Back to Journals » International Journal of Women's Health » Volume 16
Higher Cumulative Live Birth Rate but Also Higher Late Miscarriage Risk in Non-Obese Women with Polycystic Ovary Syndrome Undergoing the First IVF/ICSI Cycle
Authors Liu S, Zhou X, Jie H, Zheng Z, Cai B, Mai Q, Zhou C
Received 27 October 2023
Accepted for publication 22 January 2024
Published 23 February 2024 Volume 2024:16 Pages 289—298
DOI https://doi.org/10.2147/IJWH.S445021
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Simin Liu,1,2 Xiu Zhou,1,2 Huiying Jie,1,2 Zetong Zheng,1,2 Bing Cai,1,2 Qingyun Mai,1– 3 Canquan Zhou1– 3
1Reproductive Medicine Center, The First Affiliated Hospital, Sun Yat-Sen University, Guangzhou, People’s Republic of China; 2Guangdong Provincial Key Laboratory of Reproductive Medicine, Guangzhou, People’s Republic of China; 3Guangdong Provincial Clinical Research Center for Obstetrical and Gynecological Diseases, Guangzhou, People’s Republic of China
Correspondence: Canquan Zhou, Reproductive Medicine Center, The First Affiliated Hospital, Sun Yat-Sen University, No. 1 Zhongshan Second Road, Guangzhou, 510080, People’s Republic of China, Fax +86 87330736, Email [email protected]
Purpose: To determine the impact of polycystic ovary syndrome on in vitro fertilization/intracytoplasmic sperm injection and embryo transfer outcomes while analyzing the influencing factors.
Patients and Methods: A retrospective cohort study comprised 4839 patients who underwent their first cycle of IVF/ICSI treatment from January 2016 to December 2021. Cumulative pregnancy rates, cumulative live birth rates, and late miscarriage rates compared between the PCOS group and control group. Subgroup analysis and binary regression were used to analyze the influence of BMI on clinical outcomes among individuals diagnosed with PCOS.
Results: Non-obese PCOS patients exhibited higher cumulative pregnancy rates, cumulative live birth rates, and late miscarriage rates compared to the control group with the normal BMI population (84.7% vs71.2%, P < 0.001; 74.1% vs 61.6%, P < 0.001; 4.1% vs 2.0%, P = 0.002), but there was no significant difference in early miscarriage rates between the two groups.
Conclusion: Non-obese PCOS patients demonstrated a notably higher cumulative live birth rate but also a higher risk of late miscarriage compared to non-PCOS females with a normal BMI.
Keywords: body mass index, cumulative live birth rate, in vitro fertilization, intracytoplasmic sperm injection, late miscarriage, polycystic ovary syndrome
Introduction
Polycystic Ovary Syndrome (PCOS) is a complex endocrine disorder characterized primarily by a combination of clinical features, including hyperandrogenism, anovulation, and the presence of polycystic ovaries.1 The intricate physiopathology of PCOS remains elusive, with the complexity attributed to the intricate interplay of components, including genetic predisposition, neuroendocrine dysfunction, prenatal influences, and lifestyle factors.2–5 The global prevalence of PCOS among women of childbearing age varies, ranging from 6% to 21%.6–9 PCOS represents a significant contributor to ovulatory infertility, carrying substantial implications for those affected by the condition.10,11 Additionally, PCOS frequently coexists with metabolic disorders such as obesity, hyperlipidemia, insulin resistance, further complicating its clinical landscape.12,13
Assisted Reproductive Technology (ART), which includes approaches such as in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI), presents promising prospects for PCOS patients aiming to overcome their fertility challenges.11,14 The Cumulative Live Birth Rate (CLBR), a metric that considers outcomes from both fresh embryo transfer cycles and frozen embryo transfer (FET) cycles, provides a more comprehensive measure for assessing the overall success of IVF/ICSI interventions.15,16 The substantial response observed during ovarian stimulation in PCOS women contributes to an impressive CLBR of approximately 70%.17
It is crucial to acknowledge that although PCOS patients may exhibit enhanced reproductive capacity, the presence of underlying metabolic disorders underscores the potential for an increased vulnerability to pregnancy complications and adverse perinatal outcomes.18–21 While approximately 40–60% of PCOS patients are overweight or obese,22,23 a clinically significant subset maintains a normal body mass index (BMI < 25 kg/m²).24 These metabolic abnormalities extend beyond overweight or obese individuals with PCOS, impacting even those with a normal BMI.25 Research has emphasized the adverse impact of obesity on IVF outcomes, including live birth rates and the risk of miscarriage.26 However, there remains a notable scarcity of dedicated investigations specifically aimed at exploring the clinical outcomes of IVF/ICSI in individuals diagnosed with non-obese PCOS.
Accordingly, we conducted a comprehensive evaluation of the clinical outcomes among a cohort of PCOS patients undergoing IVF/ICSI treatment. Our particular emphasis was on comparing these outcomes, especially in relation to non-PCOS patients. The study aimed to provide valuable insights into the potential differences in treatment outcomes that could arise between non-obese and obese PCOS patient groups.
Materials and Methods
Study Design and Population
This retrospective study has undergone a thorough review and received approval from the Ethics Committee of the First Affiliated Hospital of Sun Yat-sen University. The study initially enrolled PCOS patients (n = 913) who underwent their first IVF/ICSI treatment at our reproductive center between January 2016 and December 2021. According to the Rotterdam Criteria, patients were diagnosed as PCOS if they met two of the three following criteria: oligoovulation or anovulation; hyperandrogenism; and polycystic ovaries.27 The control group (n = 5553) included patients who underwent first IVF/ICSI treatment due to fallopian tubal factor or male factor infertility. Both the PCOS and control groups were subjected to exclusion criteria encompassed: (1) age > 40 years; (2) diagnosis of recurrent spontaneous abortion, endometriosis, congenital uterine malformation, and intrauterine adhesions; (3) endocrine disorders such as Cushing’s syndrome, hyperprolactinemia, pituitary microadenoma, and thyroid dysfunction; (4) autoimmune diseases. Additionally, cases with missing information regarding cycles, embryos, and clinical pregnancy data were excluded from the analysis. The study ultimately comprised 787 PCOS patients and 4052 controls.
Ovarian Stimulation and Laboratory Protocols
All patients underwent ovarian stimulation, oocyte retrieval, and embryo transfers in accordance with standard protocols.28 Ovarian stimulation protocol was selected and carried out by female age and ovarian reserve function. Human chorionic gonadotropin (hCG) was administered when at least three follicles measured exceeded 18 mm to induce oocyte maturation. Oocyte retrieval was performed 36h later. Different fertilization methods were performed according to sperm quality. Embryo transfers followed a standard protocol, and patients received vaginal and/or intramuscular progesterone for luteal support. Fresh embryo transfers occurred on either day 3 or 5 days after oocyte retrieval. In cases where fresh embryo transfer was deemed unsuitable due to factors such as ovarian hyperstimulation syndrome (OHSS), inadequate endometrial thickness, or abnormal laboratory parameters, a comprehensive strategy involving the freezing of all embryos was adopted. For subsequent FET cycles, endometrial preparation was carried out using either natural cycles or hormone replacement therapy. Following successful embryo transfer and confirmation of clinical pregnancy, the administration of luteal support drugs was continued until the tenth week of pregnancy.
Main Outcome Measures
The clinical pregnancy was defined as the presence of a gestational sac detected via ultrasound examination four weeks after the embryo transfer procedure. Miscarriage events were categorized into early miscarriage, referring to pregnancy loss occurring prior to 12 weeks of gestation, and late miscarriage, defined as pregnancy loss transpiring between 12 and 24 weeks of gestation.29 The live birth rate was defined as the successful delivery of one or more live infants. The cumulative pregnancy rate was the proportion of at least one pregnancy per started cycle. The cumulative live births encompassed the live births arising from both fresh cycles and subsequent FET cycles subsequent to the same ovarian stimulation cycle, until the occurrence of one live birth or the exhaustion of all available embryos.
Statistical Analysis
The statistical analysis was conducted using SPSS software (version 26.0, Chicago, USA). Continuous variables that followed a normal distribution were presented as mean ± standard deviation, while continuous variables with non-normal distribution were described using median and interquartile range. Comparisons between continuous variables were performed using either the two tailed t-test or the Mann–Whitney U-test, depending on the distributional characteristics of the data. Categorical variables were presented as rates and percentages, and differences between groups were assessed using the chi-square test or Fisher’s exact test, as appropriate. Odds ratios (ORs) along with their corresponding 95% confidence intervals (CIs) were calculated to evaluate the strength of associations. Univariate analysis and multivariate analysis were performed by binary Logistics regression. Variables with statistical differences in the univariate analysis were included in the multivariate regression equation. Statistical significance was established at P < 0.05.
Results
Patient Characteristics
The primary baseline characteristics of the two cohorts are systematically outlined in Table 1. Notably, individuals diagnosed with PCOS displayed a slightly younger mean age in contrast to the control group (29.39 ± 3.53 vs 31.97 ± 4.28, P < 0.001). It is pertinent to highlight that patients grappling with PCOS exhibited a notably higher BMI when compared to their counterparts in the control group (22.60 ± 3.43 vs 21.50 ± 2.81, P < 0.001). Furthermore, discernible differences were observed in total testosterone levels, with the PCOS group showcasing significantly elevated values as compared to the control group (0.45 ± 0.16 vs 0.29 ± 0.11, P < 0.001). Of particular significance is the marked discrepancy in the distribution of infertility types between the two cohorts, with the PCOS group presenting a notably greater proportion of primary infertility cases (65.9% vs 35.3%, P < 0.001).
 |
Table 1 Baseline Characteristics of Patients with and without PCOS |
Ovarian Stimulation Results
Cycle characteristics and ART outcomes have been meticulously compiled in Table 2. Compared to the control group, the PCOS cohort exhibited a notably favorable ovarian response, characterized by a diminished total gonadotropin dosage and an augmented count of retrieved oocytes. Parallels were observed in oocyte maturation rates between the two groups. Encouragingly, the rates of both cleavage and blastocyst formation registered a slight elevation within the PCOS group as compared to the control group (97.8% vs 97.4%, P = 0.017 and 67.5% vs 64.3%, P < 0.001, respectively). Nonetheless, it is imperative to note that no significant discrepancy emerged in terms of the rate of high-quality embryos between these two cohorts.
 |
Table 2 Oocyte Retrieval Cycle Characteristics of the Patients in the PCOS Group and Control Group |
Pregnancy Outcomes
The embryo transfer outcomes are presented in Table 3. In comparison to the control group, the PCOS cohort exhibited notably elevated rates of clinical pregnancy, cumulative pregnancy, and cumulative live birth. Although the overall miscarriage rates in both groups displayed a semblance (15% vs 14.8%, P = 0.891), it is noteworthy that the late pregnant loss rate within the PCOS group surpassed that within the control group, with statistical significance (3.8% vs 2.3%, P = 0.023). Upon scrutinizing the embryo transfer cycle modalities, discernment reveals that the PCOS group registered higher abortion rates than the control group in the context of fresh embryo transfer cycles (21.2% vs 13.5%, P = 0.034). Moreover, while an upward trend in late miscarriage rate during FET cycles was observed within the PCOS group, this escalation did not attain statistical significance (3.4% vs 2.2%, P = 0.058).
 |
Table 3 Pregnancy Outcomes of Patients with and without PCOS |
Subgroup Analysis
In order to deepen our understanding of the potential influence of BMI on clinical outcomes among individuals diagnosed with PCOS, a meticulous subgroup analysis was conducted. This analysis involved the stratification of women into two distinct categories based on their BMI, as meticulously presented in Table 4. In non-obese people (BMI < 25 kg/m²), our findings illuminated a compelling trend: the PCOS group displayed notably elevated rates in cumulative pregnancy and live birth compared to the control group. It is of particular significance that the late miscarriage rate among non-obese PCOS patients stood higher compared to the control group (4.1% vs 2.05%, P = 0.002). In the obesity subgroup (BMI ≥ 25 kg/m²), PCOS women also showed a higher cumulative live birth rate than the control group, and there was a trend toward higher late miscarriage rate (4.9% vs 2.4%, P = 0.181), but the difference did not reach statistical significance.
 |
Table 4 Subgroup Analysis for the Effect of BMI on Reproductive Outcome Over Multiple IVF/ICSI Cycles in PCOS and Control Group |
Logistic Regression Analysis
To assess the comparative predictive capacity of variables including PCOS diagnosis, age, type of embryo transfer, BMI, and infertility type with respect to the late miscarriage rate, a logistic regression analysis was undertaken, as detailed in Table 5. The outcomes of this analysis unveiled significant associations between the diagnosis of PCOS and the late miscarriage rate (OR 1.811; 95% CI 1.110–2.957; P = 0.018). Additionally, it was discerned that BMI stands as an independent factor possessing predictive potential for the late miscarriage rate (OR 0.577, 95% CI; 1.081–2.931; P = 0.023).
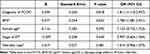 |
Table 5 Logistic Regression Analysis for the Prediction of Late Miscarriage Rate |
Discussion
The study’s findings reveal a significantly elevated CLBR among women diagnosed with PCOS compared to the control group. This distinction persists even among individuals within the obese subgroup. It is imperative to acknowledge that PCOS patients exhibit an increased susceptibility to late-stage miscarriage. Notably, this heightened risk of late pregnancy loss extends beyond the confines of obesity, affecting non-obese cohorts as well.
Compared to the ovaries of the normal population, those of patients with PCOS exhibit a greater follicle storage capacity,30 and the number of oocytes obtained plays a pivotal role in cumulative live birth outcomes.31,32 Numerous studies consistently report that the CLBR among PCOS patients exceeds that of control groups,33,34 even in women aged ≥ 35.35,36 Our findings align with prior research, reinforcing the notion that PCOS patients achieve higher CLBR than their non-PCOS counterparts. Obesity is recognized for its adverse impact on oocyte quantity and quality, as well as reduced endometrial receptivity,37,38 ultimately influencing embryo implantation and clinical pregnancy rates.39 Remarkably, the obese PCOS group still demonstrated a significantly higher CLBR compared to the control group. This phenomenon may be attributed to the superior oocyte reserve and increased availability of embryos among PCOS patients, surpassing the influence of obesity on patients’ internal environments and embryo quality, thus conferring enhanced fertility.
While women with PCOS may indeed exhibit improved reproductive potential, empirical findings emphasize the impact of inherent hormonal dysregulations in PCOS. These, combined with compromised oocyte quality and alterations in endometrial receptivity, exert significant influence on the outcomes of IVF/ICSI cycles.40,41 It is noteworthy that several comprehensive meta-analyses have rigorously investigated the clinical implications of IVF/ICSI procedures in women with PCOS, consistently revealing a higher propensity for miscarriage when compared to their non-PCOS counterparts.42–44 Recent research has also pointed towards an association between PCOS and increased rates of preclinical and early-stage pregnancy losses in IVF.45 In a retrospective study involving 2357 PCOS women who achieved pregnancy through IVF, a heightened incidence of late-stage miscarriage was observed among PCOS patients.46 Importantly, even after excluding embryo chromosomal anomalies, the frequency of miscarriages among PCOS patients remained notably higher than that within the control cohort.47 In alignment with these prior investigations, our current study similarly identifies an elevated risk of late miscarriage among PCOS patients compared to the control group.11,46–50 This consistency with previous research reaffirms the designation of PCOS as a substantive risk factor in relation to late miscarriage rates. Additionally, our study underscores the significance of BMI as a predictive parameter in assessing the likelihood of late miscarriages.
The intricate association between PCOS and miscarriages involves controversial molecular mechanisms. Elevated BMI in PCOS may profoundly impact sex hormone secretion and metabolism, influencing the bioavailability of estrogen and androgens and thereby affecting normal follicular development.51 Recent studies elucidate altered gene expression of steroid receptors and reduced expression of Hox10a, integrins, and Mmp9 in the implanted uterus region of PCOS animals.52 These changes, along with modified expression patterns of key angiogenic molecules in granulosa-lutein cells of women with PCOS and a compromised capacity to sustain vascularization, delineate impaired angiogenesis, potentially resulting in luteal phase insufficiency and and influencing the risk of pregnancy loss.53
Numerous studies have extensively investigated the heightened risk of abortion in PCOS patients with elevated BMI.54,55 However, it is surprising that clinical ART investigations and fertility outcomes in non-obese PCOS patients remain inadequately represented in the literature. A substantial proportion of clinically significant PCOS cases is characterized by normal or lower BMIs.56 Although PCOS patients with normal weight share certain clinical features with obese PCOS patients, it is believed to arise and develop endocrinopathy under distinct circumstances.57–59 PCOS patients with a normal BMI exhibit milder metabolic disturbances compared to their overweight counterparts, yet they still contend with metabolic challenges such as insulin resistance, hyperandrogenism, and low-grade chronic inflammation.60 These factors significantly contribute to the phenotypic expression of PCOS.61,62 In our study, we observed a higher incidence of late miscarriage among PCOS patients with a normal BMI when compared to the control population. Even after adjusting for obesity, non-obese PCOS patients continued to experience an elevated risk of adverse pregnancy outcomes.
When compared to BMI-matched healthy controls, women diagnosed with PCOS and falling into the emaciated category exhibit a range of pathophysiological abnormalities.63,64 Study had revealed a 4.4-fold increased prevalence of impaired glucose tolerance among lean PCOS patients.65 Moreover, there is evidence indicating that insulin resistance or hyperinsulinemia increases the risk of spontaneous abortion.66–68 Insights from a lean PCOS mouse model emphasize the correlation between reduced oocyte quality and the impairment of mitochondrial ultrastructure and function.69 Studies have documented aberrant expression of sex hormone receptors and co-expression receptors in the endometrium of PCOS patients.70 Additionally, there is conclusive evidence supporting the notion that insufficient trophoblast invasion and placental disorders in PCOS patients can lead to abortion and pregnancy complications.71–73 The mechanism contributing to the heightened risk of late-term abortion in PCOS may also be associated with alterations in endometrial metabolism. These alterations encompass disruptions in glucose metabolism, hyperinsulinemia, and hyperandrogenism, all of which can detrimentally affect endometrial function.74 The analysis from our study unambiguously demonstrates that even among individuals who are not obese, PCOS patients continue to confront an elevated risk of late-term miscarriage.
Our research is not without its limitations. Firstly, owing to the retrospective nature of the study, we were unable to investigate certain unidentified confounding factors, such as preemptive blood glucose control, lipid metabolism control, exercise, and weight loss, which might have influenced our findings. Secondly, there were varying degrees of missing data in the patients’ endocrine-related examinations, preventing further categorization based on blood glucose, insulin, and androgen levels. Additionally, our study did not track or analyze other potential pregnancy complications in patients. Lastly, to obtain a more comprehensive understanding of the relationship between PCOS and miscarriage, a prospective clinical trial is warranted, incorporating comprehensive clinical parameters such as BMI, hormone status, age, phenotype, and other relevant variables.
In conclusion, this study conducted a thorough examination of pregnancy outcomes in a cohort of patients undergoing IVF/ICSI cycles, uncovering an elevated CLBR specific to PCOS patients. Concurrently, a heightened susceptibility to late miscarriages was observed among non-obese PCOS individuals. It is of paramount importance for clinicians to be cognizant of these associations and to offer appropriate counseling and monitoring to mitigate the risk of late miscarriage in non-obese women with PCOS.
Ethics Approval and Consent to Participate
This study was approved by the Ethics Committee of the First Affiliated Hospital, Sun Yat-sen University [No. IIT-2023–593]. All procedures were performed in accordance with the Declaration of Helsinki. Since this retrospective study analyzed the medical records obtained in the past clinical diagnosis and treatment, the Ethics Committee of the First Affiliated Hospital, Sun Yat‑sen University agreed to waive the patient’s written informed consent.
Acknowledgments
This study is supported by Guangdong Provincial Key Laboratory of Reproductive Medicine [No:2020B1212090029] and Key-Area Research and Development Program of Guangdong Province [No: 2023B1111020006]. We thank all participants involved in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Robin G, Gallo C, Catteau-Jonard S, et al. Polycystic Ovary-Like Abnormalities (PCO-L) in women with functional hypothalamic amenorrhea. J Clin Endocrinol Metab. 2012;97(11):4236–4243. doi:10.1210/jc.2012-1836
2. Ehrmann DA. Polycystic ovary syndrome. N Engl J Med. 2005;352(12):1223–1236. doi:10.1056/NEJMra041536
3. Dapas M, Dunaif A. Deconstructing a syndrome: genomic insights into PCOS causal mechanisms and classification. Endocr Rev. 2022;43(6):927–965. doi:10.1210/endrev/bnac001
4. Radwan RA, Abuelezz NZ, Abdelraouf SM, Bakeer EM, Rahman A. Decreased serum level of gamma-amino butyric acid in Egyptian infertile females with polycystic ovary syndrome is correlated with dyslipidemia, total testosterone and 25(OH) Vitamin D levels. J Med Biochem. 2019;38(4):512–518. doi:10.2478/jomb-2018-0051
5. Ullah A, Jahan S, Razak S, et al. Protective effects of GABA against metabolic and reproductive disturbances in letrozole induced polycystic ovarian syndrome in rats. J Ovarian Res. 2017;10(1):62. doi:10.1186/s13048-017-0359-7
6. Bozdag G, Mumusoglu S, Zengin D, Karabulut E, Yildiz BO. The prevalence and phenotypic features of polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 2016;31(12):2841–2855. doi:10.1093/humrep/dew218
7. Diamanti-Kandarakis E, Kandarakis H, Legro RS. The role of genes and environment in the etiology of PCOS. Endocrine. 2006;30(1):19–26. doi:10.1385/ENDO:30:1:
8. Lizneva D, Suturina L, Walker W, Brakta S, Gavrilova-Jordan L, Azziz R. Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertil Steril. 2016;106(1):6–15. doi:10.1016/j.fertnstert.2016.05.003
9. March WA, Moore VM, Willson KJ, Phillips DI, Norman RJ, Davies MJ. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod. 2010;25(2):544–551. doi:10.1093/humrep/dep399
10. Azziz R, Carmina E, Chen Z, et al. Polycystic ovary syndrome. Nat Rev Dis Primers. 2016;2:16057. doi:10.1038/nrdp.2016.57
11. Balen AH, Morley LC, Misso M, et al. The management of anovulatory infertility in women with polycystic ovary syndrome: an analysis of the evidence to support the development of global WHO guidance. Hum Reprod Update. 2016;22(6):687–708. doi:10.1093/humupd/dmw025
12. Gilbert EW, Tay CT, Hiam DS, Teede HJ, Moran LJ. Comorbidities and complications of polycystic ovary syndrome: an overview of systematic reviews. Clin Endocrinol. 2018;89(6):683–699. doi:10.1111/cen.13828
13. Kalra S, Aggarwal S, Khandelwal D. Thyroid dysfunction and dysmetabolic syndrome: the need for enhanced thyrovigilance strategies. Int J Endocrinol. 2021;2021:9641846. doi:10.1155/2021/9641846
14. Della Corte L, Foreste V, Barra F, et al. Current and experimental drug therapy for the treatment of polycystic ovarian syndrome. Expert Opin Investig Drugs. 2020;29(8):819–830. doi:10.1080/13543784.2020.1781815
15. Devesa M, Tur R, Rodriguez I, Coroleu B, Martinez F, Polyzos NP. Cumulative live birth rates and number of oocytes retrieved in women of advanced age. A single centre analysis including 4500 women >/=38 years old. Hum Reprod. 2018;33(11):2010–2017. doi:10.1093/humrep/dey295
16. Maheshwari A, McLernon D, Bhattacharya S. Cumulative live birth rate: time for a consensus? Hum Reprod. 2015;30(12):2703–2707. doi:10.1093/humrep/dev263
17. Mackens S, Drakopoulos P, Moeykens MF, et al. Cumulative live birth rate after ovarian stimulation with freeze-all in women with polycystic ovaries: does the polycystic ovary syndrome phenotype have an impact? Reprod Biomed Online. 2022;44(3):565–571. doi:10.1016/j.rbmo.2021.11.009
18. Palomba S, La Sala GB. Pregnancy complications in women with polycystic ovary syndrome: importance of diagnostic criteria or of phenotypic features? Hum Reprod. 2016;31(1):223–224. doi:10.1093/humrep/dev284
19. Bahri Khomami M, Boyle JA, Tay CT, et al. Polycystic ovary syndrome and adverse pregnancy outcomes: current state of knowledge, challenges and potential implications for practice. Clin Endocrinol. 2018;88(6):761–769. doi:10.1111/cen.13579
20. Li Y, Ruan X, Wang H, et al. Comparing the risk of adverse pregnancy outcomes of Chinese patients with polycystic ovary syndrome with and without antiandrogenic pretreatment. Fertil Steril. 2018;109(4):720–727. doi:10.1016/j.fertnstert.2017.12.023
21. Kelley AS, Smith YR, Padmanabhan V. A narrative review of placental contribution to adverse pregnancy outcomes in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2019;104(11):5299–5315. doi:10.1210/jc.2019-00383
22. Ademoglu EN, Gorar S, Carlıoglu A, et al. Plasma nesfatin-1 levels are increased in patients with polycystic ovary syndrome. J Endocrinol Invest. 2014;37(8):715–719. doi:10.1007/s40618-014-0089-2
23. Ganie MA, Vasudevan V, Wani IA, Baba MS, Arif T, Rashid A. Epidemiology, pathogenesis, genetics & management of polycystic ovary syndrome in India. Indian J Med Res. 2019;150(4):333–344. doi:10.4103/ijmr.IJMR_1937_17
24. Toosy S, Sodi R, Pappachan JM. Lean polycystic ovary syndrome (PCOS): an evidence-based practical approach. J Diabetes Metab Disord. 2018;17(2):277–285. doi:10.1007/s40200-018-0371-5
25. Mirza FG, Tahlak MA, Rjeili RB, et al. Polycystic Ovarian Syndrome (PCOS): does the challenge end at conception? Int J Environ Res Public Health. 2022;19(22):14914 doi:10.3390/ijerph192214914.
26. Ribeiro LM, Sasaki LMP, Silva AA, et al. Overweight, obesity and assisted reproduction: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2022;271:117–127. doi:10.1016/j.ejogrb.2022.01.019
27. Rotterdam EA-SPCWG. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19–25. doi:10.1016/j.fertnstert.2003.10.004
28. Chen ZJ, Shi Y, Sun Y, et al. Fresh versus frozen embryos for infertility in the polycystic ovary syndrome. N Engl J Med. 2016;375(6):523–533. doi:10.1056/NEJMoa1513873
29. Giakoumelou S, Wheelhouse N, Cuschieri K, Entrican G, Howie SE, Horne AW. The role of infection in miscarriage. Hum Reprod Update. 2016;22(1):116–133. doi:10.1093/humupd/dmv041
30. Webber LJ, Stubbs S, Stark J, et al. Formation and early development of follicles in the polycystic ovary. Lancet. 2003;362(9389):1017–1021. doi:10.1016/s0140-6736(03)14410-8
31. Drakopoulos P, Blockeel C, Stoop D, et al. Conventional ovarian stimulation and single embryo transfer for IVF/ICSI. How many oocytes do we need to maximize cumulative live birth rates after utilization of all fresh and frozen embryos? Hum Reprod. 2016;31(2):370–376. doi:10.1093/humrep/dev316
32. Polyzos NP, Drakopoulos P, Parra J, et al. Cumulative live birth rates according to the number of oocytes retrieved after the first ovarian stimulation for in vitro fertilization/intracytoplasmic sperm injection: a multicenter multinational analysis including approximately 15,000 women. Fertil Steril. 2018;110(4):661–670 e1. doi:10.1016/j.fertnstert.2018.04.039
33. Su N, Zhan J, Xie M, et al. High anti-Mullerian hormone level is adversely associated with cumulative live birth rates of two embryo transfers after the first initiated cycle in patients with polycystic ovary syndrome. Front Endocrinol. 2023;14:1123125. doi:10.3389/fendo.2023.1123125
34. Kuivasaari-Pirinen P, Hippelainen M, Hakkarainen H, Randell K, Heinonen S. Cumulative baby take-home rate among women with PCOS treated by IVF. Gynecol Endocrinol. 2010;26(8):582–589. doi:10.3109/09513591003632043
35. Mai Z, Liu M, Pan P, et al. Comparison of cumulative live birth rate between aged PCOS women and controls in IVF/ICSI cycles. Front Endocrinol. 2021;12:724333. doi:10.3389/fendo.2021.724333
36. Guan Y, Kong P, Xiao Z, et al. Independent variables for determining the cumulative live birth rates of aged patients with polycystic ovary syndrome or tubal factor infertility: a retrospective cohort study. Front Endocrinol. 2021;12:728051. doi:10.3389/fendo.2021.728051
37. Lin J, Huang J, Wang N, Kuang Y, Cai R. Effects of pre-pregnancy body mass index on pregnancy and perinatal outcomes in women with PCOS undergoing frozen embryo transfer. BMC Pregnancy Childbirth. 2019;19(1):487. doi:10.1186/s12884-019-2611-1
38. Pinborg A, Gaarslev C, Hougaard CO, et al. Influence of female bodyweight on IVF outcome: a longitudinal multicentre cohort study of 487 infertile couples. Reprod Biomed Online. 2011;23(4):490–499. doi:10.1016/j.rbmo.2011.06.010
39. Provost MP, Acharya KS, Acharya CR, et al. Pregnancy outcomes decline with increasing body mass index: analysis of 239,127 fresh autologous in vitro fertilization cycles from the 2008–2010 Society for Assisted Reproductive Technology registry. Fertil Steril. 2016;105(3):663–669. doi:10.1016/j.fertnstert.2015.11.008
40. Singh N, Mishra N, Dogra Y. Do basal luteinizing hormone and luteinizing hormone/follicle-stimulating hormone ratio have significance in prognosticating the outcome of in vitro fertilization cycles in polycystic ovary syndrome? J Hum Reprod Sci. 2021;14(1):21–27. doi:10.4103/jhrs.JHRS_96_20
41. Jayasena CN, Franks S. The management of patients with polycystic ovary syndrome. Nat Rev Endocrinol. 2014;10(10):624–636. doi:10.1038/nrendo.2014.102
42. Sha T, Wang X, Cheng W, Yan Y. A meta-analysis of pregnancy-related outcomes and complications in women with polycystic ovary syndrome undergoing IVF. Reprod Biomed Online. 2019;39(2):281–293. doi:10.1016/j.rbmo.2019.03.203
43. Yu HF, Chen HS, Rao DP, Gong J. Association between polycystic ovary syndrome and the risk of pregnancy complications: a PRISMA-compliant systematic review and meta-analysis. Medicine. 2016;95(51):e4863. doi:10.1097/MD.0000000000004863
44. Bahri Khomami M, Joham AE, Boyle JA, et al. Increased maternal pregnancy complications in polycystic ovary syndrome appear to be independent of obesity-A systematic review, meta-analysis, and meta-regression. Obes Rev. 2019;20(5):659–674. doi:10.1111/obr.12829
45. Matorras R, Pijoan JI, Lainz L, et al. Polycystic ovarian syndrome and miscarriage in IVF: systematic revision of the literature and meta-analysis. Arch Gynecol Obstet. 2023;308(2):363–377. doi:10.1007/s00404-022-06757-0
46. Cai H, Mol BW, Gordts S, et al. Early and late pregnancy loss in women with polycystic ovary syndrome undergoing IVF/ICSI treatment: a retrospective cohort analysis of 21 820 pregnancies. BJOG. 2021;128(7):1160–1169. doi:10.1111/1471-0528.16590
47. Jie HY, Zhou X, Zhao MP, Hu M, Mai QY, Zhou CQ. Pregnancy outcomes in patients with polycystic ovary syndrome who conceived after single thawed blastocyst transfer: a propensity score-matched study. BMC Pregnancy Childbirth. 2022;22(1):718. doi:10.1186/s12884-022-05011-4
48. Liu S, Mo M, Xiao S, et al. Pregnancy outcomes of women with polycystic ovary syndrome for the first in vitro fertilization treatment: a retrospective cohort study with 7678 patients. Front Endocrinol. 2020;11:575337. doi:10.3389/fendo.2020.575337
49. Yang AM, Xu X, Han Y, et al. Risk factors for different types of pregnancy losses: analysis of 15,210 pregnancies after embryo transfer. Front Endocrinol. 2021;12:683236. doi:10.3389/fendo.2021.683236
50. Yang L, Ni T, Huang Y, et al. Impact of a previous late miscarriage on subsequent pregnancy outcomes: a retrospective cohort study over 10 years. Int J Gynaecol Obstet. 2023;163(2): 610–617. doi:10.1002/ijgo.14862
51. Talmor A, Dunphy B. Female obesity and infertility. Best Pract Res Clin Obstet Gynaecol. 2015;29(4):498–506. doi:10.1016/j.bpobgyn.2014.10.014
52. Dhadhal S, Nampoothiri L. Decoding the molecular cascade of embryonic-uterine modulators in pregnancy loss of PCOS mother- an ”in vivo” study. Reprod Biol Endocrinol. 2022;20(1):165. doi:10.1186/s12958-022-01041-x
53. Patil K, Hinduja I, Mukherjee S. Alteration in angiogenic potential of granulosa-lutein cells and follicular fluid contributes to luteal defects in polycystic ovary syndrome. Hum Reprod. 2021;36(4):1052–1064. doi:10.1093/humrep/deaa351
54. Yang ST, Liu CH, Ma SH, et al. Association between pre-pregnancy overweightness/obesity and pregnancy outcomes in women with polycystic ovary syndrome: a systematic review and meta-analysis. Int J Environ Res Public Health. 2022;19(15):9094 doi:10.3390/ijerph19159094.
55. Romanski PA, Bortoletto P, Magaoay B, Chung A, Rosenwaks Z, Spandorfer SD. Live birth outcomes in infertile patients with class III and class IV obesity following fresh embryo transfer. J Assist Reprod Genet. 2021;38(2):347–355. doi:10.1007/s10815-020-02011-1
56. Teede HJ, Misso ML, Costello MF, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018;33(9):1602–1618. doi:10.1093/humrep/dey256
57. Saxena P, Prakash A, Nigam A, Mishra A. Polycystic ovary syndrome: is obesity a sine qua non? A clinical, hormonal, and metabolic assessment in relation to body mass index. Indian J Endocrinol Metab. 2012;16(6):996–999. doi:10.4103/2230-8210.103011
58. Doh E, Mbanya A, Kemfang-Ngowa JD, et al. The relationship between adiposity and insulin sensitivity in African women living with the polycystic ovarian syndrome: a clamp study. Int J Endocrinol. 2016;2016:9201701. doi:10.1155/2016/9201701
59. Diamanti-Kandarakis E, Dunaif A. Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocr Rev. 2012;33(6):981–1030. doi:10.1210/er.2011-1034
60. Dumesic DA, Oberfield SE, Stener-Victorin E, Marshall JC, Laven JS, Legro RS. Scientific statement on the diagnostic criteria, epidemiology, pathophysiology, and molecular genetics of polycystic ovary syndrome. Endocr Rev. 2015;36(5):487–525. doi:10.1210/er.2015-1018
61. Pasquali R. Obesity and androgens: facts and perspectives. Fertil Steril. 2006;85(5):1319–1340. doi:10.1016/j.fertnstert.2005.10.054
62. Stepto NK, Cassar S, Joham AE, et al. Women with polycystic ovary syndrome have intrinsic insulin resistance on euglycaemic-hyperinsulaemic clamp. Hum Reprod. 2013;28(3):777–784. doi:10.1093/humrep/des463
63. Han Y, Kim HS, Lee HJ, Oh JY, Sung YA. Metabolic effects of polycystic ovary syndrome in adolescents. Ann Pediatr Endocrinol Metab. 2015;20(3):136–142. doi:10.6065/apem.2015.20.3.136
64. Song DK, Hong YS, Sung YA, Lee H. Insulin resistance according to beta-cell function in women with polycystic ovary syndrome and normal glucose tolerance. PLoS One. 2017;12(5):e0178120. doi:10.1371/journal.pone.0178120
65. Kakoly NS, Khomami MB, Joham AE, et al. Ethnicity, obesity and the prevalence of impaired glucose tolerance and type 2 diabetes in PCOS: a systematic review and meta-regression. Hum Reprod Update. 2018;24(4):455–467. doi:10.1093/humupd/dmy007
66. Ke RW. Endocrine basis for recurrent pregnancy loss. Obstet Gynecol Clin North Am. 2014;41(1):103–112. doi:10.1016/j.ogc.2013.10.003
67. Grodnitskaya EE, Kurtser MA. Homocysteine metabolism in polycystic ovary syndrome. Gynecol Endocrinol. 2012;28(3):186–189. doi:10.3109/09513590.2011.589927
68. Glueck CJ, Streicher P, Wang P. Treatment of polycystic ovary syndrome with insulin-lowering agents. Expert Opin Pharmacother. 2002;3(8):1177–1189. doi:10.1517/14656566.3.8.1177
69. Chappell NR, Zhou B, Schutt AK, Gibbons WE, Blesson CS. Prenatal androgen induced lean PCOS impairs mitochondria and mRNA profiles in oocytes. Endocr Connect. 2020;9(3):261–270. doi:10.1530/EC-19-0553
70. Palomba S, Piltonen TT, Giudice LC. Endometrial function in women with polycystic ovary syndrome: a comprehensive review. Hum Reprod Update. 2021;27(3):584–618. doi:10.1093/humupd/dmaa051
71. Palomba S, Russo T, Falbo A, et al. Decidual endovascular trophoblast invasion in women with polycystic ovary syndrome: an experimental case-control study. J Clin Endocrinol Metab. 2012;97(7):2441–2449. doi:10.1210/jc.2012-1100
72. Palomba S, Falbo A, Chiossi G, et al. Early trophoblast invasion and placentation in women with different PCOS phenotypes. Reprod Biomed Online. 2014;29(3):370–381. doi:10.1016/j.rbmo.2014.04.010
73. Zhang B, Wei D, Legro RS, et al. Obstetric complications after frozen versus fresh embryo transfer in women with polycystic ovary syndrome: results from a randomized trial. Fertil Steril. 2018;109(2):324–329. doi:10.1016/j.fertnstert.2017.10.020
74. Schulte MM, Tsai JH, Moley KH. Obesity and PCOS: the effect of metabolic derangements on endometrial receptivity at the time of implantation. Reprod Sci. 2015;22(1):6–14. doi:10.1177/1933719114561552
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
