Back to Journals » Journal of Healthcare Leadership » Volume 15
Pediatric Faculty Engagement and Associated Areas of Worklife After a COVID19 Surge
Authors Uong AM , Cabana MD, Serwint JR, Bernstein CA, Schulte EE
Received 20 April 2023
Accepted for publication 23 August 2023
Published 28 November 2023 Volume 2023:15 Pages 375—383
DOI https://doi.org/10.2147/JHL.S410797
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Pavani Rangachari
Audrey M Uong,1 Michael D Cabana,1 Janet R Serwint,2 Carol A Bernstein,3 Elaine E Schulte1
1Department of Pediatrics, Children’s Hospital at Montefiore/Albert Einstein College of Medicine, Bronx, NY, USA; 2Department of Pediatrics, Johns Hopkins University School of Medicine, Baltimore, MD, USA; 3Department of Psychiatry, Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, NY, USA
Correspondence: Audrey M Uong, Department of Pediatrics, Children’s Hospital at Montefiore, 3411 Wayne Ave, Bronx, NY, 10467, USA, Tel +1 718 741-2282, Fax +1 718 920-6506, Email [email protected]
Purpose: Healthcare organizations strive to increase physician engagement and decrease attrition. However, little is known about which specific worklife areas may be targeted to improve physician engagement or retention, especially after stressful events such as a COVID19 surge. Our objective was to identify demographic characteristics and worklife areas most associated with increased physician engagement and decreased intent to leave in pediatric faculty.
Patients and Methods: In September 2020, we conducted a cross-sectional survey of faculty at an academic, tertiary-care children’s hospital. A convenience and voluntary sampling approach was used. The survey included demographics, Maslach Burnout Index-Human Services Survey (MBI-HSS) and the Areas of Worklife Survey (AWS). The MBI-HSS was used to measure faculty engagement. The AWS measures satisfaction with six worklife areas (workload, control, reward, fairness, community, values). We used bivariate analyses to examine relationships between worklife areas and engagement and between worklife areas and intent to leave. We included multivariate logistic regression models to examine worklife areas most associated with increased work engagement and decreased intent to leave.
Results: Our response rate was 41% (113/274 participants). In bivariate analysis, engaged faculty reported higher satisfaction in all worklife areas. In multivariate analyses, positive perceptions of workload (odds ratio (OR) 2.83; 95% confidence interval (CI), 1.2– 6.9), control (OR, 3.24; 95% CI 1.4– 7.3), and community (OR, 6.07; 95% CI 1.9– 18.7) were associated with engagement. Positive perceptions of values (OR, 0.07; 95% CI 0.02– 0.32) and community (OR, 0.19; 95% CI 0.05– 0.78) were negatively associated with intent to leave.
Conclusion: We found that positive perceptions of workload, control, and community were most associated with engagement. Alignment of values and increased sense of community were associated with decreased intent to leave. Our findings suggest specific worklife areas may be targeted to increase faculty engagement and retention.
Plain Language Summary: Physician engagement and retention are growing concerns for healthcare organizations. We conducted a cross-sectional survey of pediatric faculty after a COVID19 surge in 2020 to examine whether there are worklife areas highly associated with physician engagement and decreased intent to leave their current practice. We found that respondents with high positive perceptions of their workload, autonomy and community in their workplace were more likely to be engaged, and that respondents who felt that their values aligned with their organization’s values and felt a positive sense of community were less likely to report intent to leave the organization. Prioritizing improvements in physician workload, autonomy, and community, and recruiting physicians with similar values may be an effective strategy for organizations who desire to increase physician engagement and retention.
Keywords: physician burnout, workforce, physician well-being
Introduction
Physician engagement is critical for the vitality of many healthcare organizations, especially academic institutions.1–3 Engaged physicians are associated with increased retention, decreased medical errors, improved patient-care outcomes and increased cost-effectiveness.4–6 Physicians suffering from burnout, in comparison, are at increased risk for substance use, mental health problems, decreased professionalism and increased risk of patient safety events.2,7,8 Highly engaged physicians are theorized to have the opposite characteristics of burnout.9 Recent literature has therefore shifted focus to find strategies to improve physician engagement rather than decreasing physician burnout.2,5,10–13 Improving physician engagement may become even more crucial due to the COVID19 pandemic, which disrupted the personal and professional lives of physicians and led to increases in physician attrition.14–16
The Maslach Burnout Index (MBI) is a nationally recognized, validated survey which identifies physicians at risk for burnout and also measures engagement in work. It can be used in combination with the Areas of Worklife Survey (AWS), a validated survey which identifies worklife areas within the work environment that may be key indicators affecting physician engagement.9 Organizational strategies to address worklife areas may be more effective than addressing individual characteristics (such as age or gender) or addressing individual strategies (such as yoga or meditation) in influencing physician engagement.7 Identifying specific worklife areas most associated with physician engagement or intent to leave a current practice setting may provide organizations with more clarity on how to prioritize resources to improve physician engagement and retention.
To our knowledge, there is limited literature identifying worklife areas most associated with physician engagement or intent to leave practice. No previous studies have explored these associations in general pediatric faculty practicing in the United States, although associations between worklife areas and physician engagement have been explored in other subspecialties.17,18 It is also unclear whether stressors such as the COVID19 pandemic may change physician perceptions of their worklife environment.
Our objective was to examine faculty engagement in a pediatric department at a tertiary-care children’s hospital impacted by a COVID19 surge, and to explore demographic and professional characteristics and worklife areas most associated with physician engagement.
Materials and Methods
Context and Study Design
This was a cross-sectional survey of pediatric faculty at an academic, urban, tertiary-care children’s hospital located in New York City and conducted in September 2020, five months after a COVID19 surge in April 2020. During the COVID19 surge, faculty were deployed to care for adult and pediatric COVID19 patients,19 deployed to care for convalescent adult COVID19 patients in temporary units, joined a palliative telehealth team,20 or were shifted to outpatient telehealth care. At the time of survey administration, faculty were no longer deployed, the average COVID19 census was low (less than 5 admissions daily), and outpatient clinics had reopened. This survey was administered as part of a departmental effort to monitor physician well-being and used a convenience and voluntary sampling approach. All pediatric faculty working at our institution in September 2020 were invited to participate in the survey, and completion of the survey indicated consent to participate.
Eligible participants were identified from a department list of currently employed pediatric faculty and staff, including nurse practitioners, physician assistants and affiliated faculty, such as pediatric surgeons who held appointments in both departments of surgery and pediatrics. These participants were then emailed a link to the survey with a cover letter explaining the purpose of the survey and included details of informed consent to participate in the study. The cover letter explained that completion of the survey indicated consent to participate. Inclusion criteria were participants who self-identified as holding a rank of instructor or above. Participants who reported having no faculty rank or did not know their rank were excluded as they were less likely to share workplace stressors with pediatric faculty. Of note, this survey was the third in a series of cross-sectional surveys evaluating well-being in pediatric faculty, which was published previously.21 This study was approved by the Institutional Review Board at Albert Einstein College of Medicine (Bronx, NY), which reviews research protocols to ensure that they comply with United States federal regulations and ethical principles for human subjects, including the Declaration of Helsinki.
Survey Content
This 72-question survey included three sections. The first section included the AWS, a 28-question validated survey assessing six key organizational areas of the work environment (worklife areas) affecting engagement.9 The second section included the validated Maslach Burnout Inventory-Human Services Survey (MBI-HSS) for Medical Personnel. This is a 22-question survey to measure burnout and engagement in individuals working in healthcare. The third section assessed demographic and professional (work-related) characteristics, including age range, race/ethnicity, gender, faculty rank, responsibility for dependents, and intent to leave academic medicine or the organization. Finally, due to the unique timepoint of the survey, we included questions related to the pandemic, such as whether participants had difficulty meeting work commitments since the COVID19 pandemic.
Measures
The AWS includes six worklife areas (workload, control, reward, community, fairness and values)9 theorized to impact physician burnout and engagement. Each worklife area score is calculated using level of agreement with statements evaluating the participant’s worklife and measured on a 1 (strongly disagree) – 5 (strongly agree) Likert scale. Lower worklife area scores (generally <3 out of 5, in the lowest 25th percentile of the general population) suggest higher dissatisfaction or problems in a worklife area, such as unmanageable workload, limited control in their work, or feeling unrecognized and unrewarded in their work.9,17
The MBI-HSS utilizes three subscales to measure engagement. Emotional Exhaustion (EE) measures feelings of stress or exhaustion, Depersonalization (DEP) measures low enthusiasm and feelings of detachment, and Personal Accomplishment (PA) measures feelings of competency. Scores are calculated using self-reported frequency of symptoms on a 0 (never) to 6 (every day) Likert scale. Mean scores of each subscale for each participant are calculated with cutoffs determined by population norms. Engaged participants are defined as those with EE score less than or equal to 3.0, DEP score less than or equal to 2.73, and PA greater than 4.66. Participants who met all three cutoffs on these subscales were defined as engaged (ie, reporting low emotional exhaustion, low depersonalization, and high personal accomplishment, or the “positive antithesis” of burnout),9 and those who did not meet these cutoffs were defined as not engaged.
As part of the demographics section, we measured whether participants had responsibility for caring for dependents less than 18 years of age. We also measured likelihood to stay at our organization. Response options to this category included “extremely likely, likely, unsure, unlikely, and extremely unlikely”. We initially used a 5 point Likert scale during data collection to ensure we were able to capture the breadth and diversity of faculty perceptions and responses, and then dichotomized responses to this variable during data analysis for ease of interpretation. “Intent to leave the organization” was defined as faculty who reported that they were “extremely unlikely”, “unlikely”, or “not sure” to stay at our organization. “No intent to leave the organization” was defined as faculty who reported they were “likely” or “extremely likely” to stay at our organization.
To measure the impact of the COVID19 pandemic further, the survey also assessed whether the demands of family or personal life made it more difficult for faculty to meet work commitments since the start of the pandemic. Response options included “never”, “rarely”, “some of the time”, and “a great deal of the time.” We defined “difficulty meeting work commitments” as faculty who reported difficulty meeting work commitments “some of the time” or “a great deal of the time” since the COVID19 pandemic.
Outcomes
Our primary analysis focused on demographic and worklife areas most associated with faculty engagement. Our secondary analysis focused on worklife areas most associated with engagement and intent to leave the organization, when adjusted for age, gender, worklife areas, and other demographic factors.
Statistical Analysis
Univariate analyses were performed to summarize demographic and areas of worklife variables. Variables were assessed for normality to ensure validity of statistical assumptions. Continuous variables were analyzed using Student’s t-test or Mann–Whitney test, as appropriate, to measure associations between survey demographics and faculty demographics and between demographic or areas of worklife variables and faculty engagement. Categorical variables were analyzed using chi-square or Fisher’s Exact tests to measure association between demographic variables or areas of worklife variables and faculty engagement, as appropriate.
A logistic regression model was developed with faculty engagement and intent to leave the organization as outcomes. Variables with p values <0.25 found on bivariate analysis or thought to be clinically significant were entered into the model. Three participants who self-identified as “other” or “non-binary” for gender were not included in the logistic regression analysis. In both regression models, we initially controlled for all areas of worklife, faculty rank, impact of the COVID19 pandemic, responsibility for dependents <18 years of age, and age range, gender, and ethnicity. Based on selection at p<0.05 significance, we excluded areas of worklife and exploratory demographic variables that were not statistically significant to the model, while variables thought to be clinically significant (such as age range and gender) remained in the final model. A final etiologic model was constructed to assess for demographic or worklife variables that were significantly associated with faculty engagement or intent to leave the organization, after adjusting for age range and gender. All continuous variables in the model were assessed visually to ensure they were being used in their correct functional form in the final model. We also assessed for multicollinearity in our model by using Variance Inflation Factors (VIF) and determined concern for multicollinearity if any variable had a VIF of 10 or above. All statistical analysis was performed using Stata 15.1 (Stata Corp, College Station, TX).
Results
One hundred and thirteen faculty of 275 eligible faculty (41%) responded. When comparing demographics of survey participants and overall faculty, we found differences in rank (56% Instructors or Assistant Professors answered survey versus 69% Instructors or Assistant Professors in overall faculty, p=0.02, Table 1) and race/ethnicity (72% of survey participants self-identified as White versus 54% White in faculty, p<0.01, Table 1). No other significant differences between survey and faculty demographics were found. The majority of our participants were female (66%), White (72%), and held the rank of Assistant Professor (51%). Sixty-two percent of faculty met criteria for engagement, and 23% of our faculty met criteria for intent to leave the organization.
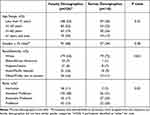 |
Table 1 Faculty and Survey Demographics |
No demographic or professional characteristics were significantly associated with engagement. However, engaged faculty reported significantly higher scores in all worklife areas compared to non-engaged faculty (Figure 1), meaning engaged faculty reported higher satisfaction in all worklife areas. Engaged faculty were also more likely to report that they had no intent to leave the organization (p<0.01, data not shown), and that they had no difficulty meeting work commitments during the COVID19 pandemic (p<0.01, data not shown).
When entered into a logistic model with faculty engagement as the outcome, older participants (those older than 61 years of age) were more likely to be engaged than those less than 41 years of age (OR, 12.8; 95% CI, 1.5–106.6, Table 2). Caregivers of dependents less than 18 years of age were also more likely to be engaged (OR, 19.6; 95% CI, 3.0–127.5). Positive perceptions of workload, control, and community were associated with engagement (OR, 2.83; 95% CI, 1.2–6.9; OR, 3.24; 95% CI 1.4–7.3; OR, 6.07; 95% CI 1.9–18.7, respectively). Those who reported that the COVID19 pandemic created difficulty meeting work commitments were significantly less likely to be engaged (OR, 0.13; 95% CI 0.03–0.57). We also assessed all variables for multicollinearity, which was not present in this final model.
 |
Table 2 Multivariate Odds Ratios for Associations with Increased Faculty Engagementa |
A logistic model analyzing associations with intent to leave the organization as the outcome found that participants aged less than 41 years were more likely to report intent to leave compared to those aged 41–50 years (OR, 0.11; 95% CI 0.02–0.72, Table 3). Positive perceptions of the worklife areas of values and community were associated with decreased intent to leave (OR, 0.07; 95% CI 0.02–0.32, OR, 0.19; 95% CI 0.05–0.78, respectively). Finally, those who reported the COVID19 pandemic created difficulty meeting work commitments were also more likely to report intent to leave the organization (OR, 5.3; 95% CI 1.3–21.0).
 |
Table 3 Multivariate Odds Ratios for Associations with Decreased Intent to Leave Organizationa |
Discussion
We examined demographic and professional characteristics and worklife areas associated with increased engagement at work in pediatric faculty during a highly stressful time (recent COVID19 surge) using a cross-sectional survey. We also examined the association between these worklife areas and intent to leave our organization, which is correlated with work engagement. To our knowledge, no prior studies have examined associations between work engagement and demographic or professional characteristics and worklife areas in pediatric faculty.
Areas most associated with increased faculty engagement in multivariate analyses were positive perceptions of workload, control, and community. These results suggest that faculty who felt that their workload was manageable, that they had autonomy or influence over their work, and that they were part of a supportive work group were most likely to be engaged in their work. Other studies examining physician job satisfaction or well-being, which are associated with engagement,6 also demonstrate that strong peer support22–24 and autonomy at work6,22,25 are important factors for engagement. Organizations with limited resources may consider strategies to improve engagement by prioritizing these three worklife areas: workload, control, and community.
For example, institutions have improved physician workload by studying and improving workflow processes to improve efficiency, such as the use of medical scribes.26,27 The American Academy of Pediatrics (AAP) suggests that allowing physicians more autonomy in their work environment, such as flexible hours or telemedicine, may improve physician well-being.28 Finally, improving collegiality, such as introducing peer mentorship groups or encouraging peer support with group debriefings and reflection, may also improve feelings of community and increase productivity.29,30
Improving engagement may also decrease attrition, as we found that engaged faculty were less likely to report intention to leave the organization. This finding is consistent with prior studies.12,31–33 Rates of intent to leave in our faculty (24%) were similar to studies examining faculty physician intent to leave within 24 months during the COVID19 pandemic.34 We found that alignment of institutional and individual values are important in faculty retention, a finding that is supported by other studies examining faculty retention.35 The worklife area of community was also significantly associated with decreased intention to leave. Organizations that concentrate on improving collegiality, enhancing peer support, and fostering inclusion may be able to improve both faculty engagement and decrease intention to leave.24 Recruiting faculty whose values are consonant with those at the institution may also prevent attrition. Reducing or preventing faculty attrition is particularly critical given increased healthcare worker turnover after the COVID19 pandemic.36
We also found certain demographic characteristics that were associated with increased engagement and/or decreased intent to leave. Increased awareness of specific demographic or professional characteristics may help organizations identify faculty at risk for disengagement and attrition in order to provide increased support to these faculty. Younger participants (those less than 41 years of age in our study) were less engaged and more likely to report intention to leave, consistent with previous studies.6,31 Institutions may therefore benefit from faculty development programs targeting early-career faculty to increase engagement.
We also found that faculty who self-reported being caregivers of dependents <18 years of age were more likely to be engaged, despite literature suggesting work-life conflict may negatively impact physician wellbeing.25 This is not entirely inconsistent with prior literature. A study examining predictors of intent to leave and aspirations to leadership found that women with children and higher faculty rank predicted leadership seeking, which may suggest higher work engagement, although the authors also found negative associations between leadership-seeking and family and work-life conflict in women.37 Our institution does not offer financial support to faculty but did institute a series of peer support groups for faculty with small children immediately after the pandemic surge in New York City, recognizing there may be specific stressors for faculty with small children related to child care, virtual schooling, and reopening of schools. Enhancing options for flexibility at work to decrease work-life conflict, and increasing opportunities to build community, especially in younger faculty, may be important ways to increase engagement at work and to decrease attrition.
Our findings suggest that stressors from the COVID19 pandemic impacted faculty engagement and retention. Faculty who reported that the COVID-19 pandemic created difficulties meeting work commitments were more likely to be disengaged and more likely to report intent to leave the organization. In a cross-sectional study examining COVID-19 related stress in US healthcare workers, Sinsky et al also found that those reporting increased COVID19-related stress, increased fear of COVID-19 exposure or transmission, or high workload were more likely to report intention to leave in the next 24 months.34 Faculty disproportionately impacted by changes secondary to stressful events or disasters such as the COVID-19 pandemic may therefore require increased support from their institutions, such as increased flexibility at work.25,38
Finally, studying faculty engagement can be challenging due to the myriad ways in which faculty engagement is defined or measured.4 Many survey tools and definitions have noted that a physician who is fulfilled, dedicated, and satisfied with their work is likely to be more engaged.2,23,32,33,39–41 However, many surveys evaluating levels of physician engagement do not include the context in which these physicians work, which may lead to challenges with interpreting and generalizing data for use at other organizations.39 We believe one of the strengths of this study is that we were able to measure faculty engagement in the context of faculty worklife environment. Burnout and engagement do not occur in isolation.42,43 Our concurrent examination of faculty engagement and worklife areas may be more useful for organizations to find strategies to initiate appropriate interventions.
Limitations to this study include a sub-optimal response rate, though response rates were similar to those in other physician surveys.34,37 Senior faculty and White faculty were more likely to respond to our survey, which may have impacted our findings. Due to low numbers, we excluded faculty who identified as non-binary. This study was also conducted in a pediatrics department at a single institution located in an urban setting, which may limit its generalizability to other physician specialties or organizations in different settings. Our findings were from a single time-point using a cross-sectional study; however, we found similar patterns with faculty engagement and areas of worklife in subsequent surveys, suggesting consistency and bolstering our findings. Although there are many ways to measure work engagement, our study included just one modality. Finally, this study was conducted during a unique period—recovery from the initial surge of the COVID19 pandemic—and the findings may not be generalizable to other time periods. We theorize it is possible that the COVID19 pandemic may have exacerbated current stressors in the workplace and highlighted influential worklife areas that may be most critical when considering physician engagement and intent to leave.
Conclusion
In a cross-sectional survey examining worklife areas associated with faculty engagement and intention to leave in a pediatrics department impacted by the COVID19 pandemic, we found that positive perceptions of the specific worklife areas of workload, control, and community were highly associated with increased engagement, and that alignment with values and community were highly associated with decreased intent to leave. This study suggests specific target areas which institutions may consider in efforts to enhance physician engagement and retention.
Abbreviations
95% CI, 95% Confidence Interval; AAP, American Academy of Pediatrics; AWS, Areas of Worklife Survey; DEP, Depersonalization; EE, Emotional Exhaustion; MBI, Maslach Burnout Inventory; MBI-HSS, Maslach Burnout Inventory Human Services Survey; OR, Odds Ratio; PA, Personal Accomplishment; VIF, Variance Inflation Factors.
Disclosure
Dr Cabana is a member of the United States Preventive Services Task Force (USPSTF). This manuscript does not necessarily represent the views of the USPSTF. Dr Janet Serwint reports grants from NICHD, HRSA; Associate Editor for Pediatrics in Review Editorial Board, consultant for Cameron Kravitt Foundation, outside the submitted work. The remaining authors report no conflicts of interest in this work.
References
1. Monavvari A. Physician engagement is essential in designing the medical home. Can Fam Physician. 2019;65(9):609–611.
2. Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129–146. doi:10.1016/j.mayocp.2016.10.004
3. Swensen S, Kabcenell A, Shanafelt T. Physician-organization collaboration reduces physician burnout and promotes engagement: the Mayo Clinic experience. J Healthc Manag. 2016;61(2):105–127.
4. Perreira TA, Perrier L, Prokopy M, Neves-Mera L, Persaud DD. Physician engagement: a concept analysis. J Healthc Leadersh. 2019;11:101–113. doi:10.2147/JHL.S214765
5. Milliken AD. Physician engagement: a necessary but reciprocal process. CMAJ. 2014;186(4):244–245. doi:10.1503/cmaj.131178
6. Perreira TA, Perrier L, Prokopy M. Hospital physician engagement: a scoping review. Med Care. 2018;56(12):969–975. doi:10.1097/MLR.0000000000000983
7. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272–2281. doi:10.1016/S0140-6736(16)31279-X
8. Panagioti M, Geraghty K, Johnson J, et al. Association between physician burnout and patient safety, Professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(10):1317–1331. doi:10.1001/jamainternmed.2018.3713
9. Leiter MP, Maslach C. Six areas of worklife: a model of the organizational context of burnout. J Health Hum Serv Adm. 1999;21(4):472–489.
10. Rabkin SW, Dahl M, Patterson R, et al. Physician engagement: the Vancouver Medical Staff Association engagement charter. Clin Med (Lond). 2019;19(4):278–281. doi:10.7861/clinmedicine.19-4-278
11. Kruskal JB, Shanafelt T, Eby P, et al. A road map to foster wellness and engagement in our workplace-A report of the 2018 Summer Intersociety Meeting. J Am Coll Radiol. 2019;16(6):869–877. doi:10.1016/j.jacr.2018.10.025
12. Dandar VM, Field JP, Garrison GE. Promising Practices for Promoting Faculty Engagement and Retention at U.S. Medical Schools. Association of American Medical Colleges; 2017.
13. Stark R. Increasing physician engagement: start with what’s important to physicians. J Med Pract Manage. 2014;30(3):171–175.
14. Creese J, Byrne JP, Conway E, Barrett E, Prihodova L, Humphries N. ”We All Really Need to just Take a Breath”: composite narratives of hospital doctors’ well-being during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(4):2051. doi:10.3390/ijerph18042051
15. Grasso DJ, Lewin MM, Adams B, Lapidus G. Pandemic-related experiences and stress among children’s hospital staff predict psychosocial risk. J Healthc Manag. 2022;67(2):75–88. doi:10.1097/JHM-D-21-00022
16. Abbasi J. Pushed to their limits, 1 in 5 physicians intends to leave practice. JAMA. 2022;327(15):1435–1437. doi:10.1001/jama.2022.5074
17. Verret CI, Nguyen J, Verret C, Albert TJ, Fufa DT. How do areas of work life drive burnout in orthopaedic attending surgeons, fellows, and residents? Clin Orthop Relat Res. 2021;479(2):251–262. doi:10.1097/CORR.0000000000001457
18. Dasgupta S, Dave I, McCracken CE, Mohl L, Sachdeva R, Border W. Burnout and work-life balance among pediatric cardiologists: a single center experience. Congenit Heart Dis. 2019;14(3):350–355. doi:10.1111/chd.12723
19. Philips K, Uong A, Buckenmyer T, et al. Rapid Implementation of an adult coronavirus disease 2019 unit in a children’s hospital. J Pediatr. 2020;222:22–27. doi:10.1016/j.jpeds.2020.04.060
20. Norris SE, Strumph K, Rahmani NE. Pediatric palliative care when COVID-19 positive adults are dying in a children’s hospital. Pediatrics. 2020;146(3). doi:10.1542/peds.2020-1570
21. Uong AM, Cabana MD, Serwint JR, Bernstein CA, Schulte EE. Changes in pediatric faculty burnout during the COVID-19 pandemic. Hosp Pediatr. 2021;11(12):e364–e373. doi:10.1542/hpeds.2021-006045
22. Bunton SA, Corrice AM, Pollart SM, et al. Predictors of workplace satisfaction for U.S. medical school faculty in an era of change and challenge. Acad Med. 2012;87(5):574–581. doi:10.1097/ACM.0b013e31824d2b37
23. Scheepers RA, Lases LSS, Arah OA, Heineman MJ, Lombarts K. Job resources, physician work engagement, and patient care experience in an academic medical setting. Acad Med. 2017;92(10):1472–1479. doi:10.1097/ACM.0000000000001719
24. Schneider A, Weigl M. Associations between psychosocial work factors and provider mental well-being in emergency departments: a systematic review. PLoS One. 2018;13(6):e0197375. doi:10.1371/journal.pone.0197375
25. Webber S, Babal JC, Shadman KA, Coller RJ, Moreno MA. Exploring academic pediatrician perspectives of factors impacting physician well-being. Acad Pediatr. 2020;20(6):833–839. doi:10.1016/j.acap.2020.02.018
26. Gregory ST, Menser T, Gregory BT. An organizational intervention to reduce physician burnout. J Healthc Manag. 2018;63(5):338–352. doi:10.1097/JHM-D-16-00037
27. DeChant PF, Acs A, Rhee KB, et al. Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc Innov Qual Outcomes. 2019;3(4):384–408. doi:10.1016/j.mayocpiqo.2019.07.006
28. Tothy AS. More Control Over Work Environment Can Improve Physical Wellness. AAP News American Academy of Pediatrics; 2020.
29. Schulte EE, Alderman E, Feldman J, et al. Using the “Coach approach”: a novel peer mentorship program for pediatric faculty. Acad Pediatr. 2022;22(7):1257–1259. doi:10.1016/j.acap.2022.03.020
30. Dawson J, McCarthy I, Taylor C, et al. Effectiveness of a group intervention to reduce the psychological distress of healthcare staff: a pre-post quasi-experimental evaluation. BMC Health Serv Res. 2021;21(1):392. doi:10.1186/s12913-021-06413-4
31. Zimmermann EM, Mramba LK, Gregoire H, Dandar V, Limacher MC, Good ML. Characteristics of faculty at risk of leaving their medical schools: an analysis of the standpoint faculty engagement survey. J Healthc Leadersh. 2020;12:1–10. doi:10.2147/JHL.S225291
32. Wai PY, Dandar V, Radosevich DM, Brubaker L, Kuo PC. Engagement, workplace satisfaction, and retention of surgical specialists in academic medicine in the United States. J Am Coll Surg. 2014;219(1):31–42. doi:10.1016/j.jamcollsurg.2014.03.027
33. Rao S, Ferris TG, Hidrue MK, et al. Physician burnout, engagement and career satisfaction in a large academic medical practice. Clin Med Res. 2020;18(1):3–10. doi:10.3121/cmr.2019.1516
34. Sinsky CA, Brown RL, Stillman MJ, Linzer M. COVID-related stress and work intentions in a sample of US health care workers. Mayo Clin Proc Innov Qual Outcomes. 2021;5(6):1165–1173. doi:10.1016/j.mayocpiqo.2021.08.007
35. Sancheznieto F, Byars-Winston A. Value, support, and advancement: an organization’s role in faculty career intentions in academic medicine. J Healthc Leadersh. 2021;13:267–277. doi:10.2147/JHL.S334838
36. Frogner B, Dill JS. Tracking turnover among health care workers during the COVID-19 pandemic: a cross-sectional study. JAMA Health Forum. 2022;3(4):e220371. doi:10.1001/jamahealthforum.2022.0371
37. Ellinas EH, Fouad N, Byars-Winston A. Women and the decision to leave, linger, or lean in: predictors of intent to leave and aspirations to leadership and advancement in academic medicine. J Womens Health (Larchmt). 2018;27(3):324–332. doi:10.1089/jwh.2017.6457
38. Zhang H, Zhao Y, Zou P, Liu Y, Gan L. Engagement among physicians fighting COVID-10: the mediating role of autonomy. Occup Med (Chic Ill). 2020. doi:10.1093/occmed/kqaa203
39. Keller EJ, Giafaglione B, Chrisman HB, Collins JD, Vogelzang RL. The growing pains of physician-administration relationships in an academic medical center and the effects on physician engagement. PLoS One. 2019;14(2):e0212014. doi:10.1371/journal.pone.0212014
40. Loerbroks A, Glaser J, Vu-Eickmann P, Angerer P. Physician burnout, work engagement and the quality of patient care. Occup Med (Lond). 2017;67(5):356–362. doi:10.1093/occmed/kqx051
41. Scher E, Whitehouse S, Van Harn M, et al. Does physician engagement affect satisfaction of patients or resident physicians? J Healthc Leadersh. 2019;11:75–80. doi:10.2147/JHL.S201060
42. Leiter MP, Maslach C. Latent burnout profiles: a new approach to understanding the burnout experience. Burn Res. 2016;3(4):89–100. doi:10.1016/j.burn.2016.09.001
43. Maslach C, Leiter MP. Harvard Business Review. How to measure burnout accurately and ethically. Harv Bus Rev; 2021. Available from: https://hbr.org/2021/03/how-to-measure-burnout-accurately-and-ethically.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

