Back to Journals » Infection and Drug Resistance » Volume 17
Isolation, and Identification of Escherichia coli O157:H7 Recovered from Chicken Meat at Addis Ababa Slaughterhouses
Authors Tegegne H , Filie K, Tolosa T, Debelo M, Ejigu E
Received 20 December 2023
Accepted for publication 1 March 2024
Published 6 March 2024 Volume 2024:17 Pages 851—863
DOI https://doi.org/10.2147/IDR.S430115
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Hailehizeb Tegegne,1 Kassahun Filie,1 Tadele Tolosa,2 Motuma Debelo,2 Eyoel Ejigu2
1Department of Veterinary Science, College of Agriculture and Environmental Science, Debre Tabor University, Debre Tabor, Amhara, Ethiopia; 2Department of Veterinary Medicine, College of Agriculture and Veterinary Medicine Jimma University, Jimma, Oromia, Ethiopia
Correspondence: Hailehizeb Tegegne, Email [email protected]
Introduction: It is a growing concern that pathogenic bacteria can be found in poultry meat, and an additional problem is the ongoing rise in food-derived bacteria’s resistance to antibiotics.
Methods: A cross-sectional study was conducted from February 2021 to March 2023. This study aimed to isolate, identify and analyze E. coli in poultry meat collected from slaughterhouses in Addis Ababa. A total of 499 samples were collected from fecal content, carcass, hand and knife swab samples by using purposive and systematic random sampling methods.
Results: An overall 5.2% Escherichia coli (E. coli O157:H7) prevalence was found in this study. On average, antimicrobial susceptibility tests revealed that the sensitivities of (Escherichia coli) E. coli O157:H7 isolates from carcass swabs, fecal content, manuals, knife swabs and water samples were 62.3%, 52.5%, 53%, 60% and 60%, respectively.
Discussion: However, few (Escherichia coli) E. coli O157:H7 isolates have developed multidrug resistance to some antibiotics, for an overall rate of 13.8%. Knowledge and attitude assessment of the slaughterhouse workers showed that 44.2% had no wash their hands at all and that 125.6% had washed their hands before slaughter commencement.
Conclusion: The detection of (Escherichia coli) E. coli O157:H7 isolates from all sample types had a slight prevalence of serious public health concerns. It is important to monitor antibiotic use for both human and animal health in order to make sure that it is safe and effective.
Keywords: Addis Ababa, antibiogram, chicken, Escherichia coli, slaughterhouse
Introduction
Food and water polluted with pathogens are typical routes of transmission, but protein remains the main source of energy in many developing countries, which has caused a rise in the amount consumed and production of meat1 Several steps can lead to food contamination by these pathogens, starting with the food chain, through manufacturing and processing, after distribution, and retail marketing, completing with the management and getting ready for the food.2
Foodborne illnesses cover a broad range of health issues and represent a growing global concern for public health. These diseases are the result of eating tainted food and include illnesses brought on by a variety of microorganisms as well as chemical hazards.2 We currently do not know how common foodborne illnesses are in developed and developing nations, or how they affect trade and the economies of those nations. However, foodborne illnesses typically affect developing nations the most and they are regarded as a serious public health concern and a significant cause of morbidity and mortality.3
In less economically developed nations, urban dwellers typically incorporate a higher proportion of animal protein into their diets compared to their rural counterparts. This is primarily attributed to the greater prosperity of city residents and their access to a diverse range of food options in local markets.3 As these areas undergo economic growth, there is a rising middle class that can financially support the consumption of commercially produced chicken meat. The swift establishment of facilities and infrastructure for broiler chicken production becomes feasible, contributing to the swift generation of this popular meat. Chicken, being not only perceived as a healthy choice but also the most affordable among livestock meats, further fuels its widespread popularity.4
One significant benefit of incorporating eggs and poultry meat into the human diet is that their consumption is generally free from significant cultural or societal restrictions. Furthermore, a single chicken can conveniently serve as a meal for an average family, eliminating the necessity for a refrigerator to preserve any uneaten portions.4 Meat from other livestock, such as pigs and cattle, is used mainly for special holidays, partly because of a lack of storage facilities (no refrigerator or electricity supply).5 Poultry meat is a rich in protein and low in carbohydrates. However, its high water content supports the multiplication of virulence bacteria.5 Poultry meat is acknowledged to harbor a higher prevalence of food-borne pathogens compared to red meat. Consequently, a greater number of foodborne illnesses are linked to poultry consumption, posing a significant public health issue in contemporary society.5 This concern holds importance due to its impact on the health and welfare of individuals, as well as its substantial economic ramifications, imposing a burden and diminishing economic growth for the country.6
The field of food safety encompasses the scientific principles governing the management, cooking, and preservation of food. Despite being a crucial aspect of food service operations, it often tends to be overlooked and lacks the attention it deserves.7 Nonetheless, there has been a great deal of public concern over the necessity of food preparation and storage throughout to guarantee food safety.8 According to the National Hygiene and Sanitation Strategy program, inadequate hygiene and sanitation in Ethiopia are linked to about 60% of infections.9 Foodborne disease outbreaks have been linked to unsafe sources of contaminated raw food items, improper food storage, inadequate cooling and reheating of food items, inadequate personal hygiene during food cooking, and a prolonged period of time between food preparation and consumption.9
Over 50% of the foodborne disease outbreaks can be linked to poultry, beef, and mutton meat products, primarily resulting from inadequate practices observed in restaurants, households, institutions, and various other settings.10 Pathogens, including STEC O157:H7, have been isolated from food, clinical samples, animals, and the environment on every continent during the last 20 years. 10,200 cases of STEC infections occur in Africa each year, with an incidence rate of 1.4 cases per 100,000 people. STEC O157:H7 causes 2,801,000 acute illnesses annually worldwide, with an incidence rate of 43.1 cases per 100,000 persons per year.11
The two primary sources of microorganisms present in slaughtered chickens are the birds’ digestive tracts and the slaughterhouse’s surroundings, which include live poultry, tools, and personnel.12 A typical slaughterhouse is typically partitioned into areas designated as clean and dirty, aimed at reducing contamination in the end products and maintaining a seamless flow of technical processes and materials. The dirty zone encompasses spaces for securing poultry by their feet and handling poultry carcasses following electrical immobilization. Subsequently, the deceased birds undergo water scaling in a confined tunnel.12 On the other hand, the clean zone comprises sections for evisceration, water chilling, cutting, deboning, and packaging.13 Since many cattle are thought to be the primary reservoir of Escherichia coli (E. coli O157:H7), a large number of studies have concentrated on this species. As a result, little information is known about the function of other possible reservoir animals, particularly poultry.14 As a result, little is known about the ecology and host specificity of Escherichia coli (E. coli O157:H7), as well as the significance of animal species other than cattle in the organism’s epidemiology.15
Due to the significance of Escherichia coli (E. coli) in both animal and public health, it is crucial to have a thorough understanding of the disease’s effective control and the necessary prerequisites, including knowledge about the microbiological and epidemiological conditions associated with it.15
Previous research findings have documented prevalence of Escherichia coli (E. coli O157:H7) bacteria ranged from 0.8% to 21.9% on uncooked meat sourced from butcher shops and slaughterhouses in Addis Ababa.11
However, the previous studies tend to suffer from small samples and sampling approaches that fail to obtain a representative sample of a population of interest. However, there is currently a lack of published reports on the isolation and identification, proportion, and associated risk factors for Escherichia coli (E. coli) in the Addis Ababa slaughterhouse. Moreover, limited information is available regarding the microbiological and epidemiological status of Escherichia coli (E. coli) in the study area. The primary objective of this study is to investigate the prevalence and antibiotic resistance of Escherichia coli (E. coli O157:H7) in poultry meat collected from a slaughterhouse.16
Materials and Methods
The investigation took place in Addis Ababa, the capital of Ethiopia and one of the largest cities in Africa. Addis Ababa holds particular prominence as the headquarters of the African Union and the former Organization of African Unity (OAU). Additionally, it houses the headquarters of the United Nations Economic Commission for Africa (UNECA) and several other continental and international organizations. Given its historical, diplomatic, and political significance for the continent, Addis Ababa is commonly referred to as “the political capital of Africa”.10 The climate of the area is close to that of the subtropical highlands, with average temperatures (16.4°C) slightly higher than those of the lower lands, and the average rainfall is 1165 mm per year. Geographically, the region is located at a latitude of 9° 01’ 28.80’ N and longitude of 38° 44’ 14.39’ E with an elevation of 2355 m (Figure 1).
 |
Figure 1 Map of the study areas. |
Study Animals
The animals included in this study are, Chickens slaughtered at Addis Ababa ELFORA, and municipal abattoirs. The samples were taken from chicken meat; intestinal contents, rinse water, slaughterhouse worker hands, equipment and environment (floor).
Study Design
A cross-sectional study design was conducted in Addis Ababa city from February 2021 to March 2023 to isolate, identify and determine the characteristics of Escherichia coli (E. coli O157:H7).
Sample Size Determination
The sample size was determined according to the formula given by.17 Since there was no similar study conducted in the present study area, the expected prevalence was 50%, and the absolute precision was 5%, with a 95% confidence interval.
where n = the needed sample size, Pexp = the expected incidence and d = the desired absolute precision. Substituting each value gives n = 384 (192 feces and carcass swab samples each). However, to improve the precision of the study, 90 samples (45 hand and knife swab samples) were taken purposefully and separately. Similarly, 25 tap water samples were collected from the slaughterhouse. Thus, the total number of samples collected and analyzed was increased to 516.
Sampling Techniques
A simple systematic random sampling technique was used, in which the identification codes of the individual slaughtered chicken meat were obtained. The number of chicken meats available during a particular day (N) was divided by the desired sample size (n) to obtain the sampling interval (k), ie, k=N/n. Thus, the individual sampling units were sampled every kth after randomly selecting the starting point of selection between one and k. In addition to the study concerning samples from chicken meat and from other sources (hand swabs, knife swabs and water samples), the questionnaire survey was also undertaken by allowing the workers of the slaughterhouse to participate in the questionnaire survey on a voluntary basis. In this study, samples such as fecal samples, carcass swabs, hand swabs, knife swabs and water samples were taken and analyzed.
Laboratory Protocols
Sample Collection, Transportation and Storage
Test tubes and cotton-tipped swabs, sterilized and saturated with regular saline water, were employed for sample collection. Pooled swabs from workers’ hands, equipment, and the environmental floor were collected using a sterile wooden cotton swab. These swabs were then inserted into 10 mL test tubes containing sterile buffered peptone water, serving as pre-enrichment media, and were left for 24 hours at 37°C. Proper coding based on the collection date, sample source, and type was applied, with sources categorized as animals, personnel, or equipment.
Aseptic techniques were consistently maintained throughout the sampling and handling processes, involving the use of sterile materials, flaming, and refrigeration. Samples were promptly analyzed to prevent unforeseen alterations, and identical samples underwent three analyses to verify contamination levels. For in-depth microbial studies, pure culture was employed. Prior to sterilization, receptacles with essential nutrients were devoid of contaminants, and water-containing solutions and equipment underwent autoclaving at 121°C for 15 to 20 minutes. Contamination checks were performed by incubating 5% of the batch media at 37°C for 18–24 hours. An icebox was utilized during sample handling collection and transportation to the Microbiology Laboratory of the National Animal Health Diagnostic and Investigation Center (NAHDIC). The performance of the media was checked using E. coli (ATCC, 25922) for MAC.
Isolation of Escherichia coli (E. coli O157:H7)
About 1 mL/g of aseptically obtained feces, carcass swabs, butcher hand swabs, knife swabs, and water samples were suspended in modified peptone water. Roughly 50 μL of the resulting mixture was then suspended in modified peptone water and streaked onto MacConkey agar. A single colony exhibiting a pink color from the growth on MacConkey agar was selected and cultured on Eosin methylene blue agar. Similarly, from colonies displaying distinctive metallic sheen appearances on Eosin methylene blue agar, a single colony was chosen and cultured on sorbitol MacConkey agar (Oxoid Ltd., Hampshire, UK). The plates were subsequently incubated at 37°C for 24 hours. Finally, colonies with a pale periphery or those appearing colorless were subjected to an indole test. Indole-positive isolates underwent further confirmation through serological testing on nutrient agar using latex agglutination.
Serological Identification of Escherichia Coli (E. coli O157:H7)
The confirmation of non-sorbitol-fermenting and indole-positive colonies, previously placed on nutrient agar, was conducted using a serological method called the Escherichia coli (E. coli O157:H7) latex agglutination test (Oxoid, Hampshire, UK). To perform this test, a drop of saline was added separately to designated areas for both the test and control reactions, ensuring no mixing with the dried latex reagents. A sterile single-use plastic loop was used to pick a portion of the colony for testing, which was then carefully mixed in the saline drop until a smooth suspension formed. This suspension was thoroughly blended with the dry latex spots using a paddle until fully dispersed across the reaction area. The test card was gently rocked for up to 60 seconds and observed for any agglutination. A positive result was noted if the latex particles clumped together within 1 minute, signifying the presence of Escherichia coli (E. coli O157:H7) in that specific sample. Conversely, a negative result was recorded if no clumping occurred and a uniform blue suspension persisted after 60 seconds in the test region.18
Antimicrobial Susceptibility Test
Using commercially available antimicrobial disks and following the guidelines for antimicrobial susceptibility testing, antimicrobial susceptibility tests were conducted using the standard disc diffusion technique.18 Ampicillin (10 μg), cephalothin (30 μg), ciprofloxacin (5 μg), chloramphenicol (30 μg), gentamicin (10 μg), kanamycin (30 μg), nalidixic acid (30 μg), sulfamethoxazole trimethoprim (30 μg), streptomycin (10 μg), and tetracycline (30 μg) were utilized in antimicrobial disks (HI media, India). Serologically confirmed colonies of Escherichia coli (E. coli O157:H7) isolates from pure fresh culture were transferred into a test tube containing 5 mL of Oxoid, England’s Tryptone Soya Broth (TSB) and incubated for 6 hours at 37°C to get the turbidity of the culture broth comparable to that of 0.5 McFarland standards (roughly 3×108 CFU/mL), the turbidity was often adjusted with sterile saline solution or by adding more isolated colonies.19
A Mueller-Hinton agar plate from Oxoid, England, was prepared following the manufacturer’s instructions. Subsequently, a sterile cotton swab was dipped into the bacterial suspension and rotated against the tube’s side to eliminate excess fluid. The swab was then evenly streaked in three directions on the plate’s surface. After the plates were air-dried, antibiotic disks were aseptically placed using sterile forceps. The disks were gently pressed onto the agar to ensure firm contact and were then incubated at 37°C for 24 hours. Following incubation, the diameter of the inhibition zone around each disk was measured using a digital caliper placed directly on the plates. The results were categorized as sensitive, intermediate or resistant based on a standardized table provided by the manufacturer.19
Questionnaire Survey
The respondents were consented verbally through the administration of semi-structured questionnaires, along with an explanation of the survey’s objectives. The selection of respondents was deliberate, considering the nature and stability of temporary employment in the chicken meat industry. In cases where respondents lacked literacy skills, interviews were conducted. The questionnaire primarily concentrated on evaluating meat sanitary handling procedures, encompassing aspects such as personal hygiene practices among workers, the presence of facilities for hygienic meat handling, the existence of waste disposal systems, and other pertinent issues commonly observed in slaughterhouses.
Data Management and Analysis
After conducting laboratory analysis and a questionnaire survey, the gathered data were coded and inputted into a Microsoft Excel spreadsheet (Microsoft Corp., Redmond, USA). Subsequently, the MS Excel data underwent analysis using STATA version 15 statistical software. Descriptive statistics, including frequencies, were examined. Furthermore, statistical associations between suggested risk factors and the prevalence of Escherichia coli (E. coli O157:H7) in fecal contents, carcass swabs, hand swabs, and knife swabs were determined using a Pearson chi-square test. Statistical significance was defined as a P value less than 0.05.
Verbal Informed Consent
To ensure compliance with ethical standards, it was imperative to confirm that verbal informed consent was deemed acceptable and duly approved by the ethics committee. This procedural step underscores our commitment to respecting the rights and autonomy of the participants involved in the study. Therefore, prior confirmation of the acceptability and approval of verbal informed consent by the ethics committee was sought and obtained, in accordance with established protocols. The verbal informed consent was given by Debre Tabor University, College of Agriculture and Environmental science research and community service coordinator.
Results
Prevalence of Escherichia coli O157:H7 as Associated with Risk Factors
A 5.2% was found to be the overall prevalence of Escherichia coli (E. coli O157:H7) from the 499 samples that were collected. Different categories had different prevalence rates of Escherichia coli (E. coli O157:H7), according to an analysis of the sample types. In particular, it was found that the prevalence of Escherichia coli (E. coli O157:H7) was 4.2%, 6.8%, 4.2%, 4.4%, and 2.2% in hand and knife swabs, feces, and water samples, respectively (Table 1).
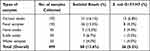 |
Table 1 Proportion of the E. coli and O157:H7 Serotypes in Different Types of Samples |
Antimicrobial Sensitivity Patterns of E. coli O157:H7
Ten antimicrobial agents’ patterns of antimicrobial susceptibility were examined. Numerous isolates from carcass samples were found to be susceptible to the chosen antimicrobial agents in different amounts, according to the study. From 26 Escherichia coli (E. coli O157:H7) isolates’ the overall antimicrobial resistance patterns showed high rates of resistance to streptomycin (47.5%) and ampicillin (40.8%). No resistance, however, were noted for kanamycin, gentamicin, and ciprofloxacin. The lowest rates of resistance were recorded in Cephalothin (1.5%), chloramphenicol (2.5%), and sulfamethoxazole trimethoprim (3.1%). According to the current investigation, it was found that approximately 57.6% of Escherichia coli (E. coli O157:H7) samples exhibited sensitivity to various antibiotics, while 11.7% displayed resistance to multiple antimicrobial agents, indicating resistance to two or more types of antimicrobials (Table 2).
 |
Table 2 The Serologically Positive Isolates of E. coli O157:H7 Exhibit Specific Patterns of Antimicrobial Sensitivity |
Five distinct sample types were collected with the primary aim of isolating Escherichia coli (E. coli) and exploring its antimicrobial resistance characteristics. Analysis of the overall antimicrobial resistance patterns for Escherichia coli (E. coli O157:H7) across these sample types revealed that isolates obtained from water and hand swabs demonstrated complete resistance (100%) to both streptomycin and ampicillin. Carcass swabs exhibited a resistance pattern of 53.8% for ampicillin, while Escherichia coli (E. coli O157:H7) from hand swabs displayed an equivalent resistance pattern of 66.7% for streptomycin and nalidixic acid. Remarkably, no resistance was observed in E. coli isolated from all sample types against kanamycin, gentamicin, and ciprofloxacin. This investigation underscores that approximately 53.8% of the sampled E. coli strains manifested resistance to an unspecified antimicrobial agent (Table 3).
 |
Table 3 Antibiotic Resistance Patterns of E. coli O157:H7 from Different Sample Types |
Questionnaire Survey Analysis
Workers in the slaughterhouse were asked about their hygienic status in the workplace. A total of 43 respondents, consisting of 39 males and 4 female workers, were interviewed. The survey showed that 31 (72%) of the respondents had completed primary school, 10 (23%) had completed high school, and the remaining 2 (5%) had graduated from a high school. Most of the respondents did not wash their hands during their working hours (44.2%), whereas approximately 25.6% of them reported that they washed their hands before commencement of slaughter activities. They were also interviewed to determine whether they used protective clothing during their work time in the slaughterhouse. Approximately 28%, 11.6% and 9.2% of the participants had boots, aprons and hairnets, respectively, whereas 35% of them had both overall and boots. In addition, to ensure that these survey participants had updated their understanding of the hygienic handling of meat, 77.40% of them had no training about hygienic handling, whereas 22.6% of the respondents indicated that they received training (Table 4).
 |
Table 4 Results from Questionnaire Survey |
Discussions
The present research demonstrated that Escherichia coli (E. coli O157:H7) was found in water samples, chicken carcasses, feces, as well as hand and knife swabs at rates of 4%, 6.8%, 4.2%, 4.4%, and 2.2%, respectively, resulting in an overall prevalence of 5.2%. The study highlighted a concerning risk of heightened Escherichia coli (E. coli O157:H7) presence specifically in chicken carcasses. Furthermore, the findings of this investigation mirrored the significant prevalence of Escherichia coli (E. coli O157:H7) infection in chicken meat, consistent with similar studies conducted in Addis Ababa, Bishoftu and Modjo by20,21 with overall prevalence of Escherichia coli (E. coli O157:H7) 4.2%.
The prevalence rate of Escherichia coli (E. coli O157:H7) in carcass samples was greater than that in fecal samples. And the prevalence rates of E. coli O157:H7 in fecal, hand and water samples were slightly similar. This result is in line with the findings of22 who reported that a higher prevalence rate of Escherichia coli (E. coli O157:H7) was recorded from carcass samples than from other types of samples. On the other hand, the findings of21 support the prevalence of Escherichia coli (E. coli O157:H7) in hand and knife swab samples. However, the finding by23 contradicts the present report regarding the prevalence rates of both hand and knife swab samples, which could be attributed to the level of sanitary procedures applied where the samples were collected.
Poor sanitation is the primary reason for the elevated presence of gut microflora elements, such as of Escherichia coli (E. coli O157:H7), in food products. It was evident that individuals involved in meat handling, particularly those working in slaughterhouses, were not adhering to proper hand washing practices. A significant number of meat handlers were neglecting the use of gloves or utensils when transferring meat to customers. Instead, they were using bare hands, and instead of washing their hands, they commonly opted to wipe them with a cloth. The prevalence of Escherichia coli (E. coli O157:H7) in samples obtained from supermarkets remained notably high. The increased occurrence of Escherichia coli (E. coli O157:H7) in this study could be attributed to inadequate food handling and substandard hygienic practices.6,22
All the isolates were sensitive to ciprofloxacin (100%), while a few isolates had varying resistance rates to some antimicrobial agents, such as ampicillin (53.8%), streptomycin (42.3%), tetracycline (11.4%) and nalidixic acid (15.4%). Similarly, most of the Escherichia coli (E. coli O157:H7) isolates that were collected from carcasses also exhibited susceptibility to many antimicrobial agents even though some Escherichia coli (E. coli O157:H7) isolates exhibited resistance to a few antimicrobial agents, such as ampicillin (53.8%), tetracycline (15.4%) and streptomycin (46.1%). The study also revealed that the Escherichia coli (E. coli O157:H7) isolates that were collected from carcass samples had an average sensitivity of 62.3%, despite the remaining isolates being intermediately susceptible (22.6%) and resistant (15.1%).
Furthermore, Escherichia coli (E. coli O157:H7) isolates from water, hand and knife swabs also showed resistance to some antimicrobial agents. For instance, 100% of the Escherichia coli (E. coli O157:H7) isolates from hand swab samples developed resistance to ampicillin. Similarly, 100% of the isolates from water samples were resistant to streptomycin, in contrast to the isolates from knife swab samples, in which 100% of the isolates were susceptible to all the antimicrobial agents. The study also revealed that, on average, the isolates from knife swab samples had higher intermediate sensitivity (40%) than isolates from other sample types, whereas the isolates from carcass swab samples had shown the highest susceptibility (62.3%) compared to isolates from other sample types.
The current study revealed that Escherichia coli (E. coli O157:H7) showed an AMR value of 96.2%, suggesting significant detrimental effects of mostly used antibiotics on patients. The high incidence of resistance to ampicillin and streptomycin in Escherichia coli (E. coli O157:H7) isolated from poultry meat indicates widespread antibiotic use. Common antibiotics are used in farm animals and veterinary medicine for various purposes, such as promoting growth, enhancing feed efficiency, reducing waste production, and preventing diseases. The repeated and unregulated use of antibiotics contributes to multidrug resistance in associated bacteria, potentially leading to the acquisition of antibiotic resistance genes. Additionally, the presence of antimicrobial residues can impact the normal microflora in host animals, allowing the proliferation of antibiotic-resistant bacteria over time.
In particular, Escherichia coli (E. coli O157:H7) can transfer resistance genes to other bacteria once antimicrobial resistance is acquired.11,24
Bacteria resistant to multiple drugs can pass on genes that confer resistance to antimicrobials to other bacteria present in the human intestinal microflora. This process might lead to the development of zoonoses characterized by acquired resistance. Escherichia coli (E. coli O157:H7) shows a specific mechanism of AMR through the production of extended-spectrum β-lactamases, which makes Escherichia coli (E. coli O157:H7) infections even more difficult to treat with fluoroquinolones, aminoglycosides, and trimethoprim sulfamethoxazole. Because of the resistance mechanisms involved, Escherichia coli (E. coli O157:H7) that produce ESBLs have the ability to render such antibiotics inactive. Due to widespread use of outmoded and low-cost antimicrobial drugs, the worldwide burden of antimicrobial resistance (AMR) has reached intolerable proportions. This usage pattern will increase if the required steps are not done in the near future. Compared to many other wealthy countries, the burden of the antimicrobial resistance (AMR) problem is notably higher in low-income countries where affordable antimicrobial medicines are frequently utilized to treat a wide spectrum of nosocomial infections.25–27
Several studies in the literature suggest the presence of AMR and a relatively similar level of AMR to support the findings of the present study in Escherichia coli (E. coli O157:H7) isolated from chicken meat.28,29 reported 78.06% AMR in Bangladesh, with ampicillin and tetracycline resistance (98.95% and 85.3%, respectively). Ampicillin resistance is found in most human cases and is caused by the presence of plasmid-encoded β-lactamases, such as TEM-1, TEM-2, or SHV-1, which can hydrolyze and inactivate amoxicillin and ampicillin drugs.30,31 Previous studies have suggested antimicrobial resistance by extended-spectrum cephalosporin (ESC)-resistant Escherichia coli (E. coli O157:H7) which is coresistant to ampicillin, chloramphenicol and tetracycline.22 Another study suggested that nearly 75% of ampicillin-resistant Escherichia coli (E. coli O157:H7) strains were also resistant to tetracycline.32 High resistance to ampicillin,33 tetracycline,34,35 and chloramphenicol has also been reported from Escherichia coli (E. coli O157:H7) specimens isolated from poultry samples due to increased usage of these drugs in commercial poultry.36
These findings support the theory that the colonization of ciprofloxacin-resistant Escherichia coli (E. coli O157:H7) in the human gut may be the cause of the high resistance to ciprofloxacin observed globally, which could be attributed to the increased use of quinolones on poultry farms.36 The usage of veterinary medications that structurally resemble gentamycin may be the cause of antimicrobial resistance to gentamicin. Tetracycline resistance may also exist in the ampicillin-resistant Escherichia coli (E. coli O157:H7) strain.36 Resistance to cephalosporin antibiotics is mainly associated with the extensive use of cephalosporins.36 Escherichia coli (E. coli O157:H7) isolated from fecal-contaminated water bodies shows significantly greater resistance to ampicillin, which indicates a high risk of ampicillin-resistant Escherichia coli (E. coli O157:H7) infections after the consumption of contaminated water from such water bodies.22
However, previous studies suggest that the level of resistance observed in human Escherichia coli (E. coli O157:H7) O157:H7 isolates is lower than that observed in Escherichia coli (E. coli O157:H7) isolates collected from poultry and animal samples.20,36 Although, the use of antibiotics as growth promoters in animal feed has been outlawed in the EU since 2016, certain nations continue to utilize common antimicrobial drugs to stimulate farm animal growth. Numerous frequently used antibiotics are easily obtained and available over-the-counter (OTC) without a prescription in a number of nations. Antimicrobial drug misuse is made easier by the public’s ease of access to over-the-counter medications without a prescription.22,23,37
Given the alarming nature of the multi-drug resistance (MDR) issue and the urgent need for effective measures to curb the continued emergence of multi-drug resistance (MDR) genes, various initiatives can be implemented to mitigate the acceleration of the AMR problem. Immediate actions should include the use of targeted antibiotics, responsible antibiotic use in veterinary medicine and poultry feed, adopting a rotational approach for antimicrobial agents, employing combined antimicrobial therapy in clinical settings, and promoting proper veterinary practices to discourage unnecessary use of antimicrobials and antibiotics through regulatory measures and monitoring systems. It is imperative to prevent antibiotic misuse by the public, implement antimicrobial surveillance programs, particularly for zoonotic infections, as mandatory steps to minimize the spread of antibiotic-resistant bacteria. The potential link between the antimicrobial resistance of multiple strains of Escherichia coli (E. coli O157:H7) found in poultry meat and edible organs and the presence of resistance genes on their plasmids should be considered.20,22,36
In this study, the attitudes and knowledge of the slaughterhouse workers were assessed using a questionnaire. The most important principles of maintaining carcass hygiene are to avoid contact between a carcass and contaminated environment and to ensure that the carcass is off the ground as soon as possible during the first steps of the slaughter process. Moreover, meat handlers need to know the presence of harmful microorganisms such as Escherichia coli (E. coli O157:H7) in the slaughter environment. Nevertheless, the majority of the participants in the present study had limited knowledge about these harmful microorganisms, which are at risk of meat contamination and are most likely related to their educational background. Meat is potentially subjected to contamination from a range of sources through the slaughtering process. Contamination may be associated with the animals themselves or may be introduced to a clean carcass through cross contamination. In this regard, the potential contaminants arising from slaughterhouse workers are assumed to be the major cause of meat contamination.38
The present survey revealed that the majority of workers at slaughter did not wash their hands or knives before slaughter. Even though they made contact with dirty materials that most likely resulted in meat contamination, they continued slaughter activities without washing their hands. This is due to the poor understanding and attitudes of workers regarding hygienic meat handling. Since the purpose of wearing overalls and other protective clothing is to protect both food products and meat handlers from cross contamination, overalls should be worn over other clothing.39 However, in this study, most of the workers were engaged in slaughter activities without wearing protective clothing. The basic reason forwarded was mainly the negligence of employers in providing these protective clothes to their workers. Nonetheless, microbiological contaminants, including Escherichia coli (E. coli O157:H7) are available on the body, and personal closure of the worker results in meat contamination; these findings are consistent with those of.40,41
Conclusion and Recommendations
During the present study, Escherichia coli (E. coli O157:H7) was isolated from fecal content, carcass, hand and knife swab samples at a considerable prevalence rate, which calls for due attention since it presents severe public health challenges. Additionally, carcass contamination was aggravated by the poor knowledge and attitudes of the workers regarding the implementation of sanitary meat handling procedures during slaughter operations. The antimicrobial sensitivity test showed that cephalothin, ciprofloxacin, gentamicin, sulfamethoxazole trimethoprim and tetracycline inhibited the growth of Escherichia coli (E. coli O157:H7) isolates at various concentrations. However, several Escherichia coli (E. coli O157:H7) strains developed multidrug resistance against antimicrobial agents, such as ampicillin, nalidixic acid and streptomycin. In addition, poor hygienic practices were observed for meat handlers, which might have implications for cross-contamination of meat.
Based on the above remarks, the following points are recommended:
- Improving workers’ knowledge and practices related to safe meat handling and distribution.
- The monitoring of antibiotic use in human and animal health may have a significant impact on the prevention and control of food-borne infections caused by antibiotic-resistant strains.
- Further studies evaluating the existing toxicity and virulence genes in Escherichia coli (E. coli O157:H7) isolates are recommended.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Germini A, Masola A, Carnevali P, Marchelli R. Simultaneous detection of Escherichia coli O175: H7, Salmonella spp., and Listeria monocytogenes by multiplex PCR. Food Control. 2009;20(8):733–738. doi:10.1016/j.foodcont.2008.09.010
2. Todd EC. Epidemiology of foodborne diseases: a worldwide review. World Health Stat Q. 2010;50(1/2):30–50.
3. Kaper JB, Nataro JP, Mobley HL. Pathogenic Escherichia coli. Nat Rev Microbiol. 2004;2(2):123–140. doi:10.1038/nrmicro818
4. Hiko A, Asrat D, Zewde G. Occurrence of Escherichia coli O157:H7 in retail raw meat products in Ethiopia. J Infect Developing Countries. 2008;2(05):389–393. doi:10.3855/jidc.203
5. Ahmad S, Yousaf M, Kamran Z, Sohail MU. Effect of feeding whole linseed as a source of polyunsaturated fatty acids on performance and egg characteristics of laying hens kept at high ambient temperature. Brazil Scie. 2019;15(1):21–25. doi:10.1590/S1516-635X2013000100004
6. Akbar A, Sitara U, Ali I, Khan MI, Phadungchob T, Anal AK. Presence of Escherichia coli in poultry meat: a potential food safety threat. Int Food Res J. 2018;21(3):941.
7. Manask AM, Schechter M. The Complete Guide to Foodservice in Cultural Institutions: Keys to Success in Restaurants, Catering, and Special Events. John Wiley & Sons; 2002:234.
8. Mauer WA, Kaneene JB, DeArman VT, Roberts CA. Ethnic-food safety concerns: an online survey of food safety professionals. J Environ Health. 2006;68(10):32.
9. World Health Organization. Shiga Toxin-Producing Escherichia Coli (STEC) and Food: Attribution, Characterization and Monitoring. Vol. 19. World Health Organization; 2018.
10. Centers for Disease Control and Prevention (CDC). Preliminary Food Net data on the incidence of foodborne illnesses--selected sites, United States, 2021. MMWR Morb. 2022;71(40);1260–1264.
11. Iancu I, Al Kaddah Y, Cătana N, Degi J, Pascu C, Herman V. Evaluation of antimicrobial resistance in strains of E. Coli isolated from broiler carcasses. Rev Rom Med Vet. 2018;28:35-38.
12. Majowicz SE, Scallan E, Jones-Bitton A, et al. Global incidence of human Shiga toxin–producing Escherichia coli infections and deaths: a systematic review and knowledge synthesis. Foodborne Pathogens Dis. 2014;11(6):447–455. doi:10.1089/fpd.2013.1704
13. Tsola E, Drosinos EH, Zoiopoulos P. Impact of poultry slaughter house modernization and updating of food safety management systems on the microbiological quality and safety of products. Food Control. 2020;19(4):423–431. doi:10.1016/j.foodcont.2007.05.003
14. Khan MA, Steiner TS. Mechanisms of emerging diarrheagenic Escherichia coli infection. Curr Infect Dis Rep. 2002;4(2):112. doi:10.1007/s11908-002-0050-y
15. Karch H, Tarr PI, Bielaszewska M. Enterohaemorrhagic Escherichia coli in human medicine. Int J Med Microbiol. 2005;295(6–7):405–418. doi:10.1016/j.ijmm.2005.06.009
16. Blagojevic B, Antic D, Ducic M, Buncic S. Ratio between carcass-and skin-microflora as an abattoir process hygiene indicator. Food Control. 2023;22(2):186–190. doi:10.1016/j.foodcont.2010.06.017
17. Thrusfield M. Veterinary Epidemiology.
18. Momtaz H, Dehkordi FS, Rahimi E, Ezadi H, Arab R. Incidence of Shiga toxin-producing Escherichia coli serogroups in ruminant’s meat. Meat Sci. 2013;95(2):381–388. doi:10.1016/j.meatsci.2013.04.051
19. Singh R, Schroeder CM, Meng J, et al. Identification of antimicrobial resistance and class 1 integrons in Shiga toxin-producing Escherichia coli recovered from humans and food animals. J Antimicrob Chemother. 2022;56(1):216–219. doi:10.1093/jac/dki161
20. Gashe F, Mulisa E, Mekonnen M, Zeleke G. Antimicrobial resistance profile of different clinical isolates against third-generation cephalosporins. J Pharm. 2018;2018:1–7. doi:10.1155/2018/5070742
21. Akond MA, Alam S, Hasan SM, Mubassara S, Uddin SN, Shirin M. Antibiotic resistance of Escherichia coli isolated from poultry and poultry environ- ment of Bangladesh. Am J Environ Sci. 2023;5:47–52.
22. Schlegelova J, Babak V, Holasova M, et al. Microbial contamination after sanitation of food contact surfaces in dairy and meat processing plants. Czech J Food Sci. 2010;28(5):450–461. doi:10.17221/65/2009-CJFS
23. Varela J, Cabrera-Diaz E, Cardona MA, et al. Isolation and characterization of Shiga toxin-producing E. coli O157:H7 and non-O157 from beef carcasses at a slaughter plant in Mexico. Int J Food Microbiol. 2021;113(2):237–241. doi:10.1016/j.ijfoodmicro.2006.06.028
24. Haile AF, Alonso S, Berhe N, Atoma TB, Boyaka PN, Prevalence GD. Antibiogram, and multidrug-resistant profile of E. coli O157:H7 in Retail Raw Beef in Addis Ababa, Ethiopia. Front Vet Sci. 2022;9:734896. PMID: 35280130; PMCID: PMC8907516. doi:10.3389/fvets.2022.734896
25. Rosa F, Oriol S, Alvar A, et al. The microbiome in respiratory medicine: current challenges and future perspectives. Eur Respir J. 2017;49(4):1602086.
26. Haileselassie M, Taddele H, Adhana K, Kalayou S. Food safety knowledge and practices of abattoir and butchery shops and the microbial profile of meat in Mekelle City, Ethiopia. Asian Pac J Trop Biomed. 2013;3(5):407–412. doi:10.1016/S2221-1691(13)60085-4
27. Abebe M, Hailelule A, Abrha B, et al. Antibiogram of Escherichia coli strains isolated from food of bovine origin in selected Woredas of Tigray, Ethiopia. J Bacteriol Res. 2021;6(3):17–22.
28. Hiwot D, Savoinni G, Donata C, Gabriella S, Martino P. Bacteriological quality of milk in raw bovine bulk milk in the selected milk collection centers: smallholder dairy processing Ethiopia. J Vet Med Anim Health. 2016;4(2):201.
29. Tassew H, Abdissa A, Beyene G, Gebre-Selassie S. Microbial flora and food borne pathogens on minced meat and their susceptibility to antimicrobial agents. Ethiop J Health Sci. 2021;20(3). doi:10.4314/ejhs.v20i3.69442
30. Olatoye O, Amosun EA, Ogundipe GA. Multidrug resistant Escherichia coli O157 contamination of beef and chicken in municipal abattoirs of Southwest Nigeria. J Nat Sci. 2022;10:125–132.
31. Taye M, Berhanu T, Berhanu Y, Tamiru F, Terefe D. Study on carcass contaminating Escherichia coli in apparently healthy slaughtered cattle in Haramaya University slaughter house with special emphasis on Escherichia coli O157:H7, Ethiopia. J Vet Sci Technol. 2023;4:132.
32. Tenover FC. Mechanisms of antimicrobial resistance in bacteria. Am j Med. 2019;119(6):S3–S10. doi:10.1016/j.amjmed.2006.03.011
33. Schroeder CM, Meng J, Zhao S, et al. Antimicrobial resistance of Escherichia coli O26, O103, O111, O128, and O145 from animals and humans. Emerg Infect Dis. 2002;8(12):1409. doi:10.3201/eid0812.0200770
34. Edge TA, Hill S. Occurrence of antibiotic resistance in Escherichia coli from surface waters and fecal pollution sources near Hamilton, Ontario. Can J Microbiol. 2015;51(6):501–505. doi:10.1139/w05-028
35. Sáenz Y, Zarazaga M, Briñas L, Lantero M, Ruiz-Larrea F, Torres C. Antibiotic resistance in Escherichia coli isolates obtained from animals, foods and humans in Spain. Int J Antimicrob Agents. 2001;18(4):353–358. doi:10.1016/S0924-8579(01)00422-8
36. Mohammed DS, Admasu P, Feyera T. Prevalence and antimicrobial susceptibility pattern of E. coli isolates from raw meat samples obtained from abattoirs in Dire Dawa city, eastern Ethiopia. Int J Microbiol Res. 2023;5(1):35–39.
37. Tadesse DA, Zhao S, Tong E, et al. Antimicrobial drug resistance in Escherichia coli from humans and food animals, United States; 1950–2002. Emerg Infect Dis. 2023;18(5):741. doi:10.3201/eid1805.111153
38. Solomon EB, Yaron S, Matthews KR. Transmission of Escherichia coli O157:H7 from contaminated manure and irrigation water to lettuce plant tissue and its subsequent internalization. Appl Environ Microbiol. 2022;68(1):397–400. doi:10.1128/AEM.68.1.397-400.2002
39. Bersisa A, Tulu D, Negera C. Investigation of bacteriological quality of meat from abattoir and butcher shops in Bishoftu, Central Ethiopia. Int J Microbiol. 2019;492:234.
40. Surra G, Dereje T, Chaluma N. Isolation and identification of Escherichia coli, Salmonella and Pasteurella from holding grounds of live-bird markets at Addis Ababa, Ethiopia. Afri J Microbiol Res. 2018;12(31):754–760. doi:10.5897/AJMR2018.8892
41. Clinical and laboratory standards institute. Clinical and laboratory standards institute: performance standards for antimicrobial susceptibility testing supplement M100S. In: D’Mello JF, editor. Food Safety: Contaminants and Toxins. CABI; 2022.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

