Back to Journals » Chronic Wound Care Management and Research » Volume 9
Knowledge and Practice of Wound Care and Associated Factors among Nurses Working in South Wollo Zone Government Hospitals, Ethiopia
Authors Tegegne B, Yimam F, Mengesha Yalew Z , Wuhib M , Mekonnen L, Asmamaw Yitayew Y , Ademe S , Tsegaye D , Eshetie Y, Chanie M
Received 17 March 2022
Accepted for publication 11 July 2022
Published 20 July 2022 Volume 2022:9 Pages 1—11
DOI https://doi.org/10.2147/CWCMR.S366322
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Marco Romanelli
Belachew Tegegne,1 Feruza Yimam,2 Zemen Mengesha Yalew,1 Mekuriaw Wuhib,1 Leul Mekonnen,1 Yibeltal Asmamaw Yitayew,3 Sewunet Ademe,1 Dejen Tsegaye,4 Yeshiambaw Eshetie,5 Muluken Chanie6
1Department of Comprehensive Nursing, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia; 2Department of Nursing, Tropical College of Medicine, Dessie, Ethiopia; 3Department of Pediatrics and Child Health Nursing, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia; 4Department of Nursing, College of Health Science, Debre Markos University, Debre Markos, Ethiopia; 5Department of Nursing, College of Health Science, Debre Tabor University, Debre Tabor, Ethiopia; 6Department of Nursing, Debre Tabor Health Science College, Debre Tabor, Ethiopia
Correspondence: Zemen Mengesha Yalew, Tel +251 91-805-7019, Email [email protected]
Background: Wound infection is caused by pathogenic organisms invading viable tissue surrounding a localized defect or excavation in the skin or underlying soft tissue. Nurses have a critical role in wound care and dressing selection, and they should strive to stay current in this ever-changing field. To prevent wound infection, it is essential to improve wound-care knowledge and practice.
Objective: To assess knowledge and practice of wound care and associated factors among nurses working in government hospitals of South Wollo Zone, Ethiopia.
Methods: A hospital-based cross-sectional study design was used among 422 randomly selected nurses in government hospitals in South Wollo. A pretested structured self-administered questionnaire was used to collect data. Data were entered in EpiData 4.4.2 and exported to SPSS 25.0 for analysis. Descriptive statistics and bivariate and multivariate logistic regression were applied. Variables with P value < 0.05 were considered statistically significant for knowledge and good practice of wound care.
Results: According to the findings, 40.3% and 51.0% had good knowledge and practice of wound care, respectively. Holding a bachelor’s degree or above (AOR 3.27, 95% CI 1.97– 5.43) and training (AOR 3.71, 95% CI 2.37– 5.81) were significantly associated with knowledge of wound care. More than 10 years of experience (AOR 3.15, 95% CI 1.96– 5.04), training (AOR 3.75, 95% CI, 2.38– 5.85), and not having a patient load (AOR 3.15, 95% CI 1.96– 5.04) were significantly associated with wound-care practices.
Conclusion: Nurses’ wound-care knowledge and practice were low. Knowledge and practice on wound care were determined by educatio, training, patient load, and experience. Nurses should get training and share experience.
Keywords: wound care, knowledge, practice, Ethiopia
Introduction
Wound infection is caused by pathogenic organisms invading viable tissue surrounding a localized defect or excavation in the skin or underlying soft tissue.1,2 Antimicrobial-resistant bacteria cause bacterial wound infections, which are linked to higher morbidity and health-care costs. In underdeveloped countries, they are a leading cause of morbidity and mortality.3,4
If proper wound care is not provided, the wound-healing process may be delayed,5,6 and can cause extended duration of hospitalization, bad scar formation, and hernia induced by wound dehiscence, also resulting in increased costs.7,8 A number of factors may contribute to a delayed wound-healing process, thus causing improper or impaired tissue repair.9 Some of these factors are cancer therapies (radiation, chemotherapy), comorbidities (diabetes, obesity, protein-energy deficiency), and lifestyle choices (smoking, alcohol abuse).10
For rapid wound healing, special nursing care is required at both the hospital and after discharge, within the scope of the discharge care, and also the patient and family or caregiver should be educated concerning wound care, prevention of infection development, regulation and maintenance of nutrition, medication, and under which conditions they need to be seen by a health-care provider,11,12 because quality wound care is very important for rapid and uncomplicated healing through decreasing complications, repeated admissions, length of hospital stay, and costs, and enhancing patient quality of life.13–16
Although wound care is performed by a multidisciplinary team, it is primarily a nurse-led activity.17 Indeed, wound healing depends on nurses’ knowledge of the physiology and process of wound healing and consequently the nursing interventions.18 With sufficient knowledge concerning wound healing, a nurse can perform a systematic and holistic patient assessment and identify possible wound complications at an early stage.13,14,19 Improving knowledge and practice of wound care is paramount to reducing wound infection. Better knowledge and practice of wound care decreases wound-related complications and repeated admissions and enhances one’s quality of life.20 Therefore, this study aimed to assess nurses’ knowledge and practice of wound care.
Methods
Study Area and Period
The study was conducted in governmental hospitals of South Wollo Zone, Amhara, Ethiopia from April 25 to May 25, 2021. South Wollo is in Amhara National Regional State, which has a total population, of 2,816,299 (1,409,131 male and 1,407,168 female). The zone has 13 hospitals, one a comprehensive specialized hospital. A total of 6,454 health-care providers are found in this zone (those working in health centers and hospitals), and among these, around 778 of nurses are from hospitals.
Study Design
An institution-based cross-sectional study design was used.
Source Population
All nurses working in governmental hospitals of South Wollo were the source population.
Study Population
All nurses who had worked for at least 6 months in government hospitals of South Wollo were the study population.
Exclusion Criteria
Volunteer nurses and those on annual or maternity leave were excluded from the study.
Sample-Size Determination
The sample size was calculated using a single population–proportion formula considering P=48.7%21 with a 95% CI and 5% marginal error:
where:
n = sample size
α = confidence interval
p = prevalence of good behavioral responses
W = margin of error
n = (1.96)2× 0.487 (0.513)/(0.0025) = 384
By considering a 10% nonresponse rate, the sample size was 422.
Sampling Procedure/Technique
There are 13 governmental hospitals in this zone. Among these, six were randomly selected, (through lottery method), and then to select participants, the first proportional allocation of nurses from each hospital was done based on the total number of nurses found in each hospital. Then, simple random sampling was used to select participants (Figure 1).
 |
Figure 1 Sample selection. |
Data-Collection Tool and Procedures
The data were collected using a pretested structured self-administered questionnaire. The data-collection tool was developed by reviewing the literature.21,22 It had five parts: sociodemographic characteristics (age, sex, ethnicity, religion, education, marital status, and working experience), health-care provider–related factors (lack of assertiveness, position, lack of familiarity with antiseptics, and lack of opportunity to express opinion), institution-related factors (workload, training, lack of variety in wound-cleaning and dressing material, presence of protocols and guidelines, hierarchy pressure, and clinical working unit), knowledge-related items (14 questions with yes/no responses), and practice-related items (15 items using a Likert scale ranging from “never” to “always”). The data were collected by four BSc nurses and one MSc nurse supervisor.
Variables
Dependent Variable
Knowledge and practice of wound care.
Independent Variables
Sociodemographic characteristics: age, sex, ethnicity, religion, education, marital status
Health-care provider–related factors: lack of assertiveness, position, hierarchy pressure, lack of familiarity with antiseptics, lack of opportunity to express opinion
Institution-related factors: workload, training, lack of wound-cleaning and dressing materials, absence of protocols and guidelines, clinical working unit
Operational Definitions
Good knowledge: those who scored equal to and above the mean on knowledge items
Poor knowledge: those who scored below the mean on knowledge items
Good practice: those who scored equal to and above the mean on practice items
Poor practice: those who scored below the mean on practice items
Data Quality Control
Data quality was assured through conducting training for data collectors on the overall process of data collection. The questionnaire was written in English, then translated into Amharic, which was the study subjects’ native language, and finally back to English by language experts to ensure consistency and conceptual equivalence. At the same time, each completed questionnaire was checked for coherence, completeness, and consistency. Daily evaluation was carried out to address any issues that arose during the data-collection process.
Data Processing and Analysis
Data were cleaned before being coded and entered in EpiData 4.4.2, then exported to SPSS 23 for analysis. To summarize descriptive statistics, frequency tables and figure were used. All variables with p<0.25 one bivariate binary logistic regression analysis were kept for multivariate analyses. P<0.05 was used to define statistical significance.
Results
Sociodemographic Characteristics of Respondents
A total of 400 nurses were involved in the study, yielding a response rate of 94.8%. Their mean age was 31.96±6.10 years. The religious distribution showed that a majority (211, 52.8%) were orthodox Christian. Regarding education, 273 (68.3%) held degrees and above. More than half (223, 55.8%) were male (Table 1).
 |
Table 1 Sociodemographic characteristics of participants (n=400) |
Health Service–Related Characteristics
A quarter of the study participants were working in medical wards. More than half (213, 53.3%) responded that there were no guidelines. Only 180 (45.0%) had enough dressing material in their units. Regarding training, 210 (52.5%) had formal training about wound care (Table 2).
 |
Table 2 Health service–related characteristics (n=400) |
Knowledge of Wound Care
The mean knowledge score was 20.02±2.24. Using the mean value as a cutoff point, 40.3% of respondents had good knowledge of wound care. A majority (268, 67.0%) responded that irrigation removed debris from wounds better than swabbing (Table 3).
 |
Table 3 Knowledge of wound care (n=400) |
Factors Associated with Knowledge of Wound Care
Bivariate analysis results showed that education, guideline availability, training, and age were significantly associated with knowledge of wound care, so were candidates for multivariate analysis. On multivariate analysis, only education and training were identified to be significantly associated with knowledge of wound care. The odds of having knowledge were 3.27 times (95% CI 1.97–5.43) higher among nurses who held degrees and above than diploma holders. Nurses who had had training on wound care were 3.71 times (95% CI 2.37–5.81) more likely to have good knowledge than their counterparts (Table 4).
 |
Table 4 Binary and multivariate logistic regression on predictors of knowledge of wound care |
Wound-Care Practices
Mean practice score was 31.27±4.57. Using the mean value as a cutoff point, 51.0% of respondents had good practice of wound care. Two-thirds (150, 37.5%) of the nurses “sometimes” washed their hands before and after wound dressing. Using sterilized and dressing materials for cleaning and dressing wounds had the most positive (always) responses (251, 62.8%; Table 5).
 |
Table 5 Wound-care practices |
Factors Associated with Wound-Care Practices
Bivariate analysis results showed that guidelines, patient load, training, familiarity with antiseptics, hierarchy pressure, age, and experience were significantly associated with wound-care practices. On multivariate analysis, only patient load, training, and work experience were significantly associated with wound-care practices (Table 6). The odds of having good practices were 3.15 times (95% CI 1.96–5.04) higher among nurses who had no patient load than their counterparts. Nurses who had had training were 3.73 times (95% CI 2.38–5.85) more likely to practice wound care than those who had not. The findings also showed that nurses who had >10 years of work experience were 1.82 times (95% CI 1.16–2.85) more likely to have good practice than those who had <10 years of working experience.
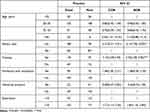 |
Table 6 Binary and multivariate logistic regression on predictors of wound-care practices |
Discussion
This study aimed to assess nurses’ knowledge and practice of wound care. Education and training were significant factors in knowledge. Similarly, training, patient load, and experience were predictors of wound-care practices. We found that 40.3% (95% CI 36.0%–45.3%) of nurses had good knowledge regarding wound care. This was lower than studies conducted in Bahir Dar, Ethiopia, Turkey, the UK, and Malaysia.22–29 This difference may be due to the inclusion of all nurses (this study included nurses working in all units), differences in organizational behavior among countries, where some might have good training and educational institutions, and study-method difference (The UK study used qualitative methods). However, our result is higher than studies conducted in Australia and Uganda.30–32 The difference might be the previous studies focused only on nurses' knowledge of pressure-ulcer prevention.
Having a degree and above was a contributing factor to knowledge of wound care. The odds of having knowledge of wound care were 3.27 times higher among nurses who had degree and above educational qualification than diploma holders. This might be due to bachelor’s degree and above holders having a deeper knowledge base on which to draw in such areas as clinical practice and critical thinking. The other factor that contributed to nurses' knowledge was training related to wound care. Nurses who had had training on wound care were 3.71 times as likely to have good knowledge than their counterparts. This finding is congruent with the study conducted in Bahir Dar.22 This may be because updating health workers’ knowledge about infection prevention improves their older understanding, resulting in a high score on knowledge questions. Furthermore, because Ethiopia’s current infection-prevention and patient-safety national guidelines include thorough information and evidence-based recommendations for infection prevention, nurses who have completed this training may have a better understanding of infection prevention. The conceptual map and assumption that the training was enhancing knowledge and skills in health-care practices of health workers and primary health-care entities would significantly improve the performance of individuals, teams, organizations, and health systems for better health outcomes. The other outcome variable addressed in this study was the practices of wound care, and and 51.0% (95% CI 46.3%–56.0%) of the nurses had good practices. This finding was lower than the study conducted in Malaysia.26 However, it was higher than the studies conducted in Bahir Dar and Australia.22,30,33 Reasons for the disparity might be a difference in health-staff awareness of how to prevent surgical site infection and the presence of specific case assessment of surgical site–infection prevention.
The first contributing factor to wound-care practices addressed in this study was having no patient load in the working unit. The odds of having good practices were 3.15 times higher among nurses who had no patient load in the working unit than their counterparts. It is clear that substantial nursing workload can influence the care provider’s decision to perform various procedures, mainly in infection prevention.34 This might be due to the fact that less patient load will also help keep employees from burnout and loss of function, and also under extensive workloads, nurses may not have adequate time to perform tasks that can have a direct effect on wound-care practices.35,36 The other contributing factor to wound-care practices was training. Nurses who had had training were 3.73 times more likely to practice wound care than those who had not. This finding is in line with the studies conducted in Bahir Dar and the UK.20,22 This might be also due to training making nurses aware of procedures and wound-care practices. Facilities can minimize on-the-job injuries and accidents with a robust safety-training program. Training workers that they are motivated to follow the procedures.
Lastly, work experience was a contributing factor to wound-care practices. Nurses who have >10 years’ work experience were 1.82 times as likely to have good practice as those with <10 years’ experience. This could be explained by the fact that when experience increases, social interaction increases, they take on more responsibility, skill development and interest in practices develops as well,37 and also due to the fact that as health workers’ years of experience increase, they are more likely to be exposed to surgical departments on a regular basis and gain experience through working with senior staff.
Limitations
Social desirability bias and recall bias could be limitations of this study. As a result, respondents were assured of complete confidentiality and anonymity throughout the study to reduce the former.
Conclusion
This study revealed that nurses’ knowledge and practice of wound care were poor. Education and training were factors for knowledge. Similarly, patient load, training, and work experience were predictors of practices. Therefore, nurses should improve their education and take basic training related to knowledge and practice of wound care.
Data Sharing
Data will be available upon request from the corresponding author.
Ethics Approval and Consent to Participate
The study protocol was approved by the Research Ethics and Approval Committee of Wollo University, College of Medicine and Health Science (RF: CMHS 187/02/12). Official letters of cooperation were written to each hospital for facilitating the study. Informed written consent was obtained from each study participant, and respondents had the right not to participate or withdraw from the study at any stage. Anonymity and confidentiality of the data were ensured, and all study methods were performed in accordance with the Declaration of Helsinki.
Acknowledgments
We would like to thank Wollo University for allowing us to conduct the study and our special thanks to our colleagues for their help in providing valuable information on the write-up. We would also like to thank data collectors and respondents for their invaluable support.
Funding
Wollo University covered the cost of data collection, entry, and supervision.
Disclosure
The authors declare no conflicts of interest in relation to this work.
References
1. Dessalegn L, Shimelis T, Tadesse E, Gebre-selassie S. Aerobic bacterial isolates from post-surgical wound and their antimicrobial susceptibility pattern: a hospital based cross-sectional study. J Med Res. 2014;3(2):18–23.
2. Shimekaw M, Tigabu A, Tessema B. Bacterial profile, antimicrobial susceptibility pattern, and associated risk factors among patients with wound infections at Debre markos referral hospital, Northwest, Ethiopia. Int J Low Extrem Wounds. 2022;21(2):182–192. doi:10.1177/1534734620933731
3. Hailu D, Derbie A, Mekonnen D, et al. Drug resistance patterns of bacterial isolates from infected wounds at Bahir Dar regional health research laboratory center, Northwest Ethiopia. Ethiop J Health Dev. 2016;30(3):112–117.
4. Mulu W, Abera B, Yimer M, Hailu T, Ayele H, Abate D. Bacterial agents and antibiotic resistance profiles of infections from different sites that occurred among patients at Debre markos referral hospital, Ethiopia: a cross-sectional study. BMC Res Notes. 2017;10(1):1–9. doi:10.1186/s13104-016-2345-3
5. Trexler RA. Assessment of surgical wounds in the home health patient: definitions and accuracy with OASIS-C. Home Healthc Now. 2011;29(9):550–559. doi:10.1097/NHH.0b013e31821feb05
6. Nunan R, Harding KG, Martin P. Clinical challenges of chronic wounds: searching for an optimal animal model to recapitulate their complexity. Dis Model Mech. 2014;7(11):1205–1213. doi:10.1242/dmm.016782
7. Mathieu D, Linke J, Wattel F. Non-healing wounds. In: Handbook on Hyperbaric Medicine. Springer; 2006:401–428.
8. Hodgetts SKC, Leslie DG. Determining risk factors for surgical wound dehiscence. Int Wound J. 2013;12:1–11.
9. Gosain A, DiPietro LA. Aging and wound healing. World J Surg. 2004;28(3):321–326. doi:10.1007/s00268-003-7397-6
10. Anderson K, Hamm RL. Factors that impair wound healing. J Am Coll Clin Wound Specialists. 2012;4(4):84–91. doi:10.1016/j.jccw.2014.03.001
11. Adkins CL. Wound care dressings and choices for care of wounds in the home. Home Healthc Nurse. 2013;31:259–267. doi:10.1097/NHH.0b013e31828eb658
12. Benbow M. Wound care: ensuring a holistic and collaborative assessment. Br J Commun Nurs. 2011;16:6–16. doi:10.12968/bjcn.2011.16.Sup9.S6
13. McFadden EA, Miller MA. Clinical nurse specialist practice; facilitators and barriers. Clin Nurse Spec. 1994;8:27–33. doi:10.1097/00002800-199401000-00010
14. McGillivray CF. The identification of barriers to pressure ulcer healing. Wound Care Can. 2010;2010:20–24.
15. Magalhaes MGA, Alcantara LF, Bezerra SM. Postoperative mediastinitis in a heart hospital of Recife: contributions for nursing care. Rev Esc Enferm USP. 2012;46:863–869.
16. Excellence NIfHaC. Press Release: NICE Guidelines are Set to Improve the Prevention and Treatment of Surgical Site Infections (SSI). London: Department of Health; 2008.
17. Gillespie BM, Walker R, Lin F, et al. Wound care practices across two acute care settings: a comparative study. J Clin Nurs. 2020;29(5–6):831–839. doi:10.1111/jocn.15135
18. Gizaw MA, Negawo MK, Bala ET, Daba DB. Knowledge, practice, and associated factors towards postoperative wound care among nurses working in public hospitals in Ethiopia: a multicenter cross‐sectional study in low resource setting area. Health Sci Rep. 2022;5(4):e677. doi:10.1002/hsr2.677
19. Mengesha RE, Saravanan M, Berhe DF, Wasihun AG, Wasihun AG. Aerobic bacteria in post surgical wound infections and pattern of their antimicrobial susceptibility in ayder teaching and referral hospital, Mekelle, Ethiopia. BMC Res Notes. 2014;7:575. doi:10.1186/1756-0500-7-575
20. Ferreira AM, Rigotti MA, da Silva Barcelos L, Simão CMF, Ferreira DN, Gonçalves RQ. Knowledge and practice of nurses about care for patients with wounds. Rev pesqui cuid fundam Online. 2014;6(3):1178–1190. doi:10.9789/2175-5361.2014.v6i3.1178-1190
21. Teshager FA, Engeda EH, Worku WZ. Knowledge, practice, and associated factors towards prevention of surgical site infection among nurses working in Amhara regional state referral hospitals, Northwest Ethiopia. Surg Res Pract. 2015;2015:1–6. doi:10.1155/2015/736175
22. Woldegioris T, Bantie G, Getachew H. Nurses’ knowledge and practice regarding prevention of surgical site infection in Bahir Dar, Northwest Ethiopia. Surg Infect (Larchmt). 2019;20(1):71–77. doi:10.1089/sur.2018.081
23. Aydin AK, Karadag A, Gül S, Avsar P, Baykara ZG. Nurses’ knowledge and practices related to pressure injury: a cross-sectional study. J Wound Ostomy Continence Nurs. 2019;46(2):117–123. doi:10.1097/WON.0000000000000517
24. De Meyer D, Verhaeghe S, Van Hecke A, Beeckman D. Knowledge of nurses and nursing assistants about pressure ulcer prevention: a survey in 16 Belgian hospitals using the PUKAT 2.0 tool. J Tissue Viability. 2019;28(2):59–69. doi:10.1016/j.jtv.2019.03.002
25. Lawrence P, Fulbrook P, Miles S. A survey of Australian nurses’ knowledge of pressure injury/pressure ulcer management. J Wound Ostomy Contin. 2015;42(5):450–460. doi:10.1097/WON.0000000000000141
26. Sham F, Abdul Raji NA, Omar MF, et al. Nurses’ knowledge and practice towards prevention of surgical site infection. Int j serv ind manag Sustain. 2021;6(1):1–20.
27. Surme Y, Kacmaz HY, Ceyhan O. Knowledge and practices of the intern nursing students on wound care. Int J Caring Sci. 2021;14(2):1212.
28. Mccluskey P, Mccarthy G. Nurses’knowledge and competence in wound management. Wounds UK. 2012;8:37–47.
29. Ayed A. Knowledge and practice of nursing staff towards infection control measures in the Palestinian hospitals; 2015.
30. Gillespie BM, Chaboyer W, Allen P, Morely N, Nieuwenhoven P. Wound care practices: a survey of acute care nurses. J Clin Nurs. 2014;23(17–18):2618–2627. doi:10.1111/jocn.12479
31. Gonzaga de Faria GB, Nascimento Do Prado T, Almeida lima E, Brunet Rogenski NM, Tomazini Borghardt A, Massaroni L. Knowledge and practice of nurses on the care of wounds. J Nurs UFPE/Revista de Enfermagem UFPE. 2016;10:12.
32. Mwebaza I, Katende G, Groves S, Nankumbi J. Nurses’ knowledge, practices, and barriers in care of patients with pressure Ulcers in a Ugandan teaching hospital. Nurs Res Pract. 2014;2014:973602. doi:10.1155/2014/973602
33. Nasreen S, Afzal M, Sarwar H. Nurses knowledge and practices toward pressure ulcer prevention in general hospital Lahore. Age. 2017;87(166):34.
34. Daud-Gallotti RM, Costa SF, Guimarães T, et al. Nursing workload as a risk factor for healthcare associated infections in ICU: a prospective study. PLoS One. 2012;7(12):e52342. doi:10.1371/journal.pone.0052342
35. Mwakanyamale AA, Mukaja A-M, Ndomondo MD, Zenas J, Stephen A, Mika EZ. Nursing practice on post-operative wound care in surgical wards at Muhimbili national hospital, Dar-es-Salaam, Tanzania. Open Journal of Nursing. 2019;09:870–890. doi:10.4236/ojn.2019.98065
36. Sürme Y, Kartın PT, Çürük GN. Knowledge and practices of nurses regarding wound healing. J Perianesth Nurs. 2018;33(4):471–478. doi:10.1016/j.jopan.2016.04.143
37. Blegen MA, Vaughn TE, Goode CJ. Nurse experience and education: effect on quality of care. JONA. 2001;31(1):33–39. doi:10.1097/00005110-200101000-00007
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.