Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 14
Hypercalcemia in a 5-Year-Old Child with Disseminated Tuberculosis: Case Report and Literature Review
Authors Salah FO , Abdela AF , Obeid ZM, Adane L , Arega G
Received 14 September 2023
Accepted for publication 28 November 2023
Published 7 December 2023 Volume 2023:14 Pages 477—481
DOI https://doi.org/10.2147/PHMT.S435222
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Fathia Omer Salah,1 Abubeker Fedlu Abdela,1 Zeinab Mustafa Obeid,2 Leul Adane,1 Gashaw Arega2
1Department of Diagnostic Radiology, Addis Ababa University, Addis Ababa, Ethiopia; 2Department of Pediatric & Child Health, Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Fathia Omer Salah, Department of Diagnostic Radiology, Addis Ababa University, P.O.Box 62058, Addis Ababa, Ethiopia, Tel +251 921 912290, Email [email protected]; [email protected]
Abstract: In tuberculous patient, abnormal extrarenal production of 1.25-dihydroxyvitamin D3 by activated macrophages results in hypercalcemia. High calcium level associated with tuberculosis is frequent in adults with active pulmonary tuberculosis even though most patients are asymptomatic, while hypercalcemia in children due to disseminated tuberculosis is rare. Here, we described a case of a 5-year-old who presented with cough and right anterior chest swelling of two-month duration with an Erythrocyte Sedimentation Rate of 144mm/hour, and a high serum ionized calcium level of 1.46millimol/L. With the epidemiologically prevalence, clinical and radiological imaging findings the diagnosis of disseminated tuberculosis to lung, pleura, lymph node, liver and bone was made, and the child was started with the anti-tuberculosis treatment, hypercalcemia was attributed to the disseminated tuberculosis precipitated by high calcium meal intake and excessive sun exposure. Tuberculosis can be complicated with hypercalcemia; care must be taken in supplementing vitamin D and high calcium meals especially in high sun exposure geographic areas.
Keywords: hypercalcemia, disseminated tuberculosis, ESR, chest CT scan
Introduction
Most granulomatous disorders are known to cause hypercalcemia. Mechanism of hypercalcemia in granulomatous disease is due to activation of extra renal macrophages trapped in granulomatous inflammation that leads to dysregulated production of 1.25-(OH2) D3. Undetected hypercalcemia causes neuropsychiatric disturbances, renal dysfunction, cardiovascular disease, or musculoskeletal disease.1 The incidence of hypercalcemia in adults with tuberculosis (tb) varies from 2% to 25%2–4 while symptomatic hypercalcemia is less common with approximate rate of occurrence around 3%.4 Variation in incidence highly depends on the geographical area where the study is conducted and on multiple other factors such as intake of calcium and vitamin D.
Relationship between type and stage of tuberculosis with serum calcium level is not clear, and discrepancies are noted in association with radiological extent of the disease.4–6
Here we report a 5-year-old with disseminated tuberculosis complicated by hypercalcemia, who was successfully treated with anti-tuberculosis medication and hydration followed by dietary restriction of calcium and vitamin D.
Case Presentation
A 5-year-old female child presented with cough and right anterior chest swelling of two-month duration associated with progressive weight loss and drenching night sweats. She had a strong contact history with an adult who had confirmed pulmonary tuberculosis on anti-tuberculosis treatment. Physical examination showed an emaciated child with pale conjunctiva, multiple matted, non-tender lymphadenopathies on the submandibular, anterior cervical, axillary, and inguinal areas with no overlying skin change. There was a 4cm x 3 cm anterior chest swelling which was fluctuant and non-tender on palpation. On chest auscultation there was a decrease air entry over the right two-thirds of the right lung zones.
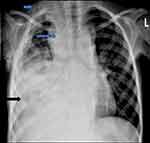
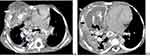
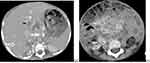
On admission, her laboratory investigations revealed a total white cell count of 24,600/mm3 with lymphocyte predominance, hemoglobin of 8.2 g/dl with a MCV of 75fl, and normal platelet count, ESR of 144mm/hour and negative serostatus for HIV/AIDS. Renal and liver function tests were normal, serum electrolytes determination showed a high level of ionized calcium [iCa level of 1.46mmol/L]. Chest radiography, postcontrast chest and abdominal computed tomography (CT) scan showed multiorgan involvement of tuberculosis evidenced by right paratracheal, right axillary and multiple mediastinal calcified lymphadenopathies with opacity at right lower lung (Figure 1). The air space opacity showed area of necrosis and peripheral calcification, right anterior chest wall fluid collection with rim enhancement is seen that suggested abscess collection (Figure 2). Postcontrast abdominal scan at hepatic level demonstrate different size multiple central hypo enhancing lesions having peripheral calcification, centrally located larger lesions had irregular rim enhancement (Figure 3). Bone involvement was evidenced by small perivertebral collection with faint rim enhancement associated with T1 vertebral endplate erosion (Figure 4).
Considering strong contact history with pulmonary tuberculosis patient, clinical, laboratory investigations, and radiological imaging findings she started anti-tuberculosis medications with 2RH/4RHZE with impression of disseminated tuberculosis (involving lung, pleura, lymph node, liver and bone) and drainage with catheter was done for anterior chest wall collection.
In this case, the cause of the hypercalcemia was attributed to extra-renal 1-alpha hydroxylase activity in the macrophages and the child was rehydrated with intravenous fluids, calcium intake was controlled and the ionized calcium level normalized.
She was discharged in a stable condition with follow up arranged for completion of anti-tuberculosis therapy. Parents were advised to avoid excessive sun exposure, oral vitamin D or calcium supplements and to decrease milk products.
Discussion
Hypercalcemia is one of the metabolic abnormalities in granulomatous disease like tuberculosis and sarcoidosis.1–6 There are several other potential triggers, such as coccidioidomycosis, histoplasmosis, Crohn’s disease, and Langerhans-cell histiocytosis.3,6–8
The incidence of hypercalcemia in adults with tuberculosis varies from 2% to 25%2,3 depending on the geographical area where the study was conducted and depending on multiple other factors such as the intake of calcium, vitamin D, and exposure to the sun.1–5 Study done by John et al to determine the incidence, risk factor and clinical presentation of tuberculosis complicated by hypercalcemia, showed incidence of 20.15% and 34.6% of patients had symptoms of hypercalcemia. Symptoms such as delirium, anorexia, nausea, weakness/lethargy, and polyuria were seen. 25% of moderate and 50% of severe hypercalcemia patients had clinical symptoms.6
The mechanism of hypercalcemia in tuberculosis is due to the extra-renal production of 1.25 (OH)2D3 by macrophages and T lymphocytes, possibly CD8 T lymphocytes.7 Although no data are available for children, symptomatic hypercalcemia in tuberculosis in adults occurs only in 3%.4
Medical literature in the past 25 years has documented a limited number of cases wherein children exhibited hypercalcemia in conjunction with tuberculosis.5 To the best of our knowledge, the case we are presenting is the first of its kind reported in Ethiopia.
Our patient is a young child presented with elevated serum ionized calcium level, measuring 1.46 mmol/l despite not receiving vitamin D supplementation and was diagnosed with disseminated TB based on the epidemiological, clinical, laboratory and radiological evidence. Diagnosis of tuberculosis in children is usually difficult and mainly based on epidemology and clinical symptomswhich are often nonspecific, Childhood TB can be categorized as TB exposure, TB infection (possible or probable) or confirmed TB disease.6,8,9 With diagnosis of probable TB infection evidenced by exposure history, clinical and laboratory findings, supported by radiological evidence which revealed peripherally calcified necrotic lung lesion, anterior chest wall abscess collection with rib destruction, multiple eggshell calcified mediastinal and abdominal lymph nodes and multiple hypo enhancing hepatic lesions that exhibit calcification and rim enhancement, she was started with anti-tuberculosis medications with 2RH/4RHZE.
Disseminated fungal infection such as histoplasmosis was considered as differential diagnosis. Which is often seen in immunocompromised patients and tends to be fatal.
Considering the epidemiology and exposure history tuberculosis was favored.
The management of hypercalcemia is primarily addressing the root cause of the condition, alongside implementing strategies to decrease the levels of calcium in the bloodstream. In certain cases, the limitation of calcium and vitamin D supplements may suffice as a treatment measure, although intravenous fluids may be employed to expedite the restoration of serum levels. Several alternative therapies have been employed: Pharmaceutical agents such as ketoconazole, hydroxychloroquine, bisphosphonates, and corticosteroids can be considered.
Conclusions
Chronic granulomatous disease like tuberculosis is known to be complicated with hypercalcemia, incidence of occurrence depends on many factors like geographic area, vitamin D and calcium supplements. In resource limited countries like Ethiopia, it is not feasible to determine calcium level for all tuberculosis patients but still high clinical suspicion is important before calcium and vitamin D supplementation.
Patient Consent
Informed consent was obtained from the parent for publication of this case report and any accompanying images. This study not only received the necessary institutional ethical clearance for its execution but also underwent a thorough review process to determine whether institutional approval was specifically required for the publication of the case details. It was determined that such approval was confirmed for the publication, ensuring full compliance with our institution’s ethical standards and guidelines.
Acknowledgments
We express special thanks to the mother of the child for giving consent to publish this report for academic purposes.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sharma OP. Hypercalcemia in granulomatous disorders: a clinical review. Curr Opin Pulm Med. 2000;6(5):442–447. PMID: 10958237. doi:10.1097/00063198-200009000-00010
2. Rajendra A, Mishra AK, Francis NR, Carey RA. Severe hypercalcemia in a patient with pulmonary tuberculosis. J Family Med Prim Care. 2016;5(2):509–511. PMID: 27843882; PMCID: PMC5084602. doi:10.4103/2249-4863.192327
3. Abbasi AA, Chemplavil JK, Farah S, Muller BF, Arnstein AR. Hypercalcemia in active pulmonary tuberculosis. Ann Intern Med. 1979;90(3):324–328. PMID: 426400. doi:10.7326/0003-4819-90-3-324
4. Roussos A, Lagogianni I, Gonis A, et al. Hypercalcaemia in Greek patients with tuberculosis before the initiation of anti-tuberculosis treatment. Respir Med. 2001;95(3):187–190. PMID: 11266235. doi:10.1053/rmed.2000.1019
5. Payne HA, Menson E, Sharland M, et al. Symptomatic hypercalcaemia in paediatric tuberculosis. Eur Respir Rev. 2011;20(119):053–056. doi:10.1183/09059180.00006910
6. John SM, Sagar S, Aparna JK, Joy S, Mishra AK. Risk factors for hypercalcemia in patients with tuberculosis. Int J Mycobacteriol. 2020;9:7–11. doi:10.4103/ijmy.ijmy_211_19
7. Cadranel J, Garabedian M, Milleron B, Guillozo H, Akoun G, Hance AJ. 1,25(OH)2D2 production by T lymphocytes and alveolar macrophages recovered by lavage from normocalcemic patients with tuberculosis. J Clin Invest. 1990;85(5):1588–1593. PMID: 2159024; PMCID: PMC296610. doi:10.1172/JCI114609
8. Concepcion NDP, Laya BF, Andronikou S, et al. Standardized radiographic interpretation of thoracic tuberculosis in children. Pediatr Radiol. 2017;47:1237–1248. doi:10.1007/s00247-017-3868-z
9. Concepcion NDP, Laya BF, Andronikou S, et al. Imaging recommendations and algorithms for pediatric tuberculosis: part 1—thoracic tuberculosis. Pediatr Radiol. 2023;53:1773–1781. doi:10.1007/s00247-023-05654-1
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.