Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 15
Knowledge, Practice, and Associated Factors Towards Supplemental Oxygen Therapy Among Nurses Working in Neonatal Intensive Care Units in Public Hospitals of Addis Ababa, Ethiopia, 2022: A Cross-Sectional Study
Authors Dansa A , Gela D , Kebede MA
Received 17 October 2023
Accepted for publication 8 February 2024
Published 12 February 2024 Volume 2024:15 Pages 77—86
DOI https://doi.org/10.2147/PHMT.S445087
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Assefa Dansa,1 Debela Gela,2 Mekonen Adimasu Kebede2
1Department of Nursing, College of Health Sciences, Wolaita Sodo University, Wolaita Sodo, Ethiopia; 2Department of Nursing, School of Nursing and Midwifery, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Mekonen Adimasu Kebede, Department of Nursing, School of Nursing and midwifery, College of Health Sciences, Addis Ababa University, P O Box 0.1176, Addis Ababa, Ethiopia, Tel +2519-17724019, Email [email protected]
Purpose: Proper administration of oxygen therapy for hospitalized newborns is undoubtedly essential. World Health Organization estimates that approximately 1.4 million deaths worldwide each year are due to inappropriate administration of oxygen, but its administration in clinical practice is usually inappropriate due to lack of knowledge and practice. Therefore, the aim of this study was to determine the level of knowledge, practice and associated factors related to supplemental oxygen therapy among nurses working in neonatal intensive care units.
Methods: An institutional cross-sectional study was conducted with 166 randomly selected respondents using a self-administered questionnaire for data collection. Bivariate and multivariable analyses were performed using SPSS version 26. Variables with a p-value of < 0.25 in the bivariate analysis were included in the multivariable logistic regression, and statistical significance was ensured by a p-value < 0.05 with 95% CI.
Results: One hundred and sixty-six nurses took part in this study, with a response rate of 96%. Of these, 60.8% had good knowledge and 54.2% had good practice in supplemental oxygen therapy. In the multivariable logistic regression analysis, work experience was significantly associated with knowledge (AOR: 5.40; 95% CI: 2.12– 13.73)) and practice (AOR = 3.69, 95% CI: 1.30– 10.44)) of supplemental oxygen therapy. Level of knowledge (AOR=2.92, 95% CI: (1.24– 6.86)) and educational status (AOR=6.51, 95% CI (1.34– 31.55)) were also significantly associated with the practice of supplemental oxygen therapy with a p < 0.05.
Conclusion: Approximately 40% and 46% of nurses in this study had poor knowledge and practice of supplemental oxygen therapy. This figure is shocking and shows a large gap in the knowledge and practice of supplemental oxygen therapy that requires urgent action. Educational status, professional experience and level of knowledge were found to be associated with good knowledge and professional experience with good practice in relation to supplemental oxygen therapy.
Keywords: knowledge, practice, neonatal nurse, oxygen therapy, neonatal intensive care unit
Introduction
Oxygen was discovered in the late 17th century and is considered to be the molecule of greatest importance for human beings.1 Supplemental oxygen therapy (SOT) is used to treat and prevent neonatal hypoxia by providing additional oxygen for neonates with respiratory distress.2 It is a life-saving medicine with acceptable dosage ranges even though higher dose and prolonged use is associated with severe toxic symptoms and physiological consequences.3 It is a fact that the toxic nature of oxygen has been a concern for more than 200 years and that too much oxygen in arterial blood, hyperoxia, is caused by medical professionals, especially nurses.4
According to a World Health Organization (WHO) estimate, at least 1.4 million deaths worldwide each year are related to either inappropriate oxygen administration or shortage of oxygen treatment.5 The administration of oxygen should be based on the patient’s needs. In clinical practice, both indiscriminate use of supplemental oxygen and limited knowledge of hyperoxia have been observed.6 Nurses must be aware that, like that of too little oxygen, too much oxygen can cause hyperoxia, and a lot of complications including long-term disability and death.7 For instance, excessive oxygen dose in premature infants increases the risk of retinopathy of prematurity (ROP) and bronchopulmonary dysplasia (BPD) and lengthens hospitalization.8
Pulse oximetry is the most commonly used noninvasive tool to assess oxygen saturation in neonates and both theoretical and practical knowledge of pulse oximetry are needed during assessment of oxygenation in pediatric patients even though the accurate saturation depend on the correct placement of the probe.9,10
The flow rate, dose, and method of monitoring should be given special attention to ensure safe and effective oxygen delivery, and nurses should be concerned with the effects and possible hazards of oxygen.11 Proper administration of SOT is not only about the dose of oxygen but also humidification of oxygen. Humidification is required by the airway to maintain proper ciliary function, prevent squamous epithelial changes, prevent dehydration and thickening of secretions, minimize atelectasis and tracheitis, and prevent heat loss.12,13 Moreover, inadequate humidification may contribute to staphylococcal sepsis due to drying and cracking of the mucosa.14
Despite the existence of updated guidelines on supplemental oxygen therapy, compliance with best SOT practices remains poor8. In Ethiopia, about 35.5% of infants had ROP, 22.6% had vision-threatening diseases, 33.3% required treatment, and 12.9% were blind primarily due to Hyperoxia. The primary cause of hyperoxemia is inappropriate practice of oxygen by healthcare workers and oxygen saturation levels of more than 95% in newborns are potentially harmful.15
Factors that influence inappropriate administration of oxygen for neonates were nurses’ lack of adequate knowledge regarding the use of O2 delivery equipment and lack of training in practical aspects.16 The level of knowledge of nurses regarding oxygen administration has been assessed in certain studies, and their knowledge scores were shown to be low.3,5,13,16 It is expected that assessing nurses’ level of knowledge of oxygen therapy would aid in determining the requirement for appropriate in-service training and developing the substance of in-service training to be delivered, thus addressing practical weaknesses.17 Although this problem is huge, no study on supplemental oxygen therapy for newborns has been conducted in Ethiopia.
Therefore, this study aimed to assess the knowledge, practices, and associated factors of SOT among nurses working in NICUs in public hospitals in Addis Ababa, Ethiopia.
Materials and Methods
Study Design Area and Period
This institutional-based cross-sectional study was conducted in public hospitals in Addis Ababa, Ethiopia, from February 8, 2022, to April 6, 2022. Addis Ababa, the capital city of Ethiopia, is the largest city in the country. There were 42 hospitals in the city (14 public, 28 non-governmental organizations (NGO), and private). The current metro area population of Addis Ababa in 2022 is 5,227,794, up a 4.44% increase from 2021.18
Population and Eligibility Criteria
All nurses working in the NICUs of public hospitals in Addis Ababa, Ethiopia, were used as the source population. All nurses working in the NICUs of the selected public hospitals in Addis Ababa were included, whereas nurses on annual, sick, or maternal leave during data collection were excluded from this study.
Sample Size Determination and Sampling Procedure
In Addis Ababa, there are 10 public hospitals with NICUs, and five of them (Tikur-Anbessa Specialized Hospital (TASH), St. Paulo’s Hospital, Gandhi Hospital, St. Peter’s Specialized Hospital, and Zewditu Hospital) were randomly selected using the lottery method with 171 nurses working in the NICU. Sample size was determined by using a single population proportion formula and with the following assumptions: Z = standard normal distribution value at 95% confidence level of Zα/2 = 1.96, and margin of error (d) = 5%: which is the degree of accuracy set at 0.05 is the standard allowed deviation from the true proportion.
Because the sampling frame was less than 10,000, a correction formula was used, and the final sample size was determined using the correction formula: NF = n/n+1/N=131.
Finally, a complete census was used to include all nurses working in the NICUs of selected public hospitals in Addis Ababa, as the calculated sample size was nearly equal to the number of nurses in the selected hospitals.
Data Collection Tool and Procedure
The respondents’ knowledge and practice of SOT were assessed using structured self-administered questionnaires. The questionnaire was divided into four sections: part-I sociodemographic characteristics of nurses (05 questions), part II respondents’ knowledge of the SOT (10 questions), part-III practice-related questions about the SOT (14 questions), and part-IV organization-related questions (11 questions).
Knowledge testing questions were adopted from previous literature.2,3,5,19 An item of questions was chosen, and each question had a score of one point when the answer was correct and zero when the answer was incorrect. Nurses’ total knowledge score was 10 points and classified as the following: “poor knowledge” when the totals score < mean value and “good knowledge” when the total score > mean value.
The questionnaire for the practice item was a yes-or-no question, which was adopted from the literature from a previous study.20 The total score ranged from 0 to 14. The scoring system for nurses’ practice questions had a score of one point for the answer “Yes”, and zero for “No”. Then, the total score of the practice of nurses was categorized as a score of ≥ mean value considered as good practice and a score < mean value considered poor practice.
The organizational factor-related item also had yes or no questions. The study data were collected through a structured self-administered questionnaire on nurses’ knowledge and practice at the NICU regarding supplemental oxygen therapy. For this study, one supervisor and five trained BSc nurses were data collectors, and pretests were conducted on 5% of the total respondents to maintain data quality.
Data Processing and Analysis
The collected data were coded and entered into Epi-data version 4.6 and exported to SPSS version 26 for cleaning, editing, and analysis. Tables, pie charts, bar graphs, and text were used to present the data. After bivariate logistic regression analysis, variables with a p-value <0.25 were included in the multivariable logistic regression analysis. On multivariable analysis, an odds ratio with a 95% CI and a p-value <0.05 was used to determine the statistical association between the outcome variable and independent variables.
Results
Socio-Demographic Characteristics of Nurses
Out Of 173 nurses involved in this study, about 166 nurses were willing to participate with a response rate of 96%. Among them, 134 (80.7%) were females and 47% were married. The mean and standard deviation age of the nurses was 28.93± 2.819 years. In terms of the level of education, about 71 (42.8%) of nurses were general BSc nurses and 67 (40.4%) were BSc in neonatal nurses. Regarding, experience. More than half of the study participants, 93 (56%) had work experience of 6–10 years in nursing profession (Table 1).
 |
Table 1 Distribution of Socio-Demographic Characteristics of Nurses at Public Hospitals of Addis Ababa, 2022 (n=166) |
The Overall Knowledge of Participants in SOT
The mean and standard deviation score of knowledge questioners answered correctly by study participants was 7.88 ±1.75. Nurses who scored more than or equal to the mean value were 101 (60.8%), whereas nurses who scored less than the mean value were 65 (39.2%) (Figure 1).
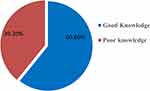 |
Figure 1 Shows the overall knowledge Level of supplemental of oxygen therapy among nurses working in NICU of public hospitals of Addis Ababa, Ethiopia. |
The Overall Practice of Participants in SOT
The mean score of practice questioners answered correctly by the study participants 9.59 ±1.45. Nurses who scored more than or equal to the mean value whereas 90 (54.2%), whereas nurses who scored less than the mean value were 76 (45.8%) (Figure 2).
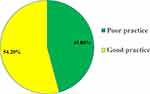 |
Figure 2 Shows the overall practice level of supplemental of oxygen therapy among nurses working in NICU of public hospitals of Addis Ababa, Ethiopia. |
Possible Organizational Factors of Nurses’ Knowledge and Practice Regarding Supplemental Oxygen Therapy
More than two-thirds of the participants, 122 (73.5%) said that workload impacted supplemental oxygen therapy, and about 75% of respondents believed that nurse-to-patient ratios of >1:2 were a burden. Approximately 45 (27.1%) nurses did not receive SOT training and the majority of nurses, 163 (98%) replied that a pulse oximeter was not available for each neonate during SOT (Table 2).
 |
Table 2 Organizational Factors Associated with Knowledge and Practice Towards SOT Among Nurses Working at NICU of Public Hospitals in Addis Ababa, Ethiopia, May 2022 (n=166) |
Factors Associated with Nurses’ Knowledge Regarding Supplemental Oxygen Therapy
In bivariate logistic regression analysis, variables associated (p < 0.25) with nurses’ knowledge of SOT were marital status, work experience, and reference guidelines before oxygen administration. In the multivariate logistic regression analysis, only work experience was significantly associated with SOT knowledge level (p < 0.05). Nurses with work experience of 6–10 years were five times more knowledgeable than those with work experience of < 5 years ([AOR: 5.40; 95% CI: 2.128–13.738), and nurses with work experience of >10 years were 14 times more knowledgeable about SOT than those with work experience < 5 years. (AOR: 14.42; 95% CI: 2.91–71.45) (Table 3).
 |
Table 3 Bivariate and Multivariate Analysis of Factors Associated with Nurses’ Knowledge towards SOT in the NICU of Public Hospitals, Addis Ababa, Ethiopia, 2022 (n=166) |
Factors Associated with the Practice of Nurses Towards Supplemental Oxygen Therapy
In the bivariate logistic regression analysis, the variables associated (p-value < 0.25) with nurses’ practice of nurses towards SOT were work experience, training on SOT, marital status, use of guidelines on SOT, knowledge of SOT, and educational level. Among these, only three variables (level of knowledge of SOT, educational level, and work experience) were significantly associated with nurses’ practice of nurses towards SOT (p ≤ 0.05).
Theoretically knowledgeable nurses were almost three times more likely to practice SOT than their counterparts (AOR=2.92, 95% CI: 1.24–6.86). Nurses who had MSc in neonatal nursing were 6.5 times more likely to practice SOT as compared to those who had BSc in neonatal nursing (AOR=6.51, 95% CI: (1.34–31.55)].
Regarding work experience, nurses with work experience of 6–10 years were four times more likely to practice SOT as compared to those who had < 5 years of work experience (AOR = 3.69, 95% CI: (1.30–10.44). Similarly, nurses with work experience of >10 years were approximately seven times more likely to practice towards SOT as compared to those who had <5 years of work experience (AOR=6.88, 95% CI: (1.34–35.35)) (Table 4).
 |
Table 4 Bivariate and Multivariate Analysis of Factors Associated with Nurses’ Practice Towards SOT in the NICU of Public Hospitals, Addis Ababa, Ethiopia, 2022 (n=166) |
Discussion
In this study, 60.8% of nurses had good knowledge of supplemental oxygen therapy. This result indicates that approximately 40% of nurses who are working in NICUs of public hospitals in Addis Ababa had a significant knowledge gap regarding SOT. This is alarming and shows a large gap in the knowledge of supplemental oxygen therapy, which requires urgent action. This study is in line with another study conducted in Harari region, Ethiopia (61.4%).21 The proportion of knowledgeable users in this study was higher compared to a descriptive cross-sectional study conducted in Debre Tabor, Ethiopia (52%).22
However, proportion of knowledgeable users were a little bit lower than a study in Turkey (63.6%).3 Similarly, proportion of knowledgeable nurses was very low compared to a descriptive cross-sectional study conducted in Southwest Nigeria (81.2%).23 A possible difference might be that participants in the Turkish study were well-experienced, which might have increased their knowledge level. On the other hand, nurses’ knowledge level of nurses in this study regarding SOT was higher than a study conducted in Cairo, Egypt (26%).20
Regarding nurses with ≤ 5 years of work experience, those with 6–10 years and >10 years of work experience were 5 times and 14 times more likely to be knowledgeable about SOT, respectively. This finding is in line with those of studies done in Iran19 and Southwest Nigeria.23 A possible scientific explanation might be that more years of experience led to an increase in their need for improvement in their level of knowledge. However, work experience was not significantly associated with knowledge of oxygen therapy in a study conducted in the Harari region of Ethiopia.21
The current study revealed that only about 54.2% of the nurses had good practice of SOT. According to this study, nearly half (45.8%) of nurses had practice gap regarding SOT, even though improper administration of oxygen in this age-group was fatal. In this study, nurses with good practices were lower than the study conducted in Netherlands; approximately 58% nurses had good practice in Netherlands.19 A possible explanation for this difference might be the study period; the study in Netherlands was conducted in 2018, which is five years ago, when self-learning was not as simple as 2022/2023. However, the proportion of nurses with good practice in this study was higher than descriptive cross-sectional studies conducted in Nigeria,23 Debre Tabor, Ethiopia (33%)22 and Harari region, Ethiopia21
Using multivariate logistic regression, this study found that nurses’ SOT practices were significantly associated with their educational status, work experience, and level of knowledge. Nurses with an MSc in neonatal nursing were 6.5 times more likely to practice SOT than those with a BSc in neonatal nursing. The scientific explanation for this association might be that the higher the level of education, the better is the performance of practice. This study is in line with another cross-sectional study conducted in Debre Tabor, Ethiopia.22
However, this result was contradicted by a study conducted in Iran and Saudi Arabia,24,25 which indicated that participants with nursing diplomas had higher levels of practice than BSc nursing participants. A possible reason might be the effect of the educational curriculum in these countries on the practice of nursing; diploma nurses are expected to perform skill activities more frequently than knowledge.
Regarding work experience, nurses with 6–10 and >10 years of work experience were 4 and 7 times more likely to practice SOT than those with <5 years of work experience. This finding is supported by a study conducted in 318 European intensive care units that found that the length of years in ICU practice increases nurses’ practice.26
Furthermore, this study revealed that knowledgeable nurses were three times more likely to practice SOT than those with poor knowledge. Even though whether knowledge or practice comes first is controversial, it is scientifically accepted that knowledge is the basis for practice.
This study was supported by a descriptive cross-sectional study conducted in Ethiopia in 2021.14 Though, the authors were tried their best, the limitations of this study were the presence of limited previous research for discussions and comparison; it was conducted at public hospitals only; and missed some important variables like child ownership.
Conclusions
This study found that approximately 40% and 46% of nurses had poor knowledge and practice regarding SOT, respectively. On this study, educational status and level of knowledge were found associated with practice of SOT and work experience was found associated with both knowledge and practice of SOT. Therefore, in-service training and workshops should be prepared to increase their experience and opportunities to escalate nurses’ level of education must be given for better knowledge and practice of SOT among nurses working in NICU.
Abbreviations
NICU, Neonatal intensive care unit; SOT, Supplemental oxygen therapy; SPSS, Statistical Package for the Social Sciences; ROP, Retinopathy of Prematurity.
Data Sharing Statement
The dataset used and/or analyzed during the current study is available upon reasonable request from the corresponding author.
Ethics Approval and Informed Consent
This study was conducted in accordance with the principles of the Declaration of Helsinki. Ethical clearance was obtained from the Institutional Review Board (IRB) of Addis Ababa University, College of Health Sciences, School of Nursing and Midwifery (protocol number-023/22/SNM). This letter of ethical clearance was sent to each hospital’s administrative office and official permission was obtained. The study objectives and procedures were disclosed to participants. Thereafter, all study participants were asked to sign an informed written consent form, and all information gathered from each participant was kept confidential.
Consent for Publication
Not applicable in this study
Acknowledgments
We are grateful to Addis Ababa University, College of Health Sciences, for providing financial support for data collection. We are thankful to the staff of Tikur-Anbessa Specialized Hospital, St. Paulo’s Hospital, Gandhi Hospital, St. Peter’s Specialized Hospital, and Zewditu Hospital. The authors are grateful to their supervisor and data collectors.
Author Contributions
All authors made a significant contribution to the work reported, in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by Addis Ababa University, Ethiopia, for data collection. The funder had no role in the study design, data collection, and analysis, interpretation of data, decision to publish, or preparation of the manuscript.
Disclosure
All authors declared that they have no conflicts of interest in this work.
References
1. Rousseau A, Sjo¨ Berg F. The time of uncritical oxygen treatment is over. La¨kartidningen. 2006;103:1100–1104.
2. Taş Arslan F, Özkan S, Ak B, Karayağız Muslu G. Neonatal intensive care nurses’ opinion on oxygen therapy: a survey conducted in Turkey. J Contemp Med. 2017;4:184. doi:10.16899/gopctd.326667
3. Demirel H, Kazan EE. Knowledge levels of nurses about oxygen therapy in Turkey. Internat J Health Serv Res Pol. 2020;5(1):1–14. doi:10.33457/ijhsrp.700150
4. Sola A, Golombek SG, Montes Bueno MT, et al. Safe oxygen saturation targeting and monitoring in preterm infants: can we avoid hypoxia and hyperoxia? Acta Paediatr. 2014;103:1009–1018. doi:10.1111/apa.12692
5. Ayuk AC, Nwosu NI. Oxygen delivery systems and training needs in pediatric and adult settings- A call to action beyond the COVID-19 era. JPATS. 2021;2:119–121. doi:10.25259/JPATS_13_2021
6. Sola A, Saldeño YP, Favareto V. Clinical practices in neonatal oxygenation: where have we failed? What can we do? J Perinatol. 2008;28(Suppl 1):S28–34. doi:10.1038/jp.2008.47
7. Bancalari E, Claure N. Control of oxygenation during mechanical ventilation in the premature infant. Clin Perinatol. 2012;39:563–572. doi:10.1016/j.clp.2012.06.013
8. Parmar J, Pawar V, Warathe A, et al. Rationalizing oxygen usage in a level II special newborn care unit in Madhya Pradesh, India. BMJ Open Qual. 2021;10(Suppl 1):e001386. doi:10.1136/bmjoq-2021-001386
9. Bilan N, Behbahan AG, Abdinia B, et al. Validity of pulse oximetry in detection of hypoxaemia in children: comparison of ear, thumb and toe probe placements. Eastern Mediterr Health J. 2010;16:218–222. doi:10.26719/2010.16.2.218
10. Popovich DM, Richiuso N, Danek G. Pediatric health care providers’ knowledge of pulse oximetry. Pediatr Nurs. 2004;30:14–20.
11. Goharani R, Miri M, Kouchek M, Sistanizad M. Familiarity of physicians and nurses with different aspects of oxygen therapy; a brief report. Emerg. 2017;5(1):e39.
12. Loftus BC, Ahn J, Haddad J. Neonatal nasal deformities secondary to nasal continuous positive airway pressure. Laryngoscope. 1994;104(8 Pt 1):1019–1022. doi:10.1288/00005537-199408000-00018
13. Robertson NJ, McCarthy LS, Hamilton PA, Moss AL. Nasal deformities resulting from flow driver continuous positive airway pressure. Arch Dis Child Fetal Neonatal Ed. 1996;75(3):F209 F212. doi:10.1136/fn.75.3.F209
14. Kopelman AE, Holbert D. Use of oxygen cannulas in extremely low birthweight infants is associated with mucosal trauma and bleeding, and possibly with coagulase-negative staphylococcal sepsis. J Perinatol. 2003;23(2):94–97. doi:10.1038/sj.jp.7210865
15. Lema G, Tsadik AW, Beza L. Knowledge, attitude and practice study of oxygen therapy among emergency department nurses in Addis Ababa, Ethiopia. Prehosp Disaster Med. 2017;32(S1):S149. doi:10.1017/S1049023X17004113
16. Omer IM, Ibrahim NG, Nasr AMA. Oxygen therapy in neonatal intensive care units in Khartoum State. Sudan J Pediatric. 2015;15(2):49–54.
17. Melesse MA. Retinopathy of prematurity - an emerging cause of childhood blindness in Ethiopia. Ethiopian Med J. 2020;58:02.
18. Addis Ababa, Ethiopia metro area population 1950–2021. Addis Ababa, Ethiopia Metro Area Population 1950–2023. Available from: https://www.macrotrends.net/cities/20921/addis-ababa/population.
19. Huizing MJ, Villamor-Martínez E, Meus S, de Jonge FM, Villamor E. Dutch neonatal intensive care nurses’ perceptions of pulse oximeter saturation target limits for preterm infants. J Pediatric Nurse. 2019;1(49):e36–41. doi:10.1016/j.pedn.2019.08.005
20. Mayhob M. Nurses’ knowledge, practices and barriers affecting a safe administration of oxygen therapy. J Nurs Health Sci. 2018;7(3):42–51.
21. Jamie AH. Knowledge and practice of nurses towards oxygen therapy in the public hospitals of Harari region, Ethiopia. J Res Develop Nurs Midwif. 2021;2021:1.
22. Zeleke S, Kefale D. Nurses’ supplemental oxygen therapy knowledge and practice in Debre Tabor general hospital: a cross-sectional study. Open Access Emerg Med. 2021;13:51–56. doi:10.2147/OAEM.S299139
23. Adeniyi BO, Akinwalere OO, Ekwughe FC, et al. Assessment of knowledge and practice of oxygen therapy among doctors and nurses: a survey from Ondo State, Southwest Nigeria. J Pan Af Thoracic Soc. 2021;2:161–166. doi:10.25259/JPATS_4_2021
24. Mohammed QN, Alsawaf BF. Assessment of nursing staff’s knowledge and practice regarding care of premature babies in Mosul teaching hospitals. Mosul J Nurs. 2016;4(2):70–73.
25. Elsayed L, Elsayed L. Nursing care provided for neonates with respiratory distress syndrome in the neonatal intensive care units at Makkah Al-Mukarramah in Saudi Arabia. Life Sci J. 2013;10(1):3403.
26. Fulbrook P, Albarran J, Baktoft B, Sidebottom B. A survey of European intensive care nurses’ knowledge levels. Internat J Nurs Stud. 2011;49:191–200. doi:10.1016/j.ijnurstu.2011.06.001
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

