Back to Journals » Integrated Pharmacy Research and Practice » Volume 12
Medicines Wastage and Its Contributing Factors in Public Health Facilities of South Gondar Zone, Amhara Regional State, Ethiopia
Authors Guadie M, Asemahagn MA , Tefera A, Melkam W, Habteweld HA , Derebe D
Received 5 May 2023
Accepted for publication 21 July 2023
Published 25 July 2023 Volume 2023:12 Pages 157—170
DOI https://doi.org/10.2147/IPRP.S415375
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Walid Al-Qerem
Muluneh Guadie,1 Mulusew Andualem Asemahagn,2 Abekyelesh Tefera,3 Wondim Melkam,4 Habtemariam Alekaw Habteweld,5 Dagninet Derebe4
1Department of Regional Regulatory Offices, Amhara Health Bureau, Bahir Dar, Ethiopia; 2School of Public Health, Bahir Dar University, Bahir Dar, Ethiopia; 3Department of Pharmacy, GAMBY Medical and Business College, Bahir Dar, Ethiopia; 4Department of Pharmacy, Bahir Dar University, Bahir Dar, Ethiopia; 5Department of Pharmacy, Debre Berhan University, Debre Berhan, Ethiopia
Correspondence: Dagninet Derebe, Email [email protected]
Background: In developing countries like Ethiopia, medicines wastage becomes a major healthcare system challenge. However, data that displayed the type, extent, and contributing factors of medicines wastage were limited.
Methods: A health facility-based explanatory sequential mixed study was conducted from December 2021 to February 2022. One drug and therapeutics committee (DTC) and one store man per health facility, working during the study period were included for their perception of medicines wastage and possible causes. As key informants, 1 Chief Executive Officer (CEO) and 1pharmacy head were also included per facility. In total, 80 participants were included in this study. The quantitative data to determine the magnitude of medicine wastage were collected using a structured interviewer-administered questionnaire and analyzed using SPSS version 25.
Results: The overall medicines wastage in the three consecutive years was 6.3%. The trend over the three years indicated that medicines wastage is 6.5%, 5.9%, and 6.5% in 2011, 2012, and 2013 Ethiopian Fiscal Year (EFY), respectively. The medicine wastage rate has been increasing nearly by 3% between 2011/2012 and 2012/2013. The main sources of wastage of medicines were expiry (99.3%). The perceived reasons for such medicine’s wastage were near-expiry medicines (< 6 months) being delivered to the health facilities by suppliers, poor communication and coordination with key stakeholders, and the presence of overstocked medicines due to improper forecasting of need in the facilities.
Conclusion: There is an excessive rate of medicines wastage which needs immediate mitigation by exchanging nearly expired medicines with other health facilities, communicating with suppliers and even prescribers, using auditable pharmaceutical transactions and services (APTS), providing continuous training, pursuing quality and safety medicines reuse scheme, implementation of pharmacist waste-reducing activities in all stages of the pharmaceutical supply chain, reducing medication amounts in stock, and through the use of electronic stock management tools.
Keywords: medicines wastage, contributing factors, public health facilities
Background
In the process of ensuring the availability of medicines to the population, there is a possibility that these medicines may be damaged or expired and become unsafe for use.1 In addition, medicines leftover from patients and those identified to be defective may accumulate over time adding to the stock of unsafe-for-use medicines. The resulting stockpiling of these unfit-for-use medicines is usually called medicines waste.2
According to World Health Organization (WHO), medicines wastage is defined as unwanted medications which include expired, unused, spilled, and contaminated medicines that are no longer required and need to be disposed of appropriately.3 Medication waste can occur in all stages of the pharmaceutical supply chain and it involves various stakeholders in the medication supply chain, from manufacturer to patient, contributing to medication waste.4,5 It may occur due to various factors, such as mismanagement of drugs and inadequate governance.6 Supply chain inefficiencies at healthcare facilities have been causing substantial resource wastage due to factors such as product expirations, theft, and damage. Moreover, the absence of adequate transparency and accountability in managing medicines and financial transactions has led to a risk of theft and misappropriation of resources.7
Ethiopia developed a national medicine policy in 1993 that guides the country’s pharmaceutical sector and to establish a structured approach to the supply and distribution of medicines, as well as to guarantee access to essential medications.8
The Ethiopian medication supply chain faces several challenges that require strategic intervention. These include frequent stockouts of medications, medicine wastage due to theft, damage, and expiration, lack of transparency and accountability in medication transactions and service delivery, poor supplier performance, long procurement lead times for certain drugs, inadequate record-keeping and low-quality data, insufficient vehicles to distribute medication from healthcare centers to health posts, inadequate support, and follow-up mechanisms, lack of performance monitoring and evaluation systems, training gaps, and high staff turnover.9 In response to these challenges, the Ethiopian government has launched various strategic initiatives, such as health sector transformation plans aimed at improving the medicine supply chain system.10
Medicines wastage emerges as one of the major healthcare systems problems worldwide that jeopardize the budget of pharmaceuticals.11 In developed nations like the USA, medicines wastage reaches 23%.12 In developing countries like Ethiopia and Ghana medicine wastage varies between 3.68% and 10% respectively.13,14 Public dispensaries in Ghana contributed to 10% of wasted medicines due to expiry. According to a study done at Dessie, Ethiopia, approximately 3.68% of medicines having an estimated cost of USD 159,762.6, were recorded as wastage, of which the majority (92.05%) were due to expiry. Determinant factors of medicines waste were the availability of training, labeling of medicines, waste segregation at the dispensary unit, and the presence of a plan for pharmaceutical disposal.13
Pharmaceutical wastes may result in many disease conditions like salmonellosis, and cholera in people handling these wastes or in those who are living at sites where this pharmaceutical wastage gets discharged. Worldwide, the yearly recorded death from waste-related diseases exceeds 5.2 million people, of which 4 million are children and this disaster will likely become worsen unless a proper intervention is not designed.15–17
Wastage of medicines can pose the community with a pronounced health problem by endangering the environment and human life and wasting available resources. It compromises the quality of care provided to the community by limiting the number of available medicines. It can also result in further compromisation of the overall healthcare system.15,18
Reports in Ethiopia indicated that the wastage of medicine is continuously challenging the pharmaceutical supply chain management. For instance, in 2003, a report from the national assessment that medicines wastage due to expiry reaches 8%.10 In Ethiopia, the practice of documenting wasted medicines is poor for several reasons. These may include a lack of health facilities accountability, systems, and tools helpful for documenting and reporting wasted medicines in the country.19 Another study in Ethiopia revealed that suppliers issuing pharmaceuticals beyond or without health facility needs and requests due to the absence of communication between health facilities and suppliers, failure to adhere to the principle of first expired first out during issuing pharmaceuticals from the store to other dispensing units, lack of adequate pharmacy professionals and inadequate monitoring of the supply chain management as a contributing factor of medicines wastage in addition to a budget shortage, medicines stock out and store congestion.20
Although there are studies that support the prevalence of medicines wastage in Ethiopia, there is a continuous quote to know the extent and type of medicines wasted and its determinants in South Gondar. Therefore, the current study planned to assess the type and extent of waste of medicines and its contributing factors in public health facilities of South Gondar zone, Amhara Regional State, Ethiopia. Knowing the burden and contributing factors of medicines wastage would help the regional health bureau and Ministry of Health to design strategies helpful for curtailing the burden of medicine wastage and ensuring their appropriate use. The evidence from this study would have a positive impact on the healthcare delivery systems of the area, and the nation at large. Moreover, the finding of this study will also serve as baseline information for future studies.
Methods and Materials
Study Area and Period
The study was conducted in public health facilities at South Gondar Zone, Amhara Regional State from December 2021 to February 2022. Debre Tabor town is serving as the capital of this zone, and is located 702 KM away from Addis Ababa the capital city of Ethiopia. This zone has 3 town administrations, 12 woredas, and 269 kebeles (the smallest administrative unit of the governmental structure). Currently, this zonal health department has 7 government hospitals, 95 health centers, 268 health posts, 8 pharmacies, 56 drug stores, and 8 rural drug vendors.
Study Design
A facility-based mixed study was conducted in the public health facility of South Gondar Zone, Amhara regional state, Ethiopia.
Source Population
All health professionals and documents related to wasted medicines like the wasted medicines registration/disposal report and model 19 found in the public health facility of South Gondar Zone.
Study Population
All health professionals taking part in a role in pharmaceutical supply chain management tasks and all recorded documents of wasted medicines/disposal report and model 19 of the year 2011 EFY-2013 EFY in health facilities being sampled.
Inclusion and Exclusion Criteria
Inclusion Criteria
All public health facilities having a history of more than 3 years of operation, public health professionals who had more than 6 months of work experience and who are engaged with medicines and working in selected public health facilities during the study period, value of medicine wasted with their price recorded from 2011EFY-2013EFY were included in the present study.
Exclusion Criteria
Program and donation medicines that are wasted and recorded as free of price were excluded from the study. Public health facilities that were distracted by the recent war between the Tigray People Liberation Front (TPLF) and the federal government of Ethiopia are also excluded from the study.
Variables of the Study
The magnitude of medicines wastage valued in terms of money is the dependent variable, and variables related to supply management (provision of medicines without needs and requisition, irrational procurement, provision of non-selected drugs), storage conditions (overstocking, poor ventilation and exposure to sunlight), inventory related (poor quantification and forecasting of medicines, pilferage of highly potent medicines, poor stock management), communication associated (negligence to monitor stocks, use bin and stock card, poor event documentation) human resources related (inadequate number of professionals for monitoring, absence of knowledgeable and skilled pharmacy personnel in pharmaceutical supply management) are the independent variables of the study.
Operational Definitions
Medicines wasta − A term used to describe damaged, expired, lost, unused and obsoleted medicines.
Medicines wastage rate – It is a calculated percentage obtained from dividing the wasted value in monetary forms by the total value of medicines received during the same year.
Sample Size Determination and Sampling Techniques
The size of public healthcare facilities to be included in the study were determined by applying the Logistics Indicators Assessment Tool (LIAT).9 The document recommended that at least 15% of the targeted health facilities shall be included in the survey. However, the current study adopted to use 20% (to be more representative) of the 96 health facilities excluding health posts in the south Gondar zone (20 health facilities) owing to budget and time constraints. Hospitals use multiple numbers of drugs as compared to health centers, thus all five of the hospitals were included purposively for better estimation of medicines wastage. One hospital, Nifas Mewuch primary hospital is excluded due to the distraction of the recent war in the area. The other hospital, Dera primary hospital is also excluded due to its new establishment. The remaining 14 health centers were selected from 12 woredas. Depending on the size of the woreda, more than one health center might be selected per woreda. Healthcare professionals working in the Drug and Therapeutics Committee (DTC) (1 person per health facility) and other activities in managing medicine supply (1 store person per health facility), worked throughout the study period, and were volunteer to participate were included purposively for their perception on medicines wastage and possible causes. As key informants, 2 individuals (1 CEOs and 1 heads of the pharmacy case team) were included per facility. In total 80 participants (40 for quantitative and 40 for qualitative) will take part in this study.
Data Collection Tools and Procedures
Data Collection
Two trained pharmacists collected data on the extent and contributing factors of medicines wastage by using a structured questionnaire (questionnaire adopted from LIAT,21 and Auditable pharmaceutical transactions and services (APTS), Ethiopia.13 Data involving qualitative aspects were collected using an in-depth interview of key informants (CEO, and pharmacy head).
Data Collection Instrument
The quantitative data on the type of wasted medicines were collected by reviewing wasted medicine records, model 19, and a report of medicines disposal. Logistics Indicator Assessment Tool (LIAT)21 were utilized to develop structured checklist for collecting medicine’s wastage value data in line with medicines waste management and disposal directive of the EFMHACA.22 A self-administered questionnaire was utilized for socio-demographic characteristics of participants. Factors contributing to wastage of medicines were adopted from a similar literature.23 A 5-point Likert scale scoring ranging from 1 (strongly disagree) to 5 (strongly agree) were applied for each item.
For the qualitative data, an in-depth interview and key informants guiding questionnaires, observation checklist, audio recorder, and field notebook were qualitative data collection tools. The interview was focused on the situation in wastage of medicines at their facility, barriers hindering proper medicine wastage, the effect of wastage on the provision of service, supports from concerned offices, training availability, supervision access, and directives for reducing wastage.
Data Quality Assurance
Prior to the actual data collection, a pre-test was done in two health facilities (1 type A and 1 type B) that will not be included in the study to ensure its suitability for the intended application. Prior to the data collection, a one-day orientation and training regarding data collection instruments and processing were given for the data collectors. The principal investigator supervised every activity and provide a timely amendment in case incontinency happens during the data collection. Adoption of the questions from the USAID logistics indicators assessment tool, EFMHACA wasted medicine management, and disposal directive, and Auditable pharmaceutical transactions and services (APTS), Ethiopia would assure the validity of the instrument to this study.21–23
Data Entry and Analysis
Data collected were checked for completeness, stratified based on the theme, and coded into Epi-data V 3.1. Then, it was exported into SPSS V25 for analysis. The data analyzed were presented using the descriptive statistics (mean, frequency, percentage, standard deviation (SD), and graph). The correlation analysis between perceived factors, and reliability analysis was conducted. Besides, the qualitative data was analyzed through thematic analysis (aggregate). The descriptive analysis was performed to investigate respondents’ characteristics and perceived contributing factors in terms of the mean score. The Cronbach`s Alpha value higher than 0.7 were taken to prove the internal consistency of the measurement.
Medicines wasted in each health facilities and the calculated costs of each wastage (from the selling price) registered on wasted and disposed medicine list were recorded to estimate and describe the type and extent of medicines wasted. The pharmaco-therapeutic classification system of Ethiopian national essential medicine list was utilized to classify medicines.18 Medicines having variable dosage forms and strength were taken as two variable medicines. The price recorded on model 19 were utilized to estimate the total costs of medicines received or purchased. A thematic analysis approach was applied to analyze the qualitative aspects of the study. An interview guide and themes and patterns from the data reviewed were utilized to draw the initial categories of data analysis. Situations in wastage of medicine, its effect, predisposing factors, and recommendations for improving wastage of medicine.
Results
Socio-Demographics of Respondents
Twenty store men and 20 DTC participated in the study to estimate medicines wastage quantitatively. The mean age of the store man and DTCs was 34.7 years (±SD =7.0). Regarding the educational status of the sore man and DTC enrolled in the study: about two-thirds were degree holders (65%), the rest 32.5% had diplomas and 2.5% were having master’s degrees. The study participants have a mean working experience of 11.64 years (±SD= 5.9) and it ranges from 4 to 24 years of experience. On another hand, 40 key informants (20 pharmacy heads and 20 CEOs (health officers and BSC nurses)) were involved in the qualitative data collection to explore the factors of medicines wastage. The mean ages of the key informants were 36.13 years (±SD =6.4). The highest proportion of the key informants were females (57.5%), and of those, 36 (90%) were bachelor’s degree holders and have a mean working experience of 12.01 years (Table 1).
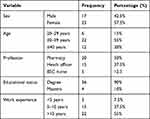 |
Table 1 Socio-Demographic Characteristics of Key Informants at Public Health Facilities of South Gondar Zone, Ethiopia, 2022 (n = 40) |
The Magnitude of Medicine Wasted
The twenty health facilities included in the present study received a total monetary value of 156,001,434 Ethiopian Birr (ETB) between 2011 and 2013 EFY. The three-year estimations for medicines wastage indicated that the overall wastage rate was 6.3% (6.5%, 5.9%, and 6.5% in 2011, 2012, and 2013 EFY, respectively) (Table 2). Thus, these health facilities wasted a total of 9,799,789 ETB, in the three fiscal years.
 |
Table 2 Medicines Wastage Rate at Public Health Facilities of South Gondar Zone, Ethiopia, 2022 (n = 20) |
The average medicines wastage shows an increasing trend with time as the number of received values increased over time. The average of money received from 2011/2012 increased by 14.1%, which is from an average of 2,330,747 to 2,658,279.45 ETB, and by 14.5% from 2012/12,013 from an average of 2,658,279.45 to 2,811,045.1 ETB. The wastage rate was non-proportional increasing from 2.8% in 2011/2012 to 5.7% in the 2012/2013 fiscal year. This study found that the medicines wastage rate increased by almost 3% every year irrespective of the 0.4% increase in the average monetary value received per year (Table 2 and Figure 1).
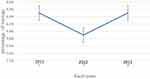 |
Figure 1 Trend of medicines wastage by fiscal years of the 20 public health facilities in South Gondar, Ethiopia. |
Wasted Medicines by Items and Dosage Forms
There was a total of 168 medicines items listed as the top ten mostly wasted medicines by each of the twenty health facilities. However, half of them were the most frequently reported medicines covering 616,865ETB (Table 3).
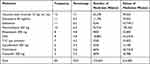 |
Table 3 Top ten Medicines Wastage Rate by Items (n=168 Items) in South Gondar Zone, 2022 |
Of the 168 medicines items identified as most commonly wasted medicines, 94.2% of them were found to be under eight different classes of dosage forms. From the different identified dosage forms, the highest number of wasted medicines were those with tablets 12,320 (28%) dosage forms, followed by injections (20.8%), and syrup (12.5%). These top eight dosage forms were worth 1,301,231.84 ETB. According to the top eight dosage forms wasted, injections were the first worth 325,470.38 ETB followed by tablets worth 300,646.8 ETB, and capsules worth 269,268.10 ETB (Table 4).
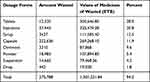 |
Table 4 Wastage of Medicines by Dosage Forms in South Gondar Zone, 2022 |
Regarding the general class of medicines wasted, the majority (35%) of medicines wasted were anti-infective followed by gastrointestinal medicines (10.7%). The percentage of most frequently wasted medicines is listed in Figure 2.
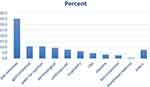 |
Figure 2 Medicines wastage by classes of medicines in South Gondar Zone, 2022. |
Sources and Perceived Contributing Factors for the Wastage of Medicines
Based on the quantitative data, the major sources of wastage of medicines were expiry (99.3%), and damage (0.7%) costing 9,735,335ETB, and 64,454 ETB, respectively. The Likert scale items questions indicated that delivering medicines with near-expiry date (<6 months) to health facilities (Ms=4.23), lack of communication and coordination with key stakeholders (Ms=4.2), and availability of overstocked medicines caused by ineffective forecasting of health facility needs (Ms=3.83) were the most perceived contributing factors to wastage of medicines at public health facilities in South Gondar zone, Ethiopia. Other factors like the purchase of medicines without a procurement plan, and weak or absence of monitoring and evaluation of the wastage of medicine in the health facilities were among the moderately contributing factors for the wastage of medicines at public health facilities in South Gondar, Ethiopia (Table 5). The various indicators were rated by using the 5-point Likert scale (Table 5) whereby 1 point was given to strongly disagree’, 2 points as “Disagree”, 3-point as “Neutral”, 4-point as “Agree”, and 5-point strongly Agree’. The mean score was calculated where the mean score below 3.39 was taken as low, 3.40 to 3.79 as moderate, and a mean score above 3.8 was taken as high.
 |
Table 5 Perceived Factors Contributing to Medicines Wastage at Public Health Facilities in South Gondar Zone, Ethiopia, 2022 |
Qualitative Findings
The qualitative finding indicated that the situation of medicines wastage has been increasing over time. One CEO stated the problem as follows:
…Medicines wastage becomes worth from time to time in our facility and the zone at large. (42, CEO)
Almost all health facilities CEO and pharmacy heads indicated that the absence of support and supervision from concerned offices and bodies were factors contributing to the medicine wastage. They evidenced this using the following quotes.
Absence of supports from zonal, regional, national, and or NGOs on medicine wastage prevention; and supportive supervision from concerned offices are factors contributing to medicinal wastage in our facilities and the zone at large. (Many of the CEO and Pharmacy heads)
The other challenge for high medicines wastage that all the health facilities surveyed are the push system of near-expired medicines distribution by the supplier.
The NGOs and EPSA distributed medicines with near expiration dates to health facilities. This is due to the delay in distributing the required medicines timely to each health facility. This process results in having a high rate of medication wastage. (One DTC pharmacy head)
The practice of distributing nearby expiry date medicines and their impact on patients was also supported by responses from the CEO as follows.
There is a push from EPSA in distributing nearby expiry medicines to health facilities. Health professionals are also not supportive to use/ordering/near expiring medicines to prevent medicines wastage. All these practices result in the presence of high medicines wastage in each facility and the zone at large. This situation creates difficulty to give standard treatment to patients. This makes patients hopeless since they don’t get what is prescribed to them there in the facilities. Hence, they are forced to search for other options and this creates patient dissatisfaction with services given by health facilities. (46, CEO)
In addition, key informants noted the lack of electric stock management tools was a factor contributing to high medicinal wastage in the study area. The following quote illustrates this idea.
For me, the use of electronic tools to manage the entrance and distribution of medicine would highly decrease medicines wastage in every health facility. However, in practice, there was no availability of such devices for this purpose resulting in high medicines wastage in our health facility. I think this has its contribution on medicines wastage. (Pharm.11)
The absence of functional DTC was also mentioned as contributing factor to medicines wastage.
Because of the push and pull means of medicines distributions, PFSA sometimes provides medicines that have a short expiry date. If we tried to refuse to receive these medicines, we will not get other required medicines listed on the same voucher… [So,] we are forced to receive the near-expiry medicines. What makes the problem worse is that we don`t have a functional DTC who will dispose on time. (Pharm.12)
Limited communication with EPSA was another factor raised by key informants that contributed more to the wastage of medicines in the health facility of the south Gondar Zone.
Though we have listed out needed medicines, the regional coordinators and, EPSA did not provide the medicines we requested in type and quantity. Most of the time they adjust the quantity and provide stock medicines to compensate the budget. this practice led to wastage of medicines. This is an example of communication limitation between suppliers like EPSA and health facilities. (Pharm.07)
Moreover, inadequate pharmacy personnel and absence of training on medicine wastage were stated as a factor that contributed to medicines wastage in the study area. This is supported by the following quote from key informants.
Because of the shortage of pharmacy professionals in the facility, the available staffs are not primarily focusing on medicines management function due to high workload and clinical nurses became responsible for store management in addition to their routine nursing functions. [So] there is no one dedicated to medicines supply management and because clinical nurses lack training in medicines logistics management, inefficiencies which result in medicine wastage occurs in medicines management practice. (38, CEO).
Suggestions to Reduce Medicines Wastage
The pharmacy heads and CEOs interviewed suggested their idea to lower medicines wastage as follows.
Medicine wastage can be reduced by giving near-expire medicines to other health facilities, and by communicating with prescribers and make generic substitutions even if 1st line agents are available. (AZH CEO)
CEO and pharmacy heads also recommended applying APTS and using electronic stock management tools can decrease the wastage of medicines in the health facility.
I think the use of electronic and APTS would be very important for managing medicines wastage in every health facility. If the regional and other concerned bodies offer support in this regard, there would be a better achievement in decreasing medicines wastage to our health facility. (Pharmacy head, 13)
Discussion
In the present study, the estimated wastage rate of medicines (in monetary terms) was 6.3%. These results were comparable with findings in Ghana (10%), public health facilities of South West Shoa zone, Ethiopia (7.5%), with the national report (8%), Dire Dawa, Ethiopia (3.07%) and teaching hospitals in Addis Ababa (4.8%),14,19,24–26 The estimated medicines wastage rate was lower as compared to the findings of a study conducted in Tanzania where the value of medicines wasted worth 23% of the total medicines dispensed.7 The difference could be due to the difference in the sampled interest of the study where the Tanzanian study assessed the wastage of medicines dispensed to patients, not the institution base wastage rate. Thus, patients may not use or get prescribed medicines or may be changed to other potential medications for better management of patient cases; this would result in a higher wastage rate of medicines.
However, the finding from the present study was quite higher than other studies done at Tikur Anbessa specialized hospital (2.86%)17 and public health facilities in Dessie, Ethiopia (3.68%).13 The relatively higher number of health facilities incorporated in the present study, and the increased number of health facilities over time could be the reason for this.
Our study showed that the financial burden resulting from medicine waste was very huge (9.8 million Ethiopia birr (217,773.1USD, considering 1 USD as 45 ETB)). This much value would be a three to five health center budget or would be a two to three primary hospitals budget (Table 2). This might not be easy to amend the national healthcare expenditures for poor nations like Ethiopia. For instance, in the well-developed nation, US households wasted 59,264.20 to 152,014.89 USD which led the US government to protect its national healthcare costs from 2.4 billion USD to 5.4 billion USD.12
Although this study investigated a higher number (of 20 health facilities (7 hospitals and 13 health centers in South Gondar)), the monetary wastage was quite lower than a study conducted at seven hospitals which revealed that the total monetary wastage was 11,078,910.52 ETB.26 This could be due to the largest budget allocated to the referral hospitals (where the previous study included only referral and teaching hospitals) relative to health centers, primary and comprehensive hospitals in our present study, variations in the study period, and differences in budget allocation in recent time would be the possible reasons.
The government has been implementing the newer APTS initiative to reduce medicines wastage and was expected to be expanded to primary health facilities in Ethiopia.19,27 The above figure has shown that medicines wastage was constantly increasing over time even in the APTS implementation phase in Ethiopia. However, this study’s medicines wastage rate (6.3%) was higher than the previous APTS report in Ethiopia,1.1%.27 This discrepancy could be due to the difference in APTS implementation and /or APTS performance or APTS may not be implemented in public health facilities in the South Gondar zone. The other reason for this variation could be due to variation in the number as well as the type of health facilities and the duration time where the study gets reviewed. Generally, the medicine wastage rate for the present study increased by nearly 3% from 2011/2012 to 2012/2013. This showed us medicine wastage rate is dramatically increasing in each successive year beyond the national standard (2%) medicine wastage rate.10 This might be due to the increasing number of patients in the facility.
Our study identified that a higher proportion (35.1%) of the 168 medicines mostly wasted were anti-infective medicines. This finding was in line with the result from Southwest Shoa, Ethiopia, Tanzania, and Dessie, Ethiopia where anti-infectives were the most frequently wasted class of medicines.13,18,19 The class of medicines getting wasted in developed countries was different from that of developing ones.28,29 The most common categories of medicines wasted in the UK were gastrointestinal medicines (12.4%);30 while in Middle east countries like Jordan anti-infective were the leading class of medicines wasted (17.7%).31 In Africa, anti-infectives were the common medicines getting wasted13,18 which is similar to Middle Eastern Asian countries.31 The higher accumulations and wastage of anti-infective medicines in the study area and developing countries as a whole may be indicative for overstocking of these classes of medicines hence infectious diseases are more prevalent in developing nations like Ethiopia than in developed ones.26
Many of the factors that contributed to the wastage of medicines in developing nations are not yet documented.18,20 However, the weakening of the pharmaceutical supply management system was the predominant contributing factor to deterioration and expiration.19 The other contributing factors to the expiry of health commodities and wastage were a weak stock control system, and over supplying of drugs.32 In this study, the main sources of wastage of medicines were expiry (99.3%). The perceived reasons for such medicine’s wastage were delivery of medicines with the near-expiry date (<6 months) to the health facilities by suppliers (Ms=4.23), excessive supply of nearly expired medicines,32,33 poor coordination and communication with key stakeholders (suppliers, health bureau/office, NGOs‟s) (Ms=4.2) and availability of overstocked medicines caused by inappropriately forecasted needs of health facility (Ms=3.83) of South Gondar zone, Ethiopia. This was in line with a similar study conducted in South West Shoa Zone, Ethiopia.19 This similarity might be due to the similar level of the healthcare facilities in both study areas which might have similar working environments and management systems.
The key informant interview result shows that the wastage of medicines is worthwhile from time to time. But, the government of Ethiopia has been taking measures in building the capacity of human resources like those who support, train, and guide on the prevention of medicines wastage. For instance, training in Masters of Regulatory related affairs is being provided at Addis Ababa University with the aims of addressing the shortage of skilled manpower and to equip with the required competencies for appropriate pharmaceutical supply distributions.34
Despite the efforts made by the government of Ethiopia, the present study report has shown the gaps in that regulatory bodies do not train and/or provide support to those professionals in the health facility settings. The key informants involved in the present study assured the absence of support from zonal, regional, national, and or NGOs on medicine wastage prevention; the absence of training-on-training access on medicine wastage and related issues, and also the absence of supportive supervision from concerned offices would aggravate the medicines wastage rate. However, the key cause of wastage was the push system distribution of nearly expired medicines by suppliers, and absence of electronic stock management tools, and functional DTC, poor communication with suppliers like EPSA, and inadequacy of pharmacy personnel working in the health facility. However, if supervision and training were provided; health professional at the health facilities would their performance, manages potential problems such as understocks and overstocks, and poor storage conditions, and will communicate and manage the near-expiry medications.9
The key informants also forwarded their suggestions that medicine wastage can be reduced by transferring near expired medicines to other health facilities, and by communicating with prescribers “make generic substitutions even if 1st line agents are available. The other recommendation forward was to apply” APTS and to use electronic stock management tools to decrease the wastage of medicines in public health facilities.
Conclusion
This study showed a high rate of wasted medicines in public health facilities of the South Gondar zone which calls for urgent action for intervention by health policymakers and healthcare providers. Anti-infective followed by gastrointestinal drugs were the most common therapeutic classes of wasted medicines. Expiry was the main source of medicine wastage. Delivering medicines with a near expiry date by PFSA/EPSA, failure to exchange medicines with nearly expiry date among facilities, poor coordination, and communication with key stakeholders (suppliers, health bureau/office, NGOs) presence of improper forecasting and overstocking of medicines beyond the health facility needs, absence of electronic tools for managing the stock and an inadequate number of pharmacy professionals in the health facilities were the main contributing factors for wastage of medicines. Healthcare providers should create a system of supplying and procuring medicines with long expiry dates in accordance with the needs of the specific health facility, exchanging near-expiry and overstocked medicines across a health facility, proper execution of APTS, using computerized/electronic inventory management tools that allow to properly quantify and monitor levels of stock and expiry dates to curtail the higher rate of medicines wastage. Moreover, health policymakers should enforce waste minimization by creating awareness, providing guidelines on waste-minimizing measures or stimulating collaborations and alliances with key stakeholders and supporting adequate staffing of pharmacy professionals to improve pharmaceutical supply management through workload reduction.
Limitations of the Study
The present study is facility-based and did not include unused prescribed medicines that are wasted at the larger community level. Moreover, Program and donation wasted medicines without price lists were not included in the study.
Abbreviations
APTS, Auditable Pharmaceutical Transactions and Services; DTC, Drug and Therapeutic Committee; EFMHACA, Ethiopia Food, Medicine and Health Care Administration and Control Authority; EFY, Ethiopian fiscal year; EPSA, Ethiopian Pharmaceutical Supply Agency; ETB, Ethiopian birr; LIAT, Logistics Indicators Assessment Tool (LIAT); WHO, World Health Organization.
Ethics Approval and Consent to Participate
Ethical approval was obtained from the Ethical review board of Amhara public health institute (APHI), which is one of the ethical boards responsible to review any research done on human in our state. Then, a formal letter of cooperation was granted from the South Gondar Zone health department to get permission for conducting the study. Then, the selected health facilities’ willingness was assured and the health facility was coded to be kept confidential. Informed consent was taken from each health facility administrative and study participant before actual data collection. Similarly, the health professional’s information was also kept confidential by omitting professional identifiers. All health professionals included in the study have been granted the right to withdraw from the study at any time. Voluntary written and informed consent was obtained for the participation in the study and publication of the manuscript from each study participant by removing identifying information that should be anonymized.
Acknowledgments
First of all, we would like to acknowledge GAMBY Medical and Business College for allowing us to undertake this study. Our gratitude extends to all public health facilities in the south Gondar zone and all health professionals who have participated in the qualitative aspects of our study.
Author Contributions
All authors made a significant contribution to this work in the conception, execution, study design, acquisition of data, analysis, and interpretation, as well as in drafting, revising, or critically reviewing the article; gave final approval of the manuscript to be published; agreed on the journal to which the manuscript has been submitted; and agreed to be accountable for all aspects of this work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ebrahim AJ, Teni FS, Yimenu DK. Unused and expired medications: are they a threat? A facility-based cross-sectional study. J Prim Care Community Health. 2019;10:2150132719847857. doi:10.1177/2150132719847857
2. Tong AY, Peake BM, Braund R. Disposal practices for unused medications around the world. Environ Int. 2011;37(1):292–298. doi:10.1016/j.envint.2010.10.002
3. World Health Organization. Guidelines for Safe Disposal of Unwanted Pharmaceuticals in and After Emergencies. World Health Organization; 1999.
4. Bekker CL, van den Bemt BJF, Egberts ACG, Bouvy ML, Gardarsdottir H. Patient and medication factors associated with preventable medication waste and possibilities for redispensing. Int J Clin Pharm. 2018;40(3):704–711. doi:10.1007/s11096-018-0642-8
5. Bekker CL, Gardarsdottir H, Egberts ACG, Bouvy ML, van den Bemt BJF. Pharmacists’ activities to reduce medication waste: an international survey. Pharmacy. 2018;6(3):94. doi:10.3390/pharmacy6030094
6. World Health Organization. Measuring Transparency in the Public Pharmaceutical Sector: Assessment Instrument. World Health Organization; 2009.
7. Makenya F. Factors associated with medicines wastage at muhimbili national hospital: muhimbili university of health and allied sciences; 2013.
8. Gebregeorgise DT. Detailed countries case study- Ethiopia’s health supply chain system; 2018.
9. Shewarega A, Dowling P, Necho W, Tewfik S, Yiegezu Y. Ethiopia: A National Survey of the Integrated Pharmaceutical Logistics System. Arlington: USAID/DELIVER PROJECT, Task Order; 2015:4.
10. FMOH. Health Sector Transformation Plan 2015/16–2019/20. Addis Ababa, Ethiopia: Federal Ministry of Health; 2015.
11. Smale EM, Egberts TC, Heerdink ER, van den Bemt BJ, Bekker CL. Waste-minimising measures to achieve sustainable supply and use of medication. Sustain Chem Pharm. 2021;20:100400. doi:10.1016/j.scp.2021.100400
12. Law AV, Sakharkar P, Zargarzadeh A, et al. Taking stock of medication wastage: unused medications in US households. Res Social Adm Pharm. 2015;11(4):571–578. doi:10.1016/j.sapharm.2014.10.003
13. Mohammed SA, Kahissay MH, Hailu AD. Pharmaceuticals wastage and pharmaceuticals waste management in public health facilities of Dessie town, North East Ethiopia. PLoS One. 2021;16(10):e0259160. doi:10.1371/journal.pone.0259160
14. MOHG. Health Facilities Survey in GHANA. Ministry of Health; 2009.
15. FC O, JS O, TG T. A review of medical waste management in South Africa. Environ Sci Technol. 2018;10(1):34–45. doi:10.2174/1876325101810010034
16. World Health Organization. Pharmaceutical Situation in Jamaica. Washington, DC, USA: WHO Assessment of Level II Health Facilities and Household Survey; 2012.
17. Milkessa S. Assessment on Auditable Pharmaceutical Transactions and Services Implementation Outcome: The Case of Tikur Anbessa Specialized Hospital: St. Mary’s university; 2019.
18. Kagashe GA, Makenya FB, Buma D. Medicines wastage at a tertiary hospital in Dar es Salaam Tanzania. J Appl Pharm Sci. 2014;4(6):98–102.
19. Gebremariam ET, Gebregeorgise DT, Fenta TG. Extent of medicines wastage and its contributing factors in public health facilities of south west Shoa Zone, Oromia Regional State, Ethiopia: a cross-sectional survey. Ethiop Pharm J. 2018;34(2):143–152. doi:10.4314/epj.v34i2.6
20. Gebremariam ETG, Fenta DT, G T. Factors contributing to medicines wastage in public health facilities of South West Shoa Zone, Oromia Regional State, Ethiopia: a qualitative study. J Pharm Policy Pract. 2019;12(1):29. doi:10.1186/s40545-019-0192-z
21. USAID. Deliver Project To. Logistics System Assessment Tool (LSAT). VA: USAID Arlington; 2009.
22. EFMHACA. Medicines Waste Management and Disposal Directive. EFMHACA; 2011.
23. Nakyanzi JK, Kitutu FE, Oria H, Kamba PF. Expiry of medicines in supply outlets in Uganda. Bull World Health Organ. 2010;88(2):154–158. doi:10.2471/BLT.08.057471
24. World Health Organization. Assessment of the Pharmaceutical Sector in Ethiopia. Addis Ababa, Ethiopia: Ministry of Health; 2003.
25. Alemu AB, Ibrahim NA, Argaw KW. Magnitude of medicine wastage and perceived contributing factors among public health facilities in Dire-Dawa city administration, in mid COVID-19 Pandemic in Ethiopia: retrospective, cross-sectional study. Integr Pharm Res Pract. 2023;12:61–75. doi:10.2147/IPRP.S395102
26. Tadeg H, Ejigu E, Geremew E, Adinew A. Auditable pharmaceutical transactions and services (APTS): findings of the baseline assessment at federal, Addis Ababa, and teaching hospitals. Submitted to the US agency for international development by the systems for improved access to pharmaceuticals and services (SIAPS) program. Arlington: Management Sciences for Health; 2014.
27. Gedif T, Teshome D, Sebsibie F, et al. Implementation of auditable pharmaceutical transaction and services in Ethiopia. Assessment Report. Special bulletin 18th annual review meeting. Addis Ababa, Ethiopia: Federal Ministry of Health; 2016.
28. West LM, Diack L, Cordina M, Stewart D. A systematic review of the literature on ‘medication wastage’: an exploration of causative factors and effect of interventions. Int J Clin Pharm. 2014;36(5):873–881.
29. Dilip C, Sayed MS, Sameer P, ShesaMajeed P, Shahanas MK. Economic burden of unused medicines and its causes in households of Perinthalmanna region. Clin Epidemiol Glob Health. 2020;8(2):356–360. doi:10.1016/j.cegh.2019.09.002
30. Trueman P, Taylor D, Lowson K, et al. Evaluation of the scale, causes and costs of waste medicines. Report of DH funded national project; 2010.
31. Al-Azzam S, Khader Y, Rawashdeh S, Hijazi S. An assessment of the extent of medication wastage among families in Jordan. Jordan J Pharm Sci. 2012;5(1):65–73.
32. Hakuzimana T, Kayumba PC, Hahirwa I, Kabalisa M. Assessment of factors contributing to medicine expiry in Rwanda: case of the medical procurement and production division. Rwanda J Health Sci. 2021;4(2):281–291. doi:10.4314/rjmhs.v4i2.7
33. Tumwine Y, Kutyabami P, Odoi RA, Kalyango JN. Availability and expiry of essential medicines and supplies during the ‘pull’and ‘push’drug acquisition systems in a rural Ugandan hospital. Trop J Pharm Res. 2010;9:6.
34. Ministry of Health and Ministry of Industry. National Strategy and Plan of Action for Pharmaceutical Manufacturing Development in Ethiopia (2015–2025). Ministry of Health and Ministry of Industry; 2015.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.