Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
Knowledge, Attitude and Associated Factors of Monkeypox Infection Among Healthcare Workers in Injibara General Hospital, Northwest Ethiopia
Authors Aynalem ZB , Abate MD , Meseret F , Muhamed AN , Abebe GK , Adal AB , Wondmieneh A , Andualem A , Ademe S , Workye H , Bewket B , Beyene GA, Alene T, Tsega TD
Received 13 December 2023
Accepted for publication 1 March 2024
Published 15 March 2024 Volume 2024:17 Pages 1159—1173
DOI https://doi.org/10.2147/JMDH.S454828
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Zewdu Bishaw Aynalem,1 Melsew Dagne Abate,1 Fentahun Meseret,2 Ahmed Nuru Muhamed,3 Gebremeskel Kibret Abebe,4 Abebaw Bires Adal,1 Adam Wondmieneh,1 Atsedemariam Andualem,1 Sewunet Ademe,1 Haile Workye,1 Bekalu Bewket,1 Getachew Amare Beyene,5 Tamiru Alene,6 Tilahun Degu Tsega7
1Department of Nursing, College of Medicine and Health Sciences, Injibara University, Injibara, Ethiopia; 2Department of Pediatrics and Child Health Nursing, School of Nursing and Midwifery, College of Health and Medical Science, Haramaya University, Harar, Ethiopia; 3Department of Nursing, College of Medicine and Health Science, Wolkite University, Wolkite, Ethiopia; 4Department of Emergency and Critical Care Nursing, School of Nursing, College of Health Sciences, Woldia University, Woldia, Ethiopia; 5Department of Midwifery, College of Medicine and Health Sciences, Injibara University, Injibara, Ethiopia; 6Department of Pediatrics and Child Health Nursing, College of Medicine and Health Sciences, Injibara University, Injibara, Ethiopia; 7Department of Public Health, College of Medicine and Health Sciences, Injibara University, Injibara, Ethiopia
Correspondence: Zewdu Bishaw Aynalem, Department of Nursing, College of Medicine and Health Sciences, Injibara University, Injibara, Ethiopia, Tel +251918375722, Email [email protected]; [email protected]
Background: Fighting health threats, especially the rise of new infectious diseases, is one of the main responsibilities of healthcare workers. However, their knowledge and attitudes toward monkeypox have not yet been assessed. Therefore, this study aimed to assess the knowledge, attitude, and factors associated with monkeypox infection among healthcare workers at Injibara General Hospital, Northwest Ethiopia.
Methods: Institution-based cross-sectional study was conducted from December 1– 30, 2022. Data were collected using a structured self-administered questionnaire. A simple random sampling technique was used to select study participants. Descriptive statistics and multivariable logistic regression analyses were computed. The degree of association was interpreted using an odds ratio with a 95% confidence interval and a p-value < 0.05.
Results: Among the 200 healthcare workers who participated, 38.5% (95% CI: 32.5%– 45%) and 62% (95% CI: 55– 68.5%) had good knowledge and positive attitudes regarding monkeypox respectively. Having a master’s degree or above (AOR = 11.25: 95% CI: 2.03– 62.33), being vaccinated against COVID-19 (AOR = 2.60: 95% CI: 1.37– 4.94), and having access to information about monkeypox (AOR = 3.37: 95% CI: 1.33– 8.50) were the factors associated with good knowledge. Furthermore, a positive attitude was significantly associated with being 30 years of age or older (AOR = 2.95: 95% CI: 1.55– 5.60) and having access to information about monkeypox (AOR = 4.14: 95% CI: 2.06, 8.30).
Conclusion: Both good knowledge and positive attitudes were relatively low among healthcare workers. Factors such as age, education level, COVID-19 vaccination status, and access to information about monkeypox were significantly associated with the knowledge and attitude of healthcare workers. To enhance the knowledge and attitude of healthcare workers, hospitals should consider offering educational upgrades, hosting educational events like seminars, conferences, webinars, and campaigns, and ensuring comprehensive coverage of the topic in medical curricula.
Keywords: monkeypox, mpox, knowledge, attitude, associated factors, healthcare worker, Ethiopia, Injibara
Introduction
Monkeypox (mpox) is a contagious illness brought by the monkeypox virus, a double-stranded DNA virus. This virus is part of the Poxviridae family and belongs to the Orthopoxvirus genus, which also encompasses the chickenpox virus and can transmit from animals to humans causing an infection called human mpox.1–4 The discovery of the mpox virus dates to 1958 when it was initially identified during an outbreak in Macaca fascicularis, which occurred during a polio vaccine trial at a laboratory in Copenhagen, Denmark.5
The first case of mpox was reported in 1970 in the Democratic Republic of the Congo (DRC), affecting a 9-month-old infant.6 Since then, it remained prevalent in Western and Central Africa,7 where a total of 59 cases were reported between 1970 and 1980 in countries such as Liberia, Nigeria, Sierra Leone, Cameroon, and Cote d’Ivoire.8,9 As of 21 May 2022, 92 cases of human mpox have been reported from 13 non-endemic countries including Australia, Belgium, Canada, France, Germany, Italy, Netherlands, Portugal, Spain, Sweden, UK, and the USA.10 Unexpectedly, when confirmed cases were asked about their travel history, they were more likely to report having been to Europe and North America rather than West or Central Africa, where the mpox virus is usually more prevalent.11,12 In response to these occurrences, the World Health Organization declared the mpox virus as a public health emergency in July 2022.13 By October 31, 2023, the pandemic had spread to 116 countries, with a total of 91,788 confirmed cases and 167 deaths.14
Monkeypox virus can be transmitted through both the animal-human and human-human pathways,15 with close contact with infected animals or individuals,16,17 as well as being in regions with outbreaks, increasing the risk of infection.18,19 The symptoms of mpox are similar to smallpox, including fever, headache, back pain, muscle pain, and skin rashes. However, mpox is generally less severe and results in lymphadenopathy, unlike smallpox.20 The case fatality rate varies depending on the clade of the virus,21 ranging from 1% for the West African clade (Clade II) to 11% for the Congo Basin clade (Clade I).22 In resource-limited settings, the fatality rate can be as high as 17%,23 falling between the mortality rates of variola minor (1%) and variola major (30%).24 Diagnosing mpox is challenging due to overlapping symptoms with other orthopoxviruses,25 limited availability of lab tests, and varying accuracy of current diagnostic tests.26 Treatment primarily focuses on managing symptoms and providing supportive care through the use of antiviral drugs, pain relievers, and fluids to prevent dehydration.26–28 Prevention measures include smallpox vaccination,29 practicing good hygiene, avoiding contact with infected individuals, isolation and quarantine, and using personal protective equipment.30,31 Effective contact tracing, early detection, and robust surveillance are also imperative in controlling mpox spread.31
Mpox poses a significant public health concern, particularly in regions of Africa. Healthcare workers (HCWs) indeed have a crucial role in combating and managing outbreaks of mpox.32,33 Several studies have assessed the level of knowledge among health workers regarding mpox. A study from Italy indicated that the knowledge status of Italian healthcare workers was quite unsatisfying, with substantial knowledge gaps towards mpox.34 In a study conducted in Bangladesh, only 30.59%,35 Indonesia, only 10%,36 Pakistan, only 34.4%,37 Turkey,38 only 32.5%, Nigeria39 only 37.8% of HCWs had good knowledge regarding the clinical presentation, transmission, and prevention of mpox. Similarly, a study in Lebanon reported low knowledge levels about mpox diagnosis and management among health workers where 33.7% of those surveyed had a good knowledge of mpox.40 In the same vein, a study done in Bangladesh revealed that almost two-thirds of the respondents had insufficient knowledge about the transmission pathways and the signs and symptoms of mpox.41 This lack of knowledge may hinder early diagnosis and appropriate management of mpox cases, leading to delayed intervention and increased risk of transmission.42–44
Health workers’ attitudes towards mpox can significantly influence their effectiveness in managing the disease and limiting its spread.45,46 Studies conducted in various countries have reported mixed attitudes among health workers. Some health workers demonstrated a positive attitude35,47 displaying a willingness to care for mpox patients and adherence to infection prevention and control measures.27,37 However, other studies reported negative attitudes, such as fear, stigmatization,48–50 and refusal to care for mpox patients.51 Satisfactory attitude towards mpox was observed in less than a third (30.7%) of Lebanon healthcare workers.40 Additionally, Nepalese healthcare workers still have a negative attitude regarding its control measures.52 This negative attitude may result from a lack of confidence,53 concerns about infection prevention safety,54,55 or limited resources.56,57 Moreover, HCWs knowledge and attitude towards mpox can be affected by years of working experience,58 level of education, and having access to information about mpox.35,37,59,60 The above literature provides evidence of gaps in knowledge and attitudes among health workers regarding mpox infection. Addressing these gaps is crucial for improving the response to mpox outbreaks.
Although there have not been any reports of mpox in Ethiopia, HCWs need to be knowledgeable about and ready for cases of mpox because Ethiopia is one of Africa’s most popular tourist destinations,61 making it more vulnerable to human mpox importation. The recent surge in mpox cases in humans requires prevention, early detection, prompt response and management by healthcare providers however, no research has been conducted in Ethiopia to assess their knowledge and attitude towards mpox. This provides an excellent opportunity to understand their knowledge gaps and attitudes toward mpox and enables relevant organizations to develop targeted training programs and interventions to address any gaps. Furthermore, by conducting such a study, we can ensure healthcare workers are well-equipped to effectively manage and combat the potential spread of mpox, ultimately protecting public health. Furthermore, the results would be extremely helpful for decision-makers and any future researchers by providing insights on this issue. Therefore, this study aimed to assess knowledge, attitude, and associated factors of mpox infection among HCWs working at Injibara General Hospital, Northwest Ethiopia.
Methods
Study Design, Period and Setup
An institution-based cross-sectional study was conducted from December 1–30, 2022 among healthcare workers working in Injibara General Hospital (IGH), Northwest Ethiopia. The hospital is located in Injibara town, which is 114 and 450 kilometers from Bahir Dar (the capital city of Amhara region) and Addis Ababa, the capital city of Ethiopia, respectively. This hospital provides outpatient and inpatient services for more than 1.2 million populations62 and in its catchment area there are 46 health centers and 4 district hospitals. In this hospital, there are a total of 317 healthcare workers.
Source and Study Population
All healthcare workers working at Injibara General Hospital and sampled medical doctors, nurses, midwives, and other allied health professionals who were directly involved in the provision of healthcare service during the data-collection period were the source and study populations, respectively.
Inclusion and Exclusion Criteria
The study included healthcare workers who met the following criteria: they were 18 years or older, had a minimum work experience of six months, were directly involved in delivering medical care or services to patients, and willingly volunteered to participate. However, HCWs who were on sick leave, annual leave, or maternity leave, as well as those in managerial positions during the data collection period, were excluded from the study.
Sample Size and Sampling Procedure
The sample size was determined using a single population proportion formula with the assumption of 50% proportion (since no previous study was done in Ethiopia on this issue), 95% confidence level, and 5% margin of error. Given that the source population was less than 10,000, a correction formula was used and a 15% nonresponse rate was added, making the final sample size 201. The hospital’s human resource management office gave us the list of HCWs employed there, which was then used as a sample frame. A simple random sampling technique was used to select the study participants.
Data Collection Tools and Procedures
Data were collected using a structured self-administered questionnaire. The data collection tool was adapted from previous studies.35,36,45,63 Previous studies have demonstrated that the tool is valid and reliable,63 with an internal consistency (Cronbach’s alpha value) of 0.86,45 indicating a high reliability. Additionally, the content validity of the instrument was reviewed by two infectious and communicable disease professionals. The tool addressed the following sections: Socio-demographic characteristics of the participants, mpox knowledge and attitude questions. There were 23 questions in the knowledge part and 10 questions in the attitude section. For the knowledge domain, correct answers received a score of 1, and incorrect answers received a score of zero. The scores were added together to give a total knowledge score that ranges from 0 to 23, where a higher score indicates better knowledge. Regarding attitude, the questions were scored on a 3-point Likert scale (disagree, have no opinion, and agree). The responses were given as 1 for disagree, 2 for have no opinion, and 3 for agree. Scores were added to give an overall score of 10–30, where a higher score indicates a more positive attitude toward the mpox preventive measures. Monkeypox knowledge and attitude scores were categorized according to the mean values. Healthcare workers who scored above the mean value of 13.05 were considered to have good knowledge, while those who scored below or equal to the mean were considered to have poor knowledge. Similarly, healthcare workers who scored above the mean value of 24.18 were considered to have a positive attitude, while those who scored below or equal to the mean were considered to have a negative attitude. To ensure consistency with positively written statements, negative questions were reverse-scored. Supplemental file 1 provided the detailed question used to assess healthcare workers’ knowledge and attitudes.
Operational Definition
Healthcare Workers
Any member of the healthcare team, such as doctors, nurses, midwives, pharmacists, laboratory professionals, or any other person directly involved in delivering medical care or services to patients as part of their professional duties.64
Good Knowledge
If the healthcare worker answers above the mean value of the knowledge question.
Poor Knowledge
If the healthcare worker answers below or equal to the mean value of the knowledge question.
Positive Attitude
If the healthcare worker answers above the mean value of the attitude question.
Negative Attitude
If the healthcare worker answers below or equal to the mean value of the attitude question.
Data Quality Control
The tool was pretested with 10% of Finoteselam general hospital healthcare workers to assess its understandability, flow, and consistency. Some adjustments, such as wording revisions were made based on the results obtained from it. Data was collected by a day-trained two data collectors and one supervisor. Data completeness and consistency were checked by the supervisor and investigators. The principal investigator and supervisor conducted day-to-day follow-ups during the whole period of data collection. Each questionnaire was checked for completeness by the supervisor and the principal investigators on each day as soon as possible and necessary feedback was given to data collectors before leaving the data collection site. The overall activities of the study were managed by the principal investigator and co-investigators.
Data Processing and Analysis
The collected data were checked and reviewed for completeness, coded, cleaned, edited, and entered into Epi-info version 7 and exported to SPSS version 25 for analysis. Descriptive statistics and summary measures were computed. The data were presented using texts, tables, and figures. The binary logistic regression model was used to determine the factors associated with the knowledge and attitude of healthcare workers regarding mpox infection. Variables having a p-value of less than 0.25 in the bi-variable logistic regression analysis were included into a multivariable logistic regression analysis to account for potential confounding variables. The backward likelihood ratio method was used to select the variables in multivariable logistic regression analysis. Multicollinearity was checked to see the correlation among the independent variables by using the variance inflation factor and no collinearity exists between them. Model fitness was checked using the Hosmer-Lemeshow test and found p values of 0.83 and 0.42 for mpox knowledge and attitude domains, respectively. The degree of association was interpreted using an odds ratio with a 95% confidence interval and a p-value of less than 0.05.
Ethical Considerations
The research Ethics Review Committee at College of Medicine and Health Sciences, Injibara University (Ref # IUCMHS 325/10) approved the study. This study was conducted in accordance with the Declaration of Helsinki. The purpose of the study, procedure, time required, data management, and the rights of the participants were explained in full. Informed consent is obtained from all the participants. To safeguard their privacy, no personal identifying information was collected. Participation was entirely voluntary and their confidentiality was ensured through anonymous coding and analysis of the collected data.
Results
Socio-Demographic Characteristics of the Study Participants
A total of 200 healthcare workers have completed the questionnaire with a response rate of 99.5%. The majority of the study participants were males (56%), under 30 years old (52%), married (65.5%), degree holders in educational status (77%), and their mean age was 29.5 (SD ± 4.2) years. Nurses were the most responding professionals (48.5%). Healthcare workers said that social media (65%) was where they got the most about mpox, followed by radio and television (36%), their coworkers (22%), and medical books or during studying (12%). The socio-demographic and other general characteristics of the respondents are shown in Table 1.
 |
Table 1 General Characteristics of Healthcare Workers Working at Injibara General Hospital, Northwest Ethiopia, 2022 (n = 200) |
Knowledge of HCWs About Human Monkeypox
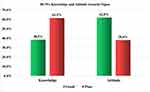
Of the surveyed healthcare workers, 38.5% (95% CI: 32.5–45%) of them had good knowledge about human mpox (Figure 1). According to the findings, 55.5% of respondents correctly identified that mpox is a viral disease. About 61% of them were aware that mpox can be spread from person to person, however, 40.5% of them were unaware that human mpox causes flu-like symptoms including fever, chills, cough, runny nose, fatigue, headache, muscle and backache (Table 2).
 |
Table 2 Healthcare Workers’ Responses to Knowledge Questions About Human Mpox in Injibara General Hospital, Northwest Ethiopia, 2022 (n = 200) |
Factors Associated with Knowledge of Monkeypox
Factors like age, gender, marital status, level of education, work experience, profession type, history of COVID-19 infection, contact history with COVID-19 infected people, being vaccinated against COVID-19, having a known chronic medical illness and having access to information about mpox either in the medical curriculum or social media or coworkers or television and radio were entered into the bivariable logistic regression analysis model. After adjustment, the level of education, being vaccinated against COVID-19, and having access to information about mpox were significantly associated with good knowledge.
Healthcare workers having master’s and above in education were eleven times (AOR = 11.25: 95% CI: 2.03–62.33) more likely to have good knowledge than those who have diplomas. The odds of having good mpox knowledge were 2.6 times higher among healthcare workers who received COVID-19 vaccine (AOR = 2.60: 95% CI: 1.37–4.94) than those who did not take it. Likewise, healthcare workers who had access to information about mpox either in the medical curriculum or social media or coworkers were nearly 3.4 times (AOR = 3.37: 95% CI: 1.33–8.50) more likely to have good knowledge than their counterparts (Table 3).
 |
Table 3 Binary Logistic Regression Analyses for Factors Associated with Mpox Knowledge Among HCWs in Injibara General Hospital, Northwest Ethiopia, 2022 (n = 200) |
Attitude of HCWs Towards Human Monkeypox
About 62% (95% CI: 55–68.5%) of healthcare workers had a positive attitude toward monkeypox prevention (Figure 1). Based on the findings, the majority (80.5%) of the study participants wanted to learn more about monkeypox. Around 62.5% of the participants agreed that traveling to monkeypox epidemic countries is risky and should be limited, and 65.5% of them agreed that this infection can add a new burden on the healthcare system (Figure 2).
Factors Associated with Attitude Toward Monkeypox
Age, sex, marital status, educational level, work experience, profession type, history of COVID-19 infection, contact history with COVID-19 infected people, being vaccinated against COVID-19 vaccine, having a known chronic medical illness, having mpox information access and mpox knowledge were entered into the bivariable logistic regression analysis. Accordingly, participants’ age and mpox information were found to be statistically significant with mpox attitude after adjusting for confounders.
According to the results of multivariable logistic regression analysis, healthcare workers who are 30 years or older were almost 3 times (AOR = 2.95: 95% CI: 1.55–5.60) more likely to have a positive mpox attitude than those who are under 30 years old. Those who had access to mpox information were nearly 4.1 times (AOR = 4.14: 95% CI: 2.06, 8.30) more likely to have positive attitudes than those who had not (Table 4).
 |
Table 4 Binary Logistic Regression Analyses for Factors Associated with Mpox Attitude Among HCWs in Injibara General Hospital, Northwest Ethiopia, 2022 (n = 200) |
Discussion
Healthcare workers play a vital role in both preventing and treating emerging diseases.65 Their ability to effectively respond to these diseases is dependent on their knowledge and attitudes.32,33,66 As study, being the first of its kind in Ethiopia, aimed to assess the knowledge, attitude, and factors associated with monkeypox infection among healthcare workers.
Only 38.5% (95% CI: 32.5–45%) of healthcare workers in this study had good knowledge of mpox. The finding was in line with the studies from Indonesia,36 Pakistan,37 Turkey,38 Lebanon,40 and Nigeria39 where 36.5%, 34.4%, 32.5%, 33.7%, and 37.8% of the healthcare workers had good knowledge about mpox respectively. In a similar vein, a study done on the Lebanese general population showed that 33.04% of those surveyed had a good knowledge of mpox.60 However, this finding is lower than the results found in other studies, that 55.5% of physicians in Saudi Arabia had good knowledge,63 64.9% of healthcare workers in Algeria had medium knowledge,67 60.5% of participants in Nigeria having sufficient knowledge,68 and 91.1% of medical workers in China being knowledgeable about mpox.69
Moreover, this finding was in contrast with the general population results in Nepal where 53.8% of the study participants had good knowledge;70 in Saudi Arabia, 48% of the total participants had high knowledge;71 in Nigeria, 58.7% had good knowledge;72 in China, 56.5% had a high level of knowledge;73 in Malaysia, 49.3% of medical students had good mpox knowledge;74 in Bangladesh, 30.59% medical doctors had good knowledge;35 55.3% of medical students from 27 low and high-income countries75 and 26% global healthcare workers had good mpox knowledge.44 Differences in the study setting, study period, perceptions about mpox infection, source of information, and taking of training could all be contributing factors to this discrepancy. The fact that mpox infection is not endemic and has not yet been reported in Ethiopia may also be a contributing factor to HCWs’ low level of knowledge.
In this study, the odds of having good mpox knowledge were 11 times higher among healthcare workers having master’s and above in education than those who have diplomas. Other studies in Bangladesh,41 Lebanon,60 China59 and Nigeria68 also revealed that a greater level of education was related to having good knowledge. The reason could be thought that education plays an important part in helping people adopt healthier habits and tackling epidemics because it increases awareness of health-related issues.37 Moreover, individuals with a higher level of education frequently have higher-paying jobs and have access to authoritative information from scientists and other experts.60 Additionally, healthcare workers who fall under this category are more likely to study scientific research papers, engage in publications, participate in recent appropriate training and education programs, and improve their knowledge and skills through frequent reading.71 Furthermore, education leads to improved information-gathering habits and effective media input utilization for the prevention and treatment of mpox.76
The multivariable logistic regression analysis found a significant association between healthcare workers’ knowledge scores and having information access about mpox. Healthcare workers who had mpox information either in the medical curriculum or social media or coworkers were nearly 3.4 times more likely to have good knowledge than their counterparts. Findings from Bangladesh35 and the Kurdistan Region of Iraq43 indicate that healthcare workers who had information about mpox before 2022 had higher levels of knowledge, which is consistent with this finding. Indeed, this finding is not surprising given that healthcare workers who were exposed to information about mpox had a better degree of awareness than those who were not. This is because HCWs can receive up-to-date information about its transmission, symptoms, prevention, and treatment options.
Likewise, mpox knowledge was significantly associated with being vaccinated against COVID-19. Healthcare workers who took COVID-19 Vaccine were 2.6 times more likely to have good knowledge about mpox than those who did not take it. This finding is supported by a study done in Lebanon which seemed to be connected to their level of awareness with knowing more about the vaccine was considered as a sign that someone was better informed.77 Again, it could be linked to the notion that COVID-19 has given healthcare workers a plethora of knowledge that could be applied to help stop the spread of mpox.78 Once more, healthcare workers who received the COVID-19 vaccine might be highly motivated to remain informed about mpox.
This study revealed that 62% (95% CI: 55.0–68.5%) of the participants had a positive attitude towards mpox prevention which was lower than the finding in Bangladesh (84.83%).35 Compared with studies conducted outside of Ethiopia, our finding was higher than a study conducted by Jamil et al,37 Sahin et al,38 Malaeb et al,40 Jahromi et al,44 Das et al52 and León-Figueroa et al79 revealing low levels of positive attitude regarding mpox preventive practices with 41.7%, 41.7%, 30.7%, 34.6% 51.1% and 40% of healthcare workers exhibited a positive attitude towards it respectively. The discrepancy may be attributed to the differences in the cut values to measure positive and negative attitude levels, sample sizes, study design, population, and study settings. Moreover, the reason HCWs involved in our study had a good attitude could be that they had already experienced some of the hard times that came with the COVID-19 pandemic and were aware of how severe it is and they were open to learning more about the virus.
In this study, age was found to be significantly associated with mpox attitude. Healthcare workers who are 30 years or older were almost 3 times more likely to have positive mpox attitudes than those who are under 30 years old. This finding is in line with a study from Bangladesh.35 This could be because as people get older, they will have a higher level of education which is a predictor of good knowledge in this study, increase their depth of understanding, and gain more experience, which allows them to be more open-minded and positive.
Moreover, when compared to healthcare workers who had no access to mpox-related information, those who had access were nearly 4.1 times more likely to have a positive mpox attitude. This is congruent with a cross-sectional study conducted in 27 different countries on three continents that found receiving information about mpox through social media or scientific websites was a predictor for positive attitude.75 This may be explained by the fact that people who received information about mpox via sources such as their medical curriculum, social media, friends, television, and radio are more likely to become aware of the disease’s effects and health consequences. This would compel them to be more positive about its preventive measures.
Strengths and Limitations
This study is the first of its kind in Ethiopia to assess knowledge, attitudes, and factors associated to mpox infection among healthcare workers. The study found significant gaps in both knowledge and attitude among study participants. Such findings have important implications for program managers looking to implement effective interventions in the field and offer valuable insights for future researchers. However, certain limitations should be noted when interpreting the findings. Firstly, the study had a relatively small sample size and was conducted at a single center, potentially limiting the generalizability to all Ethiopian healthcare workers. Secondly, the use of self-reported questionnaires may introduce bias, although the anonymity of the questionnaire may have mitigated this. Thirdly, the study did not compare knowledge and attitudes across different types of healthcare workers involved. Additionally, the cross-sectional design of the study presents another limitation. Furthermore, qualitative studies should be conducted to gain a better, broader, and more integrative understanding regarding the knowledge and attitude of healthcare workers in Ethiopia in association with mpox.
Conclusions
The prevalence of both good knowledge and positive attitudes among healthcare workers was relatively low. Factors such as age, level of education, being vaccinated against COVID-19, and having information access about mpox had a significant association with the knowledge and attitude of healthcare workers. Hospitals could improve their healthcare workers’ knowledge and attitudes by providing opportunities to upgrade their educational level, organizing seminars, conferences, webinars, and campaigns, and ensuring that the medical curriculum fully covers this topic.
Data Sharing Statement
Data are available from the corresponding author upon reasonable request.
Ethical Approval
This study was approved by the College of Medicine and Health Sciences Research Ethics Review Committee at Injibara University (Ref # IUCMHS 325/10).
Acknowledgments
The authors would like to thank Injibara University’s Health Science College Ethical Review Committee for their approval. As well, we want to extend our heartfelt thanks to the supervisors, data collectors, study participants, and Injibara General Hospital for their collaboration and help during the data collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is, in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest related to this study.
References
1. World Health Organization. WHO Informal Consultation on Monkeypox 2017. Geneva, Switzerland; 2017.
2. Bunge EM, Hoet B, Chen L, et al. The changing epidemiology of human monkeypox—A potential threat? A systematic review. PLoS Negl Trop Dis. 2022;16(2):e0010141. doi:10.1371/journal.pntd.0010141
3. León-Figueroa DA, Bonilla-Aldana DK, Pachar M, et al. The never-ending global emergence of viral zoonoses after COVID-19? The rising concern of monkeypox in Europe, North America and beyond. Travel Med Infectious Dis. 2022;49:102362. doi:10.1016/j.tmaid.2022.102362
4. Mileto D, Riva A, Cutrera M, et al. New challenges in human monkeypox outside Africa: a review and case report from Italy. Travel Med Infectious Dis;2022. 102386. doi:10.1016/j.tmaid.2022.102386
5. Parker S, Buller RM. A review of experimental and natural infections of animals with monkeypox virus between 1958 and 2012. Future Virol. 2013;8(2):129–157. doi:10.2217/fvl.12.130
6. Ladnyj I, Ziegler P, Kima E. A human infection caused by monkeypox virus in Basankusu Territory, Democratic Republic of the Congo. Bulletin of the World Health Organization. 1972;46(5):593.
7. Durski KN, McCollum AM, Nakazawa Y, et al. Emergence of Monkeypox — west and Central Africa, 1970–2017. Morb Mort Week Rep. 2018;67(10):306. doi:10.15585/mmwr.mm6710a5
8. Foster SO, Brink EW, Hutchins DL, et al. Human monkeypox. Bulletin of the World Health Organization. 1972;46(5):569.
9. Heymann DL, Szczeniowski M, Esteves K. Re-emergence of monkeypox in Africa: a review of the past six years. Br Med Bul. 1998;54(3):693–702. doi:10.1093/oxfordjournals.bmb.a011720
10. Multi-country monkeypox outbreak in non-endemic countries. (n.d.). Who.Int. Available from: https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON385.
11. World Health Organization. Monkeypox outbreak - Global. Available from: https://www.who.int/emergencies/situations/monkeypox-oubreak-2022.
12. Xiang Y, White A. Monkeypox virus emerges from the shadow of its more infamous cousin: family biology matters. Emerg Microb Inf. 2022;11(1):1768–1777. doi:10.1080/22221751.2022.2095309
13. Lin GSS, Tan WW, Chan DZK, Ooi KS, Hashim H. Monkeypox awareness, knowledge, and attitude among undergraduate preclinical and clinical students at a Malaysian dental school: an emerging outbreak during the COVID-19 era. Asian Pac J Trop Med. 2022;15(10):461. doi:10.4103/1995-7645.359787
14. Worled Health Organization. Monkeypox Outbreak: global Trends. Available from: https://worldhealthorg.shinyapps.io/mpx_global/.
15. Gong Q, Wang C, Chuai X, Chiu S. Monkeypox virus: a re-emergent threat to humans. Virologica Sin. 2022;37:477–482. doi:10.1016/j.virs.2022.07.006
16. McCollum AM, Damon IK. Human monkeypox. Clinl Infect Dis. 2014;58(2):260–267. doi:10.1093/cid/cit703
17. Lulli LG, Baldassarre A, Mucci N, Arcangeli G. Prevention, risk exposure, and knowledge of monkeypox in occupational settings: a scoping review. Trop Med Infect Dis. 2022;7(10):276. doi:10.3390/tropicalmed7100276
18. Angelo KM, Petersen BW, Hamer DH, Schwartz E, Brunette G. Monkeypox Transmission Among International travellers—serious Monkey Business? Oxford University Press; 2019:taz002.
19. Meo SA, Al-Khlaiwi T, Al Jassir FF, Meo AS. Impact of traveling on transmission trends of human monkeypox disease: worldwide data based observational analysis. Front Public Health. 2023;11:1029215. doi:10.3389/fpubh.2023.1029215
20. Kaler J, Hussain A, Flores G, Kheiri S, Desrosiers D. Monkeypox: a comprehensive review of transmission, pathogenesis, and manifestation. Cureus. 2022;14:7.
21. Likos AM, Sammons SA, Olson VA, et al. A tale of two clades: monkeypox viruses. J Gen Virol. 2005;86(10):2661–2672. doi:10.1099/vir.0.81215-0
22. Sklenovská N, Van Ranst M. Emergence of monkeypox as the most important orthopoxvirus infection in humans. Front Public Health. 2018;6:241. doi:10.3389/fpubh.2018.00241
23. Breman JG, Steniowski M, Gromyko A, Gromyko A, Arita I, Arita I. Human monkeypox, 1970-79. Bull World Health Organizat. 1980;58(2):165.
24. World Health Organization. Smallpox. Availabel from: https://www.who.int/teams/health-product-policy-and-standards/standards-and-specifications/vaccine-standardization/smallpox#:~:text=Two%20forms%20of%20the%20disease,most%20prominent%20on%20the%20face.
25. Chauhan RP, Fogel R, Limson J. Overview of diagnostic methods, disease prevalence and transmission of mpox (Formerly Monkeypox) in humans and animal reservoirs. Microorganisms. 2023;11(5):1186. doi:10.3390/microorganisms11051186
26. Karagoz A, Tombuloglu H, Alsaeed M, et al. Monkeypox (mpox) virus: classification, origin, transmission, genome organization, antiviral drugs, and molecular diagnosis. J Infec Public Health. 2023;16:531–541. doi:10.1016/j.jiph.2023.02.003
27. Dubey T, Chakole S, Agrawal S, et al. Enhancing nursing care in monkeypox (Mpox) patients: differential diagnoses, prevention measures, and therapeutic interventions. Cureus. 2023;15:9.
28. Rizk JG, Lippi G, Henry BM, Forthal DN, Rizk Y. Prevention and treatment of monkeypox. Drugs. 2022;82(9):957–963. doi:10.1007/s40265-022-01742-y
29. Akter F, Hasan TB, Alam F, et al. Effect of prior immunisation with smallpox vaccine for protection against human Mpox: a systematic review. Rev Med Virol. 2023;33(4):e2444. doi:10.1002/rmv.2444
30. Malik S, Ahmad T, Ahsan O, Muhammad K, Waheed Y. Recent developments in mpox prevention and treatment options. Vaccines. 2023;11(3):500. doi:10.3390/vaccines11030500
31. Shoaib HM. Monkeypox as a potential emerging pandemic: a discussion on future risks and preparedness in Saudi Arabia. Front Public Health. 2023;11:1254545. doi:10.3389/fpubh.2023.1254545
32. Ejaz H, Junaid K, Younas S, et al. Emergence and dissemination of monkeypox, an intimidating global public health problem. J Infec Public Health. 2022;15:1156–1165. doi:10.1016/j.jiph.2022.09.008
33. Hasan S, Saeed S. Monkeypox disease: an emerging public health concern in the shadow of COVID-19 pandemic: an update. Trop Med Infect Dis. 2022;7(10):283. doi:10.3390/tropicalmed7100283
34. Riccò M, Ferraro P, Camisa V, et al. When a neglected tropical disease goes global: knowledge, attitudes and practices of Italian physicians towards monkeypox, preliminary results. Trop Med Infect Dis. 2022;7(7):135. doi:10.3390/tropicalmed7070135
35. Hasan M, Hossain MA, Chowdhury S, et al. Human monkeypox and preparedness of Bangladesh: a knowledge and attitude assessment study among medical doctors. J Infec Public Health. 2023;16(1):90–95. doi:10.1016/j.jiph.2022.11.032
36. Harapan H, Setiawan AM, Yufika A, et al. Knowledge of human monkeypox viral infection among general practitioners: a cross-sectional study in Indonesia. Pathog Global Health. 2020;114(2):68–75. doi:10.1080/20477724.2020.1743037
37. Jamil H, Idrees M, Idrees K, et al. Socio-demographic determinants of monkeypox virus preventive behavior: a cross-sectional study in Pakistan. bioRxiv. 2022;2022:521248.
38. Sahin TK, Erul E, Aksun MS, Sonmezer MC, Unal S, Akova M. Knowledge and attitudes of Turkish physicians towards human monkeypox disease and related vaccination: a cross-sectional study. Vaccines. 2022;11(1):19. doi:10.3390/vaccines11010019
39. Oyebade A, Oshineye A, Olarinmoye A, Kayode O, Akinpelu A, Oladosu M. Monkeypox related knowledge, attitudes and practices among students in a tertiary institution in southwest, Nigeria: a cross-sectional study. Res J Health Sci. 2023;11(3):205–212. doi:10.4314/rejhs.v11i3.3
40. Malaeb D, Sallam M, Salim NA, et al. Knowledge, attitude and conspiracy beliefs of healthcare workers in Lebanon towards Monkeypox. Trop Med Infect Dis. 2023;8(2):81. doi:10.3390/tropicalmed8020081
41. Nath SD, Islam AK, Majumder K, et al. Assessment of knowledge on human monkeypox virus among general population in Bangladesh: a nationwide cross-sectional study. medRxiv. 2022;2022:22279445.
42. Gonzales-Zamora JA, Soriano-Moreno DR, Soriano-Moreno AN, et al. Level of knowledge regarding Mpox among peruvian physicians during the 2022 outbreak: a cross-sectional study. Vaccines. 2023;11(1):167. doi:10.3390/vaccines11010167
43. Ahmed S, Abdulqadir S, Hussein S, et al. Knowledge, Attitudes, and Willingness to Vaccinate for Mpox Among Healthcare Workers in Kurdistan Region of Iraq: A Nationwide Cross-Sectional Study. Preprints; 2023.
44. Jahromi AS, Jokar M, Sharifi N, Kashkooli S, Rahmanian K, Rahmanian V. Global knowledge and attitudes towards mpox (monkeypox) among healthcare workers: a systematic review and meta-analysis. International Health. 2023;ihad094. doi:10.1093/inthealth/ihad094
45. Sobaikhi NH, Alshahrani NZ, Hazazi RS, et al. Health workers’ knowledge and attitude towards monkeypox in Southwestern Saudi Arabia: a cross-sectional study. Diseases. 2023;11(2):81. doi:10.3390/diseases11020081
46. Wang B, Peng X, Li Y, et al. Perceptions, precautions, and vaccine acceptance related to monkeypox in the public in China: a cross-sectional survey. J Infec Public Health. 2023;16(2):163–170. doi:10.1016/j.jiph.2022.12.010
47. Rony MKK, Sharmi PD, Akter D, Parvin MR, Alamgir HM. Knowledge and attitude regarding human monkeypox virus infection among nurses: a cross-sectional study. Sage Open Nurs. 2023;9:23779608231216619. doi:10.1177/23779608231216619
48. Sah R, Mohanty A, Reda A, Padhi BK, Rodriguez-Morales AJ. Stigma during monkeypox outbreak. Front Public Health. 2022;10:1023519. doi:10.3389/fpubh.2022.1023519
49. Ju W, Sannusi SN, Mohamad E. Stigmatizing Monkeypox and COVID-19: a comparative framing study of the Washington post’s online news. Int J Environ Res Public Health. 2023;20(4):3347. doi:10.3390/ijerph20043347
50. Nimbi FM, Giovanardi G, Baiocco R, Tanzilli A, Lingiardi VM. New epidemic or fake news? Study of psychological and social factors associated with fake news attitudes of monkeypox in Italy. Front Psychol. 2023;14:1093763. doi:10.3389/fpsyg.2023.1093763
51. Lesperance AM, Miller JS. Preventing Absenteeism and Promoting Resilience Among Health Care Workers in Biological Emergencies. Richland, WA (United States);: Pacific Northwest National Lab.(PNNL); 2009.
52. Das SK, Bhattarai A, Kc S, et al. Socio-demographic determinants of the knowledge and attitude of Nepalese healthcare workers toward human monkeypox: a cross-sectional study. Front Public Health. 2023;11:1161234. doi:10.3389/fpubh.2023.1161234
53. Harapan H, Setiawan AM, Yufika A, et al. Confidence in managing human monkeypox cases in Asia: a cross-sectional survey among general practitioners in Indonesia. Acta Trop. 2020;206:105450. doi:10.1016/j.actatropica.2020.105450
54. Ibrahim AM, Zaghamir DEF. Knowledge and attitudes towards mpox and effect of intervention among college of applied medical sciences students. Libyan J Med. 2023;18(1):2222448. doi:10.1080/19932820.2023.2222448
55. Decousser J-W, Romano-Bertrand S, Glele LA, et al. Healthcare worker protection against mpox contamination: position paper of the French Society for Hospital Hygiene. J Hosp Infect. 2023;140:156–164. doi:10.1016/j.jhin.2023.08.004
56. Manirambona E, Musa SS, Shomuyiwa DO, et al. The monkeypox virus: a public health challenge threatening Africa. Public Health Challenges. 2022;1(4):e33. doi:10.1002/puh2.33
57. Persad G, Leland R, Ottersen T, et al. Fair domestic allocation of monkeypox virus countermeasures. Lancet Public Health. 2023;8(5):e378–e82. doi:10.1016/S2468-2667(23)00061-0
58. Miraglia Del Giudice G, Della Polla G, Folcarelli L, et al. Knowledge and attitudes of health care workers about monkeypox virus infection in Southern Italy. Front Public Health. 2023;11:1091267. doi:10.3389/fpubh.2023.1091267
59. Z-H L, Zhang X-R, Zhong W-F, et al. Knowledge, attitudes, and practices related to coronavirus disease 2019 during the outbreak among workers in China: a large cross-sectional study. PLoS Negl Trop Dis. 2020;14(9):e0008584. doi:10.1371/journal.pntd.0008584
60. Youssef D, Abboud E, Kawtharani M, Zheim Z, Abou Arrage N, Youssef J. When a neglected tropical zoonotic disease emerges in non-endemic countries: need to proactively fill the unveiled knowledge gaps towards human monkeypox among the Lebanese population. J Pharm Pol Prac. 2023;16(1):1–20. doi:10.1186/s40545-023-00544-1
61. Africa Wanderlust. 15 Best Countrıes to Vısıt in Afrıca. Available from: https://africawanderlust.com/destinations/best-countries-to-visit-in-africa/.
62. Gebrehana Belay H, Limenih SK, Wassie TH, Ambie MB. Neonatal near miss and its associated factors at injibara general hospital, Awi Zone, Northwest Ethiopia, 2019. Explorat Res Hypoth Med. 2020;5(2):62–69.
63. Alshahrani NZ, Algethami MR, Alarifi AM, et al. Knowledge and attitude regarding monkeypox virus among physicians in Saudi Arabia: a cross-sectional study. Vaccines. 2022;10(12):2099. doi:10.3390/vaccines10122099
64. Bitew G, Sharew M, Belsti Y. Factors associated with knowledge, attitude, and practice of COVID-19 among health care professional’s working in South Wollo Zone Hospitals, Northeast Ethiopia. SAGE Open Medicine. 2021;9:20503121211025147. doi:10.1177/20503121211025147
65. Saied AA, Chandran D, Chakraborty S, Emran TB, Dhama K. Mpox and healthcare workers—a minireview of our present knowledge. Egypt J Int Med. 2023;35(1):46. doi:10.1186/s43162-023-00233-0
66. Ajayi PO, Esan DT, Ipinnimo TM, Olanrewaju MT, Solomon OO, Atanda-Owoeye OO. Knowledge and awareness of human mpox infection among healthcare workers: a cross-sectional study in southwestern Nigeria. Asian Pac J Trop Med. 2023;16(6):245–252. doi:10.4103/1995-7645.378566
67. Lounis M, Bencherit D, Abdelhadi S. Knowledge and awareness of Algerian healthcare workers about human monkeypox and their attitude toward its vaccination: an online cross-sectional survey. Vacunas. 2023;24(2):122–127. doi:10.1016/j.vacun.2022.11.003
68. Awoyomi OJ, Njoga EO, Jaja IF, et al. Mpox in Nigeria: perceptions and knowledge of the disease among critical stakeholders—Global public health consequences. PLoS One. 2023;18(3):e0283571. doi:10.1371/journal.pone.0283571
69. Peng X, Wang B, Li Y, et al. Perceptions and worries about monkeypox, and attitudes towards monkeypox vaccination among medical workers in China: a cross-sectional survey. J Infec Public Health. 2023;16(3):346–353. doi:10.1016/j.jiph.2023.01.010
70. Bhattarai A, Paudel K, Bhusal S, et al. Socio-demographic determinants of the knowledge of monkeypox virus among the general public: a cross-sectional study in a tertiary care center in Nepal; 2023.
71. Alshahrani NZ, Alzahrani F, Alarifi AM, et al. Assessment of knowledge of monkeypox viral infection among the general population in Saudi Arabia. Pathogens. 2022;11(8):904. doi:10.3390/pathogens11080904
72. Al-Mustapha AI, Ogundijo OA, Sikiru NA, et al. A cross-sectional survey of public knowledge of the monkeypox disease in Nigeria. BMC Public Health. 2023;23(1):1–9. doi:10.1186/s12889-023-15398-0
73. Ren F, Liu J, Miao J, et al. Public awareness, specific knowledge, and worry about mpox (monkeypox): a preliminary community-based study in Shenzhen, China. Front Public Health. 2023;11:1077564. doi:10.3389/fpubh.2023.1077564
74. Raman H, Jamil A, Rasheed A, et al. Knowledge of medical students towards the re-emergence of human monkeypox virus. Cureus. 2023;15(10). doi:10.7759/cureus.46761
75. ElHafeez S A, Gebreal A, Khalil MA, et al. Assessing disparities in medical students’ knowledge and attitude about monkeypox: a cross-sectional study of 27 countries across three continents. Front Public Health. 2023;2023:11.
76. Goshiye D, Abegaz Z, Knowledge GS. Attitude, and practice towards COVID-19 among mothers in Dessie town, Northeast Ethiopia, 2020. Interdiscip Perspect Infec Dis. 2022;2022:1–10. doi:10.1155/2022/4377460
77. Jamaleddine Y, Abou El Ezz A, Mahmoud M, et al. Knowledge and attitude towards monkeypox among the Lebanese population and their attitude towards vaccination. J Prev Med Hyg. 2023;64(1):E13. doi:10.15167/2421-4248/jpmh2023.64.1.2903
78. Ennab F, Nawaz FA, Narain K, Nchasi G, Essar MY. Rise of monkeypox: lessons from COVID-19 pandemic to mitigate global health crises. Ann Med Surg. 2022;79:104049. doi:10.1016/j.amsu.2022.104049
79. León-Figueroa DA, Barboza JJ, Siddiq A, Sah R, Valladares-Garrido MJ, Rodriguez-Morales AJ. Knowledge and attitude towards monkeypox: systematic review and meta-analysis; 2023.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.