Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 14
Incidence, Outcome and Determinants of Unplanned Extubation Among Pediatric Intensive Care Unit Addis Ababa, Ethiopia, 2023: Nested, Unmatched Case-Control Study Design
Authors Mekonnen AS , Kebede Z, Demissie DB
Received 31 July 2023
Accepted for publication 21 October 2023
Published 26 October 2023 Volume 2023:14 Pages 347—359
DOI https://doi.org/10.2147/PHMT.S429457
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Laurens Holmes, Jr
Aster Shawel Mekonnen,1 Zegeye Kebede,2 Dereje Bayissa Demissie3
1Schools of Nursing, Yekatit 12 Medical College, Addis Ababa, Ethiopia; 2Schools of Nursing, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia; 3Department of Neonatal, School of Nursing, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia
Correspondence: Dereje Bayissa Demissie, Department of Neonatal Nursing, School of Nursing, St. Paul’s Hospital Millennium, P.O. Box 1271, Addis Ababa, Ethiopia, Tel +251 912189560, Email [email protected]
Background: Unplanned extubating is the most common adverse event occurring in intensive care units (ICUs) and significantly increases morbidity and mortality in children, but there is limited current evidence on unplanned extubating in Ethiopia. Therefore, this study aimed to determine the incidence, outcome, and determinants of unplanned extubating among children in the pediatric intensive care unit in Addis Ababa, Ethiopia, in 2023.
Methods: A nested unmatched case–control design study was conducted at selected government hospitals in Addis Ababa from September 1, 2022, to April 30, 2023. A total of 198 intubated child patients (66 cases of unplanned extubating were nested with 132 controls of planned extubating) were followed up until they completed the full weaning process or based on hospital protocols. Data was collected through standardized data extraction, and the data was cleaned, entered into Epidata version 4.6, and exported to SPSS version 25.0 for further analysis. Binary and multiple logistic regression analyses were used to identify determinants of unplanned extubating, with an adjusted odds ratio (AOR) of 99% confidence interval (CI) at p value < 0.01.
Results: The study revealed a high mortality rate of 15.65% among intubated children in pediatric intensive care units, and the incidence of unplanned extubating was 7.2 per 100 days. This study identified determinants of unplanned extubating among patients admitted to the pediatric intensive care unit: agitated patients (AOR = 3.708; 99% CI: 1.401– 9.81), working in night shift hours (AOR: 8.789; 99% CI: 2.37– 32.58), use of plaster or roll bandages separately (AOR = 4.12; 99% CI: 1.215– 13.96), A nurse-to-patient ration 1:2 (AOR: 6.65, 99% CI: 1.87– 23.69), intermittent sedation (AOR, 3.717; 99% CI, 1.017– 10.816), physically restrained (AOR = 3.717; 99% CI: 1.02– 13.54), and death outcome (AOR = 14.86, 99% CI: 3. 24– 68.097), respectively.
Conclusion and Recommendations: This study found that the incidence and mortality rate of unplanned extubating were high, with identified determinants increasing the risk of unplanned extubating among patients admitted to pediatric intensive care unit. Therefore, policymakers and health planners should design further protocols and algorithms for the management of pediatric endotracheal intubation (ETT) quality of patient outcomes and to prevent unplanned extubating in a resource limited set up.
Plain Language Summary: Unplanned extubating is a common adverse event in intensive care units that affects critically ill patients and increases morbidity and mortality rates. This study aimed to identify the determinants of unplanned extubating among children in Addis Ababa, Ethiopia, in 2023. This follow-up, unmatched case–control study included 198 intubated children, with 66 cases and 132 controls. The study used binary and multiple logistic regression analyses to identify determinants of unplanned extubating, and the Kaplan–Meier curve to determine survival outcomes. This study determined that the incidence of unplanned extubating was high, with identified determinants increasing the risk of unplanned extubating among patients admitted to pediatric intensive care units, such as agitation, night shift, intermittent sedation, endotracheal tube (ETT) taping by plaster or roll bandage separately, physical restraint, and the type of endotracheal tube (uncuffed). Therefore, policymakers and healthcare planners should consider these determinants during pediatric care unit training and guideline development for pediatric endotracheal intubation (ETT) mechanical ventilation outcomes.
Keywords: unplanned extubation, incidence, outcome, pediatric intensive care unit and determinant
Introduction
Airway management has been a concern for clinicians because of remarkable advances in airway management in recent years. As a result of the development of life-threatening conditions, endotracheal intubation and mechanical ventilation (MV) have become routine practices in pediatric intensive care units (PICU).1
Unplanned extubation (UPE) is a frequent event after endotracheal intubation for respiratory support in critically ill patients and is associated with increased morbidity and mortality, as indicated by most studies.2 Unplanned extubation involves unintentional and uncontrolled dislodgement of the patient’s breathing tube, which occurs outside the weaning process and leads to life-threatening hypoventilation and hypoxia.3 As the study shows that in general endotracheal tube usage is associated with several complications.4
Planned extubation was performed when patients were weaned off the ventilator by reducing mandatory breaths and pressure support by a measure of two spontaneous breathing trial was initiated when pressure support 8 cmH2O, mandatory breaths 8/min, FiO2 <50%, positive end expiratory pressure 4–5 cmH2O on the MV, hemodynamically stable, and other conditions fulfilled per our ICU protocol.5,6
Globally, the incidence of UPE is estimated to be 3–16% in mechanically ventilated children in the intensive care unit (ICU) setting.2 A prospective, case-controlled multicenter study conducted in the United States showed that 189 UPE cases occurred after 25,500 endotracheal tube days or 0.74/100 days, with 654 associated controls. The UPE rates ranged from 0.3 to 2.1 per 100 endotracheal days. Age <6 years increased the rate by 0.4, and 60% of UPE need re-intubation.7
Another related study in London, UK, showed that the incidence of unplanned extubation was 0.8 per 100 ventilator days or 243 UPE in 12,585 ventilated patients, and the rate of reintubation among children with UPE was significantly higher than planned extubation (50% vs 10%), with a trend toward high mortality (3% vs 1.3%), respectively.8
A study in South Africa of 233 intubated patients was conducted in both adult and pediatric ICU during the six months study period. Twenty-four patients (10.3%) experienced an unplanned extubation. Six of the 24 patients (25%) were re-intubated for respiratory failure, the event was more frequent in children.9
In a study conducted in Addis Ababa, Ethiopia, on characteristics and outcomes of mechanically ventilated pediatric patients, unplanned extubation accounted for 1.4% out of 202 patients.10 A study in Southern Ethiopia on the factors affecting prolonged intensive care unit stay showed that unplanned extubation was strongly associated with prolonged ICU stay.11
The determinants of unplanned extubation include agitation, endotracheal tube (ETT) manipulation, prolonged mechanical ventilation (MV), lack of physical restraint, previous UPE events, procedures prior to UPE, sedation concern, endotracheal tube type and nurse–patient ratio.6,12 Most studies have shown that unplanned extubation can cause serious adverse events, including hemodynamic instability, increased duration of mechanical ventilation, ICU length of stay, and complications from re-intubation (risk of cardiopulmonary resuscitation, tracheostomy, and death).7,8,10,13,14
The primary objective of this study was to identify determinants of unplanned extubation in pediatric care unit. This study also addressed the following questions, what are the determinants of unplanned extubation? What happens after UPE? What is its incidence in the pediatric intensive care unit (PICU)?
This is very important and the cornerstone for improving the quality of service and decreasing the mortality rate of mechanically ventilated children. To the best of our knowledge, this is the first study on unplanned extubation and its determinants in Ethiopia. Therefore, at the end of this study, patients will benefit from improvement in endotracheal tube (ETT) care to prevent UPE, and it can avoid or minimize intubated patients from disability and death caused by UPE. Additionally, hospital staff members will benefit from the research result by gaining knowledge, especially regarding the determinant factors of UPE and used as input data for UPE interventions implementations. This study also helped to clearly define the problems related to the use of mechanical ventilators and to provide information about the outcomes of UPE and can also serve as a baseline for any large-scale study conducted at university level.
Conceptual Framework
This conceptual framework was developed by reviewing literature that is previously published on a particular subject from reputable sources, which measured the objectives of this study3,6–8,15,16 seed details in Figure 1.
 |
Figure 1 Conceptual framework: Determinants of Unplanned extubation (UPEs) among pediatric intensive care unit Addis Ababa, Ethiopia 2023. |
Methodology
Study Area and Period
The study was conducted at St. Paul’s Hospital Millennium Medical College and Yekatit 12 Hospital Medical College from September 1, 2022, to April 30, 2023, in 8 and 4 bedded pediatric intensive care units (PICU) in two hospitals respectively in Addis Ababa (Ethiopia’s capital city).
St. Paul’s Hospital was established in 1969, with the help of the German Evangelical Church to serve the poor. The school opened and became a higher education institution in 2007Gc under the Ethiopian Federal Ministry of Health (EFMOH), which is the largest specialized hospital in Ethiopia. It provides a tertiary-level referral hospital with over 700 beds and serves as the training center for undergraduate and postgraduate students. The pediatric intensive care unit (PICU) is located in the new MCH building on the fourth floor, with eight beds, and treats 300–350 children annually.
The Y12HMC, established in 1915, began its service with 25 beds. Since 1987, this hospital has been governed by the Addis Ababa City Administration Health Bureau; in 2003, it was named the Y12 Hospital Medical Science College and served more than 5 million people in the catchment area. The paediatric intensive care unit (PICU) was established on January 23, 2011, and was found on the fifth floor of the new building. It is the first paediatric ICU from the six hospitals of AACHB. They have four beds and nearly 180–200 children are admitted annually.
Study Design
Nested unmatched case–control study design was conducted in the pediatric intensive care unit from September 1, 2022, to April 30, 2023. A total of 198 patients (66 cases and 132 controls) were consecutively admitted to the pediatric intensive care unit (PICU) and met the following conditions: age between 1 month and 14 years and need for invasive mechanical ventilation for at least 12hrs. Patients with tracheostomy and those who died on a mechanical ventilator without planned or unplanned extubation were excluded.
Sample Size Determination
The sample size is calculated by inserting different predictors of unplanned extubation variables from a previous case–control study by using Epi-Info version 7.2 (1:2 cases-to-control ratio) with the assumption of 99% confidence level, 80% power of the test. The maximum sample size obtained was 201, with 134 controls and 67 case participants with 10% non-response rate.
Methodology for Selection of Cases and Control
All pediatric patients admitted in the two public teaching hospitals who was intubated, were included in the follow-up up to facing the event then if the patient faced unplanned extubation find the determinants based on the data collection tool retrospectively and follow the outcome up to leaving the PICU and two controls (planned extubation) selected with the following of one case conveniently during data collection time, and the hospital was selected by lottery method from having of organized pediatric (PICU) in Addis Ababa public hospitals seed details in Figure 2.
 |
Figure 2 Sample size and distribution of patients admitted and intubated in pediatric intensive care unit (PICU), Addis Ababa. Ethiopia 2023. |
Data Collection
For avoiding missing data, data were collected at the time of the event by classified into three sections. First, clinical characteristics, such as age, sex, diagnosis on admission, MV duration, severity, and outcome, were recorded for each patient. Second, daily monitoring was conducted at the bedside by the attending physician and nurses, who noted numerous clinical and therapeutic data, such as tracheal tube type and fixation used, ventilator support mode, use of intravenous sedation, route of intubation, and patient mobility, from daily physician-revised notes and hourly nursing follow-up sheets and finally, every time a UPE event occurred, a specific questionnaire was immediately delivered and completed by an attending physician or nurse. Time, date, mode of ventilator support, sedation, nurse-to-patient ratio, and specific circumstances. After UPE, the following complications were recorded: re-intubation, cardiopulmonary resuscitations, other complications, and death.
For the above data collection processes, two data collectors were prepared for each hospital working in the pediatrics intensive care unit (PICU) during the study period.
Operation Definitions
Planned extubation (PE) (control) was defined as admission to the pediatric intensive care unit, intubation equal to or greater than 12 hours, and removal of the endotracheal tube after a physician’s order, according to hospital policies and procedures.
Unplanned extubation (UPE) (case) is defined as the premature removal of an endotracheal tube by healthcare professionals, caregivers, or patients itself.
Reintubation is defined as replacement of the endotracheal tube within 24 hrs. of planned extubation (PE) or unplanned extubation (UPE).
Agitation is defined as excessive restlessness/excitement and increased motor activity before event.
Sedation is defined as a state of depression. Awareness of the environment and reduction of his or her responsiveness to external stimulation were prescribed by the physician for intubation for b Endotracheal tube (ETT)er synchrony with MV. In children, the order can be: Continuous (on continuous IV infusions of sedation before UPE) or intermittent sedation included BID, daily, QID, or a specified interval of time, endotracheal tube (ETT), and PRN (at any time the patient becomes awake or agitated).
Data Quality Assurance
A properly designed and structured data abstraction tool is used. The data collectors were health professionals or pediatric intensive care unit (PICU) nurses for better understanding and interpretation of the patients’ medical charts and follow-up sheets and additionally it provides a one-day training about the overall data collection process. A pre-test was carried out using 5% of the estimated sample at Yekatit 12 Hospital Medical College for its clarity, understandability, and completeness of the tool. Some parts of the collection tools have been revised and adjusted.
Data Analysis
The data were checked for completeness and consistency, cleaned, coded, entered using EpiData version 5.4, and exported to the SPSS software version 25 for analysis.
A chi-squared test was performed to determine the association between independent and dependent variables. Hosmer and Lemeshow were used to test the model fitness. Multicollinearity was assessed using the variance inflation factor. Bivariate binary logistic regression and multivariable binary logistic regression analyses were performed to assess the association between outcome and independent variables. On bivariate logistic regression analysis, a P-value <0.0.01 was considered a candidate for multivariable binary logistic regression analysis.
Multivariable logistic regression analysis was performed to identify independent determinants of unplanned extubation. Crude odds ratio (COR) and adjusted odds ratio (AOR) were determined. An AOR with 99% confidence interval (CI) was computed to identify the presence and strength of associations, and statistical significance was set at P < 0.01.
Results
Socio-Demographic Characteristics
A total of 389 patients were admitted to the pediatric ICU, of whom 241 were intubated for more than or equal to 12 h and underwent both PE and UPE extubation from September 1, 2022, to April 30, 2023. A total of 198 (132 controls and 66 patients) were included in this study, with a 98.5% response rate, which is acceptable because we added 10% attrition rate. There were 96 unplanned extubation events were observed in the 66 patients. Of these 66 children, each of the two patients experienced six unplanned extubations, other each two patients had three unplanned extubations and the other six patients had two unplanned extubations. The minimum age of facing unplanned extubations was one month, and the maximum age was 168 months (14 years), with a mean age of 27.31 months, a median age of nine months, SD: 38.9 and 116 (59%) of admissions to the pediatric intensive care unit (PICU) were male.
The incidence of unplanned extubations among children in the pediatric intensive care group was 39.8/100 (96/241) per person-day; in other words, the patients were ventilated for a total duration of 1321 days within the incidence of (7.2 UPE per 100 intubation days. The analysis was performed on 132 controls and 66 single cases (UPE)).
The most common causes of admission to the pediatric intensive care unit (PICU) were respiratory problems (mean, 49%), sepsis (32%), and neurological problems (10%), and cardiovascular problems accounted (7%). All patients with unplanned extubations had been orally intubated, no patients in the unit intubated nasally, and 187 (94.4%) of patients intubated with cuffed endotracheal tube (ETT). The patient-to-nursing ratios varied between 1:1 and 2:1. The most common type of mechanical ventilator mood was spontaneous intermittent mandatory mechanical ventilation (SIMV) used by 75.7% and next 12 (6%) was pressure regulated volume control ventilation (PRVC) but not significantly associated with UPE.
Of the total planned and unplanned extubated patients, 59 needed re-intubation, 46 (69.7%) vs 13 (9.85%) after UPE and planned extubation (PE), respectively. Of the 59 patients, 20 of them needed re-intubation within 1 h, 20 patients needed re-intubation + CPR + cold medications, 8 faced difficulty in re-intubation, and 11 pts need re-intubation after 1 h. See Table 1.
 |
Table 1 Socio-Demographic Characteristics and Circumstances of Unplanned Extubation Among Children in Pediatric Intensive Care Unit, Addis Ababa, Ethiopia from Sep 2022 to Apr 2023 |
The minimum stay on mechanical ventilation was 2 days, and the maximum was 30 days, with a mean of 6.67 days, a median of 5 days, and an SD of 4.3. The minimum pediatric intensive care unit stay was 2 days, with a maximum of 40 days, a mean of 9, a median of 8, and an SD of 5.8 days. Of the total 198 patients, 89% of the patient stayed in pediatric intensive care unit less than 14 days and 94% of the patients were mechanically ventilated for less than 14 days. See Table 1
Of the total 66 cases, 78.8% of UPEs occurred during acute endotracheal tube (ETT) and the remaining 21% occurred at the time of weaning endotracheal tube (ETT). Twenty-four (36.4%) UPEs occurred at night. Thirty-one (46.97%) UPEs occurred at the time of different nursing procedures like endotracheal tube (ETT) adjustment 8 (12%), suctioning 5 (7.6%), positioning 4 (6%), hand-over/round 7 (10.6%), line placement,1 and other 6 (9%) during new patient admission. See Figure 3.
 |
Figure 3 Producers Aactivities at a time of unplanned extubation at the selected public hospital in Addis Ababa City, Ethiopia, 2022. |
Determinants of Unplanned Extubations
The multivariate logistic analysis was performed using the significant variables in the binary logistic regression, and various determinant factors of UPE were differentiated under the model of (higher Hosmer–Lemeshow test, P=0 0.649).
Agitated infants and children were 3.7 times more likely at risk of unplanned extubation compared to infants and children who were not agitated (AOR = 3.708; 99% CI: 1.401–9.81).
Working in night shift hours was 8.8 times more likely to result in unplanned extubation than working in day shift (AOR: 8.789; 99% CI: 2.37–32.58).
The use of plaster or roll bandages separately for endotracheal tube fixation or taping was four times more likely at risk of unplanned extubation compared to taping with both plaster and roll bandages together (AOR = 4.12; 99% CI: 1.215–13.96).
This study also found that patients intubated with an uncuffed endotracheal tube were six times more likely to undergo unplanned extubation than those intubated with a cuffed endotracheal tube (AOR: 6.45; 99% CI: 1.275–32.62).
A nurse-to-patient ration 1:2 was 6.65 times (AOR: 6.65, 99% CI: 1.87 −23.698) more likely at risk to faced unplanned extubating than those the nurse-to-patient ration of 1:1 at a time of event.
Infants and children who were intubated and received intermittent sedation were three times more likely to develop unplanned extubation than those who received continuous sedation (AOR, 3.717; 99% CI, 1.017–10.816).
Infants and children who were physically restrained during mechanical ventilation were 3.7 times more likely at risk of developing unplanned extubation compared to those who were not physically restrained (AOR = 3.717; 99% CI: 1.02–13.54).
Finally, infants and children who had died were 12.82 times more likely to have unplanned extubating compared to those who were alive and discharged (AOR = 14.86, 99% CI: 3.24–68.097). See Table 2.
 |
Table 2 Determinants of Unplanned Extubation Among Children in Pediatrics Intensive Care Unit in Addis Ababa, Ethiopia, 2023 |
Subsequent Complications and Outcomes of Unplanned Extubations
The study found prolonged pediatric intensive care unit (PICU) stays and mechanical ventilation days that faced unplanned extubation compared to plan extubation (8.9:9.3 and 6.5:7.0) control-to-case ratio, respectively, or in the rate difference of 0.4 and 0.5, respectively. Of 198 intubated patients, 59 of them needed re-intubation (69.7% and 9.8% re-intubation UPE and PE, respectively). Table 3.
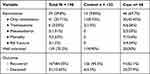 |
Table 3 Outcomes of the Patients Experienced UPE Compared to the Unmatched Control Participants 2023 |
After the event of both PE and UPE, 41 (20.7%) of the patients were successfully reintubated. Seven (3.53%) died, six (3%) tracheostomy, two (1.01%) rib fractures, and three (1.5%) died. All mortalities, pneumothorax, and rib fractures were associated with UPE. Figure 4.
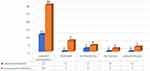 |
Figure 4 The immediate outcomes of after unplanned and planned extubation among Pediatrics Intensive Care Unit in Addis Ababa, Ethiopia, 2023. |
The study found that the overall mortality rate of intubated children admitted to the pediatric intensive care unit was 15.65% (31/198), with disproportionately high case-control revealed that the majority of 25 (37.9%) were from unplanned extubating or cases, and only 6 (4.5%) were from the control groups or planned extubating. See Figure 5.
 |
Figure 5 Recovery and death of the patients experiencing unplanned extubation compared to the unmatched control participants 2023. |
Discussion
This nested case–control study assessed patient, health care and sociodemographic determinants of unplanned extubation among children in a pediatric intensive care unit. The majority of pediatric patients admitted to the pediatric intensive care unit (PICU) were aged <6 years, which is in line with a study conducted in Philippines and Brazil.14,17
The present study shows the incidence of unplanned extubation was 39.8% or 7.2 UPE per 100 intubation days, which was greater compared to other similar studies conducted in Brazil, London, and United States.4,6,8 This may be related to the higher threshold for intubation, differences in the clinical setup, patient conditions, and training differences among health professionals.
Of the total of unplanned extubations, 21.2% occurred during the weaning ventilation setting. A possible justification for this during the weaning process is the inappropriate reduction in sedative drugs, prolonged weaning time, failure of early weaning initiation and early extubation, and decrease in caregiver concentration because the patient becomes more stable than at the beginning of the patient’s condition.
Thirty-one (46.97%) unplanned extubations occurred at the time of different nursing procedures such as endotracheal tube adjustment, suctioning, positioning, handover/round, and during new patient admission compared to a study done by Se´rgio and da Silva,17 and our study results were higher. This may also be due to inadequate training and skills of nurses regarding suctioning, care for mechanically ventilated patients, excessive endotracheal tube (ETT) manipulation, lower nurse–patient ratio, setup difference, and incoordination during an event occurring in one of the other patients.
This study found that patient agitation is a paramount importance in anticipating unplanned extubation. This finding is supported by studies conducted in other countries.6,15,16,18 This could be because, when patients are agitated, they become unstable and experience unnecessary movements. This movement leads to accidental removal of the endotracheal tube (ETT) or by the action of the patient, and no adequate sedation protocols and pain management protocols were found, as evidenced by visualizations of the use of sedation and pain management protocols at the time of supervising the data collection process. Moreover, the clinician challenging the measures to estimate the balance between agitation and fear of sedation may cause further complications such as cardiovascular compromise, prolonged paralysis, and prolonged mechanical ventilation.
Our study results showed that there was a marked difference in the type of endotracheal tube (ETT) fixation device; plaster or roll bandage usage separately increased the risk by four times compared with the use of both plaster and roll bandages together. The literature has highlighted for this as an important risk factor in endotracheal tube (ETT) fixation practice,7 but no numeric explanation has been found regarding the device. The reason may be the standardization of the ICU setup and the unavailability of taping devices for fixing the endotracheal tube (ETT) in the appropriate place, as the health professional also has less power to remove and only secured by plaster and in the patient. If contact with secretion the plaster becomes easily detached and pulls out of the endotracheal tube (ETT).
The present study revealed that night shifts were significantly associated with unplanned extubations. This finding was supported by a previous study.6 The reason for this could be that staff assigned for night shift work for a longer time than staff working on day shift, which causes exhaustion, decreases the number of staff at night because of classifying time in two halves, and the ratio becomes 1:2 because of the biological sleep-wake cycle. In addition, patients may be disturbed by excessive lighting, ventilator alarms, and monitoring at night.
Physical restraint use was significantly associated with unplanned extubation. This finding is in agreement with those of previous studies.3,6–8 This may be because physical restraint increases feelings of discomfort, stress, and anxiety due to the inability to express themselves by moving their hands or bodies. Another reason could be that restraining patients is considered a preventive strategy for unplanned extubation in agitated patients without appropriate and adequate sedation.
Another significant association was found in the case of intermittent sedation, which was three times more likely than that of continuous sedation. In a similar study, continuous sedation was more effective.6,10 This discrepancy may be due to differences in the set-up of sedation protocols, unavailability of sufficient sedation drugs, population differences, and health professionals, as well as the endotracheal tube (ETT)er to order sedation in PRN based on fear of complications and then missed and ignored by assuming that the infant has less power to remove endotracheal tube (ETT).
Furthermore, an uncuffed endotracheal tube was significantly associated with unplanned extubation compared to a cuffed endotracheal tube. This finding is consistent similar with those of previous studies.6–8,10 This may also be due to the inability to fix the endotracheal tube properly because of the loss of function of the inflation valve inside the trachea.
This study also found that the overall mortality of patients in the case of unplanned extubation was increased by 12.8 times compared to planned extubation. The mortality rate was higher than that in other similar studies,8,12,16 which may be explained by resource scarcity, inadequate ICU-trained nurses, and after UPE, the patient became hemodynamically unstable due to hypoxia, fights for re-intubation, difficulty in re-intubation, exacerbation of clinical conditions, and death.
This found in this study nurse-to-patient ratio 1:2 had significantly associated with the incidence of unplanned extubating. This finding was supported by previous study done in Great Britain in 20196 and Fontanez-Nieves.7 In these study settings, the staff ratio becomes 1:2 on the night shift, and the majority of unplanned extubations also happen during the night shift. The reason for this could be that staff assigned to the night shift are working longer than staff working the day shift and become exhausted, resulting in a decrease in the number of staff at night b/c of classifying time in two halves and the ratio becoming 1:2 because of the biological sleep-awake cycle. In addition, during the night, the patient may be disturbed by the alarming sound of the ventilator and monitoring.
This study also found that the overall mortality rate from the total 198 pts was 31 (15.7%). The rest 183 (84.34%) were improved, 25 (38%) were related to UPE as compared to 6(4.5%) in PE. Or the risk was increased by 15 times compared to those planned extubation. The mortality rate was higher than similar studies, this high mortality rate in this study area may be explained by resource scarcity, inadequate PICU trained professionals, and after UPE the patients become hemodynamically unstable due to hypoxia and fights for re-intubation and faced difficulty of reintubation and exacerbate the clinical conditions and leads to death.
Strength and Limitations
Data were collected at the time of the event and prospectively to obtain complete information on UPE events, and this study was purposefully investigated the determinants of UPE to help healthcare facilities and researchers inform the development of their own implementation framework to reduce UPEs and improve patient outcomes.
The limited availability of previous case–control studies on this topic may influence the comparison of our outcomes to those of other studies (population similarity), and some variables not included in this study may have influenced the occurrence of UPE, such as the presence of caregivers or family members at the bedside when the UPE episode occurred, nursing work experience, and floating nurses from other units (rotation). Further studies incorporating these variables may provide additional information.
Conclusion and Recommendation
This study found that the incidence and mortality rate of unplanned extubating were high, with identified determinants increasing the risk of unplanned extubating among patients admitted to pediatric intensive care unit. The identified determinants that increased the risk of unplanned extubation among intubated pediatric patients admitted to pediatric intensive care units includes being agitated, night shift, intermittent sedation, endotracheal tube (ETT) taping by plaster or roll bandage separately, having of physical restraint, and nurse-to-patient ratio.
This study also identified unplanned extubating as having a multifactorial etiology. Therefore, if patients are identified as having a high risk for UPE, temporarily intensified surveillance and prevention are important. Therefore, policymakers and health planners should design further protocols and algorithms for the management of pediatric endotracheal intubation (ETT) quality of patient outcomes and to prevent unplanned extubating in a resource limited set up.
Health professionals working in pediatric intensive care unit should undertake surveillance of these identified determinants to improve pediatric intensive care unit outcomes. Do not restrain the patients rather follow appropriate sedation protocols and make the patient comfortable, calm, and pain-free, use roll bandage and plaster together instead of separate use during endotracheal tube taping and special attention should be paid to early intubation, weaning, and extubation based on hospital protocols.
Policymakers should consider these identified determinants of unplanned extubation during intensive care unit training and develop guidelines for endotracheal tubes (ETT) and mechanical ventilation outcomes.
Abbreviations
AACHB, Addis Ababa city health bureau; CCU, Critical care unit; EFMOH, Ethiopian federal ministry of health; ETT, Endotracheal tube; ICU, Intensive care unit; MV, Mechanical ventilation; OI, Oxygen index; PE, Planned extubation; PICU, Pediatrics intensive care unit; SE, Self extubation; SPHMMC, St. paul’s hospital millennium medical college; TT, Tracheostomy tube; UPE, Unplanned extubation; Y12HMC, Yekatit 12 hospital medical college.
Ethics Approval
Ethical approval was obtained from St. Paul Hospital Millennium Medical College Ethical Review Board (Ref. No. Pm 23/417), this requirement was not waived by the Institutional Review Board and confirmed that all experimental protocols were approved by St. Paul’s Hospital Millennium Medical College Institutional Ethical Review Board.
Informed Consent
The authors confirmed that written informed consent was obtained from all subjects aged greater than 18 years, and for minor subjects less than 18 years old prior to study initiation and written inform consent was obtained from their parent or legal guardian(s) or legally authorized representatives before the study. Authors had confirmed that all methods were carried out in accordance with relevant guidelines and regulations of Helsinki Declaration. Authors had confirmed that all experimental protocols were approved by St. Paul Hospital Millennium Medical College Institutional Review Board/Ethics Committee (Ref. No. Pm 23/417).
Acknowledgment
First, thank the Almighty God for his grace and blessings. Our deepest gratitude goes to Saint Paul’s Hospital, Millennium Medical College, for the financial support and pursuit of this opportunity. The authors would also like to express their gratitude to the pediatrics intensive care unit (PICU) facilities in Addis Ababa, data collectors, supervisors, and study participants.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by the Saint Paul’s Hospital, Millennium Medical College. However, the funder had no role in the study design, data collection, analysis, preparation of the manuscript, or the decision to publish.
Disclosure
The authors(s) declare no potential conflicts of interest with respect to the research, authorship, or publication of this article.
References
1. Kapadia FN, Bajan KB, Raje KV. Airway accidents in intubated intensive care unit patients: an epidemiological study. Crit Care Med. 2000;28(3):659–664. doi:10.1097/00003246-200003000-00010
2. Debaisi GE. Impact of a quality improvement intervention on the incidence of unplanned extubations in a Pediatric Intensive Care Unit. Arch Argent Pediatr. 2013;111(5):391–397. doi:10.5546/aap.2013.eng.391
3. de Groot RI, Dekkers OM, Herold IH, de Jonge E, Arbous MS. Risk factors and outcomes after unplanned extubations on the ICU: a case-control study. Crit Care. 2011;15(1):1–9. doi:10.1186/cc9964
4. Movement, P.S. Actionable Patient Safety Solutions (APSS)# 15: nasogastric tube (NGT) placement and verification; 2020.
5. Peñuelas Ó, Frutos-Vivar F, Esteban A. Unplanned extubation in the ICU: a marker of quality assurance of mechanical ventilation. Crit Care. 2011;15(2):1–2. doi:10.1186/cc10049
6. da Silva PS, Fonseca MC. Factors associated with unplanned extubation in children: a case–control study. J Intensive Care Med. 2020;35(1):74–81. doi:10.1177/0885066617731274
7. Fitzgerald RK, Davis AT, Hanson SJ. Multicenter analysis of the factors associated with unplanned extubation in the PICU. Pediatr Crit Care Med. 2015;16(7):e217–e223. doi:10.1097/PCC.0000000000000496
8. Kanthimathinathan HK, Durward A, Nyman A, Murdoch IA, Tibby SM. Unplanned extubation in a paediatric intensive care unit: prospective cohort study. Intensive Care Med. 2015;41(7):1299–1306. doi:10.1007/s00134-015-3872-4
9. Mpe MJ, Moloto MS, Mphahlele BV. Unplanned extubations in an academic intensive care unit. South African J Anaesth Analg. 2004;10(5):17–19. doi:10.1080/22201173.2004.10872377
10. Bacha T, Tsegaye N, Tuli W. Characteristics and outcomes of mechanically ventilated pediatric patients in a tertiary referral hospital, Addis Ababa, Ethiopia: cross sectional study. Ethiop J Health Sci. 2021;31(5):915–924. doi:10.4314/ejhs.v31i5.2
11. Mohammed SO, Bedilu GW, Tahir AW. Factors affecting prolonged intensive care unit stay in Nigist Eleni Mohammed Memorial Hospital, Hosanna, Southern Ethiopia. Int J Med Med Sci. 2017;9(9):105–110. doi:10.5897/IJMMS2017.1307
12. Klugman D, Melton K, Maynord PO, et al. Assessment of an unplanned extubation bundle to reduce unplanned extubations in critically ill neonates, infants, and children. JAMA Pediatr. 2020;174(6):e200268. doi:10.1001/jamapediatrics.2020.0268
13. Kaufman J, Rannie M, Kahn MG, et al. An interdisciplinary initiative to reduce unplanned extubations in pediatric critical care units. Pediatrics. 2012;129(6):e1594–e1600. doi:10.1542/peds.2011-2642
14. Uy AB, Ramos EF, Rivera AS, et al. Incidence, risk factors, and outcomes of unplanned extubation in adult patients in a resource-limited teaching hospital in the Philippines: a cohort study. Revista Brasileira de Terapia Intensiva. 2019;31(1):79–85. doi:10.5935/0103-507X.20190012
15. Ansari S. Implementation Strategies Used to Reduce Unplanned Extubations (UPE) in the Neonatal Intensive Care Unit at the Hospital for Sick Children (Sickkids). University of Ontario Institute of Technology (Canada); 2021.
16. Kambestad KK, Huack A, Nair S, et al. The adverse impact of unplanned extubation in a cohort of critically ill neonates. Respir Care. 2019;64(12):1500–1507. doi:10.4187/respcare.06721
17. da Silva PS, Reis ME, Aguiar VE, Fonseca MC. Unplanned extubation in the neonatal ICU: a systematic review, critical appraisal, and evidence-based recommendations. Respir Care. 2013;58(7):1237–1245. doi:10.4187/respcare.02164
18. Roddy DJ, Spaeder MC, Pastor W, Stockwell DC, Klugman D. Unplanned extubations in children: impact on hospital cost and length of stay. Pediatr Crit Care Med. 2015;16(6):572–575. doi:10.1097/PCC.0000000000000406
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
