Back to Journals » Integrated Pharmacy Research and Practice » Volume 12
Knowledge, Perception, and Readiness of Indonesian Pharmacists for the Implementation of Telepharmacy-Based Pharmaceutical Services in Indonesia
Authors Wathoni N , Lestari K , Iftinan GN , Rahayu SA, Nurlatifah A, Khairinisa MA , Elamin KM
Received 6 September 2023
Accepted for publication 2 November 2023
Published 22 November 2023 Volume 2023:12 Pages 213—225
DOI https://doi.org/10.2147/IPRP.S434790
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Walid Al-Qerem
Nasrul Wathoni,1 Keri Lestari,2 Ghina Nadhifah Iftinan,2 Susi Afrianti Rahayu,3 Anggun Nurlatifah,2 Miski Aghnia Khairinisa,2 Khaled M Elamin4
1Department of Pharmaceutics and Pharmaceutical Technology, Faculty of Pharmacy, Universitas Padjadjaran, Sumedang, 45363, Indonesia; 2Department of Pharmacology and Clinical Pharmacy, Faculty of Pharmacy, Universitas Padjadjaran, Sumedang, 45363, Indonesia; 3Department of Pharmacy, Akademi Farmasi Bumi Siliwangi, Bandung, 40286, Indonesia; 4Graduate School of Pharmaceutical Sciences, Kumamoto University, Chuo-ku, Kumamoto, 862-0973, Japan
Correspondence: Nasrul Wathoni, Department of Pharmaceutics and Pharmaceutical Technology, Faculty of Pharmacy, Universitas Padjadjaran, Jl. Raya Bandung Sumedang KM 21, Jatinangor, 45363, Indonesia, Tel/Fax +622 842 888888 3510, Email [email protected]
Background: Telepharmacy, a digital technology-driven approach, has emerged as a potential solution to address the challenges posed by this pandemic. Telepharmacy is a method used in pharmaceutical practice where a pharmacist utilizes telecommunications technology to supervise aspects of pharmacy operations or provide patient care services. This study aimed to assess pharmacists’ level of knowledge, perception, and readiness toward telepharmacy in Indonesia.
Methods: A cross-sectional approach was used in this study, and non-probabilistic purposive sampling technique was used to select respondents who were Indonesian pharmacists. The Telepharmacy Knowledge, Perception, and Readiness questionnaire, translated into Indonesian and administered online, was used to measure the pharmacist’s knowledge, perception, and readiness level. Descriptive and inferential data analyses were performed using SPSS version 26, with a p-value of ≤ 0.05 considered statistically significant.
Results: A total of 378 responses were obtained, with 96.83% exhibiting high knowledge and 63.23% showing high readiness for telepharmacy services. Furthermore, 58.20% of respondents had a positive perception of telepharmacy services. The results indicate a significant influence of pharmacist’s knowledge and perception on their readiness to implement telepharmacy services in the future practice.
Conclusion: Most study participants had sufficient knowledge, positive perceptions, and readiness to implement telepharmacy services in their future pharmaceutical practice. However, they expressed concerns about the potential for an increased workload and the potential lack of incentives associated with the widespread adoption of telepharmacy practice models. Telepharmacy practice models must be included in the training programs that train future’s pharmacists in order to ensure that they have the abilities required to offer telepharmacy services.
Keywords: telepharmacy, pharmacists, knowledge, perception, readiness, Indonesia
Introduction
Corona Virus Disease 2019 (COVID-19), which emerged at the end of 2019, has caused extraordinary panic throughout the world with its rapid transmission and quite high death rate.1 In an effort to suppress the spread of the virus, the government must implement policies in the form of controlling social distance and quarantine.2 The implementation of this policy has an impact on changing the way society interacts. The frequency of physical interactions has decreased, while the use of technology to support daily needs has increased.3
With the global problems that have occurred, traditional ways of providing health services also need to be modified. With the digital revolution, a health service method called telemedicine is considered to be a solution in overcoming this global problem. Telemedicine is a modern way of providing health services to patients and the general public via communication tools such as telephones, smartphones, tablets, laptops, or other communication devices.4 Based on research in United Arab Emirates, 31.3% participants used telemedicine during the COVID-19 pandemic for seeking advice from pharmacist or physician.5 As a part of telemedicine, there are also methods of providing pharmaceutical care to patients using technology and telecommunications. This method is called telepharmacy.6 Telepharmacy is a method used in pharmaceutical practice where a pharmacist utilizes telecommunications technology to supervise aspects of pharmacy operations or provide patient care services.7 Telepharmacy operations and services may include, but are not limited to, medication review and monitoring, compounding and dispensing verification, medication therapy management, patient assessment, patient counseling, clinical consultation, outcome assessment, decision support, and medication information provision.8
Telepharmacy was soon recognized as a tool to address the multiple challenges of the pandemic while ensuring the quality of patient care.6 Telepharmacy has promising benefits in increasing access to pharmaceutical services for the community when distance is an obstacle. During the COVID-19 pandemic, many countries, including European countries, Canada, and the United States, have facilitated medical services via the Internet, such as virtual medical consultations, e-prescriptions, and home delivery of medications to promote social distancing among patients.9 However, telepharmacy is not free from challenges and problems that may arise from its use.10 Telepharmacy can only be implemented in the presence of a digital device and is supported by an adequate internet connection. Lack of access to digital devices and internet connections is considered an obstacle in implementing telepharmacy.11 In addition, it’s necessary to anticipate the digital skills and inability to use technology appropriately on elderly patients.12 Moreover, telepharmacy services increased concerns about patients’ privacy and data, as an electronic record can store individuals’ details more easily than documented paper. Therefore, protecting the privacy of patient data must be prioritized, and healthcare professionals, including pharmacists, must maintain its protection.13
In Indonesia itself, telepharmacy has been implemented, one of which is at the Harapan Kita Heart and Blood Vessel Hospital, Jakarta. Telepharmacy services are carried out by answering questions by chat application, sending barcodes to patients who will be connected to a drug education video link, making video calls with patients who are receiving narrow therapeutic index therapy or patients who request education, and sending drugs to their homes. Educational videos are short 1–2 minutes videos consisting of heart medication administration videos, how to use warfarin medication videos, how to use digoxin medication videos, insulin videos, and antibiotic medication videos.14
Evaluation of the implementation of telepharmacy is important due to the many challenges and problems that may arise from telepharmacy, such as lack of access to digital devices and internet connections, low digital literacy in society, and concerns about loss of privacy.15 One important element in implementing telepharmacy is the pharmacist as the provider of pharmaceutical services. The pharmacist’s readiness to provide telepharmacy services will be related to telepharmacy knowledge and perceptions regarding telepharmacy.16,17 Considering the background, we designed a nationwide study to explore pharmacists’ knowledge, perception, and readiness to carry out pharmaceutical services through telepharmacy in Indonesia.
Methods
Study Design
A descriptive observational study using a cross-sectional approach and non-probabilistic purposive sampling technique was conducted from March to May 2023 among Indonesian pharmacists to assess the correlation between knowledge, perceptions, and readiness for telepharmacy. Subjects that were involved in this study is pharmacists with Indonesian pharmacist registration certificates who perform pharmaceutical services and eligible for the inclusion that include have internet access, and willing to participate in this study. The exclusion criteria for this study are pharmacist who do not conduct pharmaceutical services such as pharmacist who work in industrial section and not willing to filling out the questionnaire. Before collecting the data, subjects were received informed consent through an online form that also explained the purpose of the study. After reading the research information, research subjects will be asked to fill out an agreement to participate in the research. After filling out the consent, the research subjects can fill out the questionnaire until completion. Any research subject who experiences difficulties can contact the researcher via the contact number provided on the research information sheet during the process of filling out this digital questionnaire. The subjects’ involvement was voluntary, and no monetary incentive.
An online survey was used to obtain data from the participants, and it was based on a validated questionnaire used by Elnaem (2022).16 The questionnaire used in this study comprised 35 questions related to Indonesian pharmacists’ knowledge, perception, and readiness. The questionnaire was available in English. In this study, the questionnaire was translated into Indonesian using forward – back translation method by 3 experts in the field of pharmacy with bilingual ability. The language translation process was carried out to maintain the instrument’s validity, and the meaning of each item can be understood the same as the original language.
The questionnaire was created using Google Forms as an online form. Respondent demographics, employment statistics, workplace, pharmacist knowledge, attitudes, and readiness profile of telepharmacy were collected. The online survey was sent to the respondent’s email or WhatsApp messages. After the respondent sent their responses, we checked the form to ensure it was completed.
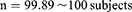
Validity and Reliability Test
Validity testing using the Pearson Product Moment correlation technique was carried out before the research, to ensure that the variable measurement instrument met the requirements and produced accurate result data. The validity test was carried out with a number of respondents of 5–10 times the number of variables, namely 30 pharmacist respondents. The results of validity testing on each knowledge domain question item show that all question items are said to be valid because they have a correlation value (rcount) >0.361 (rtable). The results of testing the validity of all the questions in this questionnaire show that the correlation value (rcount) is >0.361 (rtable) so that the questionnaire is said to be valid for use in the data collection process (Table 1).
 |
Table 1 Validity Test |
Reliability testing was also carried out by calculating Cronbach’s alpha for each variable measured. With an alpha coefficient value for reliability measurement >0.600, the questionnaire can be said to be reliable.18 Because all Cronbach’s Alpha values are >0.600, the questionnaire is said to be reliable or reliable for use in the data collection process (Table 2).
 |
Table 2 Reliability Test |
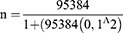
Sample Size Calculation
The population is the total of research subjects. In this study the population was pharmacists in Indonesia. According to 2021 data, the number of pharmacists in Indonesia who have a Pharmacist Registration Certificate (STRA) is recorded at 95,384 people.19 A sample is a part of a population that is considered to represent the entire total population. In this study, a sample of pharmacists in Indonesia met the inclusion criteria. The sample size was calculated using the Slovin formula.20 The total population was 95,384 people, the margin of error was 10% and the response percentage to the questionnaire was presumed to be 50%.
After final calculations, our study’s recommended minimum sample size was 100 respondents.
Statistical Analysis
Data were analyzed using SPSS software version 26. The data were gathered using an Excel spreadsheet, and the descriptive results were presented as numbers and percentages. The total score of each section was used to categorize responses into low ≤ 40%, moderate 41%-74%, and high ≥ 75%.16 The correlation test between demographic characteristics and the level of knowledge, perception, and pharmacist readiness for telepharmacy was carried out using the Kendall Tau c statistical test by looking at the p significance level. While the correlation test between the level of knowledge and perception with the level of readiness of pharmacists for telepharmacy was carried out using the Kendall Tau b statistical test by looking at the p significance level. The significance level was set at p<0.05.
These two statistical methods were chosen because they are appropriate statistical methods for the type of data in this research. The requirements for the Eta and Kendall Tau tests are for types of data with non-parametric data scales (at least ordinal) and do not require initial testing such as normality and homogeneity tests.21
Results
Demographic Information
This study received 378 responses to the questionnaire, exceeding the minimum sample required (Table 3). Respondents in this study were all pharmacists or had completed the pharmacist professional study program. Most pharmacists were female (79.89%), aged 26–30 (36.24%). The workplace of all pharmacists was spread across 30 provinces. The three provinces with the largest distribution of pharmacists were West Java (34.66%), East Java (11.11%), and Central Java (8.99%). Based on the highest education, the respondents who participated in this study were dominated by pharmacists, with 349 respondents (92.33%).
 |
Table 3 Characteristics of Pharmacist Respondents and Results of Correlation Analysis |
The results of the correlation test showed that there was a significant association between gender and telepharmacy knowledge (p-value <0.005). Meanwhile, there is no significant association between perception variables and readiness to carry out pharmaceutical services through telepharmacy (p-value > 0.05).
Based on age, the respondents in this study were dominated by respondents in the 26–30 age category, namely 137 respondents (36.24%). The correlation test results showed no significant association between the age variable and the variables of knowledge, perception, and readiness to carry out pharmaceutical services through telepharmacy (p-value > 0.05).
Based on the highest education, the respondents who took part in this study were dominated by the category with the highest educational pharmacist, namely 349 respondents (92.33%). The correlation test results showed no significant association between education, knowledge, perception, and readiness to provide pharmaceutical services through telepharmacy (p-value > 0.05).
Respondents with the category of practicing in community pharmacies dominated the total respondents, namely 229 (60.58%). Respondents with the category of practicing in hospitals were 60 respondents (15.87%), then respondents with the category of practicing in both clinics and health centers were 89 people (23.55%) respectively. The correlation test results showed no significant association between the place of work practice and knowledge, perception, and readiness to carry out pharmaceutical services through telepharmacy (p-value > 0.05).
Respondents who took part in this study were spread across 30 provinces in Indonesia. This research did not cover all provinces in Indonesia, but overall, almost all regions in Indonesia are represented in this study. The three provinces with the largest distribution of respondents were West Java (131 respondents; 34.66%), East Java (42 respondents; 11.11%), and Central Java (34 respondents; 8.99%). The results of the correlation test showed that there was no significant association between the area of practical work and the variables of knowledge, perception, and readiness to carry out pharmaceutical services through telepharmacy (p-value > 0.05).
Level of Knowledge, Perception, and Readiness of Indonesian Pharmacists for Telepharmacy
In this study, out of 378 pharmacists, most pharmacists (92.33%) were classified as having a high level of telepharmacy knowledge, with an average knowledge score of 25.23 ± 2.27. Most pharmacists (58.20%) are also classified as having a positive perception of telepharmacy, with an average perception score of 49.95 ± 6.74. Likewise, with the level of readiness of pharmacists for telepharmacy, it was found that the majority of pharmacists (63.23%) were classified as having a high level of readiness with an average score of 46.58 ± 8.74 (Table 4).
 |
Table 4 Average Score of Indonesian Pharmacists’ Knowledge, Perception and Readiness for Telepharmacy (n=378) |
Pharmacists’ Knowledge of Telepharmacy
In the pharmacist’s knowledge of telepharmacy, statement number 2 “Knowledge of information and communication technology is important for pharmacists on how to perform telepharmacy”, showed the highest score (98.15%). Almost all respondents had a high level of knowledge, namely 264 respondents (97.78%), only 6 respondents (2.22%) had a moderate level of knowledge, and no respondents had a low level of knowledge (Table 5).
 |
Table 5 Distribution of Answers to Statements Regarding Knowledge for Telepharmacy (n=378) |
Pharmacists’ Perception of Telepharmacy
The question with the highest cumulative percentage of agreed and strongly agreed answers was found in statement 10 (51.32%), “Do you think pharmacy schools should provide educational programs on computers, IT, and telepharmacy to to assist in future utilization of telepharmacy”? Question number 2, “Do you agree that telepharmacy will have a higher error rate for drug dispensing and filling, compared to traditional pharmacies”? Is a negative question with the most varying percentage of answers. About 42 respondents (11.11%) answered strongly agree, 64 respondents answered agree (16.93%), 83 respondents answered agree (21.92), 79 respondents answered strongly disagree (20.90%), and 110 respondents answered neutral (29.10%). This shows that there are quite a number of pharmacists who have a negative perception of the level of errors in dispensing and filling telepharmacy medicine.
Based on the results of the overall pharmacist perception score regarding telepharmacy shown in Table 6, most pharmacists had a positive perception, namely 220 respondents (58.20%), 157 respondents (41.53%) had a neutral perception, and only 1 respondent (0, 26%) who had a negative perception.
 |
Table 6 Distribution of Answers to Statements Regarding Perceptions of Telepharmacy (n=378) |
Pharmacist Readiness of Telepharmacy
Table 7 shows the distribution of respondents’ answers on the dimensions of pharmacist readiness to carry out pharmaceutical services through telepharmacy. Statement 5 “I am ready to undergo ethics and legal training related to telepharmacy”, has the highest cumulative percentage of agree and strongly agree answers (81.75%). This shows that most pharmacists are ready to participate in ethical and legal training programs in telepharmacy. The statement with the lowest cumulative percentage of agreed and strongly agreed answers was statement 1 (44.44%), “I am ready to work on a telepharmacy project, even without incentives”. Many respondents expressed concern about the lack of incentives for implementing telepharmacy services because most respondents did not agree to work on telepharmacy projects without incentives.
 |
Table 7 Answer Distribution to Statements Regarding Readiness for Telepharmacy (n=378) |
In general, the responses to the readiness domain questions were primarily characterized by agree and highly agree responses. This finding is further illustrated in Table 7, which indicates that a significant proportion of participants, specifically 239 individuals (accounting for 63.23% of the total sample), exhibit a high degree of preparedness. A total of 133 participants, accounting for 35.19% of the sample, exhibited a moderate level of readiness, while a mere 6 individuals, representing 1.59% of the sample, demonstrated low readiness.
The Correlation Between Knowledge and Perceptions of the Readiness of Indonesian Pharmacists in Facing Telepharmacy
The results of the correlation analysis using the Kendall Tau b statistical test showed a statistically significant association (p-value = 0.137) in the association between the level of knowledge and the level of readiness of Indonesian pharmacists to face telepharmacy (Table 8). It can be concluded that there is a significant correlation between the level of knowledge and the readiness to carry out pharmaceutical services through telepharmacy. Whereas the results of the correlation analysis between perception and the level of readiness of Indonesian pharmacists to face telepharmacy showed a statistically significant (p-value = 0.000) and strong (ι = 0.503) correlation (Table 9).
 |
Table 8 Correlation Test Results of the Value of Knowledge with the Readiness of Indonesian Pharmacists to Face Telepharmacy (n=378) |
 |
Table 9 Correlation Test Results of Perception Value with the Readiness of Indonesian Pharmacists to Face Telepharmacy (n=378) |
Discussion
This research evaluated pharmacists in Indonesia regarding their knowledge, perception, and readiness to implement pharmaceutical services through telepharmacy. Out of 278 pharmacists in Indonesia who were involved in this study, most respondents were female (79.89%), and there was a significant correlation between gender and telepharmacy knowledge. Similar results were also shown by research conducted in Saudi Arabia,22 where there was a significant association between gender and knowledge of telepharmacy services. This could be due to differences in technological experience between men and women. Women tend to use technology more frequently, and therefore women may have more knowledge about newly introduced services.23 But in contrast, the result from Ethiopia reported that being male was also found to be significantly with knowledge of telepharmacy in population of pharmacy students.24
Based on age, the respondents were dominated by the 26–30 years age category (36.24%), and there was no significant correlation between age and the variables of knowledge, perception, and readiness to carry out pharmaceutical services through telepharmacy. Similar results were shown by research conducted in Saudi Arabia, where the age variable did not show a significant association with the variables of knowledge, perception, and readiness for telepharmacy services.22 This can be caused by the fact that in digital era, as it is today, information and communication technology can be accessed by all levels of society and even all age categories.25 But based on research in Ethiopia, the study shows that pharmacy students in older age groups were 65% less likely to have sufficient knowledge of telepharmacy compared with students in younger groups. This was explained because most university students in the Ethiopian were under the age of 25, and younger students were more active in using information and communication technology.24
Pharmacists also dominated the respondents who participated in this study as their highest education. No significant association was shown between education and knowledge, perception, and readiness to provide pharmaceutical services through telepharmacy. These results contrast with previous studies related to telemedicine in Egypt, which found that a higher level of education is associated with better knowledge and attitudes towards telemedicine.26 This was explained because the research conducted in Egypt was aimed at the general population, whereas this research was aimed at pharmacists who had not much different levels of education and had been exposed to knowledge about telepharmacy.
For the practice area category, respondents who work in community pharmacies dominate (60.58%). And there is also no significant association between the place of work and knowledge, perception, and readiness to carry out pharmaceutical services through telepharmacy. Previous research on telemedicine in Egypt found that jobs with higher working hours affect knowledge and attitudes towards telemedicine.26 This study’s results could be because all work practices in hospitals, pharmacies, clinics, and health centers have the same workload. But the study in Saudi Arabia presented that community pharmacists had more positive attitudes toward telepharmacy because of the small number of pharmacy in rural areas, and most of community pharmacists believe that telepharmacy helps reduce pharmacist shortages and help delivery for patients living in rural areas or locations where access to healthcare is difficult.27
Respondents who took part in this study were spread across 30 provinces in Indonesia. This research cannot cover all provinces in Indonesia, but overall, almost all regions in Indonesia are represented in this study. The correlation test results showed no significant association between the area of practical work and the variables of knowledge, perception, and readiness to carry out pharmaceutical services. In today’s digital era, information and communication technology can be accessed from various regions of Indonesia. Although there may be regions where technological development is slower than other regions, information and communication technology can generally be accessed throughout Indonesia.28 With the accessibility of information and communication technology, it means that telepharmacy can also be accessed in all regions in Indonesia.29 Therefore, it can be concluded that there is no significant association between the area of residence and the knowledge, perception, and readiness of telepharmacy services due to telepharmacy access, which is accessible in various regions in Indonesia.
In this study, out of 378 respondents, the majority of respondents (96.83%) were classified as having a high level of telepharmacy knowledge and also classified as having a positive perception of telepharmacy (58.20%). Likewise with respondents’ readiness level to carry out pharmaceutical services through telepharmacy, it was found that the majority of pharmacists (62.23%) were classified as having a high level of readiness. A similar study previously conducted in Malaysia on pharmacy students showed that 67% of respondents had a high level of knowledge regarding telepharmacy, 61% of respondents had positive perceptions regarding telepharmacy, and 68% showed high readiness for telepharmacy.16 Meanwhile, a study in Pakistan showed that 59.7% of pharmacists had a negative perception of the benefits of implementing telepharmacy, 67.9% of pharmacists had a positive perception of the feasibility of telepharmacy, 71.3% of pharmacists had a positive perception of regulatory issues, and as many as 82.1% had a positive perception of telepharmacy during a pandemic.17
The association between knowledge and readiness to carry out pharmaceutical services through telepharmacy showed a very weak association and it can be concluded that there is a significant association between the level of telepharmacy knowledge and the readiness to carry out pharmaceutical services through telepharmacy. In a previous study by Elnaem et al, a significant association was found between knowledge items and telepharmacy readiness. The results of this study state that telepharmacy knowledge points regarding its role in the COVID-19 pandemic affect readiness and implementation to teach patients to use drug preparations in health facilities, carry out Home Medication Reviews (HMR), reduce the risk of medication errors among patients, increase workload, improve the use mobile applications and the Internet to take patient orders and transfer prescriptions.30
The association between perceptions and the readiness of pharmacists to carry out pharmaceutical services through telepharmacy showed a strong association, so it can be concluded that there is a significant association between perceptions and readiness to carry out pharmaceutical services through telepharmacy. In previous studies in Pakistan, the readiness to implement telepharmacy was linked to pharmacists’ perceptions of the benefits, feasibility, regulatory issues, legal frameworks, and the role of telepharmacy during a pandemic. This significant research has provided important insights into pharmacists’ readiness and perceptions of telepharmacy, which is currently an area of under-regard in Pakistan.17 In another study conducted in Vietnam, it was found that there was a significant association between readiness to carry out telepharmacy services and attitudes towards telepharmacy. The attitude points in this study also include perception points.31 Previous research also mention that having access to electronic devices is the most critical factor in having a positive perception and readiness of the Telemedicine system.32 This was reasonable since pharmacists with a positive perception would also have a higher level of readiness to apply telepharmacy in pharmacy practice.17
Indonesian pharmacists generally demonstrate the right knowledge, perception, and readiness for telepharmacy services in Indonesia. Participants recognized the urgency and benefits of telepharmacy during COVID-19 and understood the importance of information communication and technology (ICT) knowledge for pharmacists in performing telepharmacy and the need for a standardized education program in information communication technology knowledge. This is supported by previous research, in which over 50% of healthcare providers agreed that ICT skills determine attitudes towards telepharmacy.33 A study performed in Italy revealed the importance of ICT knowledge for pharmacy students to develop essential skills for future professional practice.34
In addition, this study also shows that most pharmacists have a positive perception of the benefits of telepharmacy in terms of cost efficiency and time for patients to reach health facilities. Telepharmacy can save time and travel costs, a major barrier for the elderly in rural areas and patients with physical limitations.35 Access to rural areas for medicines and information through telepharmacy will help remove important barriers such as time and travel costs, increasing patient satisfaction and trust in telepharmacy services.36 However, many negative perceptions remain regarding the error level in dispensing and filling telepharmacy drugs. Influenced by the relatively recent implementation of telepharmacy in Indonesia, some participants agreed that telepharmacy may be associated with an increased incidence of medication errors. Previous studies have shown that prior exposure is very important for pharmacists to know whether telepharmacy will be associated with higher error rates or not.37 As emphasized earlier, telepharmacy can help reduce medication error rates. In many hospitals, the application of telepharmacy has led to a reduction in medication error rates.38
Another obstacle to introducing telepharmacy is that most respondents disagreed with working on telepharmacy projects without incentives and expressed concern about the lack of incentives to perform telepharmacy services. An Iranian study conducted to explore pharmacists’ views on telepharmacy found that incentives pose a major barrier to the telepharmacy practice models.39 In the future, to better prepare future pharmacists to offer telepharmacy services, pharmacy colleges should incorporate telepharmacy practice models into their curricula. Additionally, through giving lectures, attending workshops, and participating in conferences, pharmacists can increase their understanding of and readiness for using telepharmacy. Continuing professional education is a relevant venue to increase knowledge and promote a positive attitude towards telepharmacy, especially for older pharmacists. And also developing a nation-wide telepharmacy system with appropriate features is essential to meet the requirements of pharmacy practice for future development.
Limitations
This study comes with several limitations that should be considered when interpreting the results. In this study there were limitations in obtaining unbalanced sample group proportions. This imbalance in the proportions of the sample group is considered to be able to bias the statistical test results obtained. Data results that are too homogeneous in the telepharmacy knowledge domain are also considered to be able to bias the statistical test results obtained.
In addition, because the questionnaire is filled out by respondents online, there is difficulty in ensuring that the questionnaire is filled in honestly by the respondent, even though information regarding on instructions for filling out the questionnaire has been provided. Future research can consider sampling with more attention to the proportion of the sample group to avoid possible bias in the research results.
Conclusion
Most of the participants had adequate knowledge, perception, and readiness of pharmacists to carry out pharmaceutical services through telepharmacy in Indonesia. However, they expressed concerns about the potential for an increased workload and the potential lack of incentives associated with the widespread adoption of telepharmacy practice models. Also, there is a significant association between the level of knowledge and the readiness of Indonesian pharmacists to carry out pharmaceutical services through telepharmacy, and there is a significant association between perceptions and the readiness of Indonesian pharmacists to carry out pharmaceutical services through telepharmacy.
Ethics Approval and Consent to Participate
The research and ethics committee at the Faculty of Medicine of Padjadjaran University examined the proposal before embarking on data collection (approval reference number: 1176/UN6.KEP/EC/2022 date: 21 November 2022). Prior to completing the questionnaires, the subjects were provided with informed consent. Stringent measures were implemented to ensure data confidentiality right from the data collection tool development and design. These precautions involved meticulously excluding any identifiable provider information from the gathered data and prohibiting third-party access.
Acknowledgments
We thank Rector of Universitas Padjadjaran for Travel Award 2023 and Minister of Education and Culture, Republic of Indonesia for Matching Fund-Kedaireka Grant 2022.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Misbah S, Ahmad A, Butt MH, Habib Khan Y, Alotaibi NH, Mallhi TH. A systematic analysis of studies on corona virus disease 19 (COVID-19) from Viral emergence to treatment. Syst Rev Artic JCPSP Case Reports. 2020;2:9–18. doi:10.29271/jcpsp.2020.JCPSPCR.CR9
2. Anderson RM, Heesterbeek H, Klinkenberg D, T D, Irdre H. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi:10.1016/S0140-6736(20)30567-5
3. Pascoal FB The rise of telemedicine in Indonesia; 2020. Available from: https://www.dentons.com/en/insights/articles/2020/july/20/the-rise-of-telemedicine-in-indonesia.
4. Dorsey ER, Topol EJ. State of Telehealth. N Engl J Med. 2016;375(2):154–161. doi:10.1056/NEJMra1601705
5. Al Meslamani AZ, Aldulaymi R, El Sharu H, Alwarawrah Z, Ibrahim OM, Al Mazrouei N. The patterns and determinants of telemedicine use during the COVID-19 crisis: a nationwide study. J Am Pharm Assoc. 2022;62(6):1778–1785. doi:10.1016/j.japh.2022.05.020
6. Unni EJ, Patel K, Beazer IR, Hung M. Telepharmacy during COVID-19: a Scoping Review. Pharmacy. 2021;9(4):183. doi:10.3390/pharmacy9040183
7. Alexander E, Butler CD, Darr A, et al. ASHP Statement on telepharmacy. Am J Heal Pharm. 2017;74(9):e236–e241. doi:10.2146/ajhp170039
8. Iftinan GN, Wathoni N, Lestari K. Telepharmacy: a potential alternative approach for diabetic patients during the COVID-19 pandemic. J Multidiscip Healthc. 2021;14:2261–2273. doi:10.2147/JMDH.S325645
9. Merks P, Jakubowska M, Drelich E, et al. The legal extension of the role of pharmacists in light of the COVID-19 global pandemic. Res Soc Adm Pharm. 2021;17(1):1807–1812. doi:10.1016/j.sapharm.2020.05.033
10. Oliorah PI, Isah A, Abonyi EE, et al. The assessment of telepharmacy practice among community pharmacists in Lagos, Nigeria. Niger J Pharm. 2022;56(2):556. doi:10.51412/psnnjp.2022.39
11. Poudel A, Nissen L. Telepharmacy: a pharmacist’s perspective on the clinical benefits and challenges. Integr Pharm Res Pract. 2016;5:75–82. doi:10.2147/iprp.s101685
12. Killeen RM, Grindrod K, Ong SW. Innovations in practice: telepharmacy’s time has arrived. Can Pharm J. 2020;153(5):252–255. doi:10.1177/1715163520945732
13. Crico C, Renzi C, Graf N, et al. mHealth and telemedicine apps: in search of a common regulation. Ecancermedicalscience. 2018:12. doi:10.3332/ecancer.2018.853
14. Juwita D. Pelayanan Telefarmasi RSJPD Harapan Kita: edukasi Obat Kapan Saja, Dimana Saja, Dekat dengan Anda; 2022. Available from: https://yankes.kemkes.go.id/view_artikel/252/pelayanan-telefarmasi-rsjpd-harapan-kita-edukasi-obat-kapan-saja-dimana-saja-dekat-dengan-anda.
15. Iftinan GN, Elamin KM, Rahayu SA, Lestari K, Wathoni N. Application, benefits, and limitations of telepharmacy for patients with diabetes in the outpatient setting. J Multidiscip Healthc. 2023;16:451–459. doi:10.2147/JMDH.S400734
16. Elnaem MH, Akkawi ME, Al-Shami AK, Elkalmi R. Telepharmacy knowledge, perceptions, and readiness among future Malaysian pharmacists amid the COVID-19 pandemic. Indian J Pharm Educ Res. 2022;56(1):9–16. doi:10.5530/ijper.56.1.2
17. Muhammad K, Baraka MA, Shah SS, et al. Exploring the perception and readiness of Pharmacists towards telepharmacy implementation; a cross sectional analysis. PeerJ. 2022:10. doi:10.7717/peerj.13296
18. Setiawan ZI. Peranan bauran harga terhadap pengingkatan penjualan alat kesehatan. J Pilar Nusa Mandiri. 2016;12(2):211–218.
19. Kemenkes RI Dashboard Situasi COVID-1; 2023. Available from: https://infeksiemerging.kemkes.go.id/dashboard/covid-19.
20. Firdaus. Metodologi Penelitian Kuantitatif Dilengkapi Ananlisis Regresi IBM StatisticVersion 26.0. Dotplus Publisher; 2021.
21. Suryadinata RV, Priskilla O, Wicaksono YAS. Analisis Data Kesehatan Statistika Dasar Dan Korelasi Jilid 1. Fakultas Kedokteran Universitas Surabaya. 2021.
22. Alnajrani RH, Alnajrani NR, Aldakheel FS, et al. An assessment of the knowledge, perception, and willingness to use telepharmacy services among the general public in the Kingdom of Saudi Arabia. Cureus. 2022. doi:10.7759/cureus.31769
23. Liu S, Luo P, Tang M, et al. Providing pharmacy services during the coronavirus pandemic. Int J Clin Pharm. 2020;42(2):299–304. doi:10.1007/s11096-020-01017-0
24. Tegegne MD, Wubante SM, Melaku MS, et al. Tele-pharmacy perception, knowledge and associated factors among pharmacy students in northwest Ethiopia: an input for implementers. BMC Med Educ. 2023;23(1):1–10. doi:10.1186/s12909-023-04111-9
25. Meilinda N, Malinda F, Mutiara Aisyah S. Literasi digital pada remaja digital (sosialisasi pemanfaatan media sosial bagi pelajar sekolah menengah atas). J Abdimas Mandiri. 2020;4(1). doi:10.36982/jam.v4i1.1047
26. Alboraie M, Allam MA, Youssef N, et al. Knowledge, applicability, and barriers of telemedicine in Egypt: a national survey. Int J Telemed Appl. 2021;2021. doi:10.1155/2021/5565652
27. Ahmed NJ, Almalki ZS, Alsawadi AH, et al. Knowledge, perceptions, and readiness of telepharmacy among hospital pharmacists in Saudi Arabia. Healthc. 2023;11(8):1087. doi:10.3390/healthcare11081087
28. Gani AG. Sejarah Dan Perkembangan Internet Di Indonesia. J Mitra Manaj. 2020;5(2).
29. Tjiptoatmadja NN, Knowledge ASD. Perception, and willingness to use telepharmacy among the general population in Indonesia. Front Public Heal. 2022;10:1–6. doi:10.3389/fpubh.2022.825554
30. Le T, Toscani M, Colaizzi J. Telepharmacy: a new paradigm for our profession. J Pharm Pract. 2020;33(2):176–182. doi:10.1177/0897190018791060
31. Dat Van T, Tran TD, My NT, et al. Pharmacists’ Perspectives on the Use of Telepharmacy in Response to COVID-19 Pandemic in Ho Chi Minh City, Vietnam. J Pharm Technol. 2022;38(2):106–114. doi:10.1177/87551225221076327
32. Biruk K, Abetu E. Knowledge and Attitude of Health Professionals toward Telemedicine in Resource-Limited Settings: a Cross-Sectional Study in North West Ethiopia. J Healthc Eng. 2018. doi:10.1155/2018/2389268
33. Eshita RI. Knowledge and attitude of the physicians toward telemedicine. Glob Sci Journals. 2017;5(12):85–145.
34. Sankaranarayanan J, Murante LJ, Moffett LM. A retrospective evaluation of remote pharmacist interventions in a telepharmacy service model using a conceptual framework. Telemed e-Health. 2014;20(10):893–901. doi:10.1089/tmj.2013.0362
35. Asseri AA, Manna M, Yasin M, et al. Implementation and evaluation of telepharmacy during COVID-19 pandemic in an academic medical city in the Kingdom of Saudi Arabia: paving the way for telepharmacy. World J Adv Res Rev. 2020;2020(02):2581–9615. doi:10.30574/wjarr
36. Alhmoud E, Al Khiyami D, Barazi R, et al. Perspectives of clinical pharmacists on the provision of pharmaceutical care through telepharmacy services during COVID-19 pandemic in Qatar: a focus group. PLoS One. 2022;17(10):e0275627. doi:10.1371/journal.pone.0275627
37. Shahpori R, Hebert M, Kushniruk A, Zuege D. Telemedicine in the intensive care unit environment-A survey of the attitudes and perspectives of critical care clinicians. J Crit Care. 2011;26(3):328.e9–328.e15. doi:10.1016/j.jcrc.2010.07.013
38. Baldoni S, Amenta F, Ricci G. Telepharmacy services: present status and future perspectives: a review. Med. 2019;55(7). doi:10.3390/medicina55070327
39. Ameri A, Salmanizadeh F, Keshvardoost S, Bahaadinbeigy K. Investigating pharmacists’ views on telepharmacy: prioritizing key relationships, barriers, and benefits. J Pharm Technol. 2020;36(5):171–178. doi:10.1177/8755122520931442
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.