Back to Journals » Neuropsychiatric Disease and Treatment » Volume 20
Link Between Obsessive-Compulsive Disorder and ApoE Gene Polymorphisms
Authors Dondu A , Caliskan M, Orenay-Boyacioglu S
Received 10 October 2023
Accepted for publication 20 December 2023
Published 24 January 2024 Volume 2024:20 Pages 159—166
DOI https://doi.org/10.2147/NDT.S441128
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Ayse Dondu,1 Metin Caliskan,2 Seda Orenay-Boyacioglu3
1Department of Psychiatry, Aydın Goverment Hospital, Aydin, 09010, Turkey; 2Department of Medical Biology, Faculty of Medicine, Usak University, Usak, 64000, Turkey; 3Department of Medical Genetics, Faculty of Medicine, Aydin Adnan Menderes University, Aydin, 09010, Turkey
Correspondence: Ayse Dondu, Department of Psychiatry, Aydın Goverment Hospital, Aydin, Turkey, Email [email protected]
Objective: Many researchers have considered obsessive compulsive disorder (OCD) to be a neurodegenerative disease just like Alzheimer’s disease (AD). The most studied gene in neurodegenerative diseases is apolipoprotein E (ApoE) gene, and ApoE ɛ4 allele in particular. Although a small number of studies have explored the relationship between ApoE gene polymorphisms and OCD, the link between age at onset of OCD, its subtypes and ApoE gene polymorphisms has not been revealed so far. For this purpose, in our study, the relationship of ApoE gene polymorphisms with age at onset of OCD and its subtypes has been investigated to reveal their neurodegenerative connections.
Patients and Methods: ApoE gene polymorphisms of 64 OCD and 28 healthy cases were studied using a LightCycler480 real-time PCR platform.
Results: A statistically significant difference was found between groups of patients with early- and late-onset OCD in terms of age (p = 0.03), educational level (p = 0.00) and marital status (p = 0.002). ApoE ɛ4ɛ4 genotype, the prevalence of which is below 2% in healthy individuals, was not detected in our control groups; however, it was identified in 5.1% of our OCD cases. Correlation analysis revealed the presence of a potentially significant link between the hoarding obsession and presence of the ɛ4ɛ4 genotype. A significant correlation was detected between the presence of the ɛ3ɛ3 allele, the symmetry obsession and associated ordering compulsion in patients with OCD (p< 0.005).
Conclusion: The ApoE gene polymorphism profile and age of onset in OCD patients may play critical roles in the development process of neurodegenerative characteristics of the disease. The small number of cases and the inability to perform brain imaging in patients to detect the neurodegenerative link in OCD are limitations of our study. In this respect, we suggest conduction of further studies with a greater number of patients who will also undergo brain imaging studies. In addition, OCD patients have other genes associated with neurodegenerative diseases that can be screened.
Keywords: early-onset OCD, late-onset OCD, Alzheimer‘s disease, apoe gene, polymorphism
Introduction
Obsessive compulsive disorder (OCD) is a debilitating disease characterized by repetitive, intrusive and unwanted thoughts, impulses, and images, often associated with recurrent, time-consuming and frequently ritualized compulsive behaviour.1 Many studies have shown that OCD is a frontal lobe/basal ganglia disorder that shares links with neurodegenerative disorders such as malfunctioning of cortico–striato–thalamo–cortical circuitry, autism, schizophrenia, Tourette syndrome, and frontal lobe dementia.2–4 In addition, neuropsychological findings in cognitive impairments related to spatial working memory, spatial recognition, and motor initiation and execution have been observed in OCD, and also in some other neurodegenerative diseases such as Alzheimer’s disease (AD).5–9 In our previous study, obsessive-compulsive symptoms had been observed in AD, which suggested that pre-existing obsessive-compulsive symptoms may predispose individuals to developing dementia in later life in the case of true memory deficit.10 Some researchers have suggested that OCD may be a new risk factor for AD, considering that glutamatergic dysfunction may be a common pathophysiology shared by OCD and AD.11
Apolipoprotein E (ApoE), the most common brain lipoprotein, is expressed in the brain in three major isoforms (ApoE ε2, ApoE ε3 and ApoE ε4).12 The ApoE gene has been studied comprehensively in neurodegenerative and some psychiatric disorders.12,13 The ApoE isoform-specific effect is hypothesized to contribute to the pathogenesis of AD by impairing synaptic activity on ApoE receptor-2 and via NMDA/AMPA receptor trafficking. In contrast, neuronal maturation in ApoE ε4 knock-in mice is impaired due to the reduced survival and suppressed function of GABAergic interneurons in the hilum of the hippocampus and the potential of a GABAA receptor to rescue the ApoEε4-related reduction in hippocampal neurogenesis. Thus, ApoE contributes to adult hippocampal neurogenesis, and ApoE ε4 impairs GABAergic input to neonatal neurons, resulting in decreased neurogenesis.14
A limited number of studies in the literature have investigated the relationship between OCD, which is thought to be a neurodegenerative disease, and the ApoE gene, which is widely studied in neurodegenerative diseases. Therefore, in this study, the relationship of ApoE gene polymorphisms with age at onset of OCD and subtypes of the disease was investigated in order to reveal the neurodegenerative/AD link in OCD. ApoE gene polymorphism profile and age at onset of OCD may play a critical role in the development of the neurodegenerative manifestations of the disease.
Patients and Methods
Ethics and Participants
This study has been approved by the Institutional Non-Interventional Ethics Committee (2018/1447) in accordance with the Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects. An informed consent form was obtained from all participants prior to initiation of the study.
A total of 64 patients who applied to the Aydın State Hospital Psychiatry Outpatient Clinic and were diagnosed with OCD were included in the study. Five OCD patients who could not be genotyped were not included in the study, and the study was continued with 48 female and 11 male OCD cases. Patients received the diagnosis of OCD based on the Structured Clinical Interviews for Axis I Disorders (SCID) criteria of the Diagnostic and Statistical Manual of Mental Disorders.15,16 The Yale-Brown Obsessive Compulsive Scale (Y-BOCS) was used to determine the severity of OCD symptoms.17 OCD types were defined using the Y-BOCS symptom checklist. The Hamilton Depression Rating Scale (HDRS) and Hamilton Anxiety Rating Scale (HARS) were applied to all cases. The cases were divided into two groups based on age at onset of OCD. Cases with onset of OCD at 15 years or younger (n = 28) were considered to have early-onset OCD, and patients who had developed OCD after the age of 15 years (n = 31) were considered to have late-onset OCD. The control group contained 28 healthy people with no psychiatric or neurodegenerative diseases, who were matched with OCD cases as much as possible in terms of age and gender. Patients with psychotic disorders, autism spectrum disorders, other anxiety disorders, bipolar disorder, mental retardation, any organic mental disorder, and with a history of smoking and substance use were excluded from the study.
Genotyping
DNA was isolated from participants’ peripheral blood samples using a QIAamp DNA Blood Mini Kit (Qiagen, Hilden, Germany) in accordance with the instructions of the manufacturing company. Using isolated DNA samples, two mutations defined in codon 112 and codon 158 in the ApoE gene were studied. ApoE gene genotyping was performed using a LightMix Kit ApoE C112R R158C kit in accordance with the recommendations of the manufacturing company. A 228 bp fragment of the human ApoE gene was amplified using Real-Time PCR (Roche LightCycler480 I Instrument). Probe 519 (APOE C112R, channel 530), a Simple Probe®, and hybridization probes (APOE R158C, channel 640) labelled with Light Cycler Red 640 were used during the analysis.
Statistical Analyses
Mean, standard deviation, median and percentage values were used for descriptive statistics. Statistical analyses were performed using SPSS version 22.0 (SPSS Inc., Chicago, IL, USA). The chi-square test was used for categorical variables and the student’s t-test was used to compare independent data. Results were considered statistically significant at p<0.05.
Results
Sociodemographic and Clinical Features
In the one-to-one comparisons between early- and late-onset OCD patient groups and healthy controls we observed that those in the early-onset OCD group (n=28) were younger than both those in the late-onset OCD group (n = 31) and healthy controls (n=28); those in the control group were more highly educated (Table 1). In addition, the late-onset OCD group contained a greater number of female and unmarried participants when compared to the other groups. A significantly greater number of patients in the OCD group had suffered from depression compared to the healthy control group (p = 0.00).
 |
Table 1 Comparative Analysis of Groups in Terms of Demographic and Clinical Characteristics |
The average ages at onset of those classified as early- and late-onset OCD were 12.8 and 28.7 years, respectively. No patients in the OCD groups were using medication during their blood-letting periods; some were newly diagnosed, while others had received a diagnosis of OCD in the past but had discontinued their drug therapies.
There was no statistically significant difference in terms of symptomatology between obsession and compulsion subtypes of OCD, and also regarding Y-BOCS total and sub-scores, HARS and HDRS scores between early- and late-onset OCD (p>0.05). Only hoarding obsessions tended to be more frequent in the group with early-onset OCD. In the early-onset OCD group, cleaning, symmetry, and control rituals were more frequently observed while, in the late-onset OCD group, obsessive cleaning disorder was more often encountered.
Genetic Assessments
No statistically significant relationship could be identified in terms of ApoE genotypes between the early- and late-onset OCD groups compared to the control group (p>0.05). However, the ApoEɛ4ɛ4 genotype, which is associated with AD disease and observed at a rate below 2% in the population at large, was not detected in healthy controls, but was detected in 5.1% of our cases with OCD. ApoE ɛ4ɛ4, ɛ3ɛ3 ɛ2ɛ3, and ɛ3ɛ4 genotype frequencies differed in the early- and late-onset OCD groups and also in the control group; the ɛ2ɛ4 and ɛ2ɛ2 genotypes were not detected in any of the groups (Table 2).
 |
Table 2 Distribution Characteristics of ApoE Gene Polymorphisms in Study Group |
ApoE genotypes/alleles were evaluated in terms of age, gender, marital status, Y-BOCS total and sub-scores, depression and anxiety scores, and no statistically significant difference was found between different types of OCD (p>0.05). The results of our correlation analysis suggest the presence of a potentially significant relationship between hoarding obsessions and the presence of the ɛ4ɛ4 genotype (p<0.005). A significant correlation was found between the presence of the ɛ3ɛ3 genotype in OCD patients with symmetry obsession and related ordering compulsions (p<0.005) (Table 3).
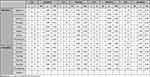 |
Table 3 Distribution Characteristics of ApoE Gene Polymorphisms in Obssession/Compulsion |
Discussion
With this study, a first in the medical literature, we aimed to investigate the relationship between ApoE gene polymorphisms, age at onset and subtypes of OCD so as to demonstrate the neurodegenerative link in OCD.
Although complaints of forgetfulness are common in OCD, many studies have revealed impairments in cognitive and executive functions, suggesting the presence of a neurodegenerative process in OCD.17 Many neuropsychological and imaging studies have showed the poor and slack performance of OCD patients on executive function tasks.18,19 However, few studies have been performed on early- and late-onset OCD. Contrary to expectations, in the study of Segalas et al, tests evaluating executive functioning, visual memory, and verbal memory in late-onset OCD yielded worse results when compared with those of early-onset OCD.20 In our study, carried out in 2015, obsessive characteristics were significantly more frequently observed in patients with a history of AD when compared with the healthy group.10 A case report demonstrated that the emergence of advanced cognitive impairment in a treatment-refractory late-onset OCD patient may result from an interaction between nonspecific effects of a neurodegenerative process.4
Although there are conflicting reports concerning the relationships between ApoE gene polymorphisms (except for the ɛ4ɛ4 genotype) and AD, the ApoE ɛ4ɛ4 genotype has been counted as a risk factor for AD and other forms of dementia. The above-mentioned information and research led us to investigate the distribution of the ApoE genotype in OCD patients in order to determine its neurodegenerative link with OCD.10
In the literature, few studies have examined the relationship between ApoE gene polymorphisms and OCD. In the study of Nicolini et al (2001), a significant difference was detected when ApoE gene polymorphisms in OCD were compared with those observed in population control groups among OCD probands.14 However, the ApoEɛ4ɛ4 genotype was detected at a higher rate in the cognitively impaired group when compared with normal controls and OCD patients. Khiari et al (2011) detected the ɛ3ɛ3 genotype in family members of patients with a history of OCD and correlated it with late-onset AD.9 In our study, in contrast to that of Nicolini et al, no statistically significant relationship could be detected in pairwise comparisons between early- and late-onset OCD and the control group regarding the ApoE genotype. However, based on the fact that the presence of the ɛ4ɛ4 genotype in control groups has been reported as below 2% in the literature,21,22 and our higher (≤ twofold) detection rate of this genotype in OCD cases relative to the control group in our study, the ɛ4ɛ4 genotype will be considered as a risk factor for OCD, suggesting the presence of a possible link between OCD and AD.
Pievanin et al (2013), revealed the presence of a relationship between strial atrophy and ApoE genotypes in early- and late-onset AD. It has been detected that the dorsal striatum is more severely affected in early-onset AD compared with late-onset AD. The ventral striatum is associated with limbic and behavioural symptoms, and its dorsal part is more closely linked to motor functions. It has been suggested that the ApoE genotype has an effect on strial and clinical variables in patients with early- and late-onset AD.23 Accordingly, in our study, when the relationship between OCD symptomatology and ApoE gene polymorphisms was examined, a significant relationship was detected between the ApoE e3e3 genotype and symptomatology in OCD patients with symmetry obsessions and an ordering compulsion. A potentially significant relationship has been detected between hoarding obsessions and the ɛ4ɛ4 genotype.
In the literature, a significant discrepancy has been detected in the results of tests examining the cognitive functions of OCD patients with symmetry obsessions compared to other types of obsession. Greatly impaired visuospatial working memory has been detected in patients with a severe symmetry obsession. In some other studies the responses of those with a symmetry obsession have shown their progressively worsening condition. The problems in visual memory and visuospatial ability have been shown in studies on motor slowing.24,25 Jalal et al (2010)26 compared OCD symptomatology with non-verbal memory and organizational strategies, and observed that the group with symmetry/ordering and checking obsessions were following a significantly and progressively worsening disease course. In this study, it has been agreed that the disruption between checking obsessions and non-verbal memory is related to anxiety rather than symmetry obsession. We examined symptoms related to aggression, order, contamination, hoarding, and sexual and religious dimensions. In this very different OCD model, hoarding and symmetry obsessions were found to be associated with early-onset OCD, and eating and addictive disorders were observed more frequently in patients with symmetry and ordering symptoms. In OCD patients with symmetry/ordering symptoms, a decrease in the volumes of the right precentral gyrus and hippocampus was observed.23 In those with symmetry obsession, detection of the e3e3 genotype probably suggests the presence of a common brain involvement related to AD, which may be genetically responsible for these pathologic alterations.9 In our study, similar to the literature, patients with the ApoE gene polymorphisms (e3e3 and e4e4) found in those with OCD displayed symmetry, ordering and hoarding symptoms. Impaired cognitive functions in some of the OCD patients can be explained by polymorphisms in this gene. Our study suggests that the ApoE e3e3 allele may be genetically related to non-verbal memory problems in OCD.
Limitations
The small number of cases and inability to perform brain imaging in patients to detect neurodegenerative links in OCD are limitations of our study. In this respect, we suggest conduction of further studies with a greater number of patients who will also undergo brain imaging studies. In addition, OCD patients have other genes associated with neurodegenerative diseases that can be screened.
Conclusion
Since OCD represents a very heterogeneous group of diseases, detection of the genetic relationships and genes responsible for the onset of symptomatic disease and, accordingly development of treatment strategies for disease-specific phenotypes can be more effective ways of both understanding the etiologic factors in OCD and disclosing its neurodegenerative/AD link. This study is the first in the literature to investigate the relationship between ApoE gene polymorphisms, age at onset and subtypes of OCD so as to demonstrate the neurodegenerative/AD link in OCD. Based on the results of this and similar studies, a new marker can be created by considering ApoE gene polymorphisms in order to define a patient carrying a high risk of developing OCD. In addition, neurodegenerative impairment in OCD subtypes may play a decisive role in the prognosis of these patients.
Data Sharing Statement
The combined datasets and materials are available upon reasonable request.
Ethics Approval
Approval for the conduction of the study was received from the Institutional Ethics Committee of Aydın Adnan Menderes University (May 12, 2018, decision no. 2018/1447).
Funding
The authors have not received support from any organization for the submitted study.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Alegría M, Frank RG, Hansen HB, Sharfstein JM, Shim RS, Tierney M. Transforming Mental Health And Addiction Services: commentary describes steps to improve outcomes for people with mental illness and addiction in the United States. Health Affairs. 2021;40(2):226–234. doi:10.1377/hlthaff.2020.01472
2. Endres D, von Zedtwitz K, Urbach H, et al. Obsessive-compulsive symptoms in two patients with strategic basal ganglia lesions. Mol Psychiatry. 2023;28(2):528–531. doi:10.1038/s41380-022-01853-8
3. Lamothe H, Schreiweis C, Mondragón-González LS, et al. The Sapap3−/− mouse reconsidered as a comorbid model expressing a spectrum of pathological repetitive behaviours. Transl Psychiatry. 2023;13(1):26. doi:10.1038/s41398-023-02323-7
4. Ruggeri M, Ricci M, Gerace C, Blundo C. Late-onset obsessive-compulsive disorder as the initial manifestation of possible behavioural variant Alzheimer’s disease. Cognitive Neuropsychiatry. 2022;27(1):11–19. doi:10.1080/13546805.2021.1996342
5. Tripathi PN, Srivastava P, Sharma P, et al. Biphenyl-3-oxo-1, 2, 4-triazine linked piperazine derivatives as potential cholinesterase inhibitors with anti-oxidant property to improve the learning and memory. Bioorg Chem. 2019;85:82–96. doi:10.1016/j.bioorg.2018.12.017
6. Srivastava P, Tripathi PN, Sharma P, et al. Design and development of some phenyl benzoxazole derivatives as a potent acetylcholinesterase inhibitor with antioxidant property to enhance learning and memory. Eur J Med Chem. 2019;163:116–135. doi:10.1016/j.ejmech.2018.11.049
7. Rai SN, Zahra W, Birla H, Singh SS, Singh SP. Commentary: mild endoplasmic reticulum stress ameliorates lpopolysaccharide-induced neuroinflammation and cognitive impairment via regulation of microglial polarization. Front Aging Neurosci. 2018;10:192. doi:10.3389/fnagi.2018.00192
8. Rai SN, Singh C, Singh A, Singh MP, Singh BK. Mitochondrial dysfunction: a potential therapeutic target to treat Alzheimer’s disease. Mol Neurobiol. 2020;57(7):3075–3088. doi:10.1007/s12035-020-01945-y
9. Khiari HM, Achouri A, N.b A, et al. Obsessive–compulsive disorder: a new risk factor for Alzheimer disease? Neurol Sci. 2011;32(5):959–962. doi:10.1007/s10072-011-0480-0
10. Dondu A, Sevicok L, Akyol A, Tataroglu C. Is obsessive–compulsive symptomatology a risk factor for Alzheimer-type dementia? Psychiatry Res. 2015;225(3):381–386. doi:10.1016/j.psychres.2014.12.010
11. Dadkhah R, Baradaran HR, Almasi-Dooghaee M, Janmohammadi F, Shalbafan M, Heidari A The relationship between the severity of obsessive compulsive disorder (OCD) and Alzheimer’s disease (AD) and frontotemporal dementia (FTD); 2022.
12. Chen Y, Strickland MR, Soranno A, Holtzman DM. Apolipoprotein E: structural insights and links to Alzheimer disease pathogenesis. Neuron. 2021;109(2):205–221. doi:10.1016/j.neuron.2020.10.008
13. Luo T, Tu YF, Huang S, et al. Alzheimer’s Disease Neuroimaging Initiative (ADNI). The time‐dependent impact of type 2 diabetes mellitus on incident prodromal Alzheimer’s disease: a longitudinal study in 1395 participants. Eur J Neurol. 2023;30(9):2620–2628. doi:10.1111/ene.15868
14. Nicolini H, Urraca N, Camarena B, et al. Lack of association of apolipoprotein E polymorphism in obsessive-compulsive disorder. CNS Spectrums. 2001;6(12):978–979. doi:10.1017/S1092852900001085
15. First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version Patient Edition. SCID-I/P: New York; 2002. 91.
16. Sertçelik S, Gündoğmuş İ, Gündüz A, Eroğlu MZ, Çipil A, Ergün N. Psychometric properties of the diagnostic interview for adult attention-deficit/hyperactivity disorder 2.0 Turkish version. Psychiatr Ann. 2022;52(2):76–84. doi:10.3928/00485713-20220125-02
17. Vogt GS, Avendaño-Ortega M, Schneider SC, Goodman WK, Storch EA. Optimizing obsessive-compulsive symptom measurement with the yale-brown obsessive-compulsive scales—second edition. J Psychiatr Pract. 2022;28(4):294–309. doi:10.1097/PRA.0000000000000640
18. Nam SH, Park J, Kim GW, Moon CM, Yang JC. Neural correlates of emotion–cognition interaction during working memory maintenance in obsessive-compulsive disorder: the role of the dorsolateral prefrontal cortex. Psychiatr Clin Psychopharmacol. 2022;32(4):344–350.
19. Heinzel S, Kaufmann C, Grützmann R, et al. Polygenic risk for obsessive-compulsive disorder (OCD) predicts brain response during working memory task in OCD, unaffected relatives, and healthy controls. Sci Rep. 2021;11(1):1. doi:10.1038/s41598-021-98333-w
20. Segalas C, Alonso P, Labad J, Jaurrieta N, Real E. Jiménez S, et al.Verbal and nonverbal memory processing in patients with obsessive-compulsive disorder: its relationship to clinical variables. Neuropsychology. 2008;22(2):262. doi:10.1037/0894-4105.22.2.262
21. Stakias N, Liakos P, Tsiapali E, Gutu M, Koukoulis GN. Lower prevalence of epsilon 4 allele of apolipoprotein E gene in healthy, longer-lived individuals of Hellenic origin. J Gerontol. 2006;61(12):1228–1231. doi:10.1093/gerona/61.12.1228
22. Li W. Association of APOE E2 and low-density lipoprotein with depressive symptoms in Chinese senile schizophrenia inpatients: a cross-sectional study. Schizophr Res. 2021;23:100193. doi:10.1016/j.scog.2020.100193
23. Barker MS, Cosentino SA, Fremont R, Devanand DP, Huey ED. Towards defining the neuroanatomical basis of late-onset psychiatric symptoms. J Geriatric Psychiatry Neurol. 2022;35(6):751–762. doi:10.1177/08919887221090213
24. Simón-Martínez V, Laseca-Zaballa G, Lubrini G, et al. Cognitive deficits and clinical symptoms in patients with treatment-refractory obsessive–compulsive disorder: the role of slowness in information processing. Psychiatry Res. 2021;304:11414. doi:10.1016/j.psychres.2021.114143
25. Palit A, Roy PK, Saha PK. Role of prospective memory in obsessive compulsive disorder. Indian J Psychol Med. 2022;44(6):586–591. doi:10.1177/02537176221100846
26. Jalal B, Chamberlain SR, Sahakian BJ. Obsessive‐compulsive disorder: etiology, neuropathology, and cognitive dysfunction. Brain Behav. 2023;13(6):e3000. doi:10.1002/brb3.3000
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
