Back to Journals » Chronic Wound Care Management and Research » Volume 8
Pathological Scar and Its Associated Factors Among Survivor of Burn Victim Pediatrics Admitted to South Gondar Zone Public Hospitals, Amhara Regional State, Ethiopia, 2020 – A Multi-Center Cross-Sectional Study
Authors Tiruneh CM , Belachew A , Mulatu S , Desie T , Abate MW , Nigat AB , Tibebu NS , Walle BG, Tigabu A , Belete A
Received 1 June 2021
Accepted for publication 8 July 2021
Published 16 July 2021 Volume 2021:8 Pages 13—19
DOI https://doi.org/10.2147/CWCMR.S322794
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Marco Romanelli
Chalie Marew Tiruneh,1 Amare Belachew,2 Sileshi Mulatu,2 Tigabu Desie,1 Moges Wubneh Abate,3 Adane Birhanu Nigat,3 Nigusie Selomon Tibebu,1 Belete Gelaw Walle,4 Agimasie Tigabu,3 Amsalu Belete5
1Department of Pediatrics and Child Health Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia; 2Department of Pediatrics and Child Health Nursing, College of Medicine and Health Sciences, Bahr Dar University, Bahr Dar, Ethiopia; 3Department of Adult Health Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia; 4Department of Pediatrics and Child Health Nursing, College of Medicine and Health Sciences, Wolayta Sodo University, Wolayta Sodo, Ethiopia; 5Department of Integrated Clinical and Community Mental Health, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
Correspondence: Chalie Marew Tiruneh
Debre Tabor University, P.O.Box 272, Ethiopia
Tel +251918057611
Email [email protected]
Introduction: Burn is a severe type of traumatic injury, which can lead to deformity, disability, or death, and remains a significant health problem worldwide. It is one of the leading causes of morbidity and mortality among Ethiopian children, as many hospitals are lacking a well-equipped and prepared burn center. Children under the age of 15 are at increased risk of burn-related complications. Because they may not be able to escape from the burning object, they often experience a long duration of contact with the hot substance, with a resultant deep burn injury and death.
Methods: Institutional cross-sectional study was used to study 375 hospitalized burn injury survivor pediatrics from 2015 to 2019. A simple random sampling method was used to select participants. Data were exported from Epidata version 4.6 to SPSS version 25 for analysis. In multivariable analysis, significant of the variables were considered at p-value of ≤ 0.05.
Results: In total, 353 were included in the study. Of 353 burn injury survivors, the prevalence of pathological scar was 125 (35.4%). In multivariable analysis, depth of burn injury, time since burn injury, a patient who have a referred to physiotherapy by the surgeon, and surgical procedure is done after burn were statistically significant with a complication of burn injury survivors.
Conclusion and Recommendation: This study revealed that the burden of pathological scar among survivors of burn injury was unacceptably high, which needs intervention from the concerned bodies. Since this high burden of complication might result from the limitation of applying Interburn recommendation, the Amhara regional health bureau and the South Gondar health department shall work in collaboration with Interburn to provide essential burn care and advanced burn care training for health care providers. The timely intervention of those who have a second- and third-degree burn, promoting early presentation to hospital, providing appropriate physiotherapy, and proper care for those who have surgical intervention may help to decrease pathological scar for burn victim children.
Keywords: burn injuries, pathological scar, pediatrics, South Gondar, Ethiopia
Introduction
Burn is a severe type of traumatic injury that can lead to deformity, disability, or death, and remains a significant health problem worldwide.1 The burn wound is dynamic, and progressive dermal ischemia can result in deeper injuries than originally were apparent.2 Because the treatment of burn demands many hours of wound care from nursing staff and possibly one or multiple surgical procedures, hospitalization costs associated with burn care are extremely high.3 Moreover, this results in a high proportion of disfigurement and impaired function for many burn victims, which may be lifelong, and returning to society with these handicaps can be extremely stressful particularly for children.4–6
For example, children under the age of 15 are at increased risk of burns and related complications. Children account for almost half of the population with severe burn injuries. Because they may not be able to escape from the burning object, they often experience a long duration of contact with the hot substance, with a resultant deep burn injury and death.4,7
Evidence from burn injury survivors in America indicated that 23% of victims developed at least one contracture at hospital discharge.8 In another observational study conducted in Mekelle Ayder referral hospital, complications among burn victim pediatrics population were 17.2%, from which 1.3% were death while the other was physical complication occurs among survivors.9 Similarly, a study conducted in Bahir Dar showed that overall complication among burn victim-survivor was 33.3%.10
Cause of burn, age of the victim, length of hospital stay, treatment time after injury, depth of burn, and total body surface area burn were factors associated with complications among survivors of burn injury pediatrics population.5,6,8,9,11
Although it might be under-reported or not documented, burn due to various accidents is ubiquitous among Ethiopian pediatrics. It is one of the leading causes of morbidity and mortality among Ethiopian children as many hospitals are lacking a well-equipped and prepared burn center. Even though Interburn was invited by the Ethiopia ministry of health in 2014 to assess burn strategy and national burn services, the application of recommendations on strategic planning, training and education, prevention, and research into burn injuries are still low.12
There are only a few studies conducted on the epidemiology of burn in the general population in Ethiopia,13–15 while very little is known about pathological scar and associated factors among survivors of the burn victim pediatrics population. So far, no researches have been conducted in our study area about pathological scar among survivor of burn injury in the pediatric population. However, different observations in this area showed burn as one of the leading causes of disability and disfigurement in the pediatric age group. Thus, this study aimed to assess pathological scar and its associated factors among survivors of burn injury in the pediatric age group (age less than fifteen years old) admitted to the south Gondar zone public hospital.
Methods
Study Setting and Design
The study was conducted from January to march at south Gondar Zone public Hospitals, Amhara Regional State, Ethiopia. South Gondar zone is one of the zones’ in the Amhara region, which is located in the Northern part of Ethiopia. Currently, there are 8 governmental hospitals and 94 functional health centers. All burn victim pediatrics (age less than fifteen years old) who fulfill the admission criteria were admitted to a general ward and there are no burn unit centers in all hospitals. In these hospitals, all burn patient who fulfills the admission criteria is admitted to the surgical ward and managed by the general surgeon.
Sample Size Determination
The sample size was determined by using the single population proportion formula with the assumptions of prevalence (P) 33.3%, which is the proportion of complication among pediatrics burn victims in Bahir Dar,10 level of confidence (CL), 95%, a margin of error (d) =5%, and adding 10% contingency gave the final sample equals to 375.
Sampling Technique and Procedure
There are eight public hospitals in the study area. After taking Ethical clearance from Bahir Dar University, Institutional Health Research Ethics Review Committee (ethical protocol number of 0065/2020), all burn victim pediatrics medical registration numbers in the selected hospitals were taken from the registration book, and study subjects were allocated to each hospital with probability proportional to the size of the victim. The sampling frame was prepared based on the victims’ medical registration numbers who were admitted from 2015 to 2020 in the study area. Then, a simple random sampling technique was used to select study subjects, which is the sample, was selected among all burn victim pediatrics in the sampling frame by lottery method.
Inclusion Criteria
Burn victim pediatrics who visited selected hospitals in the study period.
Exclusion Criteria
Lost of chart and missing of the major variable like cause of burn, degree of burn, percentage of burn area were excluded from the study.
Data Collection Tools and Methods
The data were collected and registered by using a structured checklist. The authors prepared the checklist by reviewing different literature done on the same problems.8–10,16–19 The checklist was focused on socio-demographic characteristics of an injured child, burn-related factors, treatment-related factors, and outcome-related factors. Eight trained BSc nurses who were working on the site other than the study setting were involved in the data collection and were supervised by four physicians who were also not a member of the study setting. The record of the victims was reviewed on chart and observation was made to check the presence or absence of a pathological scar by contacting the victim by their recorded address.
Operational Definition
Pathological scars are characterized by excess collagen deposition, resulting in a thick, non-pliable defect that can cause itch, pain, and contractures, limiting functionality.20
Data Processing and Analysis
Data were coded, filtered, and entered into Epi data version 4.6, then exported to SPSS version 25 for analysis. Binary logistic regression analysis was used to determine the association between the dependent and independent variables. Firstly, bivariable logistic regression was performed and all variables with P ≤ 0.25 in the bivariable analysis were included in the final model of multivariable analysis in order to control all possible confounders. The goodness of fit was tested by Hosmer-Lemeshow statistic and the data were fit to the model. The direction and strength of statistical association were measured by the odds ratio with 95% CI. The adjusted odds ratio along with 95% CI were estimated to identify factors associated with complications by using multivariable analysis in binary logistic regression. Finally, P-value < 0.05 was considered to declare as a statistically significant.
Result
Socio-Demographic Characteristics of Burn Victim Patients
From 375 charts, 353 were included in the study with a response rate of 94.1%. Almost half (50.1%) of the participants were female and the age ranged from 1 year to 14 years with a median age of three years. The interquartile range of the participant was three.2,6 Two hundred forty-nine (70.5%) burnt children were from a rural residency. Of the total study participants, 30% were community-based medical insurance users. Three hundred twenty-seven (92.6%) of the participants were exposed to burn at home. Regarding intention of injury, about 98% of the victims were exposed to burn accidentally (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Survivor of Burn Victim Pediatrics Admitted to South Gondar Zone Public Hospitals, Amhara Regional State, Ethiopia, 2020 |
Clinical and Time-Related Factors
Scald was responsible for 72.2% of burn injuries for the victim. Of 353 victims, 33.1% were injured in the summer. Fifty-nine (16.7%) of the injured were presented to the hospital after 24 hrs of injury. About 27 (7.6%) of the injured had poor clinical conditions like derangement of vital signs and decreased level of consciousness at the time of hospital arrival. Of all injured children, 77.6% had second-degree burns and 15.3% had total body surface area burnt greater than 20%. Eighty-six (24.4%) of the injured children developed an infection of the burn wound (Table 2).
 |
Table 2 Clinical and Time Related Factors of Survivor of Burn Victim Pediatrics Admitted to South Gondar Zone Public Hospitals, Amhara Regional State, Ethiopia, 2020 |
Management-Related Factors
About 27% of the injured did not get any first aid measure before hospital arrival. Seventy-one (20.1%) did not take fluid after admission to the hospital. Only 4% of the victims got wound care frequency three times per day. Regarding ointment applied on burn wounds, 54.7% of the victims were treated with Nitrofurazone. Of all admitted burns, 211 (59.8%) were managed with antibiotics and 138 (39.1%) were managed by surgical intervention. Out of the total burn victims, 12.2% were referred to physiotherapy. Antibiotics were administered to 59.8% of the victims (Table 3).
 |
Table 3 Management Related Factors of Survivor of Burn Victim Pediatrics Admitted to South Gondar Zone Public Hospitals, Amhara Regional State, Ethiopia, 2020 |
Management Outcomes of the Injured Pediatrics
Of 353 burn injury survivors, 125 (35.4%) of them develop a pathological scar. Of 125, who develop a pathological scar, 52% have occurred in male burn victim pediatrics. Ninety-seven (77.6%) of pediatric burn victims who develop pathological scars was from rural residency and 31.2% of them did not get any first aid measure before hospital arrival. From burn victim pediatrics who develops a complication, 35.2% managed by once-daily wound care. Seventeen (13.6%) of burn victim pediatrics who develop pathological scar had a depth of the third-degree burn and 20.8% of them had total body surface area burned greater than 20%.
Forty-five (36%) of the pediatrics who develop pathological scar present to the hospital after 24hrs of injury and 40% of them develop an infection in the burn wound. Of those who develop a pathological scar, 61.6% was managed by surgical intervention (Table 4).
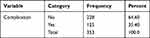 |
Table 4 Management Outcomes of Survivor of Burn Victim Pediatrics Admitted to South Gondar Zone Public Hospitals, Amhara Regional State, Ethiopia, 2020 |
Factors Associated with a Complication for Burn Injury Survivors
In multivariable analysis, depth of burn injury, time since burn injury, physiotherapy indicated victim, and surgical procedure done after burn were significantly associated with a pathological scar results from burns injury.
Those burn victim pediatrics, who had third-degree burn injury were five folds (AOR 5.071; 95% CI 1.498–17.167) of having a pathological scar compared to first-degree burn injury, while those who had second-degree burn injury had 2.4 folds (AOR 2.3981; 95% CI =1.000–5.753) of having a pathological scar. Those burn victim pediatric population who presented to hospital after 24hrs of burn injury had about five times (AOR; 5.377, 95% CI; 2.643–10.940) chance of developing a pathological scar than those who present to a hospital within 24hrs of injury. The odds of a pathological scar in pediatrics who have referred to physiotherapy were about four times (AOR; 3.768, 95% CI; 1.697–8.369) compared to those who did not have indication physiotherapy. Moreover, the odds of a pathological scar in burn victim children who had surgical intervention were four times (AOR; 4.194, 95% CI; 2.474–7.110) than those who had not surgical intervention (Table 5).
Discussion
According to this study, the prevalence of a pathological scar among survivors of burn injury was 35.4% (95% CI=30.6–40.2). In this study, the total complication is in line with the study conducted in Bahir Dar.10
However, the finding is higher than the study conducted in Addis Ababa,21 Mekelle,9 and America.8 The reason for the discrepancy is due to the study conducted in Addis Ababa and Mekelle were conducted in specialized referral hospitals, which have better facilities to manage burn injury than our study setting, which is a district hospital with a poor facility to manage burn injury. On the other hand, the discrepancy between the results of this study with America is due to the difference in socioeconomic status between the study areas.
On the other hand, this study revealed that a pathological scar among survivors of burn injury were lower than the study conducted in Ghana.11 The discrepancy between the studies is due to the difference in the study setting, which is the study conducted in Ghana is conducted in the second largest referral hospital in the country that was more prone to receive more complicated and severe burn cases among which the proportion of complication might be higher. On the other hand, in our study setting, more complicated and severe burn cases were referred to higher health institutes and complications might be lower in the study area.
Finding in this study revealed that those burn injury survivors who have second and third-degree burn has more likely to have a pathological scar than those who have first-degree burns. This is in line with a study conducted in Ghana.11 This is due to the scientific justification of those who have second or third-degree burn is an indicator for the severity of burn injury, which may have a probability of complication.
Those survivors of burn victim pediatrics who presented after 24 hours of burn injury were more likely to have a pathological scar as compared to those who present early. This is due to the increase risk of infection when staying at home without medical care, which increases the risk of developing a pathological scar.22
The result of this study revealed that those survivors of burn victim pediatrics who were referred for physiotherapy secondary to burn injury were more likely to have a pathological scar than those who were not referred for physiotherapy. This is due to those who referred for physiotherapy is an indication of the severity of the injury, which may end up with a pathological scar.
Those survivors of burn victim pediatrics who had surgical intervention were more likely to have a pathological scar than those who had not surgical intervention. This is because most of the surgical procedures done on a burn patient like debridement and skin graft may cause complications on the site of the procedure.
Strength and Limitation of the Study
Strength
Since this was multi-setting study, it provides soundable data than most of the studies conducted in the region.
Limitation
Data incompleteness and absence of charts were reflected in this study.
To contact the victim who had incomplete record of complication, Lack of infrastructure were the main challenge.
Conclusion
This study reveals that the burden of a pathological scar among survivors of burn injury is unacceptably high, which needs intervention from the concerned bodies. Since this high burden of a pathological scar might result from the limitation of applying Interburn, recommendation Amhara regional health bureau and South Gondar zone health department shall work in collaboration with Interburn to provide Essential burn care and advanced burn care training for health care providers. Moreover, these concerned bodies shall work to supply adequate human and material resources for hospitals. The timely intervention of those who have a second and third-degree burn, promoting early presentation to hospital, providing appropriate physiotherapy, and proper care for those who have severe burn injury may help to decrease burn-related pathological scar for burn victim children.
Data Sharing Statement
The data set of the current study is not available due to the presence of sensitive participant’s information’s, but it will be available with reasonable requests.
Ethical Approval and Consent to Participate
Ethical clearance was obtained from Bahir Dar University, College of Medicine and Health Sciences, Institutional Health Research Ethics Review Committee (IHRERC) (ethical protocol number of 0065/2020) with the Declaration of Helsinki. A formal letter for permission and support was written to the south Gondar zone public hospital from Bahir Dar University. For review of patient chart, written and signed voluntary consent was obtained from the hospital managers and for clinical observation to check the presence or absence of a pathological scar of burn victim children, parental informed consent was taken. The manager of each hospital and caretakers of burn victim children was informed about the purpose of the study and told that the information obtained from the chart was treated with complete confidentiality.
Acknowledgment
The authors would like to thank all those who participated in the preparation of this manuscript. Special thanks go to Bahir Dar University and Debre Tabor University for facilitating this research. Appreciation and thanks goes also to the South Gondar zone health department, public hospitals, and data collectors for their unreserved help during data collection.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, agreed to the submitted journal, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Peck MD. Epidemiology of burns throughout the world. Part I: distribution and risk factors. Burns. 2011;37(7):1087–1100. doi:10.1016/j.burns.2011.06.005
2. Feck G, Baptiste MS, Tate CL
3. Connor-Ballard PA. Understanding and managing burn pain: part 1. Am J Nurs. 2009;109(4):48–56. doi:10.1097/01.NAJ.0000348604.47231.68
4. Hansbrough JF, Hansbrough Wpediatric burns. 1999;20(4). Available from: http://pedsinreviewaappublicationsorg/. Accessed July 9, 2021.
5. Wallace HJ, Fear MW, Crowe MM, Martin LJ, Wood FM. Identification of factors predicting scar outcome after burn injury in children: a prospective case-control study. Burns Trauma. 2017;5:1. doi:10.1186/s41038-017-0084-x
6. Kee EL, Kimble R, Cuttle L, Stockton K. Scar outcome of children with partial thickness burns: a 3 and 6 month follow up. Burns. 2016;42(1):97–103. doi:10.1016/j.burns.2015.06.019
7. WHO. Factsheet on burns. Available from: http://wwwwhoint/mediacentre/factsheets/fs365/en/.
8. Jeremy Goverman RH, Gibran N, Ryan CM. Pediatric contractures in burn injury: a Burn Model System National Database Study. Burn Care Res. 2017;38:e192–e199.
9. Sielu Alemayehu BA, Kidanu K, Belete T. Management outcome of burn injury and associated factors among hospitalized children at ayder referral hospital, Tigray, Ethiopia. Int J Pediatr. 2019;2020:9.
10. Gessesse FG, Yitayew YA. Epidemiology of burn injury among children’s attended felege Hiwot referral hospital in Bahir Dar Town, Amhara Regional State, Ethiopia, 2017. J Pediatr Neonatal Care. 2020;10(1):
11. Agbenorku P. Burns functional disabilities among burn survivors: a study in Komfo Anokye Teaching Hospital, Ghana. Int J Burns Trauma. 2013;3(2):78.
12. Interburn E. Improving burn care in Ethiopia. 2014.
13. Kidanu M, Amdesilasie F, Kassa A, Tadelle Y, Befekadu M. Patterns of burn injuries in ayder comprehensive specialized hospital: a 5-year Retrospective Study, Mekelle, Ethiopia. East Afr J Health Sci. 2019;1(1):17–27.
14. Wolde A, Abdella K, Ahmed E, et al. Pattern of injuries in Addis Ababa, Ethiopia: a one-year descriptive study. East Cent Afr J Surg. 2008;13(2):14–22.
15. Mehta KA Epidemiology of burns treated by yekatit 12 burn unit 2017.
16. Droussi H, Benchamkha Y, Ouahbi S, et al. Epidemiology and treatment of paediatric burns in a large children’s hospital in Morocco: analysis of 394 cases: Épidémiologie et traitement des brûlures pédiatriques dans un grand hôpital pour enfants au Maroc: l’analyse de 394 cas. Af J Emerg Med. 2013;3(3):110–115. doi:10.1016/j.afjem.2013.04.002
17. Kiragu AW, Dunlop SJ, Wachira BW, Saruni SI, Mwachiro M, Slusher T. Pediatric trauma care in low-and middle-income countries: a brief review of the current state and recommendations for management and a way forward. J Pediatr Intensive Care. 2017;6(01):52.
18. Kliegman R, Blum N, Shah S, Tasker R, Wilson K, Behrman R. Nelson Textbook of Pediatrics. Vol. 21. Philadelphia, PA: Elsevier Inc.; 2019.
19. Sanyang E, Peek-Asa C, Young T, Fuortes L. Child supervision and burn outcome among admitted patients at major trauma hospitals in the Gambia. Int J Environ Res Public Health. 2017;14(8):856. doi:10.3390/ijerph14080856
20. Gauglitz GG, Korting HC, Pavicic T, Ruzicka T, Jeschke MG. Hypertrophic scarring and keloids: pathomechanisms and current and emerging treatment strategies. Mol Med. 2011;17(1–2):113–125. doi:10.2119/molmed.2009.00153
21. Achamyelesh TTB. Magnitude, clinical presentation, and outcome of pediatric burn injuries at yekatit 12 hospital, Addis Ababa, Ethiopia. 2014.
22. Mock C, Peck M, Peden M, Krug E. A WHO Plan for Burn Prevention and Care. Geneva: Switzerland World Health Organization; 2008.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

