Back to Journals » Infection and Drug Resistance » Volume 17
Knowledge, Attitude, and Practice About Antibiotic Use and Antimicrobial Resistance Among Nursing Students in China: A Cross Sectional Study
Authors Yang C, Xie J, Chen Q, Yuan Q, Shang J, Wu H, Yang Y, Wang M, Shu X , Yue J, Tu D, Lin Y, Zheng R, Wu X
Received 14 December 2023
Accepted for publication 6 March 2024
Published 19 March 2024 Volume 2024:17 Pages 1085—1098
DOI https://doi.org/10.2147/IDR.S454489
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Chaoping Yang,1,* Jing Xie,2,* Qianjun Chen,2 Qiongyin Yuan,3 Jianping Shang,4 Haibo Wu,5 Youhua Yang,6 Mingfang Wang,7 Xiaolan Shu,8 Jing Yue,9 Danna Tu,10 Ying Lin,1,* Ronghao Zheng,4,* Xiaolin Wu4
1Nursing Department, Maternal and Child Health Hospital of Hubei Province, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s Republic of China; 2Department of Pediatric Nephrology, Rheumatology, and Immunology, Maternal and Child Health Hospital of Hubei Province, Hubei University of Medicine, Shiyan, Hubei, People’s Republic of China; 3Obstetrical department, Huanggang Maternal and Child Health Hospital, Hubei, People’s Republic of China; 4Department of Pediatric Nephrology, Rheumatology, and Immunology, Maternal and Child Health Hospital of Hubei Province, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s Republic of China; 5School of Health and Nursing, Wuchang University of Technology, Wuhan, People’s Republic of China; 6Department of Basic Medical Sciences, School of Medicine, Jianghan University, Wuhan, People’s Republic of China; 7Department of Pediatric Gastroenterology, Maternal and Child Health Hospital of Hubei Province, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s Republic of China; 8Department of Pediatric Intensive Care Unit (PICU), Maternal and Child Health Hospital of Hubei Province, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s Republic of China; 9Emergency Department, Maternal and Child Health Hospital of Hubei Province, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei Province, People’s Republic of China; 10Department of Pediatric Cardiology, Maternal and Child Health Hospital of Hubei Province, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ronghao Zheng, Department of Pediatric Nephrology, Rheumatology, and Immunology, Maternal and Child Health Hospital of Hubei Province, Tongji Medical College, Huazhong University of Science and Technology, 745 Wu Luo Road, Hongshan District, Wuhan, Hubei Province, 430070, People’s Republic of China, Email [email protected] Ying Lin, Nursing department, Maternal and Child Health Hospital of Hubei Province, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s Republic of China, Email [email protected]
Purpose: The knowledge, attitude, and practices (KAP) concerning antibiotics by healthcare students have the potential impact on controlling antibiotic abuse and antimicrobial resistance (AMR) growth. This study aims to evaluate the levels and explore the associated factors with KAP on antibiotic use and AMR in Chinese nursing students.
Methods: A cross-sectional survey using a self-administered questionnaire consisting of demographics and selected features and KAP on antibiotic use and AMR was conducted to measure KAP levels among nursing students at various universities in Hubei Province, China. The logistic regression analyses were performed to analyze the potential factors associated with the KAP.
Results: The survey eventually included a total of 1959 nursing students. The mean scores for KAP were 57.89 ± 26.32, 55.00 ± 12.50, and 71.88 ± 15.63, respectively. Regarding knowledge, 54.3% of participants were unaware that antibiotic was ineffective against viral infections. Regarding attitude, 36% of participants agreed that current antibiotic abuse existed; 96.2% of participants thought it necessary to set up a special course on antibiotics. Regarding practice, only 48.4% of participants usually purchased antibiotics with a prescription. Multivariable analyses indicated that lack of discussion on AMR in school courses was an independent risk factor against KAP, respectively. The main knowledge sources of antibiotic being outside the classroom was an independent risk factor related to knowledge and practice. The average score > 80 points was an independent protective factor related to knowledge and practice.
Conclusion: The KAP level on antibiotic use and AMR among Hubei nursing students was general and required further strengthening. Nursing students with risk factors should be prioritized in educational interventions. The findings of our study pointed out some directions for tailored interventions to improve the training on antibiotics.
Keywords: antibiotic use, antimicrobial resistance, knowledge, attitude, practice, nursing students
Introduction
Since Alexander Fleming discovered penicillin in 1928, antibiotics have saved countless lives and expanded humans’ average life.1 At the same time, the emergence and application of antibiotics have laid the foundation of modern medicine. Unfortunately, this admirable medical practice of antibiotics is being threatened by their misuse and overuse, leading to AMR. The widespread increase of AMR has already become a huge challenge for threatening human security, which can cause unresponsiveness to antibacterial treatment, ultimately resulting in persistent illness and increased risk of death.2 Besides, AMR has brought a tremendous economic burden. It has been estimated that AMR could bring an economic impact of up to US $100 trillion by 2050.3
The knowledge of the appropriate use of antibiotics and prevention of AMR is really important to reduce AMR.4 However, previous studies have shown that the common public has a poor understanding and attitude towards antibiotics and the use of antibiotics.5,6 Numerous studies have reported that improper antibiotic use among university students is also common due to lack of adequate knowledge of antibiotics and self-medication.7 What is more, several studies indicated that the level of knowledge, attitudes and perceptions on antibiotic use and AMR even in the cohort of health workers was not good. Due to insufficient knowledge, incorrect attitudes, monetary incentives, and patient persistence, health workers prescribe inappropriate and unnecessary antibiotics, resulting in AMR.7,8
The world health organization (WHO) global action plan had suggested that improving awareness and understanding of antibiotics and AMR through effective communication, education and training, was urgently needed to control further expansion of AMR.9 It is noted that several studies have implied that education about antibiotics and their appropriate use should focus on undergraduate training, which has an important impact on the future professional’s attitudes and behaviors regarding antibiotic use and AMR.10,11 This training is really critical for senior students of professional health care degrees, such as medicine, pharmacy and nursing.
Nursing staff are the ultimate executor of antibiotic use and the ultimate quality controller of antibacterial drug use. The American Nurses Association and the Centers for Disease Control and Prevention have jointly issued a white paper on nurse participation in antimicrobial drug management, encouraging nurses across the United States to actively participate in antimicrobial drug management.12 Nursing students also shoulder important responsibilities in patient education and general public health education after employment.13 Although reports from the WHO and other studies suggest that giving training for paramedical students on rational antimicrobial prescribing and introducing the concept of antimicrobial stewardship into the undergraduate curricula are imperative, previous studies have only focused on medical students.14 Nursing students who also play a vital role in the prevention and promotion of AMR were neglected.15
The aim of the current study was to evaluate the level of knowledge, attitude and practice related to antibiotic use and AMR and explore the potentially associated factors with KAP on antibiotic use and AMR among nursing students in Hubei province, China. This study will be helpful for formulating intervention of training curriculum in nursing students in the future. The results could also provide information for policy guidance and interventions to improve their training in the proper use of antibiotics.
Materials and Methods
Study Design
This was a cross-sectional study using an online self-administered questionnaire conducted among pre-internship nursing students between February 28 and March 21, 2023. We followed the method of “simple random sampling” and randomly selected several different nursing colleges in Hubei Province, China. Then, the method of “cluster random sampling” was adopted, and several classes were randomly selected based on the classes in class on the survey day to conduct a survey on all students attending classes. The majority of nursing students in several colleges studied the knowledge of antibiotics and AMR in the course of pharmacology in the second academic year, in the third year of medical nursing and surgical nursing also involved in the relevant knowledge of antibiotics and AMR. These courses are fundamental in the consolidation of knowledge on the use of antibiotics and the problems of AMR.
Participations were voluntary, anonymous and without compensation. Before conducting the questionnaire, the researchers explained the background and intent of the survey and encouraged students to participate without undue pressure. Electronic informed consent was signed by all survey participants prior to enrolment. Participants were told to answer each item for taking at least one second and were allowed to terminate the survey at any time. The IP address of each participant was allowed to complete the questionnaire only once. Data were anonymously collected through Wenjuanxing electronic questionnaire platform (www.wjx.cn), and confidentiality of information was assured. The study was approved by the clinical research ethics committee of the Maternal and Health Hospital of Hubei Province (2023IEC124NO).
Sample Size
The sample size was measured by the Raosoft sample size calculator16 with a 5% margin of error and 95% confidence interval. Based on the above parameters, the minimum number of samples to be estimated was 384. However, to improve the reliability of the data, the sample size was expanded to not less than 1000 students.
Participants
All pre-internship nursing students enrolled in the above selected colleges were eligible to be recruited in the study. Students who were unwilling to participate in this survey were excluded from the study. Our questionnaire included a multiple-choice question on whether participants volunteered to participate in the survey; those who responded negatively were automatically excluded by the platform.
Questionnaire
The questionnaire was self-designed based on a literature review of similar studies conducted in different regions of the world and the WHO questionnaire for antibiotic resistance: multi-country public awareness survey,2,17–23 and some modifications were made to the questions based on common practical knowledge in China. The language of the questionnaire was presented in Chinese. The questionnaire consisted of the basic demographic and selected features and the KAP of antibiotic use and AMR. A pilot study was conducted among 209 students to evaluate the reliability and validity of the instrument. Necessary modifications to the questionnaire were made based on preliminary study feedback. Data from these students were not included in the final analysis. The internal consistency and reliability of the survey questions was verified using Cronbach’s alpha, with a value of 0.808 indicating high reliability.
Finally, a 56-item questionnaire with 4 sections was developed for the final survey execution. The first part of the questionnaire was the basic demographic and selected features data, which were self-reported by the participants, included 11 questions such as gender, age, and educational level. The second part consisted of 19 questions, which evaluated students’ knowledge level of antibiotic and antibacterial resistance by asking questions about the identification of antibiotics, the scope of treatment, adverse effects, and awareness of AMR. The third section included 10 questions to assess the attitudes of respondents regarding antibiotic use and AMR, including their desire for antibiotics, common misconceptions about antibiotic use, AMR, and eagerness to learn relevant knowledge. The last part was composed of 16 questions focusing on antibiotic use behavior, including antibiotic use status, preventive use, access to antibiotic, understanding of antibiotics prior to use, course of antibiotic use, and next use and recommendation of antibiotics.
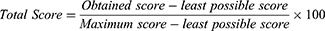
For knowledge-related questions, a score of “1” was given for correct answers, and a score of “0” was given for incorrect or “don’t know” answers. The minimum and maximum possible scores in the knowledge domain were 0 and 19, respectively. Responses to questions related to attitude and practice were scored on a 5-point Likert scale from 1 to 5, Score “1” was given for the least appropriate answer and “5” was given for the most appropriate response. Some of the questions were unfavorable, and the questions were scored in the reverse direction. The lowest possible score was 10, and the highest possible score was 50 for the attitude section. The minimum and maximum possible scores for the practice section were 16 and 80, respectively. The scores of knowledge, attitude, and practice were transformed to a scale ranging from 0 (worst possible score) to 100 (best possible score) with the formula (Equation (1.1)).2 The total scores of <80 and ≥80 were categorized as general level and good level for KAP, respectively.
Data Analysis
Data collected were checked for completeness and consistency before analysis. Incomplete questionnaires were excluded and considered non-response rates. The results were analyzed using IBM SPSS statistical software version 23.0. The scores of KAP on antibiotic use and AMR in this study were not normally distributed and thus were presented as medians with interquartile ranges (IQRs). The ranked data were presented as numbers and percentages. The Chi-square test was conducted to explore the significant associations between demographic and selected features and KAP on antibiotic use and AMR. Multivariable logistic regression analyses were employed to identify the independent factors associated with KAP on antibiotic use and AMR. The associations between factors and outcomes were presented as odds ratios (ORs) and 95% confidence intervals (CIs). A P-value of <0.05 was considered statistically significant.
Results
Demographic and Selected Features
A total of 2043 questionnaires were distributed in the study area, of which 1959 students returned completed surveys. The recorded response rate was 95.9%. The majority of responders were female (87.2%) and had an education level below undergraduate level (86.8%). Importantly, most responders stated that the main source of antibiotic knowledge is in the classroom (77.7%) and there was a discussion on AMR in the school courses (79.5%). However, the average score of the majority of students (65.4%) in the last semester was below 80 points. It is noted that almost one third of responders reported using antibiotics within the past 6 months. Detailed demographic characteristics of the participating students are illustrated in Table 1.
 |
Table 1 Demographic and Selected Features of Participants |
The Scores of KAP on Antibiotic Use and AMR
Overall, participants had general levels of KAP on antibiotic use and AMR. The average scores for knowledge, attitude and practice were 57.89 ±26.32, 55.00 ±12.50 and 71.88 ±15.63, respectively. Only a few participants had good KAP levels for antibiotic and AMR (Table 2).
 |
Table 2 The Number of Questions, Range, Score, and Level of KAP on Antibiotic Use and AMR |
Knowledge on Antibiotic Use and AMR
In the knowledge section, respondents demonstrated satisfactory knowledge in identifying whether amoxicillin was an antibiotic or not, with approximately 80% correctly responding to related statements. However, 56.9% of respondents were unaware that aspirin was not an antibiotic, 61.4% of respondents were unaware that Prednisone was not an antibiotic, which was surprising. More than half of the participants mistakenly believed that antibiotics were useful for treating viral infections and that they could boost the body’s resistance. Even more than 66% of the participants believed that antibiotics were effective in reducing fever and accelerating recovery from the common cold. Less than 50% of the participants agreed that “Antibiotic can kill good bacteria present in our organism” and that “Antibiotic resistant bacteria can spread from person to person” (Table 3).
 |
Table 3 Responses to the Questionnaire on Antibiotic Use and AMR Knowledge (N = 1959) |
Attitude on Antibiotic Use and AMR
Among the most important results on attitude (Figure 1), 15.7% of students are very willing to obtain antibiotics without a prescription. 12.4% of students stated that they would be very frustrated if their doctor did not provide antibiotics in their treatment regimen. Less than half of the students agree that every person treated with antibiotics is at an increased risk of antibiotic-resistant infection (41.6%), and AMR can affect their and their family’s health (41.0%). Even fewer participants agreed that there was antibiotic misuse (36.0%). 31.5% of participants believed they had adequate knowledge of how to use antibiotics appropriately in current practice. Fortunately, 96.3% of participants thought it was necessary to set up a special course on antibiotics.
 |
Figure 1 Distribution of attitudes on antibiotic use and AMR among nursing students. |
Practice on Antibiotic Use and AMR
When asked about previous use of antibiotics, 23.1% of participants answered that they sometimes take antibiotics when they have a fever, and 24.3% of participants sometimes use antibiotics when they have a cold. Only 48.4% of participants usually purchase antibiotics with a prescription. 17.8% of participants stop taking antibiotics when their symptoms improve, and 28.4% of participants sometimes leave the remaining antibiotic at home for use in the next illness. In addition, only 26.7% of participants would advise patients or others about the prudent use of antibiotic or infection control (Figure 2).
 |
Figure 2 Frequency distribution of antibiotic practice among nursing students. |
Univariate Analysis
Table 4 presents the relationships between the demographic and selected features and the levels of KAP on antibiotic use and AMR. Nursing students whose main source of antibiotic knowledge came from the classroom had a relatively higher KAP than students whose main source of antibiotic knowledge did not come from the classroom. Compared with nursing students with an average score of 80 or higher in the last semester, nursing students with an average score of less than 80 in the last semester have lower levels of antibiotic knowledge and practice. Compared with nursing students over 20 years old, nursing students aged 20 years and under have poorer attitudes towards antibiotic use and AMR. The education level of nursing students below undergraduate level only had a significant effect on practice level, whereas it did not have any significant effect on knowledge and attitude level. The nursing students with family members working in the health field had a significant association with practice level. However, nursing students who have used antibiotics in the past 6 months have a lower practice level. On the other hand, the gender, the parental educational level, monthly living expenses, and health status did not have any significant effect on KAP levels.
 |
Table 4 Association of Demographic and Selected Features and KAP Based on Univariate Analysis |
Multivariable Logistic Regression Analysis
Variables with a P-value of <0.05 in univariate analysis were entered into multivariate logistic regression analysis so as to identify the independent factors associated with antibiotic use and AMR KAP levels. The results of multivariable logistic regression analysis are presented in Table 5. In the Knowledge model, the main knowledge sources of antibiotics were outside the classroom (OR = 2.243, 95% CI: 1.313 to 3.829), lack of discussion on AMR in school course (OR =2.699, 95% CI: 1.473 to 4.944), and the average score over 80 points in the last semester (OR =0.418, 95% CI: 0.297 to 0.588) were selected as independent factors associated with knowledge level. Two variables were associated with attitude level among nursing students: age>20 years old (OR = 0.532, 95% CI: 0.329 to 0.860), lack of discussion on AMR in school (OR = 3.533, 95% CI: 1.412 to 8.842). For practice, higher education level (OR = 0.606, 95% CI: 0.446 to 0.825), no use of antibiotic in the past 6 months (OR = 0.499, 95% CI: 0.383 to 0.650), and the average score over 80 points in the last semester (OR = 0.791, 95% CI: 0.628 to 0.995) were independent protective factors while the main knowledge sources of antibiotic were outside the classroom (OR = 1.620, 95% CI: 1.202 to 2.183) and the lack of discussion of AMR in school course (OR = 1.887, 95% CI: 1.374 to 2.591) were independent risk factors. Overall, the results indicated that after adjusting for the confounders, the lack of discussion of AMR in school course was an independent risk factor associated with knowledge, attitude, and practice.
 |
Table 5 Multivariate Logistic Regression Analyses on Factors Associated with KAP |
Discussion
AMR is a serious public health problem threatening human security. Assessment of KAP on antibiotic use and AMR in nursing students can greatly impact how best to tackle the growing threat of the AMR and its related issues in their future professional’s attitudes and practice. This current study, which was a large sample study focusing on pre-internship nursing students, demonstrated that the level of KAP on antibiotic use and AMR was general. Moreover, our study identified certain independent factors associated with KAP on antibiotic use and AMR among Hubei pre-internship nursing students. Our findings might provide some directions for policy guidance and interventions to improve their training in the proper use of antibiotics.
The study showed that nursing students did not score high in knowledge and attitude towards antibiotic use and AMR, indicating that both knowledge and attitudes needed to be improved. Regarding practice, nursing students have some appropriate practices in some items, but still need to improve. Consistent with the study in Nigeria, which pointed out that there was a low level of knowledge among nursing students.24 A previous study also conducted in Nepal found that nursing students exhibit lower levels of attitude. Therefore, it calls for more intervention to align students’ attitudes with their knowledge of using antibiotics,25 in order to equip them with the skills needed to address practical challenges.20 A previous study, which analyzed the level of KAP in the different majors such as nursing and pharmacy, pointed out that the main reasons for the low level of KAP on antibiotic in the nursing major could be the differences in the scope of practice, education background.14 Hence, there is an urgent need to focus more attention and energy on nursing students to improve their KAP on antibiotics.
Studies have shown that there is widespread misunderstanding about the role of antibiotics in the treatment of viral infections.26 In our study, about half of the participants did not know that antibiotics were ineffective against viruses, and only one-third believed antibiotics could not speed up the recovery of common cold. Similar phenomena have been observed among medical students in previous studies in Nigeria and the United Arab Emirates.18,27 The previous research results were consistent, stating that participants used antibiotics as self-medication for treating colds, fever, and pain.28,29 The above results indicate that a large number of nursing students are not aware of the circumstances in which antibiotics need to be used, which may be due to insufficient information on antibiotics obtained by the educated during their school years. Surprisingly, only 32.4% of students know that antimicrobial resistant bacteria can spread from person to person, 50.5% of students know that AMR can spread between bacteria, accompanied by most students who hold the opposite opinion, it indicated that nursing students lack relevant knowledge about the spread of AMR, and it was important to educate them about the basic knowledge of AMR and bacterial transmission. Importantly, in terms of antibiotic identification, the accuracy of three out of four questions is less than 50%. In the field of antibiotic knowledge, respondents’ mastery of antibiotic knowledge is not accurate. Especially in the identification of antibiotics, the scope of treatment, and awareness of AMR. These domains should be addressed as the focus of health education initiatives for nursing students in the future.
Our study indicated that about 61.1% of nursing students were aware of AMR. However, only 36.0% of students agree that there is currently antibiotic abuse, which is lower than the rates reported by medical students in Rwanda (59.8%) and the Democratic Republic of Congo (90%),30,31 suggesting that the concept of AMR should be introduced to nursing students at an early stage. It seems that they believe that AMR is a remote problem, making their attitude towards responsible antibiotic use less optimistic.32 41.6% of students agree that each person receiving antibiotic treatment is at increased risk of antibiotic-resistant infection, and 41.0% of students are concerned that AMR may have an impact on their and their family’s health. These might indicate that most survey subjects are unable to fully understand the harm and severity of drug resistance issues due to the lack of relevant knowledge on the spread and consequences of bacterial resistance. This suggests that nursing students should strengthen their perception of the serious consequences of AMR and the economic burden of health. Fortunately, the majority of respondents in our study had a good attitude and perception on the desire to learn antibiotic related knowledge. They thought that there was currently a lack of sufficient knowledge to use antibiotics appropriately. Moreover, 96.3% of students believe that it is necessary to offer courses on antibiotics. It is hoped that after adequate training of nursing students, they will improve their perception of antibiotic use and AMR, and be able to adopt a positive attitude towards AMR and antimicrobial management and use policies.
In the practice section, students have appropriate practices on some issues. The widespread use of antibiotics for non-therapeutic purposes, such as prevention and growth promotion, has been identified as a strong determinant of the emergence and spread of AMR.33 It is gratifying to note that only a very small number of people in our study will take antibiotics to prevent illness. 75.1% of the nursing students correctly recognized that antibiotic abuse was the main cause of AMR, and 77.8% of the nursing students believed that improper self-medication could cause AMR. Therefore, in our study, only 3% of nursing students self-administer antibiotic before doctors examine, diagnose and prescribe them. Compared to other countries, this lower self-medication rate is appreciative, as 70% of Indian medical students and 89% of Malaysian students were found to self-medicate with antibiotics.34,35 However, some inappropriate practices have also been found among nursing students in our study. 24.4% of nursing students will purchase antibiotics without a prescription. Therefore, strict policies should be put in place to regulate the flow of antibiotics and to prevent the purchase of antibiotics without a doctor’s prescription. About 17% of nursing students reported stopping taking antibiotics when their symptoms improved and keeping the rest of their antibiotics at home for the next time when they got sick, presumably because there were no proper guidelines. Unfortunately, in the aspect of promoting good practice for antibiotic use, less than half of nursing students ask about the effects of antibiotics, the correct method to use them, and the adverse reactions and side effects of antibiotics before using them, which is similar to a previous Chinese study of nursing students.13 In our study, only a fraction of nursing students indicated that they would advise patients or others on the prudent use of antibiotics or infection control. In order to address the issue of AMR, the education of a new generation of healthcare professionals should ensure that medical and health students develop the capabilities to provide effective and safe quality patient care.36 Therefore, we call for tailor-made interventions for nursing students to improve their practice level. Internships could be a good way for nursing students to improve both their attitude level and practice level.37 At present, nursing students are allowed to participate in the hospital internship only in the final year of university in Hubei. Thus, the hospital should focus on training on antibiotic use and AMR on internship nursing students.38 In addition, simulated and actual patient care practices need to be provided in school courses to improve their practice level.39
Our results showed that nursing students who had discussions about AMR in the school course had better KAP, which suggested that medical education had a positive impact. In particular, nursing students with higher average scores had better knowledge and they were also more aware of high-risk practices. Previous studies have emphasized that education on antibiotics and their appropriate use during school training had a significant impact on professional attitudes and behaviors towards antibiotic use, which was more crucial for students majoring in healthcare such as nursing.22 Previous studies have shown that medical students in China are poorly informed about knowledge of antibiotics before they begin clinical practice.40 Medical education training was helpful in improving the level of knowledge on antibiotics and AMR, which was consistent with the fact that nursing students who have discussed AMR in school courses and students whose main knowledge of antibiotics comes from the classroom have a higher level of knowledge in our survey. In addition, targeted antibiotic education, such as the discussion of AMR in school courses and main knowledge of antibiotics coming from the classroom, is likely to have an important role to play in the reduction of injudicious and inappropriate use of antibiotics. This suggests that antibiotic courses and training should be offered in the core courses of medical colleges, and relevant knowledge lectures and discussions should be held to provide rich learning resources for nursing students. Previous studies have shown significant differences between males and females in the use of the antibiotic KAP, with women having better KAP than men.21,41 However, there was no significant association between sex and antibiotic use KAP levels in either univariate analysis or multivariate analyses in this study. We speculated the reason could be the fact that there were fewer male participants in this study because there were only relatively few men engaged in the nurse profession in China. The educational level and age were identified as associated factors influencing KAP on antibiotic use and AMR both in our study and previous study,25,27,42 but the results are inconsistent. Several studies indicated that having a family member working in the health field was associated with a higher level of practice.21,43 However, the family members working in the health field was excluded from the multivariable logistic regression model in our study, although it did have a significant association with high practice level in Univariate analysis, which implied that it might be an important confounder in our study. Therefore, nursing students under the age of 20 and/or those whose main source of knowledge about antibiotics is not in the classroom and/or who lack discussion on AMR in school courses and/or whose average score was below 80 points in the last semester and/or whose low education level should be a priority for educational intervention activities. It is needed to point out that the average score of the last semester here refers to the average score of all courses in the last semester and not all of these courses are related to antibiotics and AMR, implying that it is more necessary to add related courses and specific courses of antibiotics and AMR in nursing professional courses.
The present study has several limitations. First, this was a cross-sectional study, thus it is difficult to ascribe causal associations. Second, there could be a selection bias because of individuals who were unable or unwilling to attend the online survey even though they received the questionnaire link. Third, the use of self-report questionnaires might lead to deviation and/or false information, eg, some responses may have been given to satisfy the investigator, rather than representing a true belief or opinion of the respondent. Besides, recall bias was also inevitable, although this bias should be limited because nursing students were young and the recall period was only the past six months. Fourth, although the questions in this survey were abundant, it still could not adequately capture all aspects of antibiotic use and AMR. Hence, further longitudinal studies need to validate the present findings. Despite these limitations, the present findings provide important information for assessing and improving the knowledge, attitude, and practice of nursing students toward antimicrobial use.
Conclusion
Our findings concluded that KAP levels of antibiotic use and AMR among Hubei nursing students were general and required further strengthening. This study also identified some independent associated factors with KAP on antibiotic use and AMR among nursing students in Hubei province such as the discussion of AMR in school course, main knowledge sources of antibiotic, average score in the last semester, education level and history of using antibiotic in the past 6 months and age, which implied that nursing students with risk factors should have a priority consideration in education intervention. The findings of our study provided some directions for policy guidance and tailored interventions to improve their training in the proper use of antibiotics.
Funding
This work was partly supported by Wuhan Young and Middle-aged Medical Backbone Talent Training Project ([2018]116).
Disclosure
The authors declare there are no conflicts of interest regarding the publication of this paper.
References
1. Hutchings MI, Truman AW, Wilkinson B. Antibiotic: past, present and future. Curr Opin Microbiol. 2019;51:72–80. doi:10.1016/j.mib.2019.10.008
2. Karuniawati H, Hassali MAA, Suryawati S, Ismail WI, Taufik T, Hossain MS. Assessment of knowledge, attitude, and practice of antibiotic use among the population of boyolali, Indonesia: a cross-sectional study. Int J Environ Res Public Health. 2021;18(16):8258. doi:10.3390/ijerph18168258
3. Alawi MM, Darwesh BM. A stepwise introduction of a successful antimicrobial stewardship program. Experience from a tertiary care university hospital in Western, Saudi Arabia. Saudi Med J. 2016;37(12):1350–1358. doi:10.15537/smj.2016.12.15739
4. Min S, Zhou Y, Sun Y, et al. Knowledge, attitude, and practice associated with antimicrobial resistance among medical students between 2017 and 2022: a survey in East China. Front Public Health. 2022;10:1010582. doi:10.3389/fpubh.2022.1010582
5. Duan L, Liu C, Wang D. The general population’s inappropriate behaviors and misunderstanding of antibiotic use in china: a systematic review and meta-analysis. Antibiotic. 2021;10(5):497. doi:10.3390/antibiotics10050497
6. Jairoun A, Hassan N, Ali A, Jairoun O, Shahwan M, Hassali M. University students’ knowledge, attitudes, and practice regarding antibiotic use and associated factors: a cross-sectional study in the United Arab Emirates. Int J Gene Med. 2019;12:235–246. doi:10.2147/IJGM.S200641
7. Sunusi LS, Awad MM, Hassan NM, Isa CA. Assessment of knowledge and attitude toward antibiotic use and resistance among students of International University of Africa, medical complex, Sudan. Glob Drugs Ther. 2019;4:1–6.
8. Lu L, Gao M. Reducing antibiotic overuse in rural China. Lancet Glob Health. 2018;6(4):e375. doi:10.1016/S2214-109X(18)30070-6
9. World Health Organization. Global Action Plan on Antimicrobial Resistance. World Health Organization; 2015.
10. Justo JA, Gauthier TP, Scheetz MH, et al. Knowledge and attitudes of doctor of pharmacy students regarding the appropriate use of antimicrobials. Clinl Infect Dis. 2014;59(suppl_3):S162–S169. doi:10.1093/cid/ciu537
11. Minen MT, Duquaine D, Marx MA, Weiss D. A survey of knowledge, attitudes, and beliefs of medical students concerning antimicrobial use and resistance. Microb Drug Resist. 2010;16(4):285–289. doi:10.1089/mdr.2010.0009
12. Castro-Sánchez E, Gilchrist M, Ahmad R, Courtenay M, Bosanquet J, Holmes AH. Nurse roles in antimicrobial stewardship: lessons from public sectors models of acute care service delivery in the United Kingdom. Antimicrob Resist Infect Control. 2019;8(1):162. doi:10.1186/s13756-019-0621-4
13. Luo Y, Li H, Deng R. Knowledge, attitude and behavior of antibiotic use among nursing students at different educational levels. Guangxi Med. 2019;41(01):141–145.
14. Seid MA, Hussen MS. Knowledge and attitude towards antimicrobial resistance among final year undergraduate paramedical students at University of Gondar, Ethiopia. BMC Infect Dis. 2018;18(1):312. doi:10.1186/s12879-018-3199-1
15. Sadasivam K, Chinnasami B, Ramraj B, Karthick NG, Saravanan A. Knowledge, attitude and practice of paramedical staff towards antibiotic usage and its resistance. Biomed Pharmacol J. 2016;9(1):337–343. doi:10.13005/bpj/944
16. RaoSoft® sample size calculator; 2004. Available from: http://www.raosoft.com/samplesize.html.
17. Sakr S, Ghaddar A, Hamam B, Sheet I. Antibiotic use and resistance: an unprecedented assessment of university students’ knowledge, attitude and practices (KAP) in Lebanon. BMC Public Health. 2020;20(1):535. doi:10.1186/s12889-020-08676-8
18. Jairoun A, Hassan N, Ali A, Jairoun O, Shahwan M. Knowledge, attitude and practice of antibiotic use among university students: a cross sectional study in UAE. BMC Public Health. 2019;19(1):518. doi:10.1186/s12889-019-6878-y
19. Higuita-Gutiérrez LF, Roncancio Villamil GE, Jiménez Quiceno JN. Knowledge, attitude, and practice regarding antibiotic use and resistance among medical students in Colombia: a cross-sectional descriptive study. BMC Public Health. 2020;20(1):1861. doi:10.1186/s12889-020-09971-0
20. Al-Taani GM, Karasneh RA, Al-Azzam S, et al. Knowledge, attitude, and behavior about antimicrobial use and resistance among medical, nursing and pharmacy students in Jordan: a cross sectional study. Antibiotic. 2022;11:11.
21. Scaioli G, Gualano MR, Gili R, Masucci S, Bert F, Siliquini R. Antibiotic use: a cross-sectional survey assessing the knowledge, attitudes and practices amongst students of a school of medicine in Italy. PLoS One. 2015;10(4):e0122476. doi:10.1371/journal.pone.0122476
22. Sakeena MHF, Bennett AA, Jamshed S, et al. Investigating knowledge regarding antibiotics and antimicrobial resistance among pharmacy students in Sri Lankan universities. BMC Infect Dis. 2018;18(1):209. doi:10.1186/s12879-018-3107-8
23. World Health Organization. Antibiotic Resistance: Multi-Country Public Awareness Survey. Geneva: World Health Organization; 2015.
24. Akande-Sholabi W, Ajamu AT. Antimicrobial stewardship: assessment of knowledge, awareness of antimicrobial resistance and appropriate antibiotic use among healthcare students in a Nigerian University. BMC Med Educ. 2021;21(1):488. doi:10.1186/s12909-021-02912-4
25. Shah P, Shrestha R, Mao Z, et al. Knowledge, attitude, and practice associated with antibiotic use among university students: a survey in Nepal. Int J Environ Res Public Health. 2019;16(20):3996. doi:10.3390/ijerph16203996
26. Mo Y, Seah I, Lye PSP, et al. Relating knowledge, attitude and practice of antibiotic use to extended-spectrum beta-lactamase-producing Enterobacteriaceae carriage: results of a cross-sectional community survey. BMJ open. 2019;9(3):e023859. doi:10.1136/bmjopen-2018-023859
27. Odetokun IA, Akpabio U, Alhaji NB, et al. Knowledge of antimicrobial resistance among veterinary students and their personal antibiotic use practices: a national cross-sectional survey. Antibiotics. 2019;8(4):243. doi:10.3390/antibiotics8040243
28. Shehadeh M, Suaifan G, Darwish RM, Wazaify M, Zaru L, Alja’fari S. Knowledge, attitudes and behavior regarding antibiotics use and misuse among adults in the community of Jordan. A pilot study. Saudi Pharm J. 2012;20(2):125–133. doi:10.1016/j.jsps.2011.11.005
29. Karuniawati H, Hassali MAA, Suryawati S, Ismail WI, Taufik T, Wiladatika A. Public practices towards antibiotics: a qualitative study. Clin Epidemiol Global Health. 2020;8(4):1277–1281. doi:10.1016/j.cegh.2020.04.027
30. Thriemer K, Katuala Y, Batoko B, et al. Antibiotic prescribing in DR Congo: a knowledge, attitude and practice survey among medical doctors and students. PLoS One. 2013;8(2):e55495. doi:10.1371/journal.pone.0055495
31. Nisabwe L, Brice H, Umuhire MC, et al. Knowledge and attitudes towards antibiotic use and resistance among undergraduate healthcare students at University of Rwanda. J Pharm Pol Pract. 2020;13(1):7. doi:10.1186/s40545-020-00207-5
32. Nogueira-Uzal N, Zapata-Cachafeiro M, Vázquez-Cancela O, López-Durán A, Herdeiro MT, Figueiras A. Does the problem begin at the beginning? Medical students’ knowledge and beliefs regarding antibiotics and resistance: a systematic review. Antimicrob Resist Infect Control. 2020;9(1):172. doi:10.1186/s13756-020-00837-z
33. Ayukekbong JA, Ntemgwa M, Atabe AN. The threat of antimicrobial resistance in developing countries: causes and control strategies. Antimicrob Resist Infect Control. 2017;6(1):47. doi:10.1186/s13756-017-0208-x
34. Haque M, Rahman NAA, McKimm J, et al. Self-medication of antibiotics: investigating practice among university students at the Malaysian National Defence University. Infect Drug Resist. 2019;12:1333–1351. doi:10.2147/IDR.S203364
35. Lomi M, Jimsha V, Srinivasan S, Daniel MJ, Territory U. Assessment of knowledge, attitude and practice of antibiotic usage amongst undergraduate, intern and postgraduate dental students-a questionnaire based study. Int J Sci Healthcare Res. 2019;4:136–142.
36. Gruppen LD, Mangrulkar RS, Kolars JC. The promise of competency-based education in the health professions for improving global health. Hum Res Health. 2012;10(1):43. doi:10.1186/1478-4491-10-43
37. Nayak S, Rana MJ, Mayya SS, et al. Antibiotics to cure or harm: concept of antibiotic resistance among health professional students in Nepal. Int J Med Sci Public Health. 2016;5(12):2512–2517. doi:10.5455/ijmsph.2016.14052016515
38. Khan FU, Khan A, Shah S, et al. Exploring undergraduate pharmacy students perspectives towards antibiotics use, antibiotic resistance, and antibiotic stewardship programs along with the pharmacy teachers’ perspectives: a mixed-methods study from Pakistan. Front Pharmacol. 2021;12:754000. doi:10.3389/fphar.2021.754000
39. Courteille O, Fahlstedt M, Ho J, et al. Learning through a virtual patient vs. recorded lecture: a comparison of knowledge retention in a trauma case. Int J Med Educ. 2018;9:86–92. doi:10.5116/ijme.5aa3.ccf2
40. Hu Y, Wang X, Tucker JD, et al. Knowledge, attitude, and practice with respect to antibiotic use among Chinese medical students: a multicentre cross-sectional study. Int J Environ Res Public Health. 2018;15(6):1165. doi:10.3390/ijerph15061165
41. Assar A, Abdelraoof MI, Abdel-Maboud M, et al. Knowledge, attitudes, and practices of Egypt’s future physicians towards antimicrobial resistance (KAP-AMR study): a multicenter cross-sectional study. Environ Sci Pollut Res Int. 2020;27(17):21292–21298. doi:10.1007/s11356-020-08534-5
42. Huang Y, Gu J, Zhang M, et al. Knowledge, attitude and practice of antibiotics: a questionnaire study among 2500 Chinese students. BMC Med Educ. 2013;13(1):163. doi:10.1186/1472-6920-13-163
43. Gendel MH, Brooks E, Early SR, et al. Self-prescribed and other informal care provided by physicians: scope, correlations and implications. J Med Ethics. 2012;38(5):294–298. doi:10.1136/medethics-2011-100167
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.