Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 14
Impact of Platform Switched Implants on Marginal Bone Level in Mandibular Overdentures: A Six-Year Follow-Up Longitudinal Study
Authors Abd El Rahim NS , Ashour AA
Received 6 July 2022
Accepted for publication 29 September 2022
Published 19 October 2022 Volume 2022:14 Pages 307—319
DOI https://doi.org/10.2147/CCIDE.S378636
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Christopher E. Okunseri
Neveen S Abd El Rahim,1,2 Asmaa A Ashour1
1Department of Removable Prosthodontics, Faculty of Dental Medicine for Girls, Al-Azhar University, Cairo, Egypt; 2Department of Removable Prosthodontics, College of Dentistry, Taibah University, Medina, Saudi Arabia
Correspondence: Asmaa A Ashour, Department of Removable Prosthodontics, Faculty of Dental Medicine for Girls, Al-Azhar University, Nasr, Cairo, Egypt, Tel +20 1284048535, Email [email protected]
Purpose: To evaluate the impact of the platform-switched implant on marginal bone loss (MBL) and the probing pocket depth (PPD) in patients wearing mandibular overdenture.
Patients and Methods: This longitudinal study included 40 completely edentulous patients aged 51– 64 years. All patients received complete dentures and were distributed into two groups randomly; 20 patients each. The first group GI received two platform switched implants; however, the 2nd group GII received two platform matched implants (3.6 × 11.5 mm) in the canine region of the mandible. The radiographic evaluations were carried out every year for six years, whereas probing pocket depth was evaluated every six months for 72 months for both groups. The data were analyzed by repeated ANOVA, Friedman’s, and Student’s t-test.
Results: This study included 36 patients; 56 ± 3.6 years was the mean age; 17 females (47%) and 19 males (53%) completed the study. Statistically significant differences were observed in MBL and PPD in each of GI and GII after 6 years, p ≤ 0.05. Between GI and GII after 6 years, a statistically insignificant difference was detected in MBL or PPD, p ≥ 0.05, except in PPD at loading, 2 and 6 years, p ≤ 0.05.
Conclusion: Time positively affected MBL and PPD in platform switched and matched implants retained mandibular overdentures. Platform switching influences probing pocket depth in implants retained mandibular overdentures.
Keywords: dental implant, platform switching, overdenture, supporting structures, COVID-19
Introduction
Complete edentulism is known as a globally common obstacle. Speech, nutrition, perceived aesthetics, and self-esteem are severely compromised.1,2 Complete loss of teeth significantly impacts the individual quality of life. Although oral problems are more severe and chronic, they have been always over-sighted, especially in the aged.3
Complete dentures are performed for oral rehabilitation of complete edentulism, it is considered for long as the only prosthodontics treatment option.1 Osseo-integrated implants and the overdentures installation are used as an alternative to enhance stability, retention, and accordingly functions of complete dentures. With the increasing prevalence, availability, and utilization of dental implants a great variety of treatment approaches have been opened, especially with advanced demands for preferable function and adequate replacement of teeth. Mandibular overdentures retained by two implants are considered a treatment option already approved in the literature.4,5
The connection between abutment and implant was further improved through the “platform switching (PS)” concept. This was all simply about decreasing the abutment diameter at the implant’s platform. This includes horizontal inward relocation of abutment-implant interface, in relation to the implant platform.6 That type of implant carries several advantages like repositioning of gingival papillae and preserving the peri-implant tissues.7,8
The PS concept is believed to decrease bone loss around the implant. By moving the concentration of stress from the cervical region to the abutment’s interface and compact to cancellous bone, this concept was regarded to reduce stresses around the implant neck. Elimination of bacterial micro-leakage at the implant neck area is performed by platform switching. In addition, the PS interrupts infiltration of the inflammation and consequently prevents the migration of the tissues around the implant apically.9–11
Preservation of bone around the dental implant is a challenge. Comprehensive research concerning the assessment of marginal bone loss around implants has been established. It remains a principal aspect in anticipating the survival and prognosis of an implant. Marginal bone preservation promotes soft tissue stability, which is important for implant survival for long period. Accordingly, the clinician’s responsibility is to demand the least crestal bone loss.11,12
Bone loss around an implant around 1 mm during 1st year of service is considered to be unavoidable. Within the 1st year of implant loading, crestal bone physiology changes, it becomes mature and denser. Occlusal forces that induce initial marginal bone loss are not sufficient to induce additional bone resorption.11,13 Preservation of crestal bone should be arranged before implant placement. The PS system is considered one of the approaches which are recommended to minimize marginal bone loss.14
Moreover, it was reported that the clinical success of dental implant osseointegration will affect the soft tissue changes. This is particularly through pocket depth as well as mobility of the implant. Probing depth was used as a diagnostic tool to assess mucosa around an implant. A long follow-up period is essential to observe all these variables.15,16
There is a relative scarcity of literature, especially regarding implant-retained removable prostheses. Therefore, long-term studies are needed to identify the ideal implant-abutment junction design recommended to be used with implants retained removable prostheses.11
That longitudinal study was planned to evaluate the impact of the platform-switched implant on marginal bone loss (MBL) and probing pocket depth (PPD) in patients wearing mandibular overdenture as compared with that of the platform-matched implant during 6 years follow-up period.
The null hypotheses were that no differences were observed in MBL or probing pocket depth in each of the platform-switched and -matched implants during 6-year follow-up period. No differences between platform switched and matched implants retained mandibular overdentures in their influences on supporting structures during 6 years.
Materials and Methods
Study Design
A longitudinal study was performed from July 2015 to December 2021. A total of 40 completely edentulous patients, 18 females, and 22 males, aged (51–64 years) participated in this study. The calculation for power size detected a sample size (N = 40) at power 0.80, confidence interval 0.95, and alpha level 0.05.8,17 Selection of patients followed a specific inclusion and exclusion criteria; exempt from any systemic or local diseases, temporomandibular joint disorders (TMJDs), neuromuscular disease or bone disease. All patients had Angle’s class I jaw relationship and sufficient inter-arch space. They had well-developed maxillary and mandibular alveolar ridges with tough mucosa exempt from flappy tissues, ulceration, and inflammation. To prevent the adverse effects on the musculatures and oral functions, any patient with bruxism, clinching, or abnormal tongue habits was excluded. All patients accepted the treatment. Written, informed consents were received from all patients. This was approved by the Research Ethics Committee of the Faculty of Dental Medicine (Girls), Al Azhar University, Review Board (Code REC19-022). The current study complied with the Declaration of Helsinki.
Clinical Protocol
Cone-beam computed tomography CBCT and a preoperative panoramic radiograph was performed on all selected patients to evaluate the height, quantity, and quality of bone. Upper and lower complete dentures have been performed for the patients. Dentures constructions were performed following standard clinical and laboratory procedures. Patients were instructed to use their upper and lower complete dentures for 3 months following delivery for adaptation. The quality, height, and buccolingual width of bone available for implant placement were determined with CBCT using a radiographic template. All patients were divided randomly into 2 groups twenty in each. Group I (GI) received 2 self-tapping, tapered, endosteal (3.6 × 11.5 mm) platform switched implants in the mandibular canine region (Deyna Dental Engineering BV, Holland). Group II (GII) received 2 self-tapping, tapered, endosteal (3.6 × 11.5 mm) platform switched implants in the mandibular canine region (Deyna Dental Engineering BV, Holland). In both groups, two stages surgical techniques were performed for implants installation and implants remained submerged for 3 months to allow osseointegration. After 3 months, exposure of the implant was performed, and the cover screw of the implant was unthreaded and exchanged with a healing collar. After 10 days ball and socket attachments (Dyna Dental Engineering BV, Holland) replaced the healing collars. The female housing of attachments was picked up with the lower denture. GI was obtained, two ball and socket attachments connected to two platform switched dental implants retained mandibular-overdenture, while GII was obtained, two ball and socket attachments connected to two platform matched dental implant-retained mandibular overdenture, Figure 1.
 |
Figure 1 Two platform switched dental implants at canine areas of mandibular ridge. |
After implants loading, radiographic evaluation of MBL and periodontal pocket depth measures were performed for each patient. In both groups, all patients utilized their dentures for 6 years a follow-up period. Radiographic evaluation was performed at loading and every year for 6 years for each group while periodontal pocket depth measures were performed at loading and every 6 months for 72 months.
Radiographic Evaluation
Intraoral Indirect Digital Radiographic Measurements
For each patient, a radiographic template was performed and checked in the patient’s mouth. Both mesial and distal bone heights were assessed for every implant during each follow-up appointment. A standardized radiograph for the lower alveolar ridge was performed using The Orix x-ray machine (Orix-Aet, ARDET, S.V.R, Milano, Italy) at radiographic exposure (10-milliampere, 65-kilovolt, and 0.4-seconds). That was standardized for all patients at each follow-up appointment. The measurements of bone height were performed using Digora’s computerized system and image processing software (Orion Corporation, Soredex Medical Systems, Helsinki, Finland). The radiographic images for each patient were interpreted and analyzed to record the marginal bone height at the mesial and distal sides of the implant. The crest alveolar bone and the shoulder of the implant were utilized as reference points. The distance between these 2 reference points is considered vertical MBL and measured for mesial and distal sides. That was carried out at each scheduled follow-up visit. The data were collected and statistically analyzed.
Probing Pocket Depth Measurement
Hawe Neos (3/5/7/9mm) is a color-coded plastic periodontal probe end provided with a flexible tip (Kerr, Lugano, Switzerland). It is specially fabricated to estimate periodontal pocket depth (PPD) around implants. The distance extending from the gingival margin to the tip of the periodontal probe was considered PPD. The estimation of PPD was measured on the facial, lingual, mesial, and distal surfaces of each implant. The PPD measurements were evaluated to the nearest full millimeter, recorded on a specific chart, and become a permanent part of the patient chart. The mean of the PPD measurements with both the right and the left implants for each patient was statistically analyzed.
Statistical Analysis
The computerized data were analyzed using SPSS 20. Shapiro–Wilk normality test was performed to disclose normally distributed data. The quantitative data were represented by the mean and standard deviation (SD). The independent Student’s t-test was used to interpret the significance of differences between two continuous variables and repeated ANOVA test and Friedman test were performed to interpret the significance of differences between the means of three or more groups. The pairwise comparisons were performed using Bonferroni test. The significance level was adjusted at a p-value ≤0.05.
Results
Patients
Forty patients, GI and GII (n=20 in each) participated in this study. A total of 2 male patients in GI and 2 patients (a female and a male) in GII did not continue the follow-up appointments. In GI, a male patient rejected the follow-up appointments at the end of one year and a male patient suffered from a brain stroke following 2 years of loading of the implant and discontinued the follow-up appointments. In GII, a female patient died after 4 years of follow-up appointments and a male patient rejected the follow-up appointments at the beginning of six years. Finally, 36 patients had a mean age (56 ± 3.6 years); 17 females (47%) and 19 males (53%) finished the study, Table 1 and Figure 2.
 |
Table 1 Patient Demographics |
 |
Figure 2 Flow diagram of clinical trial. |
The follow-up appointments for the 5th year were totally missed due to the complete lockdown caused by COVID-19. The follow-up appointments (July 2019 to July 2020) were delayed six months to December 2020 until the finishing of the lockdown.
Effect of Time on MBL in Each Group
The MBL was measured in platform switched (GI) and platform matched (GII) implant-retained mandibular overdenture for patients at the loading of the implants, each year afterward for 6 years. In GI, the mean of MBL (the mesial, distal, right, and left measurements) was increased from the loading of the implants until the 6th year in patients who have received platform switched implant, Figure 3; MBL.1y < MBL.2y < MBL.3y < MBL.4y < MBL.5y < MBL.6y. Statistically significant differences were detected in mean MBL of GI following 6 years follow-up period, p≤ 0.05, Table 2 and Figure 4.
 |
Table 2 Marginal Bone Loss (MBL) in GI During 6 Years Follow-Up Period |
 |
Figure 3 Radiographic measurements for MBL in platform switched implant (GI) after (A) 1 year and (B) 6 years of follow-up. |
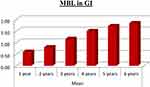 |
Figure 4 The mean of MBL in platform switched implant-retained mandibular overdenture during 6 years follow-up period. |
In GII, the mean of MBL was increased from the loading of the implants until the 6th year in patients who received platform-matched implants. Statistically significant differences were detected in the mean MBL of GII following 6-year follow-up period, p≤ 0.05, Table 3 and Figure 5.
 |
Table 3 Marginal Bone Loss (MBL) in GII During 6 Years Follow-Up Period |
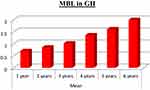 |
Figure 5 The mean of MBL in platform matched implant-retained mandibular overdenture during 6 years follow-up period. |
Effect of Time on Probing Pocket in Each Group
The mean of probing pocket depth (PPD) in platform switched implant was evaluated for (GI) at loading and every six months for 72 months follow-up periods. In GI, the mean of PPD was increased from loading of the implants and each 6 months for 72 months; PPD at loading > PPD.6m < PPD.12m < PPD.18m < PPD.24m < PPD.30m = PPD.36m > PPD.42m < PPD.48m < PPD.54m > PPD.60m < PPD.66m < PPD.72m. Statistically significant differences were detected in PPD in GI following 72 months follow-up period, p≤ 0.05, Table 4 and Figure 6.
 |
Table 4 Probing Pocket Depth in GI During 6 Years Follow-Up Period |
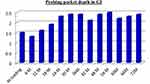 |
Figure 6 The mean of probing pocket depth during 72 months follow-up periods in GI. |
In GII, the mean of PPD was increased from loading of the implants and each 6 months for 72 months; PPD at loading < PPD.6m < PPD.12m > PPD.18m < PPD.24m < PPD.30m < PPD.36m >PPD.42m < PPD.48m < PPD.54m < PPD.60m > PPD.66m < PPD.72m. Statistically significant differences were detected in PPD in GII following 72 months follow-up periods, p≤ 0.05, Table 5 and Figure 7.
 |
Table 5 Probing Pocket Depth in GII During 6 Years Follow-Up Period |
 |
Figure 7 The mean of probing pocket depth during 72 months follow-up periods in GII. |
Effect of the Group on MBL
The mean MBL in platform switched (GI) and platform matched (GII) implants-retained mandibular overdenture were compared. No statistically significant differences were detected in the mean MBL between lower overdentures retained by two platform switched implants (GI) and that retained by two platform matched implants (GII) after 6 years follow-up periods, p≥0.05, Table 6 and Figure 8.
 |
Table 6 Marginal Bone Loss (MBL) in GI and GII During 6 Years Follow-Up Period |
 |
Figure 8 The mean of MBL in GI and GII during 6 years follow-up period. |
Effect of the Group on Probing Pocket Depth
No statistically significant differences were detected in probing pocket depth (PPD) between lower overdentures retained by two platform switched implants (GI) and that retained by two platform matched implants (GII) after 72 months follow-up period, p≥0.05. However, statistically significant differences in PPD between GI and GII at loading, 24 months, and 72 months follow-up periods, p≤0.05, Table 7 and Figure 9.
 |
Table 7 Probing Pocket Depth in GI and GII During 6 Years Follow-Up Period |
 |
Figure 9 The mean of probing pocket depth in GI and GII during 72 months follow-up period. |
Discussion
The current longitudinal study was planned to evaluate the impact of the platform-switched implant on marginal bone loss (MBL) and probing pocket depth (PPD) in patients wearing mandibular overdenture as compared with that of the platform-matched implant during 6 years follow-up period.
Carefully standardized inclusion and exclusion measures were designed for this study. Parameters including patients’ age, quantity and quality of bone, design of the implant, surgical techniques, and implant loading protocol, which can affect the outcome results of the study, were standardized. This study was caught in the clinical dilemma known because of the Covid-19 pandemic, during the follow-up period from 2019 to 2021.
Following implants installation and loading, all implants attained the criteria accepted for a successful implant. All 72 implants in GI and GII (36 in each) survived in accepted function without any detected signs of peri-implant soft tissue infection, pain, or mobility. The survival rate was 100%. Radiographically, there was no persistent mesial or distal radiolucency around the implant. This was in accordance with 5 years of follow-up delayed implants loading results in disparate designs, implants’ survival rate was 98.3%–100%.18,19
The results of the present study clarified that the first null hypothesis was rejected, as there were no differences detected in MBL or changes in probing pocket depth, in each platform switched (GI), and matched implants (GII) retained mandibular overdentures after 6 years follow-up period. Statistically significant differences were detected, in both MBL and probing pocket depth in GI and GII during the 6 years’ follow-up periods.
The mean MBL was significantly increased in GI and GII during the 6 years follow-up period. Following the results of this study, after the 6th-year follow-up, the mean MBL was (1.84±0.59 mm) for GI and (2.00±0.27 mm) for GII. This was in agreement with the criteria of success of an implant which found that bone loss equal to 1–1.5 mm within 1st year following loading and annual 0.2 mm subsequently is considered accepted.20–22 The MBL, from the loading of the implant, equivalent to or more than 2 mm was estimated as a biological problem and not as an implant failure. Also, these results can be attributed to limitations of measurements rather than biological factors.23–25
The mean probing pocket depth was significantly increased during the 6 years follow-up period in GI and GII. It was reported that generally, peri-implant pocket depths should be ≤5 mm. If the increased probing depth is not associated with other symptoms; it will be with a poor diagnostic value. In the current study, all measured preimplant probing pocket depths showed a pocket depth of ≤4 mm.26–28
These results are in agreement with an earlier study held by the same authors over five-year follow-up. This study reported a positive long-term effect of mandibular two implants retained overdentures on OHRQoL, MBL, probing pocket depth, and implant stability.29
The second null hypothesis was that no differences between platform switched (GI) and matched implants (GII) retained mandibular overdentures in their influences on MBL or the probing pocket depth after 6 years follow-up period. That hypothesis was accepted. No statistically significant differences were detected between GI and GII after 6 years follow-up period. These results are in accordance with the results of three-year follow-up study held by the same authors.30
The results of the current study found that the marginal bone resorption is not affected by platform switching (PS). This may be attributed to the resorption of bone being almost associated with biological aspects, such as biological bone width regeneration more than to biomechanical aspects, such as the size of the abutment in relation to the implant neck.23 These are in accordance with previous studies that revealed that PS may be less important for peri-implant crestal bone-level maintenance as supposed. Also, the contribution of PS is still arguable; resorption of crestal bone is to be affected by various factors.6,18,31
On the other hand, the concept of platform switching has been considered by many other authors as a primary factor in the positive or even dramatic preservation of crestal bone loss. These articles included humans and animals, original studies, and systematic reviews, but these did not include completely edentulous patients restored with implant-retained mandibular overdenture treatment modalities, especially with long-term follow-up periods.13,32,33
The results of probing pocket depths in the current study revealed no statistically significant differences between GI and GII during 6 years follow-up period except at loading, after 24 months, and 72 months. This indicates that probing pocket depth is not influenced by platform switching during the whole follow-up period except at loading, after 24 months, and 72 months. That was in agreement with the study revealed that insignificant values of probing pocket depth were observed at 4 and 5 years follow-up periods between platform-switched and -matched implants.23 It was reported that peri-implant probing pocket depths if not combined with signs and/or symptoms such as radiographic radiolucencies, purulent exudate, bleeding, pain, or discomfort, maybe a poor diagnostic value. Accordingly, marginal bone loss over time is associated with increasing probing depths without any signs of implant endosteal disease.26
Conclusion
Within the parameters of this study design, time positively affected MBL and PPD in platform switched and matched implants retained mandibular overdentures. Platform switching influences probing pocket depth in implants retained mandibular overdentures. It is recommended to conduct further studies with longer study periods and larger sample sizes to validate the concept of this study.
Data Sharing Statement
Datasets related to this study will be available from the corresponding author upon request.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Vi S, Pham D, Du YYM, Arora H, Tadakamadla SK. Mini-implant-retained overdentures for the rehabilitation of completely edentulous maxillae: a systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18(8):4377. doi:10.3390/ijerph18084377
2. Di Francesco F, De Marco G, Eb C, et al. Patient satisfaction and survival of maxillary overdentures supported by four or six splinted implants: a systematic review with meta-analysis. BMC Oral Health. 2021;21(1):1–14. doi:10.1186/s12903-021-01572-6
3. Banerjee R, Chahande J, Banerjee S, Radke U. Evaluation of relationship between nutritional status and oral health related quality of life in complete denture wearers. Indian J Dent Res. 2018;29(5):562–567. doi:10.4103/ijdr.IJDR_285_17
4. Hartmann R, Bandeira ACF, De M, et al. A parallel 3-group randomised clinical trial comparing different implant treatment options for the edentulous mandible: 1-year effects on dental patient-reported outcomes and chewing function. J Oral Rehabil. 2020;47(10):1264–1277. doi:10.1111/joor.13070
5. Gray D, Patel J. Implant-supported overdentures: part 1. Br Dent J. 2021;231(2):94–100. doi:10.1038/s41415-021-3224-4
6. Ghensi P, Tonetto G, Soldini C, Bettio E, Mortellaro C, Soldini C. Dental implants with a platform-switched Morse taper connection and an osteo growth induction surface. J Craniofac Surg. 2019;30(4):1049–1054. doi:10.1097/SCS.0000000000004795
7. Sesma N, Garaicoa-Pazmino C, Zanardi PR, Chun EP, Laganá DC. Assessment of marginal bone loss around Platform-matched and platform-switched implants - A prospective study. Braz Dent J. 2016;27(6):712–716.
8. Nayak R, Devanna R, Dharamsi AM, Shetty J, Mokashi R, Malhotra S. Crestal bone loss around dental implants: platform switching vs platform matching-a retrospective study. J Contemp Dent Pract. 2018;19(5):574–578. doi:10.5005/jp-journals-10024-2301
9. Hsu Y-T, Lin G-H, Wang H-L. Effects of platform-switching on peri-implant soft and hard tissue outcomes: a systematic review and meta-analysis. Int J Oral Maxillofac Implants. 2017;32(1):e9–24. doi:10.11607/jomi.5140
10. Eldien AMS, Mahmoud EA, Hamed H, Shoeib MA. Does the platform switching implant affect the crestal bone level? A systematic review and meta-analysis. Int J Dent Res. 2019;4(1):20–29.
11. Gehrke SA, Dedavid BA, Prados-Frutos JC. Effects of different switched or not-switched implant and abutment platform designs and marginal bone loss on fracture strength: an in vitro study. J Prosthet Dent. 2021;125:1–8. doi:10.1016/j.prosdent.2020.11.038
12. Chowdhury S, Chakraborty P. Crestal bone loss around dental implants after implantation of Tricalcium phosphate and platelet rich plasma: a comparative study Sravani. J Fam Med Prim Care. 2017;6(2):169–170.
13. Puisys A, Auzbikaviciute V, Minkauskaite A, et al. Early crestal bone loss: is it really loss? Clin Case Rep. 2019;7(10):1913–1915. doi:10.1002/ccr3.2376
14. Díaz-Castro CM, Calvo PL, Gil FJ, Fernández-Palacín A, Ríos-Santos JV, Herrero-Climent M. A non-interventional study documenting use and success of tissue level implants. Int J Environ Res Public Health. 2020;17(13):1–13. doi:10.3390/ijerph17134816
15. Santos Marino J, Cortés-Bretón Brinkmann J, García-Gil I, et al. Clinical evaluation of dental implants with a double acid-etched surface treatment: a cohort observational study with up to 10-year follow-up. Materials. 2021;14(21):6483. doi:10.3390/ma14216483
16. Correa EP. Clinical evaluation of dental implants with a double acid-etched surface treatment: a cohort observational study with up to 10-year follow-up. J Dent Heal Oral Res. 2021;02(02):1–13.
17. Telleman G, Raghoebar GM, Vissink A, Meijer HJA. Impact of platform switching on inter-proximal bone levels around 8.5 mm implants in the posterior region; 5-year results from a randomized clinical trial Gerdien. J Clin Periodontol. 2017;44(3):326–336. doi:10.1111/jcpe.12654
18. Jonker BP, Gil A, Naenni N, Jung RE, Wolvius EB, Pijpe J. Soft tissue contour and radiographic evaluation of ridge preservation in early implant placement: a randomized controlled clinical trial. Clin Oral Implants Res. 2021;32(1):123–133. doi:10.1111/clr.13686
19. Mifsud DP, Cortes ARG, Zarb MJ, Attard NJ. Maintenance and risk factors for fractures of overdentures using immediately loaded conventional diameter or mini implants with Locator abutments: a cohort study. Clin Implant Dent Relat Res. 2020;22(6):706–712. doi:10.1111/cid.12952
20. Pardal-Peláez B, Flores-Fraile J, Pardal-Refoyo JL, Montero J. Implant loss and crestal bone loss in immediate versus delayed load in edentulous mandibles: a systematic review and meta-analysis. J Prosthet Dent. 2021;125(3):437–444. doi:10.1016/j.prosdent.2020.01.032
21. Albertini M, Herrero-Climent F, Díaz-Castro CM, et al. A radiographic and clinical comparison of immediate vs. Early loading (4 weeks) of implants with a new thermo-chemically treated surface: a randomized clinical trial. Int J Environ Res Public Health. 2021;18(3):1–19. doi:10.3390/ijerph18031223
22. Anitua E, Fernandez-de-Retana S, Anitua B, Alkhraisat M. Long-term retrospective study of 3.0-mm-diameter implants supporting fixed multiple prostheses: immediate versus delayed implant loading. Int J Oral Maxillofac Implants. 2020;35(6):1229–1238. doi:10.11607/jomi.8180
23. Salman A, Thacker S, Rubin S, Dhingra A, Ioannidou E, Schincaglia G. Immediate versus delayed loading of mandibular implant-retained overdentures: a 60-month follow-up of a randomized clinical trial. J Clin Periodontol. 2019;46(8):863–871. doi:10.1111/jcpe.13153
24. Renvert S, Persson GR, Pirih FQ, Camargo PM. Peri-implant health, peri-implant mucositis, and peri-implantitis: case definitions and diagnostic considerations. J Periodontol. 2018;89(January):S304–12. doi:10.1002/JPER.17-0588
25. Yadav R, Verma U, Tiwari R, Article O. A comparative evaluation of immediate versus delayed loading of two implants with mandibular overdenture: an in vivo study. Natl J Maxillofac Surg. 2019;10(1):3–7. doi:10.4103/njms.NJMS_55_18
26. Al Amri MD, Abduljabbar TS. Comparison of clinical and radiographic status of platform-switched implants placed in patients with and without type 2 diabetes mellitus: a 24-month follow-up longitudinal study. Clin Oral Implants Res. 2017;28(2):226–230. doi:10.1111/clr.12787
27. Beschnidt SM, Cacaci C, Dedeoglu K, et al. Implant success and survival rates in daily dental practice: 5-year results of a non-interventional study using CAMLOG SCREW-LINE implants with or without platform-switching abutments. Int J Implant Dent. 2018;4(1). doi:10.1186/s40729-018-0145-3
28. Mandal AK, Dam P, Octavio L, et al. Evaluation of quality of life and oral hygiene attitudes of individuals using dental prostheses during the COVID-19 pandemic. Ann Oncol. 2020;2020(January):19–21.
29. Abd El Rahim NS, Ashour AA. Assessment of quality of life and supporting structures in implant retained mandibular overdenture: a 5-year cohort study. Clin Cosmet Investig Dent. 2022;14:171–182. doi:10.2147/CCIDE.S364814
30. Mohamed N, Ashour A. Comparison of platform switched and platform matched implants on supporting structures of mandibular overdentures: a three year follow-up longitudinal study. Egypt Dent J. 2020;66:1235–1242. doi:10.21608/edj.2020.24076.1024
31. Abd El Rahim NS, Ashour AA. Effect of platform switched implants on supporting structures of mandibular overdentures. Egypt Dent J. 2018;64:1431–1438. doi:10.21608/edj.2018.77455
32. Chen M. Clinical significance of the use of resonance frequency analysis in assessing implant stability: a systematic review. Int J Prosthodont. 2018;32(1):51–58. doi:10.11607/ijp.6048
33. Salamanca E, Lin JCY, Tsai CY, et al. Dental implant surrounding marginal bone level evaluation: platform switching versus platform matching - one-year retrospective study. Biomed Res Int. 2017;2017:1–9. doi:10.1155/2017/7191534
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
