Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 15
Health-Related Quality of Life in Sudanese Children with Nephrotic Syndrome: A Comparative Cross-Sectional Study
Authors Naim FS , Bakhiet YM, Mohmmedahmed MA, Yousef BA
Received 27 August 2023
Accepted for publication 22 March 2024
Published 28 March 2024 Volume 2024:15 Pages 133—144
DOI https://doi.org/10.2147/PHMT.S437364
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Roosy Aulakh
Fatima S Naim,1 Yassir M Bakhiet,2 Mohmmed A Mohmmedahmed,3 Bashir A Yousef4
1Department of Clinical Pharmacy, Faculty of Pharmacy, University of Khartoum, Khartoum, Sudan; 2Department of Pediatric Nephrology, Soba University Hospital, Khartoum, Sudan; 3Department of Pediatric Cardiology, Sudan Heart Centre, Khartoum, Sudan; 4Department of Pharmacology, Faculty of Pharmacy, University of Khartoum, Khartoum, Sudan
Correspondence: Bashir A Yousef, Department of Pharmacology, Faculty of Pharmacy, University of Khartoum, Al-Qasr Ave, Khartoum, 11111, Sudan, Tel +249155662037, Fax +249183780696, Email [email protected]
Background: Nephrotic syndrome (NS) is an essential chronic disease in children that has a major impact on a child’s health-related quality of life (HRQoL). This study aimed to evaluate the HRQoL of Sudanese children with NS and clinical parameters that can influence their HRQoL.
Methods: This study was a descriptive cross-sectional of children with NS conducted in Khartoum state hospitals. A standardized PedsQLTM 4.0 Scale Score evaluated the HRQoL of the participants. Patients’ socio-demographics, clinical data, and disease complications were collected using a data collection sheet. This study assessed the HRQoL of children with NS and compared it with apparent age and sex-matched to three groups (healthy children, children with chronic diseases, and kidney-transplanted children).
Results: 80 children with NS were recruited from April to August 2021. Children over eight years old represented (63.8%) of the study subjects. The total mean HRQoL scores of nephrotic children were significantly lower than those of healthy children (78.46 ± 24.01) (p = 0.001) and those with other chronic diseases (78.45 ± 24.01) (p= 0.006); however, it was not significantly different from those with kidney transplantation. Socio-demographics did not significantly affect the total mean HRQoL scores of children with NS. Clinical parameters such as the duration of illness, “less than one year” (p= 0.006), and the minimum change nephropathy histopathology (p= 0.035) significantly lowered the total mean HRQoL scores of NS children. Regression analysis further confirmed that edema, proteinuria, and hospital admission had a high impact on the total mean HRQoL.
Conclusion: The total mean HRQoL scores of children with NS were low and significantly lower than healthy children. Parameters such as the patient’s socio-demographics and phenotype of NS had no significant effect on the total mean HRQoL scores of children with NS. However, other clinical parameters significantly lowered their total mean HRQoL scores.
Keywords: health-related quality of life, nephrotic syndrome, clinical parameters, Sudanese children
Introduction
Nephrotic syndrome (NS) is a clinical syndrome characterized by the alteration of glomerular capillary wall permeability that leads to massive proteinuria (greater than 40 mg/m2/h), hypoalbuminemia (less than 30 g/L), with resulting hyperlipidemia, edema, and various complications.1 NS is the most common glomerular disease in pediatric nephrology, with an incidence of about 1.15–16.9 per 100,000 children.2 Etiologically, around 80% of NS is characterized by normal renal histology and known as NS with minimum change nephropathy (MCN), while the remaining have non-minimum change nephropathy such as focal segmental glomerulopathy (FSGP) and membranous nephropathy (MN).1,3 Based on the response to corticosteroids treatment, NS is classified into steroid-resistant nephrotic syndrome (SRNS), steroid-sensitive nephrotic syndrome (SSNS), steroid-dependent nephrotic syndrome (SDNS), and frequently relapsing nephrotic syndrome (FRNS).3 NS in children may lead to several acute or chronic complications such as infections, thromboembolic, and cardiovascular disease. Another important complication of NS is the psychological impact on children and their families and their quality of life.4
The World Health Organization defines quality of life (QoL) as
The individual’s perception of their position in life in the context of culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns.5
The health-related quality of life (HRQoL) is a multi-dimensional concept consisting of the patient’s perception of the impact of disease and its treatment on their functional aspects, including the psychological, physical, and social aspects.6,7 A high score of HRQoL means the function of health is better. It is an important outcome that allows the patient to understand the impact of the disease and the treatment on different life aspects.8 There have been several standard questionnaires used to measure HRQoL in children. The pediatrics quality of life inventory questionnaire (PedsQL™ 4.0) is one of the most commonly used questionnaires.9
The chronic and relapsing characteristics of NS and the long-term use of immunosuppressant therapy as “a core treatment” can significantly affect the HRQoL of children. Traditional management of NS usually focuses on the function of the affected organ. They rarely consider the functional impairments of health (ie, physical, social, and emotional).10 The policymaker’s decisions regarding the management of NS should focus on strategies to improve the organ’s function and include strategies to improve their HRQoL. Addressing patients’ QoL during patient care will lead to an improvement in clinical outcomes.11,12
Worldwide, several studies have demonstrated the negative impact of NS on the HRQoL of children patients and addressed the clinical parameters affecting their HRQoL. A systematic review conducted to determine the reliability of current generic quality-of-life instruments in assessing HRQoL among children and adolescents with idiopathic nephrotic syndrome (INS) found that the HRQoL scores in patients with INS were consistently low, whereas the scores of INS were higher than the scores of other chronic diseases.13 A study conducted at the University of Nigeria teaching hospital, found that; HRQoL was worse in the presence of edema and disease severity. Also, it found that the greater the degree of proteinuria in nephrotic children, the more impact on HRQoL there is. Furthermore, subjects who had SRNS had a poorer score in the emotional domain than those who were steroid-sensitive.10 Another study found that the general QoL of children with INS substantially declined compared with that of healthy children. The QoL of children with SDNS and SRNS was lower than the steroid-responsive type. It also found that the QoL of children who completed their treatment was higher than the group being treated. In addition, the longer the duration of treatment, the more children’s QoL declined.14
Emotional and social domains of HRQOL in children with chronic illnesses have been considered to be primarily related to ethnic, cultural, societal practices, and socioeconomic.15 In addition, NS in white adults is most commonly due to membranous nephropathy, whereas, in Africans, it is due to FSGS; also, African children have a particular pattern of NS, with the majority being SRNS.16 All these factors make the situation of African children different from that of the Western world. Furthermore, reports on the HRQoL of NS children from developing countries are insufficient.17,18 In Sudan, mainly, there is a lack of information regarding the HRQoL of children with NS and factors that can influence it; there is only one study that assessed the HRQoL of nephrotic children.19 Therefore, this study was undertaken to fill this information gap and support the research in developing African countries.
Methodology
Study Design & Setting
This comparative cross-sectional study was conducted on a sample of Sudanese children with diagnosed nephrotic syndrome. The participants were recruited from Khartoum state’s governmental hospitals with pediatric nephrology units, including Gaffer Ibn Auf Hospital, Soba Teaching Hospital, and Mohamed Alamin Hamid Pediatric Center.
Participants and Sampling Techniques
The study population was children with NS for the case group. Participants were selected by the convenient sampling method. Total coverage was done for patients in the hospital’s ward (inpatients) and patients who came to the referral clinic (outpatients) from April to August 2021. All children diagnosed with NS aged 2–18 years were included in the study (80 children). At the same time, children and caregivers who refused to participate were excluded from the study.
The study also included another 170 children aged 2–18, distributed into three comparable groups. Group 1 (healthy children), with a sample size of 80 children, was recruited from the regions near the hospitals. Group 2 contained 65 children without NS and had other chronic diseases such as asthma, diabetes mellitus, hyperthyroidism, and sickle cell anemia. Group 3 was recruited from children who had kidney transplantation, and its sample size was 25 patients. Children in groups 2 and 3 were recruited from the same hospitals in the study area. All children in the comparable groups were matched to NS children according to their demographic characteristics (age and gender), except the third group was matched only to the nephrotic children over ten years old because most of the kidney transplantation children who came to the hospitals during this study duration, their age were over ten years old.
Data Collection Tools
A standardized Arabic version of the PedsQL™ 4.0 Generic Core Scales was used. The PedsQL™ 4.0 is a brief and standardized instrument that systematically assesses the perceptions of patients with health problems about their HRQoL. The PedsQL™ 4.0 is a suitable age questionnaire. It has four versions according to age: (2–4) years, (5–7) years, (8–12) years, and (13–18) years. Each version contains a form for child and parent reports, except for ages (2–4) years, which only includes parents’ report forms. A data collection sheet was used to collect other information, such as disease complications.20 Information such as children’s demographic data and laboratory investigations were obtained by the data collection sheet from the participants’ medical files, and some data were obtained from their pediatric nephrologists.
Study Scenario
Before the primary investigation, a pilot study with 20 participants was conducted. Five participants for each study group (NS, healthy children, children with chronic diseases, and kidney transplanted children). All participants accurately answered the questions within 5–10 minutes, and there was no difficulty answering. Participants in the pilot study were not included in the main study. The participants were chosen based on the clinical and laboratory data from their medical files, and the selection was discussed and confirmed with the pediatric nephrologists.
After describing the study’s purpose, the participants were instructed on how to complete the PedsQLTM 4.0 questionnaire. If the child is over five and is well-oriented, the data was collected from them; otherwise, it was obtained from their caregivers. The questionnaire’s items were scored on a five-point Likert scale ranging from zero (never) to four (always) (Almost Always). The results were inverted and translated to a 0–100 scale, with 0= 100, 1= 75, 2= 50, 3= 25, and 4= 0.
Data Analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS) for Windows, Version 25 software (Armonk, NY: IBM Corp). Descriptive statistics (frequency tables) were used to describe the participants’ baseline data and clinical characteristics. Inferential statistics (unpaired t-test and ANOVA test) were used to examine the association between HRQoL scores (dependent variable) and different sociodemographic and clinical variables (independent variables). A linear regression analysis using all variables was conducted to estimate the significant predictors for the total HRQoL scores. Odds ratios (ORs) and 95% confidence intervals (CIs) were reported. An unpaired t-test was also applied to test the statistical difference in the HRQoL scores between different groups. P-value ≤ 0.05 was considered statistically significant.
Ethical Consideration
The study was conducted agreeing with the recommendations of the Declaration of Helsinki and approved by the Ethics Committee of the Faculty of Pharmacy, University of Khartoum (FPEC-04-2021). Permission for the use of PedsQL™ 4.0 was granted by the developer, Dr. James W.Varni, at the Mapi Research Trust in France. Before data collection, written informed consent was taken from children eight years and older, after providing informed consent from their parents/caregivers. For children under eight years, parents/caregivers signed a written informed permission form. The data collected from all study participants was coded to maintain confidentiality throughout the study.
Results
Out of eighty children with NS, males represented (67.5%), and children over eight years represented (63.8%) of the study subjects. Most of these cases originated from the center of Sudan (40%). The most common phenotype of NS was SSNS (38.8%), followed by SRNS (33.8%). Moreover, the most common histopathology was FSGS (18.75%). The most common disease-related complication was hypertension (61.2%) (Table 1).
 |
Table 1 Distribution of Socio-Demographic Characteristics and Disease State Among the Children Patients with Nephrotic Syndrome (n=80) |
Regarding the socio-demographic characteristics affecting HRQoL of nephrotic children, children of different age groups had no significant difference in their physical, emotional, social, and total mean HRQoL scores. However, they significantly differed in school performance (as teens had significantly lower school scores (P = 0.018) than other age groups). Moreover, no significant difference exists between the different genders and origins in the HRQoL domains and the total mean HRQoL scores (Table 2).
 |
Table 2 Distribution of Health-Related Quality of Life (HRQoL) According to Various Socio-Demographic Characteristics of Children with Nephrotic Syndrome (N= 80) |
With regards to clinical parameters affecting HRQoL of nephrotic children, the histopathology of NS was found to affect some domains of HRQoL (as children with MCNS had significantly lower scores in the emotional (70.8 ± 37.46) (P= 0.003), social domains (71 ± 39.3) (P= 0.006), and the total mean HRQoL scores (67.84 ± 30.6) (P= 0.035) than children who had Non-MCNS). In addition to that, the disease duration also affected the HRQoL; (as children with a disease duration of less than one year had significantly lower scores of physical (69.28 ± 34.5) (P= 0.001), social domains (77.1 ± 31.3) (P= 0.014), and total mean HRQoL scores (73.09 ± 27.22) (P= 0.006) than children with a duration of more than one year) (Table 3). Moreover, hospital admission had a significant effect on some domains of HRQoL such that; (inpatients had lower scores in physical (45.19 ± 37.7) (P= 0.003), emotional (47.7 ± 34.7) (P = 0.013), and social domains (55 ± 38.24) (P= 0.001) than outpatients) (Table 3).
 |
Table 3 Distribution of Health-Related Quality of Life (HRQoL) According to Various Clinical Data of Children with Nephrotic Syndrome (N= 80) |
In comparison between the different degrees of proteinuria (+1, +2, and +3 urine dipstick), children’s had a greater degree of proteinuria (+3 urine dipstick) were found to have significantly lowest scores in all domains of HRQoL (except the emotional domain) as follows: physical (61.3 ± 36.3) (p= 0.006*), social (67.2 ± 37.2) (p= 0.024*), the school performances (56 ± 33.8) (P = 0.044) and the total mean HRQoL score (63.69 ± 29.3) (p=0.009*) (Table 3). Furthermore, the findings manifested that patients on treatment had a significantly lower physical (76.5 ± 30) (P= 0.021), emotional (78.8 ± 30) (P= 0.001), and social (81.8 ± 29.4) (P= 0.005) and total mean HRQoL scores (76.5 ± 24.8) (P= 0.008) than patients who were not on treatment. Children with edema had significantly lowered scores of physical, emotional, social, and total mean HRQoL than children without edema (Table 3). However, there is no significant difference between the phenotypes of NS in all domains of HRQoL and total means HRQoL scores. (Table 3). Concerning the effect of disease complications on the HRQoL of nephrotic children, children with hypertension had an emotional domain significantly lower (73.0645 ± 32.80) (P= 0.017) than children with no hypertension. Children with infections had significantly lower physical, emotional, social, and total mean HRQoL scores than children without infection (Table 4).
 |
Table 4 Distribution of Health-Related Quality of Life (HRQoL) According to Various Disease Complications and Treatment Approaches for Children with Nephrotic Syndrome (N= 80) |
The results of linear regression analysis for the predictors of the total HRQoL score are shown in Table 5. Among these predictors, patients who had edema were 17.879 lower total mean HRQoL compared to non-edematous patients [OR = −17.879 (95% CI = −7.889– −27.869)]. As the degree of proteinuria increases by one point, this leads to a decrease in total mean HRQoL an average of −7.285 [OR = −7.285 (95% CI = −11.587– −2.984)]. Moreover, admitted NS patients had 36.834 lower total mean HRQoL as compared to NS outpatients [OR = −36.834 (95% CI = −24.847– −48.821)].
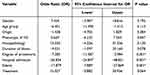 |
Table 5 Linear Regression Analysis for the Predictors of the Total Health-Related Quality of Life (HRQoL) Score for Children with Nephrotic Syndrome (N= 80) |
As demonstrated in Table 6, the control group demographic data was selected to be closely matched to the NS group; males represented (66.3%) of the healthy group and (66.1%) of the chronic disease group; this closely related to the male percentage in the NS group (67.5%). Similarly, the distribution of children according to age groups was closely matched between the NS, healthy, and chronic disease groups. Meanwhile, twenty-five patients were matched demographically from the kidney transplantation group to twenty-five patients in the NS group (Table 6).
 |
Table 6 Baseline Demographic Data of Patients with Nephrotic Syndrome (Case Group) and Different Groups (Healthy Children, Children with Chronic Diseases, and Kidney Transplanted Children) (N =250) |
In comparison to control groups, in compared to the healthy group, nephrotic children, had significantly lower scores in all domains of HRQoL: social (83.5 ± 27.89) (P =0.001), physical (78.0469 ± 29.01406) (P = 0.001), school performance (71.375 ± 27.78) (P= 0.001), and emotional (80.87± 28.95) (P = 0.017) domains and also the total mean HRQoL scores (78.458 ± 24.014) (P= 0.001) scores (Table 7). In comparison with the chronic diseases group, it has manifested that children with NS had significantly lower emotional domain (80.875 ± 28.95) (P= 0.03) and total mean HRQoL scores (78.458 ± 24.014) (P= 0.006) (Table 8). However, compared with kidney transplantation children, it was demonstrated that nephrotic children had only a significantly lower score in the physical domain (P= 0.001) (Table 9).
 |
Table 7 HRQoL of Control Group 1 (Healthy Children) and Children with NS (Case Group) |
 |
Table 8 HRQoL of Control Group 2 (Children with Chronic Diseases) and Children with NS (Case Group) |
 |
Table 9 HRQoL of Control Group 3 (Kidney Transplanted Children) and Children with NS (Case Group) |
Discussion
In this study, the total mean HRQoL scores and the scores of all domains of children were significantly impaired in NS children in comparison with healthy children, which might be due to the chronic and relapsing nature of NS. The school domain was the most affected in NS children compared to the healthy group due to the regular need for follow-up, leading to frequent school absences. These findings were similar to previous reports that also found that the general QoL of children with NS substantially declined compared to that of healthy children.18,21 The same findings were observed in a study conducted at Soba Teaching Hospital, Sudan, which showed that all scores were significantly lowered in Sudanese children with NS.19
This study found that the HRQoL of children with NS was not affected by their age group, except there was significant impairment in school performance in older children. Again, the low school scores in children over eight years might be due to a regular need for a follow-up, leading to frequent school absences. Moreover, most children under eight years were not admitted to the school. This finding is to some extent similar to the finding of Roussel et al, who concluded age did not significantly associate with an influence on the QoL of children.17 This study also showed that the HRQoL of children with NS was not affected by their gender and origin. Similar findings were obtained from a study conducted in South India that documented demographic data (gender and age) did not significantly affect the total QoL scores of nephrotic children.22 These findings can be good evidence that the patient’s sociodemographic data does not affect the HRQoL of NS patients.
Children with MCNS showed significantly lower emotional, social domains, and total mean HRQoL scores than children with non-MCNS histopathology. On the contrary, the study of Mbanefo et al found that children with non-MCNS had a poorer emotional domain and total mean HRQoL scores than children with MCNS.10 Even though some studies have confirmed that the treatment prognosis of patients with MCNS is better than that of non-MCNS, this study result might be because around 60% of steroid-responsive patients experience five or more relapses.23 As relapses increase, disease duration increases accordingly. Moreover, the disparity of the HRQoL scores was determined by disease duration and severity. The scores of HRQol tend to be lower with prolonged disease duration and patient ratings of particular HRQoL domains.24,25 The change in HRQOL scores may also reflect the current state of disease activity and therapy and the cumulative psychosocial impact of the disease course, duration, and cumulative drug exposure or high drug dosage.14
This study also demonstrated no significant difference between various phenotypes of NS in the total mean HRQoL scores. A similar finding was concluded by the study done in South India.22 However, another two studies were in contrast to this finding. Mbanefo et al study concluded that subjects with SRNS had a poorer score in the emotional domain than those who were steroid-sensitive.10 Jabbar Al Qaisy et al found that infrequent relapse phenotype and newly diagnosed NS showed better QoL and significant scores in physical and emotional domains than other phenotypes.24 However, the Haiphong Children’s Hospital study found that the QoL of children with steroid-dependent and resistant INS was lower than children with a steroid-responsive type.21 Although one study found a similar result to this study’s finding, we think “it’s a weird result” because theoretically, the phenotypes of NS are more relevant to the dose and duration of immunosuppressants. There must be some difference between different phenotypes in HRQoL scores. This result might be due to the study’s small sample size, which did not show this difference.
The duration of illness significantly affected the HRQoL of children with NS, as children with less than one year of disease had significantly lower physical, social domains, and total mean HRQoL scores than children with a disease duration of more than one year. It might be due to new symptoms that affected their daily physical and social activities. Moreover, children with longer disease duration have been adapted to their status and trying to attain better QoL. Previous studies’ findings regarding how the duration of illness affects QoL of children with NS were controversial. Three studies by Selewski et al, Nguyen et al, and Solarin et al found that those with a more prolonged illness duration had a poorer QoL.14,21,26 However, a study done in South India found that the duration of illness did not significantly influence the total QoL score of the nephrotic children.22 Another study found that the impact of disease duration on HRQoL in children with NS is most common in the physical and emotional domains, as children with less than one year of illness showed worse scores in physical functioning than those with more than one year, who had worse emotional scores.10 Furthermore, hospital admission affected some HRQoL domains significantly, as inpatient children had significantly lower physical, emotional, and social scores than outpatient children. It might be because the patients who had been admitted to the hospital (inpatients) will be newly diagnosed with NS or on relapse status, leading to low HRQoL. Moreover, most outpatient children will be stable.
This study found that the disease severity indicated by edema, a greater degree of proteinuria, and infections significantly lowered physical, social, and total mean HRQoL scores of nephrotic children. Moreover, a greater degree of proteinuria significantly lowered school performance. In addition to that, the presence of edema and infections significantly lowered the emotional score. A study conducted in Nigeria had similar findings that indicated HRQoL was worse in the presence of edema and proteinuria. Children with edema had lower scores in the school performance and physical domain and total mean HRQoL scores. Moreover, the greater the degree of proteinuria in the children, the more impact HRQoL has.10 The Libório et al study also found that the last 24 hours of proteinuria were associated with worse HRQoL and depression.27
In the current study, patients on treatment had significantly lower scores in physical, emotional, and social domains and total mean HRQoL scores than those who completed their treatment. It might be because those who completed their treatment will be in remission and subsequently have a better QoL. In addition to that, the core treatment of NS is immunosuppressant drugs, which are well known for their severe adverse effects that can also lower the HRQoL of nephrotic children. The study of Nguyen et al had a similar result that showed the QoL of children who had completed their treatment was higher than those who had been still treated.21
This study compared children with NS to two other diseased groups. It found that children with NS, compared to children with chronic diseases, had significantly lower emotional domain and total mean HRQoL scores, which might be due to prolonged steroid and immunosuppressant therapy that is well known by its mood disturbance and behavioral change and accordingly affects the total mean HRQoL scores, as children with a chronic disease have been selected from these diseases; diabetes mellitus, SCA, asthma and hyperthyroidism. Two studies were done in Iraq and South India. They found that scores in all domains of QoL were significantly higher in NS children than in those with chronic diseases. Moreover, the Indian study found no difference regarding school performance.22,24 A study by Roussel et al found that children with SDNS and SRNS had a satisfactory QoL close to that of children without chronic diseases.17
In comparison with kidney transplantation children, there was no difference between the NS group and transplant group in all domains of HRQoL except “the physical domain”. Children with NS had a significantly lower physical score than the transplant, and this might be due to the most critical clinical characteristic of NS, “edema”, which limited their physical activities. A study conducted by Libório et al found that NS patients had a lower HRQoL and a higher prevalence of depression symptoms as compared to those of hemodialysis patients.27
The present study had some limitations. Firstly, it was conducted in Khartoum, which restricted the generalization of the results to all Sudanese children. Secondly, the cross-sectional nature of the study design did not allow for assessing the long-term follow-up of these study subjects. Thirdly, some hospitals record the admission with NS under the term “a general renal disease”. This term includes some other renal diseases like nephritic glomerulopathy; this prevented us from counting the total number of nephrotic cases per year, so we had to do the sampling process by a convenient sampling method. Despite all these limitations, the current study’s findings are interesting and highlight the importance of HRQoL as a function parameter to be included in NS’s management strategies. Thus, further studies with a larger sample size and adequate representation of different phenotypes, origins, and disease parameters are needed to confirm these findings.
Conclusions
The total mean HRQoL scores of children with NS were significantly lower than those of healthy children and those with chronic diseases. However, the HRQoL of children with NS was only significantly lower in physical domains than children with kidney transplantation. The phenotype of NS and the patient’s socio-demographic data, such as gender, age, and origin, had no significant effect on the total mean HRQoL scores. Disease severity evidenced by edema, a higher degree of proteinuria, infections, duration of disease, and MCNS histology significantly lowered the total mean HRQoL scores. Persistent hypertension and admissions to the hospital had a significant effect on some HRQoL domains. The total mean HRQoL scores of children on treatment were significantly lower than children who completed their treatment.
Acknowledgments
We do appreciate all participants for their voluntary participation in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bagga A, Mantan M. Nephrotic syndrome in children. Indian J Med Res. 2005;122(1):13–28.
2. Noone DG, Iijima K, Parekh R. Idiopathic nephrotic syndrome in children. Lancet. 2018;392(10141):61–74. doi:10.1016/S0140-6736(18)30536-1
3. Tapia C, Bashir K. Nephrotic Syndrome. In: StatPearls. StatPearls Publishing LLC; 2020.
4. Soliday E, Grey S, Lande MB. Behavioral effects of corticosteroids in steroid-sensitive nephrotic syndrome. Pediatrics. 1999;104(4):e51. doi:10.1542/peds.104.4.e51
5. Group W. The World Health Organization quality of life assessment (WHOQOL): the World Health Organization position paper. Soc sci med. 1995;41(10):1403–1409. doi:10.1016/0277-9536(95)00112-K
6. Hussien H, Apetrii M, Covic A. Health-related quality of life in patients with chronic kidney disease. Expert Rev Pharmac Outcomes Res. 2021;21(1):43–54. doi:10.1080/14737167.2021.1854091
7. Sprangers MA. Quality-of-life assessment in oncology. Acta Oncologica. 2002;41(3):229–237. doi:10.1080/02841860260088764
8. Chaudhry Z, Siddiqui S. Health-related quality of life assessment in Pakistani pediatric cancer patients using PedsQL™ 4.0 generic core scale and PedsQL™ cancer module. Health Qual Life Outcomes. 2012;10(52):1477–7525. doi:10.1186/1477-7525-10-52
9. Megari K. Quality of Life in Chronic Disease Patients. Health Psychol Res. 2013;1(3):e27–e. doi:10.4081/hpr.2013.932
10. Mbanefo NR, Odetunde OI, Okafor HU, et al. The clinical parameters affecting the health-related quality of life of children with nephrotic syndrome. Arch Nephrol. 2018;1(1):11–18. doi:10.22259/2639-3573.0101002
11. Tsevat J, Weeks JC, Guadagnoli E, et al. Using health-related quality-of-life information. J Gen Intern Med. 1994;9(10):576–582. doi:10.1007/BF02599287
12. Soni RK, Porter AC, Lash JP, Unruh ML. Health-related quality of life in hypertension, chronic kidney disease, and coexistent chronic health conditions. Adv Chronic Kidney Dis. 2010;17(4):002. doi:10.1053/j.ackd.2010.04.002
13. Aronu AE, Uwaezuoke SN, Muoneke UV. Reliability of generic quality-of-life instruments in assessing health-related quality of life among children and adolescents with idiopathic nephrotic syndrome: a systematic review. Health Qual Life Outcomes. 2021;19(1):144. doi:10.1186/s12955-021-01786-w
14. Selewski DT, Troost JP, Massengill SF, et al. The Impact of Disease Duration on Quality of Life in Children with Nephrotic Syndrome: A Midwest Pediatric Nephrology Consortium Study. Pediat Nephrol. 2015;30(9):1467–1476.
15. Gupta M, Nanda S, Kaushik JS. Quality of life in symptomatic HIV infected children. Indian Pediatr. 2013;50:1145–1147. doi:10.1007/s13312-013-0300-0
16. Bhima R, Coovadia H, Adhikari M. Nephrotic syndrome in South African children: changing perspectives over 20 years. Pediatr Nephrol. 1997;11(4):429–434. doi:10.1007/s004670050310
17. Roussel A, Delbet JD, Micheland L, Deschênes G, Decramer S, Ulinski T. Quality of life in children with severe forms of idiopathic nephrotic syndrome in a stable remission-A cross-sectional study. Acta Paediatr. 2019;108(12):2267–2273. doi:10.1111/apa.14912
18. Eid R, Fathy AA, Hamdy N, et al. Health-related quality of life in Egyptian children with nephrotic syndrome. Qual Life Res. 2020;29(8):2185–2196. doi:10.1007/s11136-020-02438-0
19. Allam N, Bashar A, Eid R. Assessment of health-related quality of life in Sudanese children with nephrotic syndrome: a questionnaire-based study. Pan Afr Med J. 2022;43:154. doi:10.11604/pamj.2022.43.154.34980
20. Varni JW, Seid M, Rode CA. The PedsQL™: measurement model for the pediatric quality of life inventory. Med Care. 1999;37(2):126–139. doi:10.1097/00005650-199902000-00003
21. Nguyen SN, Tran VQ, Van Vu Q. Quality of life of children with idiopathic nephrotic syndrome according to clinical types. Vietn J Sci Technol Engin. 2018;60(1):38–41. doi:10.31276/VJSTE.60(1).38
22. Agrawal S, Krishnamurthy S, Naik BN. Assessment of quality of life in children with nephrotic syndrome at a teaching hospital in South India. Saudi J Kidney Dis Transpl. 2017;28(3):593–598. doi:10.4103/1319-2442.206452
23. Eddy AA, Symons JM. Nephrotic syndrome in childhood. Lancet. 2003;362(9384):629–639. doi:10.1016/S0140-6736(03)14184-0
24. Al Qaisy UKA J, Ali SH, Ali IH. Assessment of health-related quality of life in children with nephrotic syndrome in Iraq--A comparative study. Indian J Public Health Res Dev. 2019;10:10.
25. Troost JP, Gipson DS, Carlozzi NE, et al. Using PROMIS® to create clinically meaningful profiles of nephrotic syndrome patients. Health Psychol. 2019;38(5):410–421. doi:10.1037/hea0000679
26. Solarin A, Adekunle M, Gbelee H, Animashaun A, Njokanma F. Sat-316 health related quality of life of children with nephrotic syndrome in Lagos Nigeria. Kidney Int Rep. 2019;4(7):S140. doi:10.1016/j.ekir.2019.05.358
27. Libório AB, Santos JP, Minete NF, et al. Proteinuria is associated with quality of life and depression in adults with primary glomerulopathy and preserved renal function. PLoS One. 2012;7(5):e37763. doi:10.1371/journal.pone.0037763
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
