Back to Journals » Breast Cancer: Targets and Therapy » Volume 15
MCM-2 Levels as a Potential Biomarker for Predicting High-Risk Breast Cancer Patients According to TAILORx Classification
Authors Ünal Ç , Özmen T, İlgün AS, Ordu Ç, Özkurt E, Ak N, Alço G, Erdoğan İyigün Z, Kurt S, Duymaz T, Öztürk MA, Elbüken Çelebi F, Yararbaş K, Soybir G, Aktepe F, Özmen V
Received 17 May 2023
Accepted for publication 11 August 2023
Published 1 September 2023 Volume 2023:15 Pages 659—669
DOI https://doi.org/10.2147/BCTT.S421535
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Harikrishna Nakshatri
Çağlar Ünal,1 Tolga Özmen,2,3 Ahmet Serkan İlgün,4 Çetin Ordu,5 Enver Özkurt,6 Naziye Ak,7 Gül Alço,8 Zeynep Erdoğan İyigün,9 Sevgi Kurt,10 Tomris Duymaz,11 Mehmet Alper Öztürk,12 Filiz Elbüken Çelebi,13 Kanay Yararbaş,14 Gürsel Soybir,15 Fatma Aktepe,16 Vahit Özmen17
1Division of Medical Oncology, Department of Internal Medicine, Kartal Dr. Lütfi Kırdar City Hospital, İstanbul, Turkey; 2Division of Gastrointestinal and Oncologic Surgery, Harvard Medical School, Boston, MA, USA; 3Division of Gastrointestinal and Oncologic Surgery, Massachusetts General Hospital, Boston, MA, USA; 4Department of Surgery, Mater Dei Hospital, Msida, Malta; 5Division of Medical Oncology, Department of Internal Medicine, Gayrettepe Florence Nightingale Hospital, İstanbul, Turkey; 6Department of General Surgery, Istanbul Florence Nightingale Hospital, İstanbul, Turkey; 7Division of Medical Oncology, Department of Internal Medicine, Istanbul Florence Nightingale Hospital, İstanbul, Turkey; 8Department of Radiation Oncology, Gayrettepe Florence Nightingale Hospital, İstanbul, Turkey; 9Department of Physical Therapy and Rehabilitation, Göztepe Medical Park Hospital, İstanbul, Turkey; 10Department of Plastic Surgery, Istanbul Florence Nightingale Hospital, İstanbul, Turkey; 11Department of Physiotherapy and Rehabilitation, Faculty of Health Sciences, Istanbul Bilgi University, Istanbul, Turkey; 12Department of General Surgery, Biruni Hospital, İstanbul, Turkey; 13Department of Radiology, Yeditepe University Hospital, İstanbul, Turkey; 14Department of Medical Genetics, Demiroglu Bilim University, Istanbul, Turkey; 15Department of General Surgery, Memorial Şişli Hospital, İstanbul, Turkey; 16Department of Pathology, Memorial Şişli Hospital, İstanbul, Turkey; 17Department of General Surgery, Istanbul University Istanbul School of Medicine, İstanbul, Turkey
Correspondence: Çağlar Ünal, Division of Medical Oncology, Department of Internal Medicine, Kartal Dr. Lütfi Kırdar City Hospital, İstanbul, Turkey, Email [email protected]
Background: The minichromosome maintenance protein-2 (MCM-2) is a more sensitive proliferation marker than Ki-67. This study aimed to evaluate the relationship between MCM-2 and Oncotype DX recurrence score (ODX-RS) and determine an MCM-2 cutoff value in high-risk patients according to TAILORx risk categorization.
Methods: Hormone receptor (HR) positive HER-2 negative early-stage breast cancer patients (pT1-2, pN0-N1, M0) who had ODX-RS were included in the study. According to the TAILORx trial, patients were divided into two groups with high (ODX-RS ≥ 26) and low risk (ODX-RS < 26) in terms of ODX-RS. Formalin-fixed-paraffin-embedded tissues of patients were re-evaluated, and 3 μm sections were prepared for MCM-2 immuno-histochemical staining. The relationship between ODX-RS and the percentage of MCM-2 staining was evaluated in two groups. The ROC curve analysis was performed to determine the MCM-2 cut-off value for the TAILORx high-risk group (ODX-RS ≥ 26).
Results: The mean MCM-2 value was significantly higher in the high-risk group [(60.2 ± 11.2 vs 34.4 ± 13.8, p < 0.001)]. In the multivariate analysis, MCM-2 (OR: 1.27, 95% CI: 1.08– 1.49, p = 0.003) and progesterone receptor (PR) levels ≤ 10% (OR: 60.9, 95% CI: 4.1– 89.7, p = 0.003) were found to be independent factors indicating a high-risk group. A one-unit increase in MCM-2 level increased the likelihood of being in the high-risk group by 1.27 times. In the ROC curve analysis, the optimal MCM-2 cut-off level was 50 (AUC: 0.921, sensitivity: 86.7%, specificity: 96.0%, p < 0.001).
Conclusion: Our study is the first study in the literature to investigate the relationship between ODX-RS and MCM-2 levels in HR-positive HER-2 negative early breast-cancer patients. In this study, MCM-2 was an independent risk factor in identifying high-risk patients according to TAILORx risk classification. MCM 2 cut-off value (50) may help the decision on adjuvant chemotherapy in patients where the Oncotype DX test cannot be performed.
Keywords: breast cancer, MCM-2, Oncotype DX recurrence score, TAILORx risk categorization
Introduction
Breast cancer has overtaken lung cancer as the most common cancer worldwide, with 2.3 million new cases in women, yearly.1 According to the latest GLOBOCAN 2020 data, it is the most common cancer in women, with 24,175 (23.9%) cases in Turkey.2 As a result of the lack of community-based organized mammographic screening and low awareness, in a study we conducted with 20,000 patients, only 5% of the patients diagnosed were ductal carcinoma in situ (DCIS), 28% were Stage I and 48% were Stage II breast cancer.3 The hormone receptor (HR) positive HER-2 negative patient group constitutes ~70% of the early-stage breast cancer patients.4
The dysregulation of DNA replication has always been at the forefront of cancer research, and its inhibition is among the main targets of classical chemotherapeutic drugs. Minichromosome maintenance proteins (MCMs) are among the most well-known proteins initiating DNA replication and are crucial for genomic stability.5,6 Six MCM proteins (MCM-2-7) have a complex structure in hexameric rings and act like DNA helicase enzymes that dissolve the DNA double helix structure.7 Uncontrolled expression and the activation of MCM 2–7 proteins directly disrupt DNA replication, causing genomic instability and leading to tumorigenesis and cancer development.8,9 MCM-2 has an essential regulatory role in the initiation of DNA replication, and its dysfunction is known to correlate with progression and poor prognosis in many types of cancer, including lymphoma,10 lung11, and breast cancer.12–15 With the discovery of a small molecular inhibitor targeting MCM-2, and the anti-tumoral activity of this inhibitor in lung cancer,16 it seems that in addition to its prognostic and diagnostic roles, MCM-2 might be a molecular target that can be used to treat many cancer types.
The prognostic and predictive value of the 21-gene test Oncotype Dx (Genomic Health, Redwood City, CA, USA) were confirmed in hormone receptor-positive HER-2 negative breast cancer patients.17–19 The Oncotype Dx-Recurrences Score (ODx-RS) is used to determine the benefit of adjuvant chemotherapy. It has been approved by the American Society of Clinical Oncology (ASCO), the National Comprehensive Cancer Network (NCCN), and other guidelines.17–19 In western countries especially, treatment decisions are made using this test. Trial Assigning Individualized Options for Treatment (TAILORx) study guides clinicians in making adjuvant treatment decisions by categorizing Odx-RS according to risk level (RS <11 low risk, RS 11–25 intermediate risk, RS ≥26 high risk) in early-stage breast cancer patients.20 Giving adjuvant chemotherapy to patients in the high-risk group is also indicated in the guidelines.17,18 A benefit of chemotherapy was reported in patients with RS ≥26 based on the 12-year follow-up results of the TAILORx study presented at the last San Antonio Breast Symposium.21
Access to this genetic test is difficult due to its high cost in low-middle-income countries. Therefore, the decision for adjuvant treatment in early-stage breast cancer patients is often based on clinicopathological features. Many studies, including our previous studies, have shown that ODX-RS and some clinicopathological features are compatible.22–28 However, these correlations are often vague making clinicopathological features imprecise surrogates for ODx-RS. Therefore, we aimed to evaluate the relationship between ODx-RS and MCM-2, considered a more sensitive proliferation marker than Ki-67, and to define a cutoff value for MCM-2 to identify patients in the high-risk group according to the TAILORx risk categorization.
Methods
Study Design and Participants
A total of 72 patients with HR-positive HER-2 negative early-stage breast cancer (pT1-2, pN0-N1, M0) who were operated on in our clinic were included in the study. The demographic, clinical, and pathological characteristics of the patients (age, tumor diameter, histological grade, estrogen receptor [ER] and progesterone receptor [PR] levels, Ki67 index, and lymph node status) were recorded retrospectively. The ODX-RS was analyzed from surgically removed, formalin-fixed, paraffin-embedded tissue preparations from patients in a central laboratory. Using immunohistochemical methods, ER and PR were considered positive if ≥1% of tumor cells showed moderate or strong nuclear staining. HER-2 expression was evaluated by immunohistochemical (IHC) staining, and HER-2 negative [IHC 0/1 + or IHC 2+ but FISH (fluorescence in situ hybridization) negative] patients were included in the study. The staging was performed according to the 8th TNM Staging of the American Joint Committee on Cancer (AJCC). The clinical risk was defined as low risk if the tumor was ≤3 cm in diameter and histological grade was low, or if the tumor was ≤2 cm in diameter and histological grade was intermediate, or if the tumor was ≤1 cm in diameter and histological grade was high; patients who did not meet the low-risk criteria were defined as high risk as a clinical risk29. According to the TAILORx trial, patients were divided into two groups with high (ODX-RS ≥26) and low risk (ODX-RS <26) in terms of ODX-RS.21 Formalin-fixed-paraffin-embedded tissues of patients were re-evaluated, and 3 µm sections were prepared for MCM-2 immuno-histochemical staining. Patients were separated into two groups as having received only endocrine therapy and having received combined therapy [chemotherapy (taxane-based and/or adriamycin-based regimens) and endocrine therapy (tamoxifen or aromatase inhibitors ± LHRH analog)].
MCM 2 Immunohistochemical Staining
MCM-2 levels were evaluated by a pathologist with 30 years of experience in breast cancer pathology (FA). Formalin-fixed-paraffin-embedded tissues of patients were re-evaluated, and 3 µm sections were prepared for immunohistochemical examination from the most representative tumor area. Anti-MCM2 (phospho S53) (rabbit monoclonal, 1:100 dilution, Abcam) was used for immunohistochemical analysis. Positive (colon mucosa) and negative control (brain tissue) were used. Diaminobenzidine (DAB) was applied as a chromogen. It was stained with the appropriate immunohistochemistry staining according to the protocol in an automatic immunohistochemistry staining device (DAKO OMNIS).
Scoring of MCM2 Stained Preparations
Brown staining in invasive carcinoma cell nuclei was considered positive. Preparations were digitally scanned with Leica-Aperio at2, and examination was done via Sectra IDS7 (accessed online). The program developed by Sectra IDS7 program for counting Ki67 was used to calculate positively stained cells. With the help of this program, the rate of positive cells in 1000 cells was determined (Figures 1 and 2).
Statistical Analysis
We reviewed the patient files and electronic hospital registry between 2014 and 2022 to screen patients for study inclusion. We aimed at least 15 patients per group for the ODx-RS low- and high-risk groups to ensure adequate power. We conducted the power analysis with the following assumptions: Low-risk to high-risk patient ratio in the cohort would be three or four, and the mean MCM-2 expression difference would be around 10%. This assumption would require between 60 and 70 patients to ensure an 90% power and 0.05 type 1 error (https://riskcalc.org/samplesize/).
Our initial search retrieved a total of 72 patients with early breast cancer who had available ODx results and available tissue for MCM-2 evaluation. The number of patients in the groups (high vs low risk) was 15, and 57. This sample size and low-risk to high-risk ratio corresponded to a 92% power (https://riskcalc.org/samplesize/).
Data were analyzed using the SPSS 22.0 (IBM Corp., Armonk, N.Y., USA) program. The chi-square test was used to compare the categorical data (demographic and clinical characteristics) among groups. The Student’s t-test and Mann–Whitney U-tests were used for the evaluation of normally and non-normally distributed continuous variables. Boxplot analysis was used to evaluate the distribution of MCM-2 between the high-risk and non-high-risk groups. TAILORx scores were considered with the same analysis to assess distribution for risk classification purposes. Univariate and multivariate analyses were used to determine the factors affecting high-risk classification according to TAILORx categorization. Receptor operating characteristics (ROC) analysis was used to determine the MCM-2 cut-off value for identifying the high-risk group. A p-value of <0.05 was considered statistically significant in all tests.
Results
The median (min-max) values were as follows: age 46.5 (26–73), MCM level 41.5 (10–77), and ODX RS 17.5 (1–59) (Table 1). All patients were ER-positive (>10%), and the number of patients with a PR ≤ 10% was 14. Two of these patients were PR negative, and 12 had weak PR positive (1–10%). Pathological tumor diameter, histological grade (HG), pathological stages, Ki-67 level, lympho-vascular invasion, and axillary involvement rates in two groups are shown in Table As expected, high group (ODX RS ≥ 26) had higher HG (p = 0.008), lower PR rate (p < 0.001), and higher pathological stage (p = 0.01). There was no significant difference between groups regarding clinical risk score, radiotherapy, and surgical treatment. While all patients in the ODX-RS ≥26 groups received chemotherapy, 28% of the patients in the ODX-RS <26 groups received chemotherapy and endocrine therapy (p < 0.001).
 |
Table 1 Characteristics of the Patients in Two Groups |
The mean MCM-2 level was significantly higher in the high-risk group than the other group (60.2 ± 11.2 vs 34.4 ± 13.8, p < 0.00.1) (Table 2). Similarly, the mean age (47.2 ± 10.3 vs 55.4 ± 9.8, p = 0.009) and level of Ki-67 [15% (2–38) vs 26% (10–60), p < 0.001] were found to be high in the high-risk group. On the contrary, the level of PR [80% (3–100) vs 3% (0–90), p < 0.001] (Table 2). There was no difference between the groups in terms of estrogen receptor.
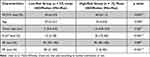 |
Table 2 Association Between Clinicopathological Characteristics According to Risk Groups |
A distribution graph made according to the TAILORx risk classification indicates that MCM-2 levels were higher in the high-risk group than in the intermediate and low-risk groups (p < 0.001). When the patients were separated into two groups those in the high-risk group and those who were not, the MCM-2 levels were found to be significantly higher in the RS ≥26 group (p < 0.001) (Figure 3).
In the univariate analysis, there were significant associations between age, MCM-2 and Ki-67 levels, histological grade, low progesterone levels (PR ≤ 10%), and high-risk group (Table 3). In the multivariate analysis, only MCM-2 (OR: 1.27, 95% CI: 1.08–1.49, p = 0.003) and low progesterone receptor levels (PR ≤ 10%, OR: 60.9, 95% CI: 4.1–89.7, p = 0.003) were found to be independent factors indicating the high-risk group (Table 3).
 |
Table 3 Regression Models of Potential Prognostic Variables Associated with the High-Risk Group |
The ROC curve analysis was performed to determine the MCM-2 cut-off value in the high-risk group, and this value was found as 50 (Figure 4) (AUC: 0.921, sensitivity: 86.7%, specificity: 96.0%, p = <0.001, positive predictive value: 95.5%, negative predictive value: 96.0%, validity of the test: 90.0%).
 |
Figure 4 ROC curve analysis of MCM-2 levels for the high-risk group (cutoff MCM-2 level was found 50). |
Discussion
Patients with early-stage breast cancer should be selected for treatment to avoid overtreatment and side effects of adjuvant chemotherapy.28 Therefore, tumor genetic assays have been used to make decisions on adjuvant therapy in patients with HR-positive HER-2 negative early-breast cancer.20,29,30 Oncotype DX, Mammaprint, Prosigna, Endopredict, and Breast Cancer Index are recommended in the NCCN guideline.31 The Oncotype Dx test is the most commonly used, and clinical trials have supported its prognostic and predictive value.32–34 In our patients, the oncotype recurrence score was considered when deciding on adjuvant therapy, similar to other guidelines.30,31 However, in patients where this test cannot be accessed, clinicians make the decision of adjuvant treatment by looking at the clinicopathologic characteristics of the patient.24 Although Ki-67 is a globally accepted proliferation marker, it is only expressed in part of the cell cycle from late G1 phase to M phase.35,36 On the other hand, MCM-2 protein is expressed in all phases of the cell cycle and is a more advantageous marker compared to Ki 67.37 Our primary goals in this study were to reveal the relationship between MCM-2 and ODX-RS and that the MCM-2 cut-off value may help in adjuvant therapy decisions in patients where the ODX test cannot be reached. The study results showed that each unit increase in the MCM-2 level increased the likelihood of being in the high-risk group by 1.27 times (OR: 1.27, 95% CI: 1.08–1.49, p = 0.003). In addition, the ROC curve analysis to find the cut-off value showed that this value is 50 (AUC: 0.921, sensitivity: 86.7%, specificity: 96.0%, p < 0.001, positive predictive value: 95.5%, negative predictive value: 96.0%, validity of the test: 90.0%) (Figure 4).
Many studies in the literature, including our own, show the relationship between clinicopathological features and the ODX-RS.22,24,28,38,39 Although these studies have revealed a statistically significant correlation between tumor diameter, age, HG, receptor status, Ki-67 level, and lymph node involvement with the ODx-RS, an explicit treatment standardization has not been established based on these clinical features.22,24,28,38,39 Better proliferation markers are necessary to determine prognosis. It should be noted that five of the 21 genes on the Oncotype Dx test are proliferation genes. The test also highlights the importance of proliferation in prognosis and clinical treatment decision-making.40 The half-life of Ki-67 is approximately 90 minutes, and its concentration fluctuates due to synthesis and degradation stages.41 MCM-2 binds to chromatin reversibly, and its level remains unchanged, and it cannot be detected only when in the silent phase, which is the resting phase of the cell cycle.42 It should also be noted that eukaryotic cells cannot proliferate without MCM-2.42 MCM-2 is a diagnostic and prognostic marker in many types of cancer, including breast cancer.10–15 MCM-2 levels can be determined via two different methods: mRNA expression level and immunohistochemical (IHC) staining percentage in breast cancer patients.42 In a large cohort, these two different determination methods were found to provide a high level of concordance of 0.97 (95% CI = 0.96–0.97, P < 0.0001).42 In our study, MCM-2 expression levels were determined by the IHC staining method. They were significantly higher in patients in the high-risk group according to the TAILORx risk classification (60.2 ± 11.2 vs 34.4 ± 13.8, p < 0.001). Moreover, by the literature,24,28,38,39 it was found that the age and PR level of patients in this group were significantly lower than that of the patients in the low-risk group (ODX-RS < 26), but the Ki-67 level was higher (Table 2). When the data were analyzed, patients were divided into three groups according to Taylor-X risk classification: [(low (0–10), intermediate (11–25)], and high risk (≥26)]; in all three groups, it was determined that there was an increase in the risk status of patients with a gradual rise in MCM-2 levels (Figures 3). Yousef et al found that the recurrence rate had a higher degree of significance with MCM-2 than with Ki-6743 (for ki-67 p = 0.045; for MCM-2, p = 0.0003) in breast cancer patients. As a result of the studies with MCM-2, it is known that there is a positive correlation between ki-67, histological grade, tumor diameter, NPI score, and MCM-2, and a negative correlation between ER and PR levels and MCM-2.13,44–46 MCM-2 has also been identified as a marker that predicts a complete pathological response, such as Ki-67, in breast cancer patients receiving neoadjuvant chemotherapy.47 In our multivariate analysis, MCM-2 and low PR levels (PR ≤ 10) were found to be independent factors affecting the high-risk group [(Table 3) (OR: 1.27, 95% CI: 1.08–1.49, p = 0.003; OR: 60.9, 95% CI: 4.1–89.7, p = 0.003; Forward: LR)]. Many studies have reported that PR negativity is a factor that increases the ODX-RS and decreases the survival rate.13,44–47 However, no study in the literature has investigated the relationship between MCM-2 and ODX-RS.
In our study, ROC curve analysis was performed to determine the cut-off value for the high-risk group. The MCM-2 cutoff value was 50 (AUC: 0.921, sensitivity: 86.7%, specificity: 96.0%, p < 0.001) (Figure 4). A study conducted by Gonzalez et al with 221 breast cancer patients showed that an MCM-2 value higher than 50 is an independent predictive risk factor for survival, disease-free survival, and distant and local recurrence, with an average of 140 months of follow-up. This study observed that ki-67, grade, and lymph node involvement were not independent factors affecting survival13 A consensus in the literature could not be reached for a standard cut-off value for MCM-2.13,43,44,48,49 In another study by Joshi et al, MCM-2, Ki-67, and geminin proliferation markers were identified as factors affecting 15-year breast cancer-specific survival (BCSS). It was stated that MCM-2 had a higher significance level than Ki-67 and geminin. In this study, the cutoff for MCM-2 was established as 12 (MCM-2, p = 0.0004; Ki-67, p = 0.014; geminin, p = 0.007).44 Although the standard cut-off value cannot be determined in the literature, studies on breast cancer typically use cut-off values between 30 and 50 for low and high MCM-2 levels in early-stage breast cancer patients.13,42,44,46,48–50 In our study, by taking the patients aged ≤50 as a single group, when the patients were evaluated as ODX-RS≥21 and ODX-RS <21, the MCM-2 cut-off score was found to be 40 (AUC: 742, p = 0.004, Sensitivity: 71.4%, Specificity: 70.4%). When patients in the high (ODX-RS≥26) and low-risk (ODX-RS <26) groups were compared by considering only patients over 50 years of age, the cut-off value was found to be 50 [(AUC: 0.859, p = 0.005, Sensitivity: 75.0%, Specificity: 75.0%)].
The most important limitation of our study was the number of patients. For this reason, subgroup analysis revealed lower sensitivity and specificity values (age ≤ 50 vs period > 50; ODX-RS ≥ 21 vs ODX-RS < 21). Studies with higher patient volumes are necessary to evaluate the relationship between MCM-2 and ODX-RS and to obtain higher sensitivity and specificity. It should be noted that although blood tests are frequently used in clinical practice because they are fast and simple, their sensitivity and specificity are not as high as pathological staining with tumor tissue.51,52
Our study is critical in the literature to investigate the relationship between ODX-RS and MCM-2 levels in HR-positive HER-2 negative early breast-cancer patients. Unlike Ki-67, MCM-2 was found to be an independent risk factor for identifying high-risk patients (ODX-RS ≥ 26). The MCM-2 proliferation marker could help clinicians in patients where an ODX-RS assay cannot be performed to determine adjuvant treatment due to economic reasons and other reasons. Accepting 50 as the cutoff value for MCM-2 might contribute to identifying patients who should receive adjuvant chemotherapy with high sensitivity and specificity.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Ethics committee approval was obtained from Istanbul Bilgi University (project number: 2021-40034-11). It is performed in accordance with the Declaration of Helsinki. All patients were informed, and consent forms were signed.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare that they have no competing interests.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. International Agency for Research on Cancer GLOBOCAN. 2020 population fact sheets 3 2021 international agency for research on cancer. GLOBOCAN; 2021. Available from: https://gco.iarc.fr/today/data/factsheets/populations/792-turkey-fact-sheets.pdf.
3. Özmen V, Özmen T, Doğru V. Breast cancer in Turkey; an analysis of 20.000 patients with breast cancer. Eur J Breast Health. 2019;15(3):141. PMID: 31312788 PMCID: PMC6619786. doi:10.5152/ejbh.2019.4890
4. Howlader N, Altekruse SF, Li CI, et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;106(5):dju055. doi:10.1093/jnci/dju055
5. Neves H, Kwok HF. In sickness and in health: the many roles of the minichromosome maintenance proteins. Biochim Biophys Acta Rev Cancer. 2017;1868(1):295–308. doi:10.1016/j.bbcan.2017.06.001
6. Wang Y, Chen H, Zhang J, et al. MCM family in gastrointestinal cancer and other malignancies: from functional characterization to clinical implication. Biochim Biophys Acta. 2020;2020:1874.
7. Maiorano D, Lutzmann M, Mechali M. MCM proteins and DNA replication. Curr Opin Cell Biol. 2006;18:130–136. doi:10.1016/j.ceb.2006.02.006
8. Pruitt SC, Bailey KJ, Freeland A. Reduced Mcm2 expression results in severe stem/progenitor cell deficiency and cancer. Stem Cells. 2007;25:3121–3132. doi:10.1634/stemcells.2007-0483
9. Wu W, Wang X, Shan C, Li Y, Li F. Minichromosome maintenance protein 2 correlates with the malignant status and regulates proliferation and cell cycle in lung squamous cell carcinoma. Onco Targets Ther. 2018;11:5025–5034. doi:10.2147/OTT.S169002
10. Obermann Ellen C, Went P, Zimpfer A, et al. Expression of minichromosome maintenance protein 2 as a marker for proliferation and prognosis in diffuse large B-cell lymphoma: a tissue microarray and clinico-pathological analysis. BMC Cancer. 2005;5(1):1–8. doi:10.1186/1471-2407-5-1
11. Ramnath N, Hernandez FJ, Tan DF, et al. MCM2 is an independent predictor of survival in patients with nonsmall- cell lung cancer. J Clin Oncol. 2001;19:4259–4266. doi:10.1200/JCO.2001.19.22.4259
12. Issac MSM, Yousef E, Tahir MR, Gaboury LA. MCM2, MCM4, and MCM6 in breast cancer: clinical utility in diagnosis and prognosis. Neoplasia. 2019;21:1015–1035. doi:10.1016/j.neo.2019.07.011
13. Gonzalez MA, Pinder SE, Callagy G, et al. Minichromosome maintenance protein 2 is a strong independent prognostic marker in breast cancer. J Clin Oncol. 2003;21:4306–4313. doi:10.1200/JCO.2003.04.121
14. Chen R, Hu B, Jiang M, et al. Bioinformatic analysis of the expression and clinical significance of the DNA replication regulator MCM complex in bladder cancer. Int J Gen Med. 2022;Volume 15:5465–5485. doi:10.2147/IJGM.S368573
15. Zhou J, Wang M, Zhou Z, et al. Expression and prognostic value of MCM family genes in osteosarcoma. Front Mol Biosci. 2021;8:668402. doi:10.3389/fmolb.2021.668402
16. Lin CY, Wu HY, Hsu YL, et al. Suppression of drug-resistant non-small-cell lung cancer with inhibitors targeting minichromosomal maintenance protein. J Med Chem. 2020;63:3172–3187. doi:10.1021/acs.jmedchem.9b01783
17. Harris LN, Ismaila N, McShane LM, et al. Use of biomarkers to guide decisions on adjuvant systemic therapy for women with early-stage invasive breast cancer: American society of clinical oncology clinical practice guideline. J Clin Oncol. 2016;34(10):1134–1150. doi:10.1200/jco.2015.65.2289
18. Gradishar WJ, Anderson BO, Balassanian R, et al. Breast cancer, version 1 2016. J Natl Compr Canc Netw. 2015;13(12):1475–1485. doi:10.6004/jnccn.2015.0176
19. Henry NL, Somerfield MR, Abramson VG, et al. Role of patient and disease factors in adjuvant systemic therapy decision making for early-stage, operable breast cancer: American society of clinical oncology endorsement of cancer care Ontario guideline recommendations. J Clin Oncol. 2016;34(19):2303–2311. doi:10.1200/jco.2015.65.8609
20. Sparano Joseph A, Gray RJ, Makower DF, et al. Adjuvant chemotherapy guided by a 21-gene expression assay in breast cancer. N Engl J Med. 2018;379(2):111–121. doi:10.1056/NEJMoa1804710
21. Updated TAILORx results confirm women with intermediate recurrence score can skip chemotherapy. Available from: https://www.breastcancer.org/research-news/updated-tailorx-results-confirm-women-with-intermediate-recurrence-score-can-skip-chemotherapy.
22. Özmen V, Çakar B, Gökmen E, et al. Cost effectiveness of gene expression profiling in patients with early-stage breast cancer in a middle-income country, Turkey: results of a prospective multicenter study. Eur J Breast Health. 2019;15(3):183.
23. Ozmen V, Atasoy A, Gokmen E, et al. Correlations between Oncotype DX Recurrence Score and classic risk factors in early breast cancer: results of a prospective multicenter study in Turkey. J Breast Health. 2016;12:107–111. doi:10.5152/tjbh.2016.2874
24. Ozmen V, Atasoy A, Gokmen E, et al. Impact of Oncotype DX Recurrence Score on treatment decisions: results of a prospective multicenter study in Turkey. Cureus. 2016;8(3):30.
25. Panousis D, Ntasiou P, Grosomanidis D, et al. Impact of Oncotype DX on chemotherapy assignment: a retrospective single-center study on female breast cancer patients. therapy. 2017;15:20.
26. Thakur SS, Li H, Chan AMY, et al. The use of automated Ki67 analysis to predict Oncotype DX risk-of-recurrence categories in early-stage breast cancer. PLoS One. 2018;13(1):e0188983. doi:10.1371/journal.pone.0188983
27. Crager M, Wijayawardana SR, Gruver AM, et al. Population-based estimate for the correlation of the Oncotype DX Breast Recurrence Score® result and Ki-67 IHC MIB-1 pharmDx in HR+, HER2−, node-positive early breast cancer. Breast Cancer Res. 2022;24:1–7. doi:10.1186/s13058-022-01571-7
28. Pilanci KN, Unal C, Ordu C, et al. Correlation between clinicopathologic factors and recurrence score according to TAILOR x risk category in patients with hormone receptor positive early-stage breast cancer. J BU ON. 2021;2021:1.
29. Piccart M, Van’t Veer LJ, Poncet C, et al. 70-gene signature as an aid for treatment decisions in early breast cancer: updated results of the Phase 3 randomised MINDACT trial with an exploratory analysis by age. Lancet Oncol. 2021;22(4):476–488. doi:10.1016/S1470-2045(21)00007-3
30. Andre F, Ismaila N, Allison KH, et al. Biomarkers for adjuvant endocrine and chemotherapy in early-stage breast cancer: ASCO guideline update. J Clin Oncol. 2022;40:1816–1837. doi:10.1200/JCO.22.00069
31. NCCN. NCCN clinical Practice guidelines in oncology V.2. Breast Cancer; 2023. Available from: https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf.
32. Paik S, Tang G, Shak S, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24:3726–3734. doi:10.1200/JCO.2005.04.7985
33. Gluz O, Nitz UA, Christgen M, et al. West German study group phase III planb trial: first prospective outcome data for the 21-gene recurrence score assay and concordance of prognostic markers by central and local pathology assessment. J Clin Oncol. 2016;34:2341–2349. doi:10.1200/JCO.2015.63.5383
34. Tang G, Shak S, Paik S, et al. Comparison of the prognostic and predictive utilities of the 21-gene recurrence score assay and adjuvant! For women with node-negative, ER-positive breast cancer: results from NSABP B-14 and NSABP B-20. Breast Cancer Res Treat. 2011;127:133–142. doi:10.1007/s10549-010-1331-z
35. Lopez F, Belloc F, Lacombe F, et al. Modalities of synthesis of Ki67 antigen during the stimulation of lymphocytes. Cytometry. 1991;12:42–49. doi:10.1002/cyto.990120107
36. Gerdes J, Lemke H, Baisch H, et al. Cell cycle analysis of a cell proliferation-associated human nuclear antigen defined by the monoclonal antibody Ki-67. J Immunol. 1984;133:1710–1715. doi:10.4049/jimmunol.133.4.1710
37. Van Dierendonck JH, Keijzer R, van de Velde CJ, et al. Nuclear distribution of the Ki-67 antigen during the cell cycle: comparison with growth fraction in human breast cancer cells. Cancer Res. 1989;49:2999–3006.
38. Clark BZ, Dabbs DJ, Cooper KL, Bhargava R, Thakur SS, Li H. Impact of progesterone receptor semiquantitative immunohistochemical result on Oncotype DX recurrence score: a quality assurance study of 1074 cases. Appl Immunohistochem Mol Morphol. 2013;21(4):287–291. doi:10.1097/PAI.0b013e31826f80c9
39. Park S, Han Y, Liu Y, et al. Adjuvant chemotherapy and survival among patients 70 years of age and younger with node-negative breast cancer and the 21-gene recurrence score of 26–30. Breast Cancer Res. 2019;21(1):1–11. doi:10.1186/s13058-019-1190-4
40. Mosley JD, Keri RA. Cell cycle correlated genes dictate the prognostic power of breast cancer gene lists. BMC Med Genomics. 2008;1:11. doi:10.1186/1755-8794-1-11
41. Heidebrecht HJ, Buck F, Haas K, et al. Monoclonal antibodies Ki-S3 and Ki-S5 yield new data on the ‘Ki-67’ proteins. Cell Prolif. 1996;29:413–425. doi:10.1111/j.1365-2184.1996.tb00984.x
42. Laskey R. The Croonian Lecture 2001 hunting the antisocial cancer cell: MCM proteins and their exploitation. Philos Trans R Soc Lond B Biol Sci. 2005;360:1119–1132. doi:10.1098/rstb.2005.1656
43. Joshi S, Watkins J, Gazinska P, et al. Digital imaging in the immunohistochemical evaluation of the proliferation markers Ki67, MCM2 and Geminin, in early breast cancer, and their putative prognostic value. BMC Cancer. 2015;15:1–12. doi:10.1186/s12885-015-1531-3
44. Wojnar A, Kobierzycki C, Krolicka A, et al. Correlation of Ki-67 and MCM-2 proliferative marker expression with grade of histological malignancy (G) in ductal breast cancers. Folia Histochem Cytobiol. 2010;48(3):442–446. doi:10.2478/v10042-010-0069-0
45. Shetty A, Loddo M, Fanshawe T, et al. DNA replication licensing and cell cycle kinetics of normal and neoplastic breast. Br J Cancer. 2005;93:1295–1300. doi:10.1038/sj.bjc.6602829
46. Tőkés T, Tőkés A-M, Szentmártoni G, et al. Prognostic and clinicopathological correlations of cell cycle marker expressions before and after the primary systemic therapy of breast cancer. Pathol Oncol Res. 2020;26:1499–1510. doi:10.1007/s12253-019-00726-w
47. Yousef EM, Furrer D, Laperriere DL, et al. MCM2: an alternative to Ki-67 for measuring breast cancer cell proliferation. Mod Pathol. 2017;30(5):682–697. doi:10.1038/modpathol.2016.231
48. Sakai H, Kimura H, Otsubo K, et al. Minichromosome maintenance 2 is an independent predictor of survival in patients with lung adenocarcinoma. Mol Clin Oncol. 2022;14:1–7.
49. Samad A, Haque F, Nain Z, et al. Computational assessment of MCM2 transcriptional expression and identification of the prognostic biomarker for human breast cancer. Heliyon. 2020;6(10):e05087. doi:10.1016/j.heliyon.2020.e05087
50. Loddo M, Kingsbury SR, Rashid M, et al. Cell-cycle-phase progression analysis identifies unique phenotypes of major prognostic and predictive significance in breast cancer. Br J Cancer. 2009;100:959–970. doi:10.1038/sj.bjc.6604924
51. Ünal Ç, Tunçer G, Çopur B, et al. Clinical and inflammation marker features of cancer patients with COVID-19: data of Istanbul, Turkey multicenter cancer patients (2020–2022). Curr Med Res Opin. 2023;39(7):987–996. doi:10.1080/03007995.2023.2223917
52. Kalelioglu T, Karamustafalioglu N, Emul M, et al. Detecting biomarkers associated with antipsychotic-induced extrapyramidal syndromes by using machine learning techniques. J Psychiatr Res. 2023;158:300–304. doi:10.1016/j.jpsychires.2023.01.003
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



