Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 14
Poor Glycemic Control and Its Contributing Factors Among Type 2 Diabetes Patients at Adama Hospital Medical College in East Ethiopia
Authors Yosef T , Nureye D , Tekalign E
Received 25 May 2021
Accepted for publication 7 July 2021
Published 15 July 2021 Volume 2021:14 Pages 3273—3280
DOI https://doi.org/10.2147/DMSO.S321756
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Tewodros Yosef,1 Dejen Nureye,2 Eyob Tekalign3
1Department of Epidemiology and Biostatistics, School of Public Health, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan Teferi, Ethiopia; 2Department of Pharmacology and Toxicology, School of Pharmacy, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan Teferi, Ethiopia; 3Department of Medical Laboratory Science, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan Teferi, Ethiopia
Correspondence: Tewodros Yosef
Department of Epidemiology and Biostatistics, School of Public Health, College of Medicine and Health Sciences, Mizan-Tepi University, P.O.Box: 260, Mizan Teferi, Ethiopia
Email [email protected]
Background: Poor glycemic control is a major public health issue among patients with type 2 diabetes mellitus and a significant risk factor for the progression of diabetic complications. This study aimed to assess the magnitude and contributing factors of poor glycemic control among type 2 diabetes patients on follow-up at Adama Hospital Medical College (AHMC) in East Ethiopia.
Methods: A cross-sectional study was conducted among 245 type 2 diabetes patients on follow-up at AHMC from March 1 to 30, 2020. All type 2 diabetes patients on follow-up at AHMC and fulfilling the inclusion criteria were included in the study. The data were collected through face-to-face interviews using structured questionnaires and reviewing the patient chart. The data were entered and analyzed using SPSS version 21. The level of significance was declared at a p-value of < 0.05.
Results: Of the 245 type 2 diabetes patients included in the study, 157 (64.1%) had poor glycemic control. The factors associated with poor glycemic control were being male (AOR = 2.28, 95% CI [1.24– 4.21]), not attending formal education (AOR = 3.12, 95% CI [1.53– 6.35]), monthly income of < 136 USD (AOR = 2.14, 95% CI [1.17– 3.91]), overweight (AOR = 2.60, 95% CI [1.32– 5.10]) and obesity (AOR = 3.44, 95% CI [1.44– 8.21]), and chewing khat (AOR = 2.77, 95% CI [1.04– 7.33]).
Conclusion: The proportion of poor glycemic control among type 2 diabetes patients at AHMC was remarkably high. Therefore, more effort should be taken to strengthening and disseminating health education programs for diabetes patients at each follow-up visit on the importance of achieving optimal body weight, avoiding khat chewing, and maintaining regular physical exercise to prevent and mitigate the complications resulting from poor glycemic control.
Keywords: type 2 diabetes, glycemic control, AHMC, Ethiopia
Introduction
Diabetes mellitus (DM) defined as a metabolic disorder characterized by a high blood glucose level (hyperglycemia).1,2 DM is a universal public health problem, resulting in about 5 million deaths annually from related complications.3 It is estimated that over 422 million adults are living with diabetes globally and this is anticipated to reach about 439 million adults by 2030 and 642 million by 2040.4,5
Diabetes mellitus is growing at an alarming rate throughout the world, and approximately 80% of diabetics live in developing countries.6 Its burden is highest in resources limited countries, where screening and access to care and treatment are not readily available.5 Type 2 DM is a heterogeneous group of disorders characterized by insulin resistance, impaired insulin secretion, and increased glucose production2 and it accounts for 90% of total diabetes.1 The occurrence of type 2 DM is rapidly increasing all over the world in which the number of adults with diabetes in the world will rise from 135 million in 1995 to 300 million in the year 2025.7
The burden of mortality and cardiovascular disease associated with uncontrolled diabetes is considerably high.8 Glycemic control is a very important goal in the management of patients with diabetes9,10 and it remains the main therapeutic target for the prevention of organ damage and other complications arising from diabetes.11 Poor glycemic control is a major public health issue among patients with type 2 diabetes mellitus and a significant risk factor for the progression of diabetic complications.12–14
Poor glycemic control is a common problem in different parts of the world. Observational studies were conducted worldwide and revealed the magnitude of poor glycemic control ranges from 50.1% to 91.8%.13,15–20 The magnitude of poor glycemic control among type 2 diabetes patients in Ethiopia was ranges from 50% to 80%.8,11,28–30,14,21–27
The factors associated with glycemic control were age, gender, marital status, residence, educational status, occupational status, monthly income, family history of DM, membership of diabetes association, type of diabetes, duration of diabetes, type of medication, body mass index, physical exercise, knowledge and attitude insulin self-administration, adherence to diet, and medication, follow-up, self-monitoring of blood glucose levels and family support.8,11,27–29,13–15,17,19,21,24,25,31,32
To minimize the burden of diabetes mellitus, strictly maintaining a patient’s blood glucose level in the normal or close to the normal range is crucial.31 Despite many studies done in Ethiopia regarding this issue,8,11,29–31,14,21,22,24–28,33 most of them were conducted in the Oromia and Amhara regions of Ethiopia, which did not truly reflect the magnitude in the Eastern parts of Ethiopia. Besides, this study done with the expectation of getting different results due to the presence of great variation in socioeconomic, cultural and lifestyle characteristics of the study populations compared to other studies in Ethiopia. Therefore, this study aimed to assess the magnitude and contributing factors of poor glycemic control among type 2 diabetes patients on follow-up at AHMC in East Ethiopia.
Methods
Study Design, Area, and Period
A hospital-based cross-sectional study was conducted in the chronic disease outpatient department clinic of AHMC from March 1 to 30, 2020. AHMC is one of the oldest public hospitals in the country and it is found in Adama city, which has 220,212 populations according to the 2007 census statistical of Ethiopia.34 Adama city is located 90 km to the East of Addis Ababa, the capital city of Ethiopia. AHMC is a referral hospital and provides outpatient, inpatient, emergency, ambulatory, and other specialized services for the community living in the Eastern part of Ethiopia.
Source and Study Populations
All type 2 diabetes patients on follow-up at AHMC were the source population. Randomly selected type 2 diabetes patients on follow-up and who fulfill the inclusion criteria were the study population.
Inclusion Criteria
- Age ≥18 years.
- Patients who were diagnosed to have type 2 diabetes.
- Patients with at least three consecutive blood glucose measurements for three months.
- Patients who have a willingness to participate in the study.
Exclusion Criteria
- Pregnant patients during the study period.
- Critically ill patients.
- If the patient chart will not be available during the data collection period.
Sample Size Determination and Sampling Method
The required sample size was determined using the single population proportion formula with the assumption of taking a proportion of diabetes with poor glycemic control from a study in Addis Ababa to be 80%,30 5% margin of error, 95% confidence level, and adding 10% for non-response rate compensation. The final computed sample size was 271. The total numbers of type 2 diabetes patients who attend AHMC chronic follow-up clinic were 562. A systematic random sampling technique was employed to select the participants of every two patients (k= 562/271= 2) during their attendance. A random number from one and two were chosen as a random start then it was 2. Hence, every two diabetic patients were studied until the total sample size was obtained.
Study Variables and Measurements
The dependent variable was poor glycemic control. The independent variables were socio-demographic variables (age, sex, educational status, income, religion, ethnicity, marital status, occupational status, BMI), patient and clinical characteristics (duration of DM diagnosis, duration of DM treatment, specific type of drug regimen, comorbidity, DM complication, treatment adherence), and behavioral characteristics (smoking, alcohol consumption, khat chewing, drug use, physical activities, dietary, and knowledge of target blood glucose).
Glycemic control is the way of managing the blood glucose level of diabetic patients at optimum level.10
Fasting Blood Sugar
Blood glucose measured from venous blood after at least 8 hours of overnight fasting.35
Good Glycemic Control
If the patients had 70–130mg/dl of fasting blood glucose upon measurement of three consecutive visits, otherwise poor glycemic control.10,35,36
Adherence to Blood Glucose Testing
If the patient was found to measure his/her blood glucose for more than or equal to 4 days in the last seven days.8
Adherence to Physical Exercise
If the patient was followed recommended level of exercise for more than or equal to 5 days in the last seven days.37
Alcohol Drinker
A patient who drinks alcohol every day or every other day basis whatever the amounts were considered alcohol drinker, otherwise not.
Data Collection Tools and Procedure
The data were collected through a face-to-face interview using a structured questionnaire and by reviewing patient charts using a checklist. The structured questionnaire incorporates information about socio-demographic characteristics, behavioral profiles, comorbidity, complication, and drug-related profiles. The questionnaire was developed by reviewing relevant literature in English and then translated into the local language, and back-translated into English to check the consistency by an independent translator. Fasting blood sugar records of the last three clinic visits (3 months) were obtained from patients’ medical cards and the mean was used to determine the level of glycemic control. The body mass index of the study participants was measured using a DHM-15A standardized scale (BMI height and weight body fat scale) at their arrival at the follow-up clinic of the hospital. BMI was categorized as underweight if BMI was <18.5 kg/m2, normal if BMI was 18.5–24.9 kg/m2, overweight if BMI was 25–29.9 kg/m2, and obese if BMI was ≥30 kg/m2. The training was given to data collectors and supervisors concerning the objective and process of data collection and to discuss the presence of an ambiguous question in the questionnaire.
Data Processing and Analysis
The data were entered and analyzed using SPSS version 21. The results are presented in tables and numerical summary measures such as mean and standard deviation (SD). Bivariate and multivariable logistic regression analyses were used to identify independent variables associated with poor glycemic control. Independent variables with a p-value of less than 0.25 in bivariate logistic regression were included in the multivariable logistic regression model. The Hosmer-Lemeshow goodness-of-fit test indicated (P = 0.522) that the model was good enough to fit the data well. The level of significance was declared at a p-value of <0.05.
Results
Sociodemographic Characteristics
Of the 271 total sample sizes, 245 study participants have completed the interview, giving a response rate of 90.4%. The mean age of the participants was 48.6 (±14.9 SD) ranging from 18 to 85 years old. One hundred sixty (65.3%) and 112 (45.7%) of the participants were married and Orthodox in religion, respectively. The average monthly income was 136, ranges from 80 to 165 USD. The average body mass index was 24.95 (±3.99 SD) ranging from 18.6 to 41.2 kg/m2 (Table 1).
 |
Table 1 Sociodemographic Characteristics of the Respondents at AHMC in East Ethiopia |
Behavioral Profiles
Of the 245 interviewed, 6 (2.4%) and 19 (7.8%) of the respondents were cigarette smokers and alcohol drinkers respectively. Forty (16.3%) of the study participants were khat chewer. Two hundred nineteen (89.4%) and 223 (91%) of the participants had no adherence to exercise and no adherence to blood glucose testing, respectively (Table 2).
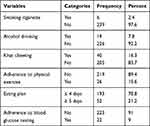 |
Table 2 Behavioral Profiles of the Respondents at AHMC in East Ethiopia |
Comorbidity, Complication, and Drug-Related Profiles
One hundred thirty-five (55.1%) and 112 (45.7%) participants had comorbidity and diabetes complications, respectively. The majority (65.7%) of the participants was used oral hypoglycemic agents and 210 (85.7%) participants were treated for seven years or more. The magnitude of poor glycemic control among type 2 diabetes patients at AHMC was 64.1% (n = 157) (Table 3).
 |
Table 3 Comorbidity, Complication, and Drug-Related Profiles of the Respondents at AHMC in East Ethiopia |
Factors Associated with Good Glycemic Control
After adjusting for confounding variables, being male (AOR = 2.28, 95% CI [1.24–4.21]), not attending formal education (AOR = 3.12, 95% CI [1.53–6.35]), monthly income of <136 USD (AOR = 2.14, 95% CI [1.17–3.91]), overweight (AOR = 2.60, 95% CI [1.32–5.10]) and obesity (AOR = 3.44, 95% CI [1.44–8.21]), chewing khat (AOR = 2.77, 95% CI [1.04–7.33]), and not adherence to exercise (AOR = 3.71, 95% CI [1.44–9.58]) were factors significantly associated with poor glycemic control (Table 4).
 |
Table 4 Factors Associated with Poor Glycemic Control of the Respondents at AHMC in East Ethiopia |
Discussion
An important strategy for the management of patients with type 2 diabetes to prevent or delay disease progression and reduce the risk of developing diabetes complications is maintaining good glycemic control.15 This study aimed to assess the magnitude and contributing factors of poor glycemic control among type 2 diabetes patients on follow-up at AHMC in East Ethiopia.
The magnitude of poor glycemic control among study participants at AHMC was 64.1%, 95% CI (58.1–70.1%). This finding was in line with 59.2%,11 63.8%,24 and 64.9%26 at Oromia region hospitals, Ethiopia, and 68.3% at Tikur Anbessa Specialized Hospital in Ethiopia.27 It was higher than 50%,25 55.3%,22 and 57.1%23 prevalence at Oromia and Amhara regional hospitals in Ethiopia. But, it was lower than 70.8%,28 70.9%,21 71.4%,14 72.7%,8 and 73.5%29 prevalence at Oromia and Amhara regional hospitals in Ethiopia. The discrepancy observed between this and other studies was due to the difference in sample size, and operational definition used (this study uses fasting blood glucose level to categorized glycemic control, while other studies use hemoglobin A1c to categorized glycemic control). Besides, the presence of great variation in socioeconomic, cultural and lifestyle characteristics of the study populations across different studies may play a great role in the observed difference.
In this study, the sex of the respondents had a significant association with glycemic control. Being male had 2.3 times higher odds of having poor glycemic control than females. This finding was supported by a study conducted in Nigeria.13 But, some studies revealed that being female is more associated with poor glycemic control.19,27 This could be because males have higher insulin resistance compared to females.38
Not attending formal education was statistically associated with poor glycemic control. Respondents who are not attending formal education were 3 times more likely to have poor glycemic control than those who attend formal education. This finding was supported by studies conducted in Ethiopia14,21,24,28 and Nigeria.15 This could be due to the low diabetes knowledge and its treatment resulted in the low practice of recommended diabetes treatment, application of diabetes-friendly lifestyles, and poor adherence to diabetes medication.39
In this study, low monthly income showed a significant association with poor glycemic control. Respondents who had a monthly income <136 USD were 2 times higher odds of having poor glycemic control than those who had a monthly income of 136 USD or more. This finding was supported by Bayisa et al24 revealed that low monthly income was significantly associated with poor glycemic control. This could be due to the inability to afford diabetes self-monitoring devices and diabetes-friendly diets that help to achieve good glycemic control.26 Since frequent self-monitoring of blood glucose levels may enable patients to better control glycemic levels as this could guide on how to respond and adjust their treatment regimen in line with blood glucose levels.31
Body mass index was associated with glycemic control. Respondents who were overweight and obese were 2.6 and 3.4 times respectively more likely to have poor glycemic control than those who had normal body mass index. This finding was supported by several studies.8,15,27 A study done by Borgharkar et al revealed that for every one-unit increase in the patient BMI, the HbA1c of the patient increases by 0.1%.40 Chewing khat was significantly associated with poor glycemic control. Respondents who chewed khat were 2.8 times higher odds of having poor glycemic control than those who did not chew khat. This could be due to the association of khat chewing with higher fasting blood glucose levels.36
In this study, lack of adherence to physical exercise was significantly associated with poor glycemic control. Respondents who did not adhere to physical exercise were 3.7 times more likely to have poor glycemic control than those who adhere to physical exercise. This finding was supported by a study conducted in Ethiopia.31 This could be due to the effect of exercise on the reduction of hemoglobin A1c either by increasing insulin secretion from the beta cells or decreasing insulin resistance from the cell of our body.41
Limitations of the Study
First, the cross-sectional nature of the study design does not allow ascertaining the causal association between the outcome variable and potential contributing factors. Second, the smaller sample size may limit the generalization of the study findings to a larger population of type 2 diabetes patients in the country. The last and foremost, the use of fasting blood glucose to assess the level of glycemic control (failure to use glycated hemoglobin due to the lack of laboratory facility), since measurement of fasting blood glucose does not show the true level of glycemic control over 3 months like that of glycated hemoglobin (HbA1c).
Conclusion
The proportion of poor glycemic control among type 2 diabetes patients at AHMC was remarkably high. Therefore, more effort should be taken to strengthening and disseminating health education programs for diabetes patients at each follow-up visit on the importance of achieving optimal body weight, avoiding khat chewing, and maintaining regular physical exercise to prevent and mitigate the complications resulting from poor glycemic control.
Abbreviations
AHMC, Adama Hospital Medical College; AOR, adjusted odds ratio; BMI, body mass index; CI, confidence interval; COR, crude odds ratio; DM, diabetes mellitus; HbA1c, hemoglobin A1c; SPSS, Statistical Package for the Social Sciences; SD, standard deviation; USD, United States Dollar.
Data Sharing Statement
The data set is handled by the corresponding author and can be provided upon request.
Ethics Approval and Consent to Participate
Ethical approval was obtained from Mizan-Tepi University-Institutional Review Board (MTU-IRB). Permission was obtained from AHMC. The study participants were informed about the purpose of the study, their right to deny participation, anonymity, the confidentiality of the information, and this study was conducted following the Declaration of Helsinki. Written informed consent was obtained from participants who participated in the study.
Acknowledgment
First, we would like to thank all study participants for their participation. Second, our thank goes to the academic and administrative staff at AHMC who gave us full collaboration during the study period.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. World Health Organization. Classification of Diabetes Mellitus. Switzerland: WHO; 2019.
2. Ramphal R, Fauci AS, Braunwald E, Kaspe D, eds. Endocrinology and Metabolism. Harrison Principles of Internal Medicine.
3. Baena-Dı´ez JM, Pen˜afiel J, Subirana I, et al. Risk of cause-specific death in individuals with diabetes: a competing risks analysis. Diabetes Care. 2016;39(11):1987–1995. doi:10.2337/dc16-0614
4. International Diabetes Federation. IDF Diabetes Atlas.
5. Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14. doi:10.1016/j.diabres.2009.10.007
6. Cho NH, Shaw JE, Karuranga S, et al. IDF diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi:10.1016/j.diabres.2018.02.023
7. Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2009;32(1):193–203. doi:10.2337/dc08-9025
8. Sheleme T, Mamo G, Melaku T, Sahilu T. Glycemic control and its predictors among adult diabetic patients attending Mettu Karl Referral Hospital, Southwest Ethiopia: a Prospective Observational Study. Diabetes Ther. 2020;11(8):1775–1794. doi:10.1007/s13300-020-00861-7
9. Imran SA, Agarwal G, Bajaj HSRS, Ross S. Targets for glycemic control. Can J Diabetes. 2018;42:S42–S46. doi:10.1016/j.jcjd.2017.10.030
10. American Diabetes Association. Classification and diagnosis of diabe- tes: standards of medical care in diabetes—2018. ADA Diabetes Care J Clin Appl Res Educ. 2018;41(Supplement 1):S13–S27.
11. Yigazu DM, Desse TA. Glycemic control and associated factors among type 2 diabetic patients at Shanan Gibe Hospital, Southwest Ethiopia. BMC Res Notes. 2017;10(1):597. doi:10.1186/s13104-017-2924-y
12. Koro CE, Bowlin SJ, Bourgeois N, et al. Glycemic control from 1988 to 2000 among U.S. adults diagnosed with type 2 diabetes: a preliminary report. Diabetes Care. 2004;27(1):17–20. doi:10.2337/diacare.27.1.17
13. Yakubu A, Dahiru S, Mainasara AS, Anaja PO, Musa B, Hassan HA. Determinants of poor glycaemic control among type 2 diabetic patients at a suburban tertiary hospital in North-Western Nigeria. Int J Sci Health Res. 2020;5(4):207–214.
14. Digssie A, Abebaw S, Achaw A, Getachew H, Achamyelew B. Level of glycemic control and its associated factors among type II diabetic patients in Debre Tabor general hospital, northwest Ethiopia. Metab Open. 2020;8:100056. doi:10.1016/j.metop.2020.100056
15. Ea D, Ri A, Ro S, Iy N, Auta A. Glycemic control and its determinants among patients with type 2 diabetes in a specialist hospital in Northeast, Nigeria. SAJ Pharma Pharmacol. 2019;6(1):2–9.
16. Ufuoma C, Godwin YD, Kester AD, Ngozi JC. Determinants of glycemic control among persons with type 2 diabetes mellitus in Niger Delta. Sahel Med J. 2016;19(4):190–195. doi:10.4103/1118-8561.196361
17. da Silva DG, Simeoni LA, Amato AA. Factors associated with poor glycemic control among patients with type 2 diabetes in the Southeast Region of Brazil. Int J Diabetes Res. 2018;7(2):36–40. doi:10.5923/j.diabetes.20180702.03
18. Sufia Ahmed N, Islahudin F, Paraidathathu T. Factors associated with good glycemic control among patients with type 2 diabetes mellitus. J Diabetes Investig. 2014;5(5):563–569. doi:10.1111/jdi.12175
19. Haghighatpanah M, Sasan A, Nejad M, Haghighatpanah M, Thunga G. Factors that correlate with poor glycemic control in type 2 diabetes mellitus patients with complications. Osong Public Health Res Perspect. 2018;9(4):167–174. doi:10.24171/j.phrp.2018.9.4.05
20. Kakade AA, Mohanty IR, Rai S. Assessment of factors associated with poor glycemic control among patients with type II diabetes mellitus. Integr Obes Diabetes. 2018;4(3):1–6.
21. Kassahun T, Eshetie T, Gesesew H. Factors associated with glycemic control among adult patients with type 2 diabetes mellitus: a cross ‑ sectional survey in Ethiopia. BMC Res Notes. 2016;9:78. doi:10.1186/s13104-016-1896-7
22. Feleke BE, Feleke TE, Kassahun MB, et al. Glycemic control of diabetes mellitus patients in referral hospitals of Amhara Region, Ethiopia: a Cross-Sectional Study. Biomed Res Int. 2021;2021:6691819.
23. Ayele AA, Tegegn HG, Ayele TA, Ayalew MB. Medication regimen complexity and its impact on medication adherence and glycemic control among patients with type 2 diabetes mellitus in an Ethiopian general hospital. BMJ Open Diabetes Res Care. 2019;7(1):e000685. doi:10.1136/bmjdrc-2019-000685
24. Bayisa B, Bekele M. Glycemic control and associated factors among type II diabetic patients on chronic follow up at Southwest Ethiopia. Res Rev J Med Health Sci. 2017;6(3):13–20.
25. Woldu MA, Wami CD, Lenjisa JL, Tegegne GT, Tesafye G, Dinsa H. Factors associated with poor glycemic control among patients with type 2 diabetes mellitus in Ambo Hospital, Ambo; Ethiopia. Endocrinol Metab Synd. 2014;3(4):2–7.
26. Fekadu G, Bula K, Bayisa G, Turi E, Tolossa T, Kasaye HK. Challenges and factors associated with poor glycemic control among type 2 diabetes mellitus patients at nekemte referral hospital, Western Ethiopia. J Multidiscip Healthc. 2019;12:963–974. doi:10.2147/JMDH.S232691
27. Demoz GT, Gebremariam A, Yifter H, et al. Predictors of poor glycemic control among patients with type 2 diabetes on follow ‑ up care at a tertiary healthcare setting in Ethiopia. BMC Res Notes. 2019;12:207. doi:10.1186/s13104-019-4248-6
28. Fiseha T, Alemayehu E, Kassahun W, Adamu A, Gebreweld A. Factors associated with glycemic control among diabetic adult out-patients in Northeast Ethiopia. BMC Res Notes. 2018;11:316. doi:10.1186/s13104-018-3423-5
29. Gebrie A, Tesfaye B, Sisay M. Evaluation of glycemic control status and its associated factors among diabetes patients on follow-up at referral hospitals of Northwest Ethiopia: a cross-sectional study, 2020. Heliyon. 2020;6(12):e05655. doi:10.1016/j.heliyon.2020.e05655
30. Tekalegn Y, Addissie A, Kebede T, Ayele W, Palazón-Bru A. Magnitude of glycemic control and its associated factors among patients with type 2 diabetes at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia. PLoS One. 2018;13(3):e0193442. doi:10.1371/journal.pone.0193442
31. Mariye T, Bahrey D, Tasew H, et al. Determinants of poor glycemic control among diabetes mellitus patients in public hospitals of the central zone, Tigray, North Ethiopia, 2018: Unmatched Case-Control Study. Endocrinol Metab Open Access. 2020;4(1):1–7.
32. Yosef T. Knowledge and attitude on insulin self-administration among type 1 diabetic patients at Metu Karl referral hospital, Ethiopia. J Diabetes Res. 2019;2019:1–7. doi:10.1155/2019/7801367
33. Ayele BA, Tadege M, Tabor D. Level of glycemic control and its associated factors among type II diabetic patients in Debre Tabor general hospital, Northwest Ethiopia. Metab Open. 2020;2(1):1–7.
34. Centeral Statistical Agency. Population and Housing Census 2007 Report, National; 2010.
35. American Diabetes Association. Glycemic targets: standards of medical care in diabetes 2020. Diabetes Care. 2020;43(Suppl 1):S66–S76. doi:10.2337/dc20-S006
36. Tadele A, Getachew T, Defar A, et al. Effect of khat consumption on blood biochemical parameters: evidences from the Ethiopian non communicable diseases STEPS Survey, 2015. Ethiop J Public Health Nutr. 2020;4(2):129–135.
37. Ministry of Health: Manatu Hauora. How Much Activity is Recommended?Available from: https://www.health.govt.nz/your-health/healthy-living/food-activity-and-sleep/physical-activity/how-much-activity-recommended. Accessed June 27, 2021.
38. Geer EB, Shen W. Gender differences in insulin resistance, body composition, and energy balance. Gend Med. 2009;6(Suppl 1):60–75. doi:10.1016/j.genm.2009.02.002
39. Kassahun T, Gesesew H, Mwanri L, Eshetie T. Diabetes related knowledge, self-care behaviours and adherence to medications among diabetic patients in Southwest Ethiopia: a cross-sectional survey. BMC Endocr Disord. 2016;16(1):28. doi:10.1186/s12902-016-0114-x
40. Borgharkar SS, Das SS. Real-world evidence of glyce- mic control among patients with type 2 diabetes mellitus in India: the TIGHT study. BMJ Open Diabetes Res Care. 2019;7:1. doi:10.1136/bmjdrc-2019-000654
41. Boulé NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA. 2001;286(10):1218–1227. doi:10.1001/jama.286.10.1218
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
