Back to Journals » Clinical Ophthalmology » Volume 12
Pediatric cataract surgery with hydrophilic acrylic intraocular lens implantation in Nepalese children
Authors Adhikari S , Shrestha UD
Received 23 August 2017
Accepted for publication 2 November 2017
Published 20 December 2017 Volume 2018:12 Pages 7—11
DOI https://doi.org/10.2147/OPTH.S149806
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Srijana Adhikari, Ujjowala D Shrestha
Department of Pediatric Ophthalmology and Strabismus, Tilganga Institute of Ophthalmology, Kathmandu, Nepal
Purpose: To assess the outcome of cataract surgery with hydrophilic acrylic intraocular lens (IOL) implantation in children with congenital and developmental cataracts.
Method: A retrospective review of medical records of children with congenital or developmental cataracts who underwent cataract surgery with hydrophilic IOL implantation, from January 2011 to December 2014 in a tertiary eye hospital in Nepal. Primary posterior capsulotomy, anterior vitrectomy, and IOL implantation was done in children 8 years or younger, while older children underwent only lens aspiration and IOL implantation.
Results: A total of 178 eyes of 120 children underwent cataract surgery with primary IOL implantation. Mean age at the time of surgery was 6.9 years (range: 3 months to 15 years). Average follow-up time was 13.7 (±5.9) months. Associated ocular anomalies were present in 84 (47.1%) eyes. Postoperative complications were found in 33 eyes (18.13%) with inflammatory membrane being the most common (10.1%). Two eyes (1.1%) developed endophthalmitis. Second intervention was needed in 12 (6.5%) eyes. Preoperative vision of less than 6/60 was present in 105 eyes (57.69%). Final best corrected visual acuity of 6/12 or better was found in 81 (44.5%) eyes.
Conclusion: Our study shows that hydrophilic IOL is suitable for use in children. Results of this study are comparable with other studies on pediatric cataract surgeries using hydrophobic acrylic intraocular lenses. Low cost hydrophilic lens implantation is an effective approach in managing pediatric cataract surgery in developing countries like Nepal.
Keywords: pediatric, cataract, hydrophilic, lens, Nepal
Introduction
Pediatric cataracts is one of the leading causes of childhood visual impairment and blindness in developing countries.1 Surgery in children is different compared to their adult counterparts in many ways. To have a good pediatric cataract surgery setup in the developing world is challenging. It needs a skilled surgeon, a very good setup of equipment, good anesthesia, and nursing care. There are many controversies in pediatric cataract management regarding timing of surgery, intraocular lens (IOL) power calculation, and the choice of IOL.2,3 The choice of IOL mainly depends upon factors like material biocompatibility, posterior capsule opacification, size of wound, and the cost of IOL, especially in developing countries like Nepal. Many studies have shown good outcome, both in the older practice of using rigid poly(methyl methacrylate) (PMMA) lenses and the newer hydrophobic lenses in children with cataracts.4–7 However, there is only a handful of studies showing the outcome of hydrophilic lenses in the pediatric age group.8,9 This study describes the outcome of pediatric cataract surgery with hydrophilic IOL implantation in Nepalese children.
Method
This study is a retrospective review of charts of all the children with congenital and developmental cataracts who underwent surgery in Tilganga Institute of Ophthalmology between January 2011 to December 2014. Children with traumatic cataract, complicated cataracts, and secondary IOL implantations were excluded. The study was approved by the Institutional Review Board of Tilganga Institute of Ophthalmology and it adheres to the tenets of the Declaration of Helsinki. Informed consent was obtained from parents of the children included in the study. All the information was collected from the charts including demographics, laterality of cataract, presenting symptoms, associated ocular abnormalities, preoperative and final best corrected visual acuity, postoperative complications, second surgery, and the follow-up time. Visual acuity in children up to 3 years was determined by the central, steady and maintained fixation method. In children 3–6 years old, visual acuity was determined by E chart at 3 m distance with matching optotype and in older children by the Snellen’s acuity chart. Anterior segment examination was done either by the handheld slit lamp (Kowa, Japan) or the operating microscope. Posterior segment examination was done by indirect ophthalmoscope (Heine Optotechnik, Germany) or B scan ultrasound in dense media opacity.
IOL
IOL power calculation was done in all children under general anesthesia by handheld keratometer (Nidek, Aichi, Japan) and A scan (Alcon Laboratories, Inc., Fort Worth, TX, USA). The type of IOL used was poly(2-hydroxyethyl methacrylate) material (poly-hema) with ultraviolet absorber produced in Fred Hollows intraocular lens lab, Tilganga Institute of Ophthalmology. The IOL power was reduced by 20% in children aged 2 years and younger and 10% in children 2–8 years of age.
Surgical technique
The pupils were dilated with a combination of 1% tropicamide and 10% phenylephrine. All the children underwent surgery under general anesthesia. The two ports were made in limbus in 2 and 10 o’ clock position to enter the anterior chamber by using a microvitroretinal blade. The entire surgery was done by an automated vitrectomy machine (Alcon Accurus). Anterior capsule vitrectorhexis and the lens aspiration was done using a 20 gauge ocutome (Alcon Accurus). The 10 o’ clock wound was enlarged with 3.4 mm keratome. IOL implantation was done using an injector. In cases where vitrectomy was indicated, primary posterior vitrectorhexis and anterior vitrectomy were performed done through the same limbal ports using bimanual ocutome and going underneath the IOL. Wound was closed using 8-0 Vicryl sutures. Primary posterior vitrectorhexis and anterior vitrectomy were performed in children 8 years or younger, older children with nystagmus, mental retardation, or those not cooperative enough for the subsequent Yag capsulotomy. Other children underwent only lens aspiration and IOL implantation.
Results
A total of 178 eyes of 120 children were included in the study. Mean age was 6.9 (±3.6 SD). There were eight children below the age of 2 years and four children below 6 months. Male to female ratio was 1.4. On presentation, nystagmus was present in 17.9% and strabismus in 12.3% of eyes. Table 1 shows demographics and clinical characteristics of children. Of 178 eyes, only lens aspiration and IOL implantation was done in 75 (42%) eyes whereas in 103 (58%) eyes lens aspiration and anterior vitrectomy with IOL implantation were carried out. Mean follow-up time was 13.7 (±5.9) months. Postoperative complications were present in 18.3% of operated eyes (Table 2). The most common complication was inflammatory membrane (10%) followed by visual axis opacification (7%). Two eyes developed endophthalmitis. Twelve (6.4%) eyes required second intervention. Out of two eyes with endophthalmitis, one was treated with intravitreal injection, the other needed core vitrectomy (Table 3). Preoperative best corrected visual acuity and the final visual acuity at last follow-up was recorded. In 46 (25%) eyes visual acuity was measured by fixation preference method. Table 4 compares the pre- and postoperative visual acuity in the children. Visual acuity improved from mean logMAR of 1.5 (±0.6) before surgery to 0.3 (±0.2) at the final follow-up. Preoperative vision of less than 6/60 was present in 105 eyes (57.69%). Final best corrected visual acuity of 6/12 or better was found in 81 (44.5%) eyes. Figure 1 shows diagrammatic representation of pre- and postoperative vision compared in these children.
  | Table 1 Demographics and clinical characteristics of children |
  | Table 2 Postoperative complications |
  | Table 3 Second interventions |
  | Table 4 Pre- and postoperative vision |
  | Figure 1 Pre- and postoperative vision compared. |
Discussion
IOL design and biocompatibility plays an important role in visual and surgical outcomes in pediatric cataract.10 Foldable acrylic hydrophobic lenses have been the IOL of choice for many years with good results.11 The rigid gas permeable PMMA lens has also been used by many surgeons, especially in developing countries.12–15 The most important reason being the cost and easy availability. There are studies on the use of PMMA lenses in pediatric cataract surgeries with postoperative outcomes comparable with the foldable acrylic lenses.16 When using PMMA lenses, the wound size needs to be large. So there is chance of induced astigmatism. The use of hydrophilic lenses in the adult population has been reported by many studies, with mixed outcomes.17,18 However, there are very few studies on the use of hydrophilic lenses in a pediatric population. Most of these studies have shown good surgical and visual outcomes in the pediatric population. The Fred Hollows intraocular lens lab has been producing lenses in Tilganga Institute for the last 20 years. However, use of foldable lenses in children has been in practice only recently. It is cheap and easily available for the pediatric population.
Most of the children in our population were in the age group of 2 to 8 years. This indicates late presentation of cataract. The other reason being our practice of only using IOLs around the age of 18 months in bilateral cases. In unilateral cases, we use IOLs at a younger age. Almost 18% of eyes had nystagmus and 10% had already developed strabismus at the time of presentation, also indicating the late presentation of cataract. The follow-up time in our population was shorter than the study done by Kleinmann et al.9 They had a mean follow-up of 47 months. Postoperative complications were found in 18.5% of operated eyes, which is comparable with other similar studies. The rate of visual axis opacification in our study was lower than in the studies done by Kleinmann et al using hydrophilic lenses and Vasavada et al using hydrophobic acrylic lenses.9,19 Contrary to the study done by Kleinmann et al, we have excluded traumatic cataracts. There were 12 children (6.4%) who needed second intervention. Table 5 shows the rate of posterior capsule opacification in studies using hydrophobic lenses compared to our study. Most of the postoperative inflammatory membrane were resolved with frequent prednisolone acetate eye drops. Five of these children received oral corticosteroids. Endophthalmitis is one of the rare complications after pediatric cataract surgery.20,21 Two eyes developed endophthalmitis in our study. Both of these children had poor medication compliance and were living in poor hygienic conditions.
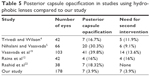  | Table 5 Posterior capsule opacification in studies using hydrophobic lenses compared to our study |
Visual outcomes in our study were similar to the studies done by Kleinmann et al.9 We achieved more than 6/12 vision in 47% eyes. Out of 45 eyes with poor fixation, 30 achieved central, steady, and maintained fixation postoperatively. This result is comparable with Kleinmann et al and Panahi-Bazaz et al’s work.9,10
In conclusion, our study shows that foldable hydrophilic lenses are safe to use in children. Visual and surgical outcomes were comparable with other studies using hydrophobic lenses. A prospective comparative study with hydrophobic acrylic lenses may be considered for future study to reach a conclusion. Managing pediatric cataracts in a low resource setting is challenging. The cost of a hydrophilic lens is US$15–US$20 each, while the cost of a hydrophobic lens is US$100–US$150 each. We locally produce hydrophilic lenses in our IOL lab. Hence, hydrophilic lenses are a cheap, easy, and effective approach to managing pediatric cataract surgeries in developing countries like Nepal.
Acknowledgment
This paper was presented at the 43rd annual meeting of American Association of Pediatric Ophthalmology and Strabismus, Vancouver, Canada as an e poster presentation. The poster’s abstract was published in “e Posters” Journal of American Association of Pediatric Ophthalmology and Strabismus (JAAPOS), August 2016, volume 20, issue 4.
Disclosure
The authors report no conflicts of interest in this work.
References
Foster A, Gilbert C, Rahi J. Epidemiology of cataract in childhood: a global perspective. J Cataract Refract Surg. 1997;23 Suppl 1:601–604. | ||
Lloyd IC, Ashworth J, Biswas S, Abadi RV. Advances in the management of congenital and infantile cataract. Eye (Lond). 2007;21(10):1301–1309. | ||
Vasavada AR, Nihalani BR. Pediatric cataract surgery. Curr Opin Ophthalmol. 2006;17(1):54–61. | ||
Trivedi RH, Wilson ME Jr. Single-piece acrylic intraocular lens implantation in children. J Cataract Refract Surg. 2003;29(9):1738–1743. | ||
Nihalani BR, Vasavada AR. Single-piece AcrySof intraocular lens implantation in children with congenital and developmental cataract. J Cataract Refract Surg. 2006;32(9):1527–1534. | ||
Rowe NA, Biswas S, Lloyd IC. Primary IOL implantation in children: a risk analysis of foldable acrylic v PMMA lenses. Br J Ophthalmol. 2004;88(4):481–485. | ||
Aasuri MK, Fernandes M, Pathan PP. Comparison of acrylic and polymethyl methacrylate lenses in a pediatric population. Indian J Ophthalmol. 2006;54(2):105–109. | ||
Panahi-Bazaz MR, Zamani M, Abazar B. Hydrophilic acrylic versus PMMA intraocular lens implantation in pediatric cataract surgery. J Ophthalmic Vis Res. 2009;4(4):201–207. | ||
Kleinmann G, Zaugg B, Apple DJ, Bleik J. Pediatric cataract surgery with hydrophilic acrylic intraocular lens. J AAPOS. 2013;17(4):367–370. | ||
Wilson ME, Elliott L, Johnson B, Peterseim MM, Rah S, Werner L, Pandey SK. AcrySof acrylic intraocular lens implantation in children: clinical indications of biocompatibility. J AAPOS. 2001;5(6):377–380. | ||
Tuncer S, Gucukoglu A, Gozum N. Cataract extraction and primary hydrophobic acrylic intraocular lens implantation in infants. J AAPOS. 2005;9(3):250–256. | ||
Raina UK, Mehta DK, Monga S, Arora R. Functional outcomes of acrylic intraocular lenses in pediatric cataract surgery. J Cataract Refract Surg. 2004;30(5):1082–1091. | ||
Hennig A, Schroeder B, Gilbert C. Bilateral pediatric cataract surgery: outcomes of 390 children from Nepal and Northern India. J Pediatr Ophthalmol Strabismus. 2013;50(5):312–319. | ||
Wilson ME, Hennig A, Trivedi RH, Thomas BJ, Singh SK. Clinical characteristics and early postoperative outcomes of pediatric cataract surgery with IOL implantation from Lahan, Nepal. J Pediatr Ophthalmol Strabismus. 2011;48(5):286–291. | ||
Thakur J, Reddy H, Wilson ME Jr, et al. Pediatric cataract surgery in Nepal. J Cataract Refract Surg. 2004;30(8):1629–1635. | ||
Küchle M, Lausen B, Gusek-Schneider GC. Results and complications of hydrophobic acrylic vs PMMA posterior chamber lenses in children under 17 years of age. Graefes Arch Clin Exp Ophthalmol. 2003;241(8):637–641. | ||
Kugelberg M, Wejde G, Jayaram H, Zetterström C. Two-year follow-up of posterior capsule opacification after implantation of a hydrophilic or hydrophobic acrylic intraocular lens. Acta Ophthalmol. 2008;86(5):533–536. | ||
Heatley CJ, Spalton DJ, Kumar A, Jose R, Boyce J, Bender LE. Comparison of posterior capsule opacification rates between hydrophilic and hydrophobic single-piece acrylic intraocular lenses. J Cataract Refract Surg. 2005;31(4):718–724. | ||
Vasavada AR, Trivedi RH, Nath VC. Visual axis opacification after AcrySof intraocular lens implantation in children. J Cataract Refract Surg. 2004;30(5):1073–1081. | ||
Agarkar A, Desai R. Endophthalmitis after cataract surgery in children. J AAPOS. 2015;19(4):e34–e35. | ||
Smith J, Poulose A, Olitsky SE. Endophthalmitis following pediatric cataract surgery with a good outcome. J Pediatr Ophthalmol Strabismus. 2006;43(4):239–240. | ||
Rashid R, Hassan J, Afzal F, et al. Management of pediatric cataract with acrylic foldable intraocular lens: our experience. Chattagram Maa-O-Shishu Hospital Medical College Journal. 2013;12(1):25–29. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
