Back to Journals » Risk Management and Healthcare Policy » Volume 13
Knowledge, Attitude, and Practice of Jinka University Students About Yellow Fever, Ethiopia: A Cross-Sectional Study
Authors Endale A , Medhin G, Hilo AA , Abegaz WE, Legesse M
Received 23 February 2020
Accepted for publication 29 June 2020
Published 19 August 2020 Volume 2020:13 Pages 1225—1236
DOI https://doi.org/10.2147/RMHP.S250930
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Kent Rondeau
Adugna Endale,1,2 Girmay Medhin,1 Abdela Alte Hilo,3 Woldaregay Erku Abegaz,4 Mengistu Legesse1
1Aklilu Lemma Institute of Pathobiology, Addis Ababa University, Addis Ababa, Ethiopia; 2School of Medicine, College of Medicine and Health Sciences, Dire Dawa University, Dire Dawa, Ethiopia; 3Jinka University, Jinka, Ethiopia; 4Department of Microbiology, Immunology & Parasitology, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Adugna Endale Email [email protected]
Background: Yellow fever (YF) is endemic in South Omo area of Ethiopia. Although Jinka University (JKU) is located in South Omo Zone, there is no information regarding the level of knowledge, attitude, and practice of students toward YF. The current study aimed to assess knowledge, attitude, and practice of JKU students toward YF and factors associated with the overall knowledge and attitude about the disease.
Methods: In this cross-sectional study, a semi-structured self-administered questionnaire was used to collect data from randomly selected regular program JNU students. Data were analyzed using SPSS. Bivariate and multivariable logistic regression analyses were performed to investigate associations of socio-demographic factors with overall knowledge and attitude scores.
Results: A total of 322 students (61.2% males, mean age of 20.7 years) participated in this study. Of these, 94.1% joined the University from places other than South Omo area and 86.0% (277/322) ever heard about YF. 9.6% were found to have a high level of overall knowledge about YF. High overall knowledge of YF was associated with being born and grown up in South Omo area (AOR=3.91; 95% CI: 1.28, 11.98) and being a student of a social science discipline (AOR=3.52; 95% CI: 1.22, 10.13). 48.8% of the participants had favorable overall attitude toward YF. Being a second-year student (AOR=1.96; 95% CI: 1.14– 3.37), being born and grown up in South Omo area (AOR=5.13; 95% CI: 1.32– 19.98), and having high overall knowledge of YF (AOR=13.24; 95% CI: 3.69, 47.44) were associated with favorable overall attitude toward YF. On the other hand, only 5.8% of the participants reported that they were vaccinated for YF.
Conclusion: The low level of knowledge and low vaccination coverage of JKU students to YF, especially among those students from other parts of the country, calls for urgent awareness creation during admission and making vaccination available.
Keywords: yellow fever, knowledge, attitude, practice, student, Ethiopia
Introduction
Yellow fever (YF) is an acute deadly disease caused by yellow fever virus (YFV). The disease is transmitted by infected female Aedes (Stegomyia) mosquitoes.1 The most common symptoms of the disease include fever, chills, loss of appetite, nausea, muscle pains particularly in the back, and headaches, and in 15% of patients liver damage is seen causing yellow skin or jaundice.2 Despite the availability of an effective vaccine since the 1930s, YF remains a major public health problem in Africa.3 In the year 2013 there were 130,000 estimated YF cases and 78,000 estimated deaths in Africa.4 Currently, YF has been considered as the commonest re-emerging disease in South America and in many African countries where there is low vaccine coverage or waned vaccine.4–6 The case fatality rate of the disease ranges from 2 to 7.5% among infected individuals but the fatality rate rises up to 50% in severe cases.7,8
In Africa, three transmission cycles of YF have been documented: sylvatic (jungle), intermediate (savannah), and urban. The sylvatic (jungle) cycle involves transmission of the virus between non-human primates (NHP) and wild mosquito species that reside within the forest canopy. In this case the virus is transmitted from the NHP like monkeys to humans by the mosquitoes when humans are visiting or working in the jungle. In the intermediate (savannah) cycle, the virus can be passed from the NHP to human or from human to human via semi-domestic mosquitoes (those of mosquitoes breeding both in the wild and near households). The urban cycle involves transmission of the virus between humans and urban mosquitoes (most of the time Aedes aegypti). Humans infected through the sylvatic or intermediate cycle usually brought the virus to the urban settings.9,10
YF is endemic in the southern parts of Ethiopia, particularly in South Omo area where it causes enormous morbidity and mortality.11–13 From 1960 to 1962, there was a large outbreak of YF in different parts of Ethiopia mainly around Gamo Gofa, Jinka, Kaffa, and Wollega areas which approximately affected about 100,000 persons and killed 30,000. In this outbreak. adults relative to children and men relative to women were more frequently affected.14 A recent epidemiological and entomological investigation made on the reemergence of YF outbreak in South Omo Zone, by Lilay et al in 2017, revealed a total of 141 suspected YF cases with 43 deaths in the South Omo area. Aedes bromeliae and A. aegypti were identified as the vectors of YF in the affected area.12 There is no routine childhood vaccination of YF in Ethiopia in general. But due to its high endemicity and recent occurrence of outbreak in the current study area, unlike the other areas of Ethiopia an emergency mass-vaccination campaign was undertaken in June 2013 in South Omo Zone to control the outbreak. Out of 607,462 people targeted for vaccination, 543,558 (89.5%) individuals were vaccinated at the time.15 Knowledge of the cause of the disease, the mode of transmission, clinical symptoms of the disease, and the correct prevention methods are vital for those individuals who are living in or travelling to YF endemic areas.16–20
Jinka University (JKU) is one of the newly established public universities and it admits students from different parts of the country. JKU is located in South Omo Zone of Ethiopia, a known hotspot for YF outbreak.12 However, there is no information on the extent of knowledge, attitude, and practice of JKU students toward YF. Therefore, this study was aimed to assess knowledge, attitude, and practice of JKU students toward YF and factors associated with overall knowledge and attitude scores with the intention of generating data to be used by JKU and other similar universities in the African setting to design appropriate intervention strategies that are useful for students from non-endemic areas for YF.
Methods
Study Area, Design, and Period
A cross-sectional study was conducted in JKU, South Omo area, southern part of Ethiopia between May and June, 2019. Students who attend their education at this university came from different parts of the country. Jinka is located 737 km south of Addis Ababa, the capital city of Ethiopia. JKU actual operation began in 2017 with an intake of 400 students. Currently, the University has a total of 2125 students in the regular program of 14 departments managed under four colleges of social sciences and humanities, business and economics, agricultural sciences, and computational and natural sciences (supplementary material 1).
Study Population, Participants, and Eligibility Criteria
The study population was all regular program students present at the time of data collection and the study participants were all randomly selected students who were eligible (both male and female, and regular program students), present at the time of data collection, and volunteered to participate in this study.
Sample Size and Sampling Technique
The sample size was determined using a single population proportion formula with the assumption that the proportion of students with a high overall level of knowledge about YF is 36%, margin of error 5%, and 95% level of confidence.21 This resulted in initial sample size of ni=354. Since the total number of JKU students (N) was 2125, application of finite population correction [nf=n/(1+n/N)] resulted in the final sample size of nf=303. Considering a 10% non-response rate, the total sample size was 333. This sample size was distributed proportionally to each department based on the number of students they had (supplementary material 1). Participants from each department were selected by a systematic random sampling technique using the list of students as a sampling frame.
Data Collection
A semi-structured self-administered questionnaire adopted from different literature21–23 was used for data collection. The questionnaire consists of items about the public health importance, cause, mode of transmission, clinical symptoms, treatment, and preventive methods of YF. Information on the socio-demographic characteristics was also part of the questionnaire (supplementary material 2). The questionnaire was self-administered to all the study participants after gathering the students in a classroom to avoid information (response) cross-exchange and the investigators closely supervised the process of data collection.
Data Management and Analysis
Participants' overall knowledge score toward YF was assessed using the following eight main questions: 1) able to mention jaundice and/or vomiting blood as the main signs/symptoms of YF; 2) able to identify that YF is different from malaria; 3) able to know that YF transmits from an infected person to another person; 4) able to know that YF is transmitted from an infected person to another person through mosquito bites; 5) able to mention that a mosquito which transmits malaria is different from a mosquito that transmits YF; 6) able to mention that YF can be transmitted from monkeys to humans through mosquito bites; 7) able to know the biting time of YF-transmitting mosquitoes; and 8) able to know that there is a vaccine to prevent YF. Responses to these questions were added together to generate an overall knowledge score ranging from 0 to 8. A score of 1 was given to correct responses and 0 for incorrect responses. Then, the response was dichotomized into a high (those who scored 5 and above) and a low (score 4 and below) overall knowledge of YF.21 Similarly, an overall attitude score of participants about YF was assessed using the following eight key questions: 1) do you think YF is a major public health issue; 2) do you think YF occurs in and around Jinka; 3) do you think YF affects all age groups; 4) do you think YF is a fatal disease; 5) do you feel you are at risk of getting YF; 6) do you believe that unvaccinated persons are at a high risk of getting YF; 7) do you think that YF is an easily treatable disease; and 8) do you think a person working/living in a forest area is at risk of getting YF? Those who respond yes to these questions are considered as a favorable attitude while the other responses (no or I am not sure) are taken as an unfavorable attitude.
After the completion of data collection, cleaning, editing, and coding, the data were computerized using Epi-Data Entry version 3.1 and analyzed using SPSS version 25.0. Descriptive statistics (ie mean and standard deviation for continuous variables and frequency for categorical variables) were used to summarize the collected data. Bivariate and multivariable logistic regression analyses were performed to quantify crude and adjusted effects of pre-specified socio-demographic characteristics on overall knowledge score and overall attitude score. The strength of association between predictors and the outcome variable was quantified using the odds ratio. Statistical significance was reported whenever the p-value was less than 0.05. Model fitness was checked using the Hosmer and Lemeshow goodness-of-fit test (P>0.05 indicating no evidence of poor fit).
Ethics Approval and Consent to Participate
The study protocol was approved by the Institutional Review Board (IRB) of Aklilu Lemma Institute of Pathobiology, Addis Ababa University. Permission was obtained from the JKU students’ Dean and the study was conducted in accordance with the Declaration of Helsinki. The objective of the study was explained to the participants. The questionnaires were administered after obtaining informed written consent from each participant. The reporting of thist study conforms to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement (supplementary material 3).
Results
Socio-Demographic Characteristics of Study Participants
A total of 322 participants with a response rate of 96.7% (61.2% males, age range from 18 to 30 years, mean age±SD=20.7±1.6 years) were involved in this study. Of these participants 67.1% were second-year students, 41.9% were from college of agriculture and natural resource management, and 94.1% joined the University from places other than South Omo area (Table 1).
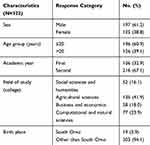 |
Table 1 Socio-Demographic Characteristics of Study Participants, JKU, South Omo Area, 2019 |
Knowledge of Study Participants About the Cause and Sign/Symptoms of YF
The majority (86.0%) of the participants heard about YF (76.4% among first-year students and 90.7% among second-year students, P<0.01) and 43.9% of them heard the information from health workers. Out of 277 participants who heard about YF, 80.1% reported that they knew common signs and symptoms of YF. The most commonly mentioned include headache (53.6%), fever (47.3%), yellowish eye and skin (46.4%), and vomiting blood (15.3%). Out of 182 (65.7%) participants who reported that they knew the cause of YF, 59 (32.4%) mentioned virus and 104 (57.1%) mentioned bacteria as the cause of YF (Table 2).
 |
Table 2 Frequency Distribution of Participants’ Knowledge About the Cause and Signs/Symptoms of YF |
Knowledge of Participants About Mode of Transmission and Prevention of YF
Out of the 277 participants, 106 (38.3%) reported that YF is transmitted from person to person (27.2% among first-year students and 42.9% among second-year students, P=0.02; 45.7% among males and 25.5% among females, P<0.01). Sixty (21.7%) individuals reported that YF can be transmitted from monkeys to human (11.1% among first-year students and 26.0% among second-year students, P=0.01; 24.6% among males and 16.7% among females, P=0.12).
From the 106 participants who stated that YF can be transmitted from person to person and 60 participants who heard that YF can be transmitted from monkey to human, 81 (76.4%) and 50 (83.3%), respectively, reported mosquito bites. From the 81 participants who said that YF can be transmitted from person to person through mosquito bites, only 14 (17.3%) mentioned that the mosquito which transmits YF is different from the one that transmits malaria.
Similarly, out of 228 participants who heard about both YF and malaria, 124 (54.4%) reported that YF is different from malaria (41.5% among first-year students and 59.5% among second-year students, P=0.02; 58.4% among males and 48.4% among females, P<0.01). From the 124 participants who had knowledge about differences between YF and malaria, 68 (86.1%) stated that the treatment for YF is different from that for malaria.
Out of the 201 participants who knew about YF being a preventable disease, 107 (53.2%) mentioned vaccine, 74 (36.8%) described preventing mosquito bites, and 94 (46.8%) said spraying chemicals around dormitories as the main prevention methods (Table 3).
 |
Table 3 Frequency Distribution of Participants’ Knowledge About Mode of Transmission and Prevention of YF |
Attitude of JKU Students Toward YF
Table 4 shows summary information about the attitude of JKU students toward YF. Out of the 277 participants who heard about YF, 53.8% believed that YF is a major public health problem in the area, and 54.2% thought that Jinka is an endemic area for YF (38.3% among first-year students and 60.7% among second-year students, P<0.01). Similarly, 72.9% believed that YF affects all age groups, 72.6% perceived that YF is a fatal/killer disease, 52.3% felt that they are at risk of getting YF, 53.8% believed that unvaccinated persons to be at high risk of getting YF, and 41.9% believed that a person who is working/living in a forest area to be at high risk of getting YF, while 41.2% were not sure (Table 4).
 |
Table 4 Frequency Distribution of Participants’ Attitude Toward YF |
Practice of JKU Students Toward YF Prevention
Out of the 277 participants who heard about YF, only 5.8% reported that they are vaccinated for YF (2.5% among first-year students and 7.1% among second-year students, P=0.13). About 23.1% reported that they got orientation about YF when they joined the University (22.2% among first-year and 23.5% second-year students), while 10.1% reported that they visited/went to forest/jungle areas for different purposes (Table 5).
 |
Table 5 Frequency Distribution of Participants YF Related Risky Practices |
Overall Knowledge of Participants About YF
Out of the total study participants, 9.6% had high level of overall knowledge of YF (8.6% among first-year students and 10.2% among second-year students) (Figure 1) (and 11.7% among males and 6.4% among females). High level of overall knowledge was associated with being born and grown up in South Omo Zone (AOR=3.91; 95% CI: 1.28, 11.98) and being a student of a social science discipline (AOR=3.52; 95% CI: 1.22, 10.13) as compared to an agricultural science discipline (Table 6).
 |
Table 6 Bivariate and Multivariable Logistic Regression Analyses Showing Factors Associated with Overall Knowledge of Study Participants About YF |
 |
Table 7 Bivariate and Multivariable Logistic Regression Analyses Showing Factors Associated with Overall Attitude of Study Participants About YF |
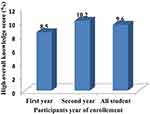 |
Figure 1 Rate of high overall knowledge score by year of enrollment and among all participants. |
Overall Attitude of Participants About YF
From the total participants, 48.8% had favorable overall attitude toward YF (34.9% among first-year students and 55.6% among second-year students) (Figure 2). Similarly, 55.3% of male participants and 38.4% of female participants had favorable overall attitude. Being a second-year student (AOR=1.96; 95% CI: 1.14, 3.37), being born and grown up in South Omo area (AOR=5.13; 95% CI: 1.32, 19.98), and having high overall knowledge (AOR=13.24; 95% CI: 3.69, 47.44) were of significantly favorable overall attitude toward YF as compared to their counterparts.
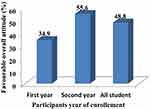 |
Figure 2 Rate of favorable overall attitude score by year of enrollment and among all participants. |
Discussion
Emerging and re-emerging mosquito-borne viral diseases such as YF, dengue fever (DF), and Chikungunya (CHIK) are becoming major public health threats in different parts of Ethiopia. In this study, we assessed the knowledge, attitude, and practice of JKU students toward YF. The students joined the University from different parts of the country including YF non-endemic areas. About 94% of the participant students in this study joined the university from areas outside South Omo Zone where no previous interventional activities including YF vaccination were conducted. The key findings of this study include: 1) the majority of the study participants have low overall knowledge about YF; 2) a high level of overall knowledge of YF was associated with being born and grown up in South Omo Zone and being a student of a social science discipline; 3) despite poor overall knowledge, nearly half of participants have favorable overall attitude toward YF; 4) favorable overall attitude of YF associated with being a second-year student, being born and grown up in South Omo, and having high overall knowledge of YF; and 5) more than three-quarters of the students were not vaccinated for YF while joining the University.
The findings of the current study revealed that the overall knowledge of the students about YF is low. The majority of the students have poor knowledge of the cause, mode of transmission, symptoms, and major prevention methods. The overall knowledge score in this study is lower than reports from similar studies conducted on the general population of residents of South Omo Zone,21 and among university students of other countries on related arboviruses.24–29 The observed low overall knowledge score in the current study might be due to the fact that the majority of the students who participated in this study were from non-endemic areas for YF. In most areas of Ethiopia, YF intervention is not actively implemented due to the intermittent nature of the disease and the lack of a supportive surveillance system which may leave the population unaware of the disease. To some extent, better interventional activities are seen in South Omo Zone unlike the other areas of Ethiopia due to the recent YF outbreak in this area.12 The proportion of students who had high overall knowledge about YF in the current study was below the assumption we set at the beginning of the study for sample size calculation (36%). Despite underestimation of the parameter, this does not affect the generalization of the study because it ensures a maximum sample size which in turn strengthens the certainty of the inference drawn from the study.
In this study, a high level of overall knowledge about YF was significantly associated with being born and grown up in South Omo as compared to students from other areas of Ethiopia. Participants who joined JKU from South Omo Zone have about four-fold higher overall knowledge about YF compared to those who joined the University from other parts of the country. Our finding is similar with the results of a study done in Iran among international students of Tehran University, which revealed that participants who came from YF endemic countries have more knowledge about YF compared to those from non-endemic countries.28 Due to the recent occurrence of the YF outbreak with significant morbidity and mortality in South Omo Zone,12 there is active YF intervention in this part of the country unlike the other areas. Thus, the existing YF interventions including health education delivery in the YF endemic areas probably increase the level of individuals' overall knowledge. Similarly, being a student of a social science discipline was also significantly associated with a high level of overall knowledge score as compared to an agricultural science discipline student. This might be due to the nature of the discipline, in which social science discipline students have more access to mass media information, including disease prevention and control issues or agendas. In addition, second-year students have relatively a little bit higher overall knowledge about YF as compared to first-year students. The level of awareness about YF among the participants in the current study showing marked difference across year of stay is congruent with a report from a Malaysian study among private University healthcare students where a statistically significant association was observed between the year of study and knowledge score about chikungunya.24 Our current study also showed that participants had limited sources of information about YF. The majority of the participants got the information from health professionals. As shown by Fritzell et al, use of alternative methods like school-based interventions, television, and social networks would be of paramount importance to increase the coverage and access of information on YF and other similar diseases.26 In the current study, no statistically significant difference was observed between male and female participants in their overall knowledge level about YF. This might be due to equal exposure status to awareness creation opportunities at school level, unlike community level, for males and females.
Although jaundice and vomiting of blood along with soft palate hemorrhage are the common symptoms of YF which help to differentiate the disease from other febrile illnesses like malaria, only 34 participants reported vomiting blood and 103 participants reported yellowish eye and skin as the main symptoms of YF. The majority of the participants had no information regarding the difference between YF and malaria as well as the differentiate mosquitoes which transmit YF and malaria. They consider YF as a synonym of sever falciparum malaria (cerebral malaria). This might be due to the better awareness of participants to malaria as three-quarters of the land of Ethiopia is endemic for malaria30 and a malaria intervention exists all over the country which might provide an opportunity to know more for the public compared to YF, which is localized to a few areas of the country.13,14 This finding is in line with a study done in South Omo among the general population.21 Moreover, most of the students consider the biting time of the mosquitoes to be at night like that of the malaria vector. It is known that the biting time of Aedes mosquitoes which transmit YF is after dawn and before dusk.31 Thus, lack of knowledge of the biting time will probably increase the likelihood of outdoor exposure to the vector in the day time while the students visit sylvatic areas.
Besides cognitive determinants, attitudes of individuals play a great role in the adoption of protective behaviors for the prevention and control of infectious diseases.32 A good or favorable attitude toward disease prevention and control among the younger generation, especially university students, is highly desired to apply good preventive practice during their campus stay in endemic areas. Moreover, the younger generation can spread the important information to a wider community. In this study, despite poor overall knowledge of participants about YF, nearly half of the participants have favorable overall attitude toward YF. The majority of the participants perceived YF as a major public health problem of the area and, a fatal disease, and that all age groups are at risk of contracting the disease. In addition, a significant number of participants believed unvaccinated individuals to be at high risk of getting YF infection, especially those visiting sylvatic areas including Mago National Park and other bushy areas. The finding of this study is in line with the finding from a similar study conducted in South Omo Zone among the general population21 and the one from Malaysia on dengue fever among university students.29 Such a positive attitude of students toward YF prevention should be supported by establishing a system of good practice to prevent and control the disease in a sustainable manner. Second-year students have about two-fold higher favorable overall attitude as compared to first-year students. Our finding is supported by the study done in Philippines which showed advanced year of study having a relatively better attitude score compared to less advanced year of study.27 In addition, in the current study local students (South Omo area students) have about five times more favorable overall attitude toward YF compared to students who joined JNU from other geographic areas of Ethiopia. The study done among international students in Tehran University also showed that students from African endemic countries have a favorable or positive attitude toward YF compared to those coming from other (non-endemic) areas of the world.28 On the top, our findings revealed that participants having higher overall knowledge of YF have about 13 times more favorable overall attitude score compared to those having lower overall knowledge score. These finding was supported by other knowledge, attitude, and practice-based studies done elsewhere.33,34
Although YF is a vaccine-preventable disease2 and JKU is located in the YF endemic area,12 the vaccine coverage among the study participants was very low, leaving this young educated generation at risk of acquiring the disease. Unvaccinated individuals particularly from non-endemic areas with no prior exposure to YF are at high risk of contracting the disease. In the current study, almost all of the YF vaccinated individuals are residents of South Omo Zone, where they received the vaccine during emergency mass vaccination that was provided for the general population immediately after the 2012/13 YF outbreak in the area.15 Moreover, only less than a quarter of the students got orientation about YF when they joined the University. There is an urgent need to address the gap identified in this study by identifying the cost-effective entry point, which is likely to be during admission to the University. Despite poor vaccination coverage, a quarter of the students reported that they visit regularly or intermittently forest areas for different activities like study, reaction, and wildlife. This would probably increase their risk of exposure to sylvatic transmission of YF.35 A study done in the Central African Republic also reported a higher infection rate of YF among residents bordering forest areas.36
Limitation of the Study
To the best of our knowledge, there is no previous study conducted on the awareness of arboviruses among students who are joining different universities found in endemic areas of Ethiopia, including JKU. However, the study has not carried out a detailed assessment of the knowledge of the study participants regarding the difference between malaria (falciparum malaria) and YF, and also was not supported by focus group discussion. Moreover, additional data were not collected from the University management and health professionals regarding activities like health education and vaccination to protect JKU students from getting YF.
Conclusion
The knowledge of JKU students about YF is low, which can in turn jeopardize their preventive practices. About half of the students have unfavorable attitude toward YF and more than 90% of the students were not vaccinated for YF. A high overall knowledge of YF was associated with being born and grown up in South Omo area and being a student of a social science discipline, and a favorable overall attitude toward YF associated with being a second-year student, being born and grown up in South Omo area, and having high overall knowledge of YF. Hence, it is highly recommended to establish appropriate prevention and control strategies customized to university students like awareness creation during admission, mass vaccination campaign, and other school-based intervention of YF and related arboviruses in parallel to the general population.
Abbreviations
YF, yellow fever; YFV, yellow fever virus; JKU, Jinka University; IRB, Institutional Review Board.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Acknowledgments
We would like to acknowledge the study participants, data collectors, and Jinka University for facilitating the data collection.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. WHO. World Health Organization: risk assessment on yellow fever virus circulation in endemic countries working document from an informal consultation of experts’ Editorial work by Biotext Pty Ltd, Australia. 2014.
2. WHO. World Health Organization: vaccines and vaccination against yellow fever WHO position paper June 2013. Wkly Epidemiol Rec. 2013;88:269–283.
3. Mutebi JP, Barrett AD. The epidemiology of yellow fever in Africa. Microbes Infect. 2002;4(14):1459–1468. doi:10.1016/S1286-4579(02)00028-X
4. Garske T, Van Kerkhove MD, Yactayo S, et al. Yellow fever in Africa: estimating the burden of disease and impact of mass vaccination from outbreak and serological data. PLoS Med. 2014;11(5):e1001638. doi:10.1371/journal.pmed.1001638
5. Gardner CL, Ryman KD. Yellow fever: a reemerging threat. Clin Lab Med. 2010;30(1):237–260. doi:10.1016/j.cll.2010.01.001
6. Ortiz-Martinez Y. Global research trends of yellow fever: a bibliometric overview. J Infect Public Health. 2018;11(2):297–298. doi:10.1016/j.jiph.2017.07.016
7. Tomori O. Yellow fever: the recurring plague. Crit Rev Clin Lab Sci. 2004;41(4):391–427. doi:10.1080/10408360490497474
8. Monath TP. Treatment of yellow fever. Antiviral Res. 2008;78(1):116–124. doi:10.1016/j.antiviral.2007.10.009
9. Douam F, Ploss A. Yellow fever virus: knowledge gaps impeding the fight against an old foe. Trends Microbiol. 2018;26(11):913–928. doi:10.1016/j.tim.2018.05.012
10. CDC. Center for disease control and prevention: yellow fever: transmission of yellow fever; 2019. Available from: https://www.cdc.gov/yellowfever/transmission/index.html.
11. Ardoin P, Rodhain F, Hannoun C. Epidemiologic study of arboviruses in the Arba-Minch district of Ethiopia. Trop Geogr Med. 1976;28(4):309–315.
12. Lilay A, Asamene N, Bekele A, et al. Reemergence of yellow fever in Ethiopia after 50 years, 2013: epidemiological and entomological investigations. BMC Infect Dis. 2017;17(1):343. doi:10.1186/s12879-017-2435-4
13. Serie C, Andral L, Lindrec A, Neri P. [EPIDEMIC OF YELLOW FEVER IN ETHIOPIA (1960–1962). PRELIMINARY STUDY]. Bull World Health Organ. 1964;30:299–319.French.
14. Sérié C, Andral L, Poirier A, Lindrec A, Neri P. Studies on yellow fever in Ethiopia: epidemiologic study. Bull World Health Organ. 1968;38(6):879–884.
15. WHO. World Health Organization: emergencies preparedness, response Yellow fever in Ethiopia. 2016.
16. Hamer DH, Connor BA. Travel health knowledge, attitudes and practices among United States travelers. J Travel Med. 2004;11(1):23–26. doi:10.2310/7060.2004.13577
17. Khatibi S, Marchou B. [Assessment of travel-associated risks and advice to travelers]. Rev Prat. 2007;57(8):831–842.French.
18. Krief I, Goldblatt JG, Paz A, Potasman I. Late vaccination against yellow fever of travelers visiting endemic countries. Travel Med Infect Dis. 2006;4(2):94–98. doi:10.1016/j.tmaid.2005.02.001
19. Van Herck K, Van Damme P, Castelli F, et al. Knowledge, attitudes and practices in travel-related infectious diseases: the European airport survey. J Travel Med. 2004;11(1):3–8. doi:10.2310/7060.2004.13609
20. Zhang M, Zhang J, Hao Y, et al. Vaccination knowledge, attitude and practice among Chinese travelers who visit travel clinics in Preparation for international travel. J Travel Med. 2016;23(6):taw051. doi:10.1093/jtm/taw051
21. Legesse M, Endale A, Erku W, Tilahun G, Medhin G, Althouse B. Community knowledge, attitudes and practices on Yellow fever in South Omo area, Southern Ethiopia. PLoS Negl Trop Dis. 2018;12(4):e0006409. doi:10.1371/journal.pntd.0006409
22. Jeelani S, Sabesan S, Subramanian S. Community knowledge, awareness and preventive practices regarding dengue fever in Puducherry - South India. Public Health. 2015;129(6):790–796. doi:10.1016/j.puhe.2015.02.026
23. Shuaib F, Todd D, Campbell-Stennett D, Ehiri J, Jolly PE. Knowledge, attitudes and practices regarding dengue infection in Westmoreland, Jamaica. West Indian Med J. 2010;59(2):139–146.
24. Ali AN, Hui CJ, Prajapati SK, Zulfikar AN. Knowledge and awareness regarding Chikungunya: a cross-sectional study among healthcare students in a private university, Malaysia. MOJ Bioequiv Availab. 2018;5(6):293–298.
25. Bota R, Ahmed M, Jamali MS, Aziz A. Knowledge, attitude and perception regarding dengue fever among university students of interior Sindh. J Infect Public Health. 2014;7(3):218–223. doi:10.1016/j.jiph.2013.11.004
26. Fritzell C, Raude J, Adde A, Dusfour I, Quenel P, Flamand C. Knowledge, attitude and practices of vector-borne disease prevention during the emergence of a new arbovirus: implications for the control of Chikungunya virus in French Guiana. PLoS Negl Trop Dis. 2016;10(11):e0005081. doi:10.1371/journal.pntd.0005081
27. Lozano Elena B. Knowledge, attitudes and practices on dengue and Zika viruses from four institutional divisions of Cebu normal university, Cebu city, Philippines. Int J Mosq Res. 2018;5(4):33–38.
28. Muhammad FM, Basseri H, Majdzadeh R, Shahandeh K, Foroushani AR. Knowledge attitude and practice (KAP) study of Yellow fever among international students of Tehran University of Medical Sciences, Iran. Iran J Public Health. 2019;48(7):1384–1386.
29. Amanah Mohamad A, Abdullah H, Abdul Ghafar N. Knowledge attitude and practice on dengue among university students. Int J Community Med Public Health. 2018;5(11):4720–4724. doi:10.18203/2394-6040.ijcmph20184562
30. Ayele DG, Zewotir TT, Mwambi HG. Prevalence and risk factors of malaria in Ethiopia. Malar J. 2012;11:195. doi:10.1186/1475-2875-11-195
31. CDC. Centers for disease control and prevention: travel yellow book. CDC, editor. CDC Health Information for International Travel. Atlanta GA; 2008.
32. Flamand C, Camille F, Obale P, Quenel P, Raude J. The role of risk proximity in the beliefs and behaviors related to mosquito-borne diseases: the case of Chikungunya in French Guiana. Am J Trop Med Hyg. 2017;97(2):344–355. doi:10.4269/ajtmh.16-1028
33. Abi Doumit C, Haddad C, Sacre H, et al. Knowledge, attitude and behaviors towards patients with mental illness: results from a national Lebanese study. PLoS One. 2019;14(9):e0222172. doi:10.1371/journal.pone.0222172
34. Kassahun CW, Mekonen AG, Ciccozzi M. Knowledge, attitude, practices and their associated factors towards diabetes mellitus among non diabetes community members of Bale Zone administrative towns, South East Ethiopia. A cross-sectional study. PLoS One. 2017;12(2):e0170040. doi:10.1371/journal.pone.0170040
35. Endale A, Daniela M, Erku W, et al. Community-based sero-prevalence of chikungunya and yellow fever in the South Omo Valley of Southern Ethiopia. PLoS Negl Trop Dis. In press 2020.
36. Staples JE, Diallo M, Janusz KB, Manengu C, Lewis RF, Perea W. Yellow fever risk assessment in the Central African Republic. Trans R Soc Trop Med Hyg. 2014;108(10):608–615.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
