi:10.3390/cancers12051265
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

